Abstract
Background
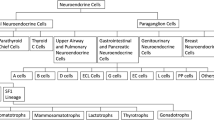
Somatostatin receptors (SSTs) are widely co-expressed in pituitary tumors. SST2 and SST5 are the most represented SST subtypes. First-generation somatostatin receptor ligands (SRLs) mainly target SST2, while pasireotide, a multi-receptor ligand, shows high binding affinity for both SST5 and SST2. Therefore, SRLs are routinely used as medical treatment for GH-, TSH-, and ACTH-secreting pituitary tumors.
Methods
Critical revision of literature data correlating SST expression with patients’ response to SRLs.
Results
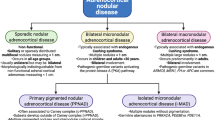
SST2 expression in somatroph tumors directly correlates with GH and IGF-1 decrease after first-generation SRL treatment. SST2 immunohistochemistry represents a valuable tool to predict biochemical response to first-generation SRLs in acromegalic patients. Pasireotide seems to exert its biological effects via SST2 in unselected patients. However, in those subjects resistant to first-generation SRLs, harbouring tumors with negligible SST2 expression, pasireotide can act throughout SST5. More than somatotroph tumors, TSH-omas represent the paradigm of tumors showing a satisfactory response to SRLs. This is probably due to the high SST2 expression observed in nearly 100% of cases, as well as to the balanced amount of SST5. In corticotroph tumors, pasireotide mainly act via SST5, although there is a need for translational studies correlating its efficacy with SST expression in this peculiar tumor histotype.
Conclusions
The assumption “more target receptor, more drug efficacy” is not straightforward for SRLs. The complex pathophysiology of SSTs, and the technical challenges faced to translate research findings into clinical practice, still need our full commitment to make receptor evaluation a worthwhile procedure for individualizing treatment decisions.

Similar content being viewed by others
References
Aflorei ED, Korbonits M (2014) Epidemiology and etiopathogenesis of pituitary adenomas. J Neurooncol 117(3):379–394. https://doi.org/10.1007/s11060-013-1354-5
Cuny T, Barlier A, Feelders R, Weryha G, Hofland LJ, Ferone D, Gatto F (2015) Medical therapies in pituitary adenomas: Current rationale for the use and future perspectives. Ann Endocrinol (Paris) 76(1):43–58. https://doi.org/10.1016/j.ando.2014.10.002
Raverot G, Burman P, McCormack A, Heaney A, Petersenn S, Popovic V, Trouillas J, Dekkers OM, European Society of E (2018) European Society of Endocrinology Clinical Practice Guidelines for the management of aggressive pituitary tumours and carcinomas. Eur J Endocrinol 178(1):G1–G24. https://doi.org/10.1530/EJE-17-0796
Serban AL, Del Sindaco G, Sala E, Carosi G, Indirli R, Rodari G, Giavoli C, Locatelli M, Carrabba G, Bertani G, Marfia G, Mantovani G, Arosio M, Ferrante E (2019) Determinants of outcome of transsphenoidal surgery for Cushing disease in a single-centre series. J Endocrinol Investig. https://doi.org/10.1007/s40618-019-01151-1
Beck-Peccoz P, Giavoli C, Lania A (2019) A 2019 update on TSH-secreting pituitary adenomas. J Endocrinol Investig 42(12):1401–1406. https://doi.org/10.1007/s40618-019-01066-x
Melmed S, Bronstein MD, Chanson P, Klibanski A, Casanueva FF, Wass JAH, Strasburger CJ, Luger A, Clemmons DR, Giustina A (2018) A consensus statement on acromegaly therapeutic outcomes. Nat Rev Endocrinol 14(9):552–561. https://doi.org/10.1038/s41574-018-0058-5
Gatto F, Hofland LJ (2011) The role of somatostatin and dopamine D2 receptors in endocrine tumors. Endocr Relat Cancer 18(6):R233–251. https://doi.org/10.1530/ERC-10-0334
Ferone D, Gatto F, Arvigo M, Resmini E, Boschetti M, Teti C, Esposito D, Minuto F (2009) The clinical-molecular interface of somatostatin, dopamine and their receptors in pituitary pathophysiology. J Mol Endocrinol 42(5):361–370. https://doi.org/10.1677/JME-08-0162
Chinezu L, Vasiljevic A, Jouanneau E, Francois P, Borda A, Trouillas J, Raverot G (2014) Expression of somatostatin receptors, SSTR2A and SSTR5, in 108 endocrine pituitary tumors using immunohistochemical detection with new specific monoclonal antibodies. Hum Pathol 45(1):71–77. https://doi.org/10.1016/j.humpath.2013.08.007
