Abstract
Background
Sedentary behavior has been identified as a significant risk factor for Metabolic Syndrome (MetS). However, it is unclear if the sedentary pattern measurement approach (posture vs. movement) impacts observed associations or if associations differ for Hispanic/Latino communities, who have higher risk of MetS.
Methods
Participants from the Community of Mine (CoM) study (N = 602) wore hip-based accelerometers for 14 days and completed MetS-associated biomarker assessment (triglycerides, blood pressure, fasting glucose, HDL cholesterol, waist circumference). Sedentary patterns were classified using both cutpoints (movement-based) and the Convolutional Neural Network Hip Accelerometer Posture (CHAP) algorithm (posture-based). We used logistic regression to estimate associations between MetS with sedentary patterns overall and stratified by Hispanic/Latino ethnicity.
Results
CHAP and cutpoint sedentary patterns were consistently associated with MetS. When controlling for total sedentary time and moderate to vigorous physical activity, only CHAP-measured median sedentary bout duration (OR = 1.15, CI: 1.04, 1.28) was significant. In stratified analysis, CHAP-measured median bout duration and time spent in sedentary bouts ≥ 30 min were each associated with increased odds of MetS, but the respective associations were stronger for Hispanic/Latino ethnicity (OR = 1.71 and 1.48; CI = 1.28–2.31 and 1.12–1.98) than for non-Hispanic/Latino ethnicity (OR = 1.43 and 1.40; CI = 1.10–1.87 and 1.06–1.87).
Conclusions
The way sedentary patterns are measured can impact the strength and precision of associations with MetS. These differences may be larger in Hispanic/Latino ethnic groups and warrants further research to inform sedentary behavioral interventions in these populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS) is a group of conditions including abdominal obesity, high blood pressure, high blood sugar levels, high blood triglycerides, and low HDL cholesterol, which together raise an individual’s risk for heart disease, diabetes, and several cancers [1]. Sedentary behavior, both self-reported and device-measured, has been identified as a significant risk factor for MetS [2,3,4,5,6,7]. Sedentary behavior is defined as all waking behaviors while in a sitting or lying position with energy expenditure ≤ 1.5 metabolic equivalents [8]. Sedentary behavior can be measured as total time spent being sedentary, or as sedentary patterns that are regular discernible sequences of sedentary behavior accumulation such as bouts or diversity of bout length [9]. Some studies investigating sedentary patterns have found that increased breaks in sedentary time and shorter sedentary bouts have beneficial effects on MetS components and related outcomes [10,11,12,13]. However, these studies have used measures that capture low movement (e.g., low accelerometer counts) but not the postural sitting or lying component key to the sedentary behavioral definition. Recent studies have shown that movement-based measures (e.g., cutpoints) show different rates of sedentary patterns than posture-based measures (e.g., activPAL) [14,15,16].
Research on sedentary patterns using posture-based measures and MetS or related health outcomes is limited and has produced mixed results [6, 17]. Reported study differences may underscore the sensitivity of posture-based measures to sedentary behaviors in a particular cohort and emphasize the need for a larger body of evidence examining the relationship between posture-based sedentary behaviors and MetS. This may be particularly true for ethnic minorities who experience an increased risk of MetS, and for whom posture-based interventions may help to reduce observed disparities.
Hispanics/Latinos in the US are at increased risk of MetS and suffer from increased rates of diabetes compared to non-Hispanic whites [18,19,20,21]. While observational studies suggest less sitting time among Hispanic/Latino adults compared to non-Hispanic whites, there is not a well-established body of literature on the relationship between MetS and sedentary time or patterns in Hispanic/Latino populations [22,23,24]. Furthermore, reduction of sedentary time may attenuate genetic associations with obesity in this population [25]. There are few assessments of sedentary patterns in the adult Hispanic/Latino population, all of which utilize movement-based measures. Only three studies currently relate sedentary patterns to metabolic outcomes in Hispanics/Latinos, finding significant and deleterious associations of prolonged and uninterrupted sedentary bouts with glucose biomarkers, obesity, and cardiometabolic biomarkers. [26,27,28]
Here we build upon previous literature by comparing associations of movement- and posture-based sedentary patterns to MetS in an ethnically diverse cohort. We draw on the Convolutional Neural Network Hip Accelerometer Posture (CHAP) algorithm; a deep neural network algorithm developed to classify sitting/lying versus non-sedentary behavioral postures [29, 30]. We add to limited research on sedentary pattern effects on MetS in minorities by assessing if associations between sedentary patterns and MetS are different for Hispanic/Latino and non-Hispanic individuals.
