Abstract
Purpose
Polycystic ovary syndrome (PCOS) is the most common cause of chronic anovulation with a prevalence of 5–10% in women of reproductive age. The etiology of this disease is not well known, and hepcidin is one of the factors affecting the pathogenesis of the disease. The aim of this study was to evaluate plasma levels of hepcidin in patients with PCOS and its correlation with serum iron level.
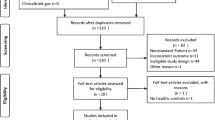
Methods
In this case-control study, plasma levels of hepcidin, IL-6, and ferritin using ELISA method and serum iron levels using a spectrophotometric method were tested on 56 women with PCOS (case group) and 41 healthy subjects (control group). The results were analyzed using t test, General Linear Model, Binary logistic regression, and linear regression tests.
Results
The mean hepcidin levels were 1.97 ± 0.53 and 2.40 ± 0.25 pg/ml in the case and control groups, respectively. The t-test results showed significant difference between the two groups (p = 0.0001). The mean serum iron levels were 72.89 ± 28.97 and 70.62 ± 31.18 g/dl in the case and control groups, respectively. The t test analysis indicated no significant difference between the two groups. The serum ferritin and iron levels had no significant relation with serum hepcidin level in two groups.
Conclusion
Despite the differences in the serum levels of hepcidin between the two groups, no significant relation was observed between serum iron levels and hepcidin level in this group of patients. This implies the need for more comprehensive studies on gene expression in hepcidin and iron pathways using real-time and Western techniques to investigate more precisely serum hepcidin level and its relationship with the factors mentioned.
Similar content being viewed by others
References
Kumarapeli V et al (2008) A simple screening approach for assessing community prevalence and phenotype of polycystic ovary syndrome in a semiurban population in Sri lanka. Am J Epidemiol 168(3):321–328
Duncan WC (2014) A guide to understanding polycystic ovary syndrome (PCOS). J Fam Plan Reprod Health Care 40(3):217–225
Cakiroglu Y et al (2016) The inflammatory markers in polycystic ovary syndrome: association with obesity and IVF outcomes. J Endocrinol Invest 39(8):899–907
4-Kucukaydin Z et al (2016) Plasma total oxidant and antioxidant status after oral glucose tolerance and mixed meal tests in patients with polycystic ovary syndrome. J Endocrinol Invest 39(10):1139–1148
Polak K et al (2017) New markers of insulin resistance in polycystic ovary syndrome. J Endocrinol Invest 40(1):1–8
Lord JM et al (2003) Insulin-sensitising drugs (metformin, troglitazone, rosiglitazone, pioglitazone, d-chiro-inositol) for polycystic ovary syndrome. Cochrane Database Syst Rev 3:CD003053.
Ganz T (2006) Hepcidin and its role in regulating systemic iron metabolism. Hematol Am Soc Hematol Educ Program 29–35:507 (Review).
Lee P et al (2005) Regulation of hepcidin transcription by interleukin-1 and interleukin-6. Proc Natl Acad Sci USA 102(6):1906–1910
Kanda J et al (2008) Serum hepcidin level and erythropoietic activity after hematopoietic stem cell transplantation. Haematologica 93(10):1550–1554
Lauth X et al (2005) Bass hepcidin synthesis, solution structure, antimicrobial activities and synergism, and in vivo hepatic response to bacterial infections. J Biol Chem 280(10):9272–9282
Dede S (2008) Plasma Levels of zinc, copper, copper/zinc ratio, and activity of carbonic anhydrase in equine piroplasmosis. Biol Trace Elem Res 125(1):41–45
Datz C et al (2013) Iron homeostasis in the metabolic syndrome. Eur J Clin Invest 43(2):215–224
Sam AH et al (2013) Hepcidin levels in diabetes mellitus and polycystic ovary syndrome. Diabet Med 30(12):1495–1499
Luque-Ramírez M et al (2011) Role of decreased circulating hepcidin concentrations in the iron excess of women with the polycystic ovary syndrome. J Clin Endocrinol Metab 96(3):846–852
Luque-Ramírez M et al (2007) Increased body iron stores of obese women with polycystic ovary syndrome are a consequence of insulin resistance and hyperinsulinism and are not a result of reduced menstrual losses. Diabetes Care 30(9):2309–2313
Kumarapeli V et al (2008) A simple screening approach for assessing community prevalence and phenotype of polycystic ovary syndrome ina semiurban population in Sri lanka. Am J Epidemiol 168(3):321–328
Fernández-Real JM et al (2009) Study of circulating prohepcidin in association with insulin sensitivity and changing iron stores. J Clin Endocrinol Metab 94(3):982–988
Le Guenno G et al(2007)Study of iron metabolism disturbances in an animal model of insulin resistance. Diabetes Res Clin Pract 77(3):363–370
Wang H et al (2014) Hepcidin is directly regulated by insulin and plays an important role in iron overload in streptozotocin-induced diabetic rats. Diabetes 63(5):1506–1518
Insenser M et al (2010) Proteomic analysis of plasma in the polycystic ovary syndrome identifies novel markers involved in iron metabolism, acute-phase response, and inflammation. J Clinical Endocrinol Metab 95(8):3863–3870
Xu X et al (2014) Effect of metformin on serum interleukin-6 levels in polycystic ovary syndrome: a systematic review. BMC women’s health 14:93.