Reubi JC, Schaer JC, Waser B, Mengod G (1994) Expression and localization of somatostatin receptor SSTR1, SSTR2, and SSTR3 messenger RNAs in primary human tumors using in situ hybridization. Cancer Res 54(13):3455–3459
Greenman Y, Melmed S (1994) Expression of three somatostatin receptor subtypes in pituitary adenomas: evidence for preferential SSTR5 expression in the mammosomatotroph lineage. J Clin Endocrinol Metab 79(3):724–729. https://doi.org/10.1210/jcem.79.3.7521350
Fougner SL, Borota OC, Berg JP, Hald JK, Ramm-Pettersen J, Bollerslev J (2008) The clinical response to somatostatin analogues in acromegaly correlates to the somatostatin receptor subtype 2a protein expression of the adenoma. Clin Endocrinol (Oxf) 68(3):458–465. https://doi.org/10.1111/j.1365-2265.2007.03065.x
Wildemberg LE, Neto LV, Costa DF, Nasciuti LE, Takiya CM, Alves LM, Rebora A, Minuto F, Ferone D, Gadelha MR (2013) Low somatostatin receptor subtype 2, but not dopamine receptor subtype 2 expression predicts the lack of biochemical response of somatotropinomas to treatment with somatostatin analogs. J Endocrinol Investig 36(1):38–43. https://doi.org/10.3275/8305
Casar-Borota O, Heck A, Schulz S, Nesland JM, Ramm-Pettersen J, Lekva T, Alafuzoff I, Bollerslev J (2013) Expression of SSTR2a, but not of SSTRs 1, 3, or 5 in somatotroph adenomas assessed by monoclonal antibodies was reduced by octreotide and correlated with the acute and long-term effects of octreotide. J Clin Endocrinol Metab 98(11):E1730–E1739. https://doi.org/10.1210/Jc.2013-2145
Hofland LJ, Lamberts SW (2003) The pathophysiological consequences of somatostatin receptor internalization and resistance. Endocr Rev 24(1):28–47
Taboada GF, Luque RM, Bastos W, Guimaraes RF, Marcondes JB, Chimelli LM, Fontes R, Mata PJ, Filho PN, Carvalho DP, Kineman RD, Gadelha MR (2007) Quantitative analysis of somatostatin receptor subtype (SSTR1-5) gene expression levels in somatotropinomas and non-functioning pituitary adenomas. Eur J Endocrinol 156(1):65–74. https://doi.org/10.1530/eje.1.02313
Cuevas-Ramos D, Fleseriu M (2014) Somatostatin receptor ligands and resistance to treatment in pituitary adenomas. J Mol Endocrinol 52(3):R223–240. https://doi.org/10.1530/JME-14-0011
Gatto F, Feelders RA, van der Pas R, Kros JM, Waaijers M, Sprij-Mooij D, Neggers SJ, van der Lelij AJ, Minuto F, Lamberts SW, de Herder WW, Ferone D, Hofland LJ (2013) Immunoreactivity score using an anti-sst2A receptor monoclonal antibody strongly predicts the biochemical response to adjuvant treatment with somatostatin analogs in acromegaly. J Clin Endocrinol Metab 98(1):E66–71. https://doi.org/10.1210/jc.2012-2609
Yoshihara A, Isozaki O, Hizuka N, Nozoe Y, Harada C, Ono M, Kawamata T, Kubo O, Hori T, Takano K (2007) Expression of type 5 somatostatin receptor in TSH-secreting pituitary adenomas: a possible marker for predicting long-term response to octreotide therapy. Endocr J 54(1):133–138
Gatto F, Barbieri F, Gatti M, Wurth R, Schulz S, Ravetti JL, Zona G, Culler MD, Saveanu A, Giusti M, Minuto F, Hofland LJ, Ferone D, Florio T (2012) Balance between somatostatin and D2 receptor expression drives TSH-secreting adenoma response to somatostatin analogues and dopastatins. Clin Endocrinol (Oxf) 76(3):407–414. https://doi.org/10.1111/j.1365-2265.2011.04200.x
van der Pas R, Feelders RA, Gatto F, de Bruin C, Pereira AM, van Koetsveld PM, Sprij-Mooij DM, Waaijers AM, Dogan F, Schulz S, Kros JM, Lamberts SW, Hofland LJ (2013) Preoperative normalization of cortisol levels in Cushing's disease after medical treatment: consequences for somatostatin and dopamine receptor subtype expression and in vitro response to somatostatin analogs and dopamine agonists. J Clin Endocrinol Metab 98(12):E1880–1890. https://doi.org/10.1210/jc.2013-1987
Batista DL, Zhang X, Gejman R, Ansell PJ, Zhou Y, Johnson SA, Swearingen B, Hedley-Whyte ET, Stratakis CA, Klibanski A (2006) The effects of SOM230 on cell proliferation and adrenocorticotropin secretion in human corticotroph pituitary adenomas. J Clin Endocrinol Metab 91(11):4482–4488. https://doi.org/10.1210/jc.2006-1245