Methods
Participants
The Community of Mine (CoM) study enrolled 602 participants aged 35–80 years living in San Diego County from 2014–2017. The study collected behavioral, clinical, and biomarker outcomes related to cancer risk with the main study aim of advancing cancer risk exposure assessment; full details have been published elsewhere [31]. The cross-sectional study recruited adults able to walk without human assistance and willing to wear study sensors for two weeks, with a goal of oversampling participants identifying as Hispanic/Latino. Ethics approval was obtained from the University of California San Diego Institutional Review Board (protocol #140,510).
Metabolic Syndrome and Covariates
Participants attended a clinic visit where blood pressure, height, and weight were recorded, and fasting blood samples were collected. Metabolic syndrome was defined using diagnostic criteria of the American Heart Association and National Heart, Lung, and Blood Institute, updated from the NCEP ATP III definition [32]. The presence of MetS (yes/no) was indicated if ≥ 3 of the following conditions were met: 1) elevated waist circumference (≥ 102 cm in males, ≥ 88 cm in females); 2) elevated triglycerides (≥ 150 mg/dL); 3) reduced HDL cholesterol (HDL-C; < 40 mg/dL in males, < 50 mg/dL in females); 4) elevated blood pressure (≥ 130 mmHg systolic or ≥ 85 mmHg diastolic); or 5) elevated fasting glucose (≥ 100 mg/dL).
Demographic covariates were assessed via survey and included age (years), sex (female or male), education (high school or less; associates/bachelor’s degree; graduate degree or higher), and ethnicity (Hispanic/Latino or not). Medications taken by participants were noted during their clinic visit and categorized by their clinical indication (summary in Supplement Table 1). A covariate was included for all participants based on if they were taking medications for the treatment of MetS components (yes/no) including elevated triglycerides, reduced HDL-C, elevated glucose, or hypertension.
Sedentary Behavior Measurement and Definitions
Participants were asked to wear an ActiGraph GT3X + accelerometer (ActiGraph LLC, Pensacola, FL, USA) on the right hip for 14 days. Non-wear time was identified using the validated Choi algorithm for vector magnitude signal [32]. Valid wear days were defined as having ≥ 10 h of wear time and participants were required to have at least 2 valid wear days. Movement-based measures of total sedentary time and sedentary patterns were derived using count per minute (cpm) cutpoint thresholds consistent with standard practice in accelerometry [33]. A cutpoint threshold of < 100 cpm on the vertical axis was used to classify 1-min epochs as sedentary time. Moderate to vigorous physical activity (MVPA) was also derived using the cutpoint method and was defined using the Troiano cutpoint of ≥ 2020 cpm. [34] Posture-based measures of total sedentary time and sedentary patterns were calculated using the CHAP-adult algorithm, which has been described in detail elsewhere [29, 30, 35], and can be found online [36]. Briefly, CHAP calculates sedentary behavior by defining bouts of sitting and/or lying postures as well as posture transitions from sitting/lying to standing using hip-worn triaxial accelerometer data. It has a mean balanced accuracy of 93% for distinguishing sitting and non-sitting as validated against activPAL posture measures. Here, CHAP-adult was run on the 10-Hz raw triaxial ActiGraph data, and the output was given in 10-s epochs covering the same overall time span as the 60-s epoch cutpoint output. Non-wear time and valid wear days were matched between methods by cross-referencing the corresponding 60-s epoch data for each 10-s CHAP epoch.
For both the cutpoint (movement-based) and CHAP (posture-based) methods, sedentary time and sedentary patterns were analyzed using the sb_summary_bouts function in the PBpatterns R package (version 0.1.0.9000), which outputs a variety of summary measures related to sedentary behaviors [37]. The full list of measures, descriptions, and calculation is in Supplement Table 2. Bouts were defined as periods of sedentary time lasting ≥ 1 min and a break in sedentary time was defined as any time a sedentary minute was followed by a non-sedentary minute (no allowance for interruptions, i.e., no tolerance). Sedentary pattern variables included time in bouts lasting ≥ 30 min, the median duration of all sedentary bouts, and the number of daily breaks in sedentary time (Supplement Table 2). Percentage of wear time spent sedentary (a standardized indicator of total sedentary time) was calculated by dividing total sedentary time by total wear time.