Ahmed HH et al (2015) Impact of long term metformin therapy on hepcidin and iron status in type II diabetic patients. Int J Pharm Clin Res 7(3):185–193
Gözdemir E et al (2013) Is hepcidin a new cardiovascular risk marker in polycystic ovary syndrome? Gynecol Obstet Invest 75(3):196–202
Taghavi M et al (2009) Evaluation of body iron stores in non-Over weight women with polycystic ovarian syndrome and its correlation with Insulin resistance. Iran J Endocrinol Metab 10(3):600–603
Li M et al (2016) Serum macroelement and microelement concentrations in patients with polycystic ovary syndrome: a cross-sectional study. Biol Trace Elem Res 176(1):73–80
Escobar-Morreale HF et al (2011) Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril 95(3):1048–1058
Ko PC et al (2015) Serum ferritin levels and polycystic ovary syndrome in obese and nonobese women. Taiwan J Obstet Gynecol 54(4):403–407
Dongiovanni P et al (2011) Iron in fatty liver and in the metabolic syndrome: a promising therapeutic target. J Hepatol 55(4):920–932
DeUgarte CM et al (2005) Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil steril 83(5):1454–1460
Piperno A et al (2011) HIGHCARE investigators. Modulation of hepcidin production during hypoxia-induced erythropoiesis in humans in vivo: data from the HIGHCARE project. Blood 117(10):2953–2959
Azziz R et al (2001) Troglitazone improves ovulation and hirsutism in the polycystic ovary syndrome: a multicenter, double blind, placebo-controlled trial. J Clin Endocrinol Metab 86(4):1626–1632
Liu J etal(2016) Hepcidin: A promising therapeutic target for iron disorders: a systematic review. Med (Baltim) 95(14):e3150
Park CH et al (2001) Hepcidin, a urinary antimicrobial peptide synthesized in the liver. Biol Chem 276(11):7806
Nemeth E et al (2004) IL.6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest 113(9):1271–1276
Zechel S et al (2006) Distribution of the iron-regulating protein hepcidin in the murine central nervous system. J NeurosciRes 84(4):790–800
Wang SM et al (2010) Role of hepcidin in murine brain iron metabolism. Cell Mol Life Sci 67(1):123–133
Acknowledgements
This article has been extracted from M.D. thesis (Reference number 93-01-39-25278) conducted in Tehran University of Medical Sciences and it was carried out with financial support from Research Deputy of Tehran University of Medical Sciences. The authors express their thanks and appreciations to Maryam Bagheri and Masomeh Masoumi for their cooperation in the project.
Funding
This research received financial support from Research Deputy of Tehran University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and the Helsinki Declaration. This article does not contain any studies with animals performed by any of the authors.
Informed consent
All patients included in the study gave their informed consent.
Rights and permissions
About this article
Cite this article
Hossein Rashidi, B., Shams, S., Shariat, M. et al. Evaluation of serum hepcidin and iron levels in patients with PCOS: a case-control study. J Endocrinol Invest 40, 779–784 (2017). https://doi.org/10.1007/s40618-017-0632-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0632-z