van der Hoek J, Waaijers M, van Koetsveld PM, Sprij-Mooij D, Feelders RA, Schmid HA, Schoeffter P, Hoyer D, Cervia D, Taylor JE, Culler MD, Lamberts SW, Hofland LJ (2005) Distinct functional properties of native somatostatin receptor subtype 5 compared with subtype 2 in the regulation of ACTH release by corticotroph tumor cells. Am J Physiol Endocrinol Metab 289(2):E278–287. https://doi.org/10.1152/ajpendo.00004.2005
Jaquet P, Ouafik L, Saveanu A, Gunz G, Fina F, Dufour H, Culler MD, Moreau JP, Enjalbert A (1999) Quantitative and functional expression of somatostatin receptor subtypes in human prolactinomas. J Clin Endocrinol Metab 84(9):3268–3276
Zatelli MC, Piccin D, Bottoni A, Ambrosio MR, Margutti A, Padovani R, Scanarini M, Taylor JE, Culler MD, Cavazzinidegli Uberti LEC (2004) Evidence for differential effects of selective somatostatin receptor subtype agonists on alpha-subunit and chromogranin a secretion and on cell viability in human nonfunctioning pituitary adenomas in vitro. J Clin Endocrinol Metab 89(10):5181–5188. https://doi.org/10.1210/jc.2003-031954
Ferriere A, Tabarin A (2020) Cushing's syndrome: treatment and new therapeutic approaches. Best Pract Res Clin Endocrinol Metab. https://doi.org/10.1016/j.beem.2020.101381
Puig-Domingo M, Marazuela M (2019) Precision medicine in the treatment of acromegaly. Minerva Endocrinol 44(2):169–175. https://doi.org/10.23736/S0391-1977.18.02937-1
Trouillas J, Vasiljevic A, Lapoirie M, Chinezu L, Jouanneau E, Raverot G (2019) Pathological markers of somatotroph pituitary neuroendocrine tumors predicting the response to medical treatment. Minerva Endocrinol 44(2):129–136. https://doi.org/10.23736/S0391-1977.18.02933-4
Bauer W, Briner U, Doepfner W, Haller R, Huguenin R, Marbach P, Petcher TJ, Pless T (1982) SMS 201–995: a very potent and selective octapeptide analogue of somatostatin with prolonged action. Life Sci 31(11):1133–1140. https://doi.org/10.1016/0024-3205(82)90087-x
Kuhn JM, Basin C, Mollard M, de Rouge B, Baudoin C, Obach R, Tolis G (1993) Pharmacokinetic study and effects on growth hormone secretion in healthy volunteers of the new somatostatin analogue BIM 23014. Eur J Clin Pharmacol 45(1):73–77. https://doi.org/10.1007/bf00315353
Ben-Shlomo A, Melmed S (2008) Somatostatin agonists for treatment of acromegaly. Mol Cell Endocrinol 286(1–2):192–198. https://doi.org/10.1016/j.mce.2007.11.024
Gadelha MR, Wildemberg LE, Bronstein MD, Gatto F, Ferone D (2017) Somatostatin receptor ligands in the treatment of acromegaly. Pituitary 20(1):100–108. https://doi.org/10.1007/s11102-017-0791-0
Oberg K, Lamberts SW (2016) Somatostatin analogues in acromegaly and gastroenteropancreatic neuroendocrine tumours: past, present and future. Endocr Relat Cancer 23(12):R551–R566. https://doi.org/10.1530/ERC-16-0151
Bruns C, Lewis I, Briner U, Meno-Tetang G, Weckbecker G (2002) SOM230: a novel somatostatin peptidomimetic with broad somatotropin release inhibiting factor (SRIF) receptor binding and a unique antisecretory profile. Eur J Endocrinol 146(5):707–716. https://doi.org/10.1530/eje.0.1460707
Boerlin V, van der Hoek J, Beglinger C, Poon KW, Hartmann S, Dutreix C, Kovarik JM, Bruns C, Weckbecker G, Lewis I, Schnieper P, Hofland LJ, Lamberts SW (2003) New insights on SOM230, a universal somatostatin receptor ligand. J Endocrinol Investig 26(8 Suppl):14–16
Cescato R, Loesch KA, Waser B, Macke HR, Rivier JE, Reubi JC, Schonbrunn A (2010) Agonist-biased signaling at the sst2A receptor: the multi-somatostatin analogs KE108 and SOM230 activate and antagonize distinct signaling pathways. Mol Endocrinol 24(1):240–249. https://doi.org/10.1210/me.2009-0321
Lesche S, Lehmann D, Nagel F, Schmid HA, Schulz S (2009) Differential effects of octreotide and pasireotide on somatostatin receptor internalization and trafficking in vitro. J Clin Endocrinol Metab 94(2):654–661. https://doi.org/10.1210/jc.2008-1919
Gatto F, Arvigo M, Amaru J, Campana C, Cocchiara F, Graziani G, Bruzzone E, Giusti M, Boschetti M, Ferone D (2019) Cell specific interaction of pasireotide: review of preclinical studies in somatotroph and corticotroph pituitary cells. Pituitary 22(1):89–99. https://doi.org/10.1007/s11102-018-0926-y