Statistical Analysis
Descriptive statistics were calculated for the full sample and stratified by MetS (yes/no). Additional descriptive statistics were calculated for the sedentary time and pattern measures by MetS and Hispanic/Latino ethnicity. Pearson correlations within cutpoint and CHAP measures were calculated to aid in selection of measures, focusing on those least correlated with each other to reduce redundancy in modeling. Paired t tests assessed differences between cutpoint and CHAP measures of sedentary time and patterns for the full sample, by MetS, and by Hispanics/Latino ethnicity. Logistic regression models assessed cutpoint and CHAP sedentary time and pattern associations with MetS, including the covariates of sex, age, education, ethnicity, MetS-related medication use, and device wear time. Two models were assessed: the base model with covariates only and the fully adjusted model which additionally controlled for MVPA and percent of total time sedentary. Interaction analysis was conducted for both models to test interaction between each sedentary pattern*Hispanic/Latino ethnicity, with likelihood ratio test performed to assess significant model fit improvement between the original and interaction model. Finally, models were stratified by Hispanic/Latino ethnicity. Results are reported as standardized odds ratios with confidence intervals, with significance set at p < 0.05 (two-tailed). All statistical analyses were conducted in R v.4.1.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Study Sample
From the 602 participants enrolled, a final sample of 579 were included in this study. We excluded participants that did not have covariate or outcome data (n = 18) or did not have sufficient valid wear accelerometer data (n = 5). Participants wore accelerometers for an average of 12.5 valid days (min 2, max 25, std 2.6), with an average of 14.4 h of daily valid wear time (min 11.6, max 20.3, std 1.3). In total, 26.4% of participants met three or more conditions for classification as having Metabolic Syndrome. More Hispanic/Latino participants had MetS (14.7%) than non-Hispanic participants (11.7%). Those with MetS averaged about 10 fewer minutes of MVPA per day compared to participants without MetS (Table 1).
Comparing cutpoint and CHAP measures of sedentary behavior
Sedentary time and pattern correlations for all cutpoint and CHAP measures are in Supplement Figs. 1 and 2, respectively. Several variables were highly correlated for both cutpoint and CHAP, including mean sedentary bout duration, sedentary bout frequency, and sedentary hours per day. Thus, these variables were excluded from further analysis. Lower correlations were observed for percent total sedentary time (0.82), mean sedentary breaks per day (0.54), median sedentary bout duration (0.53), and hours in bouts ≥ 30 min (0.82), which were retained for further analysis. All correlations were significant at p < 0.001.
For the total sample, the cutpoint measure of mean percent total sedentary time (61.1%, SD = 10.4%) and CHAP measured time (60.7%, SD = 12.2%) were not significantly different, nor when stratified by MetS (Table 2). When stratified by Hispanic/Latino ethnicity, cutpoint mean percent total sedentary time, 58.2% (SD = 11.0%) was significantly higher than CHAP measured time, 57.0% (SD = 12.5%; p = 0.009) for Hispanic/Latinos (Table 2). While estimates of total sedentary time were largely similar between cutpoint and CHAP, all of the sedentary patterns were significantly different. For example, cutpoint estimates of mean sedentary breaks per day, 83.0 (SD = 15.7) was higher than CHAP estimates, 44.3 (SD = 11.9; p < 0.001) for the total sample and this relationship was similar across MetS and Hispanic/Latino stratifications (Table 2).
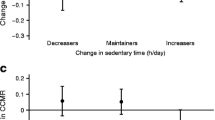
Associations of Sedentary Patterns with Total Sample MetS
Model 1 results show significant associations of similar effect magnitude (OR = 0.78) between both cutpoint and CHAP measures of mean breaks per day and MetS, and stronger associations for CHAP measures of median bout duration and hours in bouts ≥ 30 min compared to cutpoint measures (Table 3). A one standard deviation increase in cutpoint measured median sedentary bout duration was associated with 1.36 times the odds of MetS (p = 0.002), whereas a one standard deviation increase in CHAP measured median sedentary bout duration was associated with 1.56 times the odds of MetS (p < 0