Jaquet P, Saveanu A, Gunz G, Fina F, Zamora AJ, Grino M, Culler MD, Moreau JP, Enjalbert A, Ouafik LH (2000) Human somatostatin receptor subtypes in acromegaly: distinct patterns of messenger ribonucleic acid expression and hormone suppression identify different tumoral phenotypes. J Clin Endocrinol Metab 85(2):781–792
Hofland LJ, van der Hoek J, van Koetsveld PM, de Herder WW, Waaijers M, Sprij-Mooij D, Bruns C, Weckbecker G, Feelders R, van der Lely AJ, Beckers A, Lamberts SW (2004) The novel somatostatin analog SOM230 is a potent inhibitor of hormone release by growth hormone- and prolactin-secreting pituitary adenomas in vitro. J Clin Endocrinol Metab 89(4):1577–1585. https://doi.org/10.1210/jc.2003-031344
Taboada GF, Luque RM, Neto LV, Machado Ede O, Sbaffi BC, Domingues RC, Marcondes JB, Chimelli LM, Fontes R, Niemeyer P, de Carvalho DP, Kineman RD, Gadelha MR (2008) Quantitative analysis of somatostatin receptor subtypes (1–5) gene expression levels in somatotropinomas and correlation to in vivo hormonal and tumor volume responses to treatment with octreotide LAR. Eur J Endocrinol 158(3):295–303. https://doi.org/10.1530/EJE-07-0562
Korner M, Waser B, Schonbrunn A, Perren A, Reubi JC (2012) Somatostatin receptor subtype 2A immunohistochemistry using a new monoclonal antibody selects tumors suitable for in vivo somatostatin receptor targeting. Am J Surg Pathol 36(2):242–252. https://doi.org/10.1097/PAS.0b013e31823d07f3
Fischer T, Doll C, Jacobs S, Kolodziej A, Stumm R, Schulz S (2008) Reassessment of sst2 somatostatin receptor expression in human normal and neoplastic tissues using the novel rabbit monoclonal antibody UMB-1. J Clin Endocrinol Metab 93(11):4519–4524. https://doi.org/10.1210/jc.2008-1063
Remmele W, Stegner HE (1987) Recommendation for uniform definition of an immunoreactive score (IRS) for immunohistochemical estrogen receptor detection (ER-ICA) in breast cancer tissue. Pathologe 8(3):138–140
Franck SE, Gatto F, van der Lely AJ, Janssen JA, Dallenga AH, Nagtegaal AP, Hofland LJ, Neggers SJ (2016) Somatostatin receptor expression in GH-secreting pituitary adenomas treated with long-acting somatostatin analogues in combination with pegvisomant. Neuroendocrinology. https://doi.org/10.1159/000448429
Inoshita N, Nishioka H (2018) The 2017 WHO classification of pituitary adenoma: overview and comments. Brain Tumor Pathol 35(2):51–56. https://doi.org/10.1007/s10014-018-0314-3
Kasajima A, Papotti M, Ito W, Brizzi MP, La Salvia A, Rapa I, Tachibana T, Yazdani S, Sasano H, Volante M (2018) High interlaboratory and interobserver agreement of somatostatin receptor immunohistochemical determination and correlation with response to somatostatin analogs. Hum Pathol 72:144–152. https://doi.org/10.1016/j.humpath.2017.11.008
Puig-Domingo M, Gil J, Sampedro-Nunez M, Jorda M, Webb SM, Serra G, Pons L, Salinas I, Blanco A, Marques-Pamies M, Valassi E, Pico A, Garcia-Martinez A, Carrato C, Buj R, Del Pozo C, Obiols G, Villabona C, Camara R, Fajardo-Montanana C, Alvarez CV, Bernabeu I, Marazuela M (2020) Molecular profiling for acromegaly treatment: a validation study. Endocr Relat Cancer 27(6):375–389. https://doi.org/10.1530/ERC-18-0565
Chiloiro S, Bima C, Tartaglione T, Giampietro A, Gessi M, Lauretti L, Anile C, Colosimo C, Rindi G, Pontecorvi A, De Marinis L, Bianchi A (2019) Pasireotide and pegvisomant combination treatment in acromegaly resistant to second-line therapies: a longitudinal study. J Clin Endocrinol Metab 104(11):5478–5482. https://doi.org/10.1210/jc.2019-00825
Muhammad A, Coopmans EC, Gatto F, Franck SE, Janssen J, van der Lely AJ, Hofland LJ, Neggers S (2019) Pasireotide responsiveness in acromegaly is mainly driven by somatostatin receptor subtype 2 expression. J Clin Endocrinol Metab 104(3):915–924. https://doi.org/10.1210/jc.2018-01524
Coelho MCA, Vasquez ML, Wildemberg LE, Vazquez-Borrego MC, Bitana L, Camacho A, Silva D, Ogino LL, Ventura N, Chimelli L, Luque RM, Kasuki L, Gadelha MR (2018) Molecular evidence and clinical importance of beta-arrestins expression in patients with acromegaly. J Cell Mol Med 22(4):2110–2116. https://doi.org/10.1111/jcmm.13427
Venegas-Moreno E, Vazquez-Borrego MC, Dios E, Gros-Herguido N, Flores-Martinez A, Rivero-Cortes E, Madrazo-Atutxa A, Japon MA, Luque RM, Castano JP, Cano DA, Soto-Moreno A (2018) Association between dopamine and somatostatin receptor expression and pharmacological response to somatostatin analogues in acromegaly. J Cell Mol Med 22(3):1640–1649. https://doi.org/10.1111/jcmm.13440
Iacovazzo D, Carlsen E, Lugli F, Chiloiro S, Piacentini S, Bianchi A, Giampietro A, Mormando M, Clear AJ, Doglietto F, Anile C, Maira G, Lauriola L, Rindi G, Roncaroli F, Pontecorvi A, Korbonits M, De Marinis L (2016) Factors predicting pasireotide responsiveness in somatotroph pituitary adenomas resistant to first-generation somatostatin analogues: an immunohistochemical study. Eur J Endocrinol 174(2):241–250. https://doi.org/10.1530/EJE-15-0832
Murray RD, Kim K, Ren SG, Lewis I, Weckbecker G, Bruns C, Melmed S (2004) The novel somatostatin ligand (SOM230) regulates human and rat anterior pituitary hormone secretion. J Clin Endocrinol Metab 89(6):3027–3032. https://doi.org/10.1210/jc.2003-031319
Ibanez-Costa A, Rivero-Cortes E, Vazquez-Borrego MC, Gahete MD, Jimenez-Reina L, Venegas-Moreno E, de la Riva A, Arraez MA, Gonzalez-Molero I, Schmid HA, Maraver-Selfa S, Gavilan-Villarejo I, Garcia-Arnes JA, Japon MA, Soto-Moreno A, Galvez MA, Luque RM, Castano JP (2016) Octreotide and pasireotide (dis)similarly inhibit pituitary tumor cells in vitro. J Endocrinol 231(2):135–145. https://doi.org/10.1530/JOE-16-0332
Gatto F, Feelders RA, Franck SE, van Koetsveld PM, Dogan F, Kros JM, Neggers S, van der Lely AJ, Lamberts SWJ, Ferone D, Hofland LJ (2017) In vitro head-to-head comparison between octreotide and pasireotide in GH-secreting pituitary adenomas. J Clin Endocrinol Metab 102(6):2009–2018. https://doi.org/10.1210/jc.2017-00135
Colao A, Bronstein MD, Freda P, Gu F, Shen CC, Gadelha M, Fleseriu M, van der Lely AJ, Farrall AJ, Hermosillo Resendiz K, Ruffin M, Chen Y, Sheppard M, Pasireotide CSG (2014) Pasireotide versus octreotide in acromegaly: a head-to-head superiority study. J Clin Endocrinol Metab 99(3):791–799. https://doi.org/10.1210/jc.2013-2480
Gadelha MR, Bronstein MD, Brue T, Coculescu M, Fleseriu M, Guitelman M, Pronin V, Raverot G, Shimon I, Lievre KK, Fleck J, Aout M, Pedroncelli AM, Colao A, Pasireotide CSG (2014) Pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controlled acromegaly (PAOLA): a randomised, phase 3 trial. Lancet Diabetes Endocrinol 2(11):875–884. https://doi.org/10.1016/S2213-8587(14)70169-X
Volante M, Brizzi MP, Faggiano A, La Rosa S, Rapa I, Ferrero A, Mansueto G, Righi L, Garancini S, Capella C, De Rosa G, Dogliotti L, Colao A, Papotti M (2007) Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy. Mod Pathol 20(11):1172–1182. https://doi.org/10.1038/modpathol.3800954
Muhammad A, Coopmans EC, Delhanty PJD, Dallenga AHG, Haitsma IK, Janssen J, van der Lely AJ, Neggers S (2018) Efficacy and safety of switching to pasireotide in acromegaly patients controlled with pegvisomant and somatostatin analogues: PAPE extension study. Eur J Endocrinol 179(5):269–277. https://doi.org/10.1530/EJE-18-0353
Rocheville M, Lange DC, Kumar U, Patel SC, Patel RC, Patel YC (2000) Receptors for dopamine and somatostatin: formation of hetero-oligomers with enhanced functional activity. Science 288(5463):154–157. https://doi.org/10.1126/science.288.5463.154
Baragli A, Alturaihi H, Watt HL, Abdallah A, Kumar U (2007) Heterooligomerization of human dopamine receptor 2 and somatostatin receptor 2 Co-immunoprecipitation and fluorescence resonance energy transfer analysis. Cell Signal 19(11):2304–2316. https://doi.org/10.1016/j.cellsig.2007.07.007
Ferone D, Saveanu A, Culler MD, Arvigo M, Rebora A, Gatto F, Minuto F, Jaquet P (2007) Novel chimeric somatostatin analogs: facts and perspectives. Eur J Endocrinol 156(Suppl 1):S23–S28. https://doi.org/10.1530/eje.1.02356
Saveanu A, Gunz G, Guillen S, Dufour H, Culler MD, Jaquet P (2006) Somatostatin and dopamine-somatostatin multiple ligands directed towards somatostatin and dopamine receptors in pituitary adenomas. Neuroendocrinology 83(3–4):258–263. https://doi.org/10.1159/000095536
Jaquet P, Gunz G, Saveanu A, Barlier A, Dufour H, Taylor J, Dong J, Kim S, Moreau JP, Culler MD (2005) BIM-23A760, a chimeric molecule directed towards somatostatin and dopamine receptors, vs universal somatostatin receptors ligands in GH-secreting pituitary adenomas partial responders to octreotide. J Endocrinol Investig 28(11 Suppl International):21–27
Jaquet P, Gunz G, Saveanu A, Dufour H, Taylor J, Dong J, Kim S, Moreau JP, Enjalbert A, Culler MD (2005) Efficacy of chimeric molecules directed towards multiple somatostatin and dopamine receptors on inhibition of GH and prolactin secretion from GH-secreting pituitary adenomas classified as partially responsive to somatostatin analog therapy. Eur J Endocrinol 153(1):135–141. https://doi.org/10.1530/eje.1.01950
Ibanez-Costa A, Lopez-Sanchez LM, Gahete MD, Rivero-Cortes E, Vazquez-Borrego MC, Galvez MA, de la Riva A, Venegas-Moreno E, Jimenez-Reina L, Moreno-Carazo A, Tinahones FJ, Maraver-Selfa S, Japon MA, Garcia-Arnes JA, Soto-Moreno A, Webb SM, Kineman RD, Culler MD, Castano JP, Luque RM (2017) BIM-23A760 influences key functional endpoints in pituitary adenomas and normal pituitaries: molecular mechanisms underlying the differential response in adenomas. Sci Rep 7:42002. https://doi.org/10.1038/srep42002
Culler MD (2011) Somatostatin-dopamine chimeras: a novel approach to treatment of neuroendocrine tumors. Horm Metab Res 43(12):854–857. https://doi.org/10.1055/s-0031-1287769
Vazquez-Borrego MC, Galvez-Moreno MA, Fuentes-Fayos AC, Venegas-Moreno E, Herrera-Martinez AD, Blanco-Acevedo C, Solivera J, Landsman T, Gahete MD, Soto-Moreno A, Culler MD, Castano JP, Luque RM (2020) A new generation somatostatin-dopamine analogue exerts potent antitumoral actions on pituitary neuroendocrine tumor cells. Neuroendocrinology 110(1–2):70–82. https://doi.org/10.1159/000500812
de Boon WMI, van Esdonk MJ, Stuurman FE, Biermasz NR, Pons L, Paty I, Burggraaf J (2019) A novel somatostatin-dopamine chimera (BIM23B065) reduced GH secretion in a first-in-human clinical trial. J Clin Endocrinol Metab 104(3):883–891. https://doi.org/10.1210/jc.2018-01364
Beck-Peccoz P, Lania A, Beckers A, Chatterjee K, Wemeau JL (2013) 2013 European thyroid association guidelines for the diagnosis and treatment of thyrotropin-secreting pituitary tumors. Eur Thyroid J 2(2):76–82. https://doi.org/10.1159/000351007
Gatto F, Grasso LF, Nazzari E, Cuny T, Anania P, Di Somma C, Colao A, Zona G, Weryha G, Pivonello R, Ferone D (2015) Clinical outcome and evidence of high rate post-surgical anterior hypopituitarism in a cohort of TSH-secreting adenoma patients: might somatostatin analogs have a role as first-line therapy? Pituitary 18(5):583–591. https://doi.org/10.1007/s11102-014-0611-8
Fukuhara N, Horiguchi K, Nishioka H, Suzuki H, Takeshita A, Takeuchi Y, Inoshita N, Yamada S (2015) Short-term preoperative octreotide treatment for TSH-secreting pituitary adenoma. Endocr J 62(1):21–27. https://doi.org/10.1507/endocrj.EJ14-0118
van Varsseveld NC, Bisschop PH, Biermasz NR, Pereira AM, Fliers E, Drent ML (2014) A long-term follow-up study of eighteen patients with thyrotrophin-secreting pituitary adenomas. Clin Endocrinol (Oxf) 80(3):395–402. https://doi.org/10.1111/cen.12290
Horiguchi K, Yamada M, Umezawa R, Satoh T, Hashimoto K, Tosaka M, Yamada S, Mori M (2007) Somatostatin receptor subtypes mRNA in TSH-secreting pituitary adenomas: a case showing a dramatic reduction in tumor size during short octreotide treatment. Endocr J 54(3):371–378. https://doi.org/10.1507/endocrj.k06-177
Capraru OM, Gaillard C, Vasiljevic A, Lasolle H, Borson-Chazot F, Raverot V, Jouanneau E, Trouillas J, Raverot G (2019) Diagnosis, pathology, and management of TSH-secreting pituitary tumors. A single-center retrospective study of 20 patients from 1981 to 2014. Ann Endocrinol (Paris) 80(4):216–224. https://doi.org/10.1016/j.ando.2019.06.006
Grant M, Alturaihi H, Jaquet P, Collier B, Kumar U (2008) Cell growth inhibition and functioning of human somatostatin receptor type 2 are modulated by receptor heterodimerization. Mol Endocrinol 22(10):2278–2292. https://doi.org/10.1210/me.2007-0334
van Eersel MEA, Meeuwisse-Pasterkamp SH, Muller Kobold AC, Meiners LC, den Dunnen WF, Hofland LJ, van den Berg G (2017) Treatment of a thyrotropin-secreting pituitary adenoma (TSH-oma) with pasireotide LAR. Clin Endocrinol (Oxf) 87(6):877–879. https://doi.org/10.1111/cen.13431
Pivonello R, De Leo M, Cozzolino A, Colao A (2015) The treatment of Cushing's disease. Endocr Rev 36(4):385–486. https://doi.org/10.1210/er.2013-1048
Stalla GK, Brockmeier SJ, Renner U, Newton C, Buchfelder M, Stalla J, Muller OA (1994) Octreotide exerts different effects in vivo and in vitro in Cushing's disease. Eur J Endocrinol 130(2):125–131. https://doi.org/10.1530/eje.0.1300125
Lamberts SW, Uitterlinden P, Klijn JM (1989) The effect of the long-acting somatostatin analogue SMS 201–995 on ACTH secretion in Nelson's syndrome and Cushing's disease. Acta Endocrinol (Copenh) 120(6):760–766. https://doi.org/10.1530/acta.0.1200760
Ambrosi B, Bochicchio D, Fadin C, Colombo P, Faglia G (1990) Failure of somatostatin and octreotide to acutely affect the hypothalamic-pituitary-adrenal function in patients with corticotropin hypersecretion. J Endocrinol Investig 13(3):257–261. https://doi.org/10.1007/BF03349555
Hofland LJ, van der Hoek J, Feelders R, van Aken MO, van Koetsveld PM, Waaijers M, Sprij-Mooij D, Bruns C, Weckbecker G, de Herder WW, Beckers A, Lamberts SW (2005) The multi-ligand somatostatin analogue SOM230 inhibits ACTH secretion by cultured human corticotroph adenomas via somatostatin receptor type 5. Eur J Endocrinol 152(4):645–654. https://doi.org/10.1530/eje.1.01876
Ben-Shlomo A, Schmid H, Wawrowsky K, Pichurin O, Hubina E, Chesnokova V, Liu NA, Culler M, Melmed S (2009) Differential ligand-mediated pituitary somatostatin receptor subtype signaling: implications for corticotroph tumor therapy. J Clin Endocrinol Metab 94(11):4342–4350. https://doi.org/10.1210/jc.2009-1311
de Bruin C, Pereira AM, Feelders RA, Romijn JA, Roelfsema F, Sprij-Mooij DM, van Aken MO, van der Lelij AJ, de Herder WW, Lamberts SW, Hofland LJ (2009) Coexpression of dopamine and somatostatin receptor subtypes in corticotroph adenomas. J Clin Endocrinol Metab 94(4):1118–1124. https://doi.org/10.1210/jc.2008-2101
Behling F, Honegger J, Skardelly M, Gepfner-Tuma I, Tabatabai G, Tatagiba M, Schittenhelm J (2018) High expression of somatostatin receptors 2A, 3, and 5 in corticotroph pituitary adenoma. Int J Endocrinol 2018:1763735. https://doi.org/10.1155/2018/1763735
Hayashi K, Inoshita N, Kawaguchi K, Ibrahim Ardisasmita A, Suzuki H, Fukuhara N, Okada M, Nishioka H, Takeuchi Y, Komada M, Takeshita A, Yamada S (2016) The USP8 mutational status may predict drug susceptibility in corticotroph adenomas of Cushing's disease. Eur J Endocrinol 174(2):213–226. https://doi.org/10.1530/EJE-15-0689
Melmed S (2020) Pituitary-tumor endocrinopathies. N Engl J Med 382(10):937–950. https://doi.org/10.1056/NEJMra1810772
de Bruin C, Hofland LJ, Nieman LK, van Koetsveld PM, Waaijers AM, Sprij-Mooij DM, van Essen M, Lamberts SW, de Herder WW, Feelders RA (2012) Mifepristone effects on tumor somatostatin receptor expression in two patients with Cushing's syndrome due to ectopic adrenocorticotropin secretion. J Clin Endocrinol Metab 97(2):455–462. https://doi.org/10.1210/jc.2011-1264
Colao A, Petersenn S, Newell-Price J, Findling JW, Gu F, Maldonado M, Schoenherr U, Mills D, Salgado LR, Biller BM, Pasireotide BSG (2012) A 12-month phase 3 study of pasireotide in Cushing's disease. N Engl J Med 366(10):914–924. https://doi.org/10.1056/NEJMoa1105743
Lacroix A, Gu F, Gallardo W, Pivonello R, Yu Y, Witek P, Boscaro M, Salvatori R, Yamada M, Tauchmanova L, Roughton M, Ravichandran S, Petersenn S, Biller BMK, Newell-Price J, Pasireotide GSG (2018) Efficacy and safety of once-monthly pasireotide in Cushing's disease: a 12 month clinical trial. Lancet Diabetes Endocrinol 6(1):17–26. https://doi.org/10.1016/S2213-8587(17)30326-1
Asa SL, Ezzat S (2009) The pathogenesis of pituitary tumors. Annu Rev Pathol 4:97–126. https://doi.org/10.1146/annurev.pathol.4.110807.092259
Lee M, Lupp A, Mendoza N, Martin N, Beschorner R, Honegger J, Schlegel J, Shively T, Pulz E, Schulz S, Roncaroli F, Pellegata NS (2015) SSTR3 is a putative target for the medical treatment of gonadotroph adenomas of the pituitary. Endocr Relat Cancer 22(1):111–119. https://doi.org/10.1530/ERC-14-0472
Oystese KA, Casar-Borota O, Normann KR, Zucknick M, Berg JP, Bollerslev J (2017) Estrogen receptor alpha, a sex-dependent predictor of aggressiveness in nonfunctioning pituitary adenomas: SSTR and sex hormone receptor distribution in NFPA. J Clin Endocrinol Metab 102(9):3581–3590. https://doi.org/10.1210/jc.2017-00792
Colao A, Di Somma C, Pivonello R, Faggiano A, Lombardi G, Savastano S (2008) Medical therapy for clinically non-functioning pituitary adenomas. Endocr Relat Cancer 15(4):905–915. https://doi.org/10.1677/ERC-08-0181
Florio T, Thellung S, Arena S, Corsaro A, Spaziante R, Gussoni G, Acuto G, Giusti M, Giordano G, Schettini G (1999) Somatostatin and its analog lanreotide inhibit the proliferation of dispersed human non-functioning pituitary adenoma cells in vitro. Eur J Endocrinol 141(4):396–408. https://doi.org/10.1530/eje.0.1410396
Florio T, Barbieri F, Spaziante R, Zona G, Hofland LJ, van Koetsveld PM, Feelders RA, Stalla GK, Theodoropoulou M, Culler MD, Dong J, Taylor JE, Moreau JP, Saveanu A, Gunz G, Dufour H, Jaquet P (2008) Efficacy of a dopamine-somatostatin chimeric molecule, BIM-23A760, in the control of cell growth from primary cultures of human non-functioning pituitary adenomas: a multi-center study. Endocr Relat Cancer 15(2):583–596. https://doi.org/10.1677/ERC-07-0271
Zatelli MC, Piccin D, Vignali C, Tagliati F, Ambrosio MR, Bondanelli M, Cimino V, Bianchi A, Schmid HA, Scanarini M, Pontecorvi A, De Marinis L, Mairadegli Uberti GEC (2007) Pasireotide, a multiple somatostatin receptor subtypes ligand, reduces cell viability in non-functioning pituitary adenomas by inhibiting vascular endothelial growth factor secretion. Endocr Relat Cancer 14(1):91–102. https://doi.org/10.1677/ERC-06-0026
Vazquez-Borrego MC, Gupta V, Ibanez-Costa A, Gahete MD, Venegas-Moreno E, Toledano-Delgado A, Cano DA, Blanco-Acevedo C, Ortega-Salas R, Japon MA, Barrera-Martin A, Vasiljevic A, Hill J, Zhang S, Halem H, Solivera J, Raverot G, Galvez MA, Soto-Moreno A, Paez-Pereda M, Culler MD, Castano JP, Luque RM (2020) A somatostatin receptor subtype-3 (SST3) peptide agonist shows antitumor effects in experimental models of nonfunctioning pituitary tumors. Clin Cancer Res 26(4):957–969. https://doi.org/10.1158/1078-0432.CCR-19-2154
Fuentes-Fayos AC, Garcia-Martinez A, Herrera-Martinez AD, Jimenez-Vacas JM, Vazquez-Borrego MC, Castano JP, Pico A, Gahete MD, Luque RM (2019) Molecular determinants of the response to medical treatment of growth hormone secreting pituitary neuroendocrine tumors. Minerva Endocrinol 44(2):109–128. https://doi.org/10.23736/S0391-1977.19.02970-5
Hofland LJ, Lamberts SW (2003) The pathophysiological consequences of somatostatin receptor internalization and resistance. Endocr Rev 24(1):28–47. https://doi.org/10.1210/er.2000-0001
Acknowledgments
F.G. sincerely thanks the Italian Society of Endocrinology for awarding with the “Premio SIE 35”, as Best Young Researcher in 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F.G. received fees for lectures and/or participation to advisory boards for Novartis, AMCo, and IONIS Pharmaceuticals. D.F. received grants and fees for lectures and participation to advisory boards for Novartis, Ipsen and Pfizer. M.A. has nothing to disclose.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No Informed Consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gatto, F., Arvigo, M. & Ferone, D. Somatostatin receptor expression and patients’ response to targeted medical treatment in pituitary tumors: evidences and controversies. J Endocrinol Invest 43, 1543–1553 (2020). https://doi.org/10.1007/s40618-020-01335-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01335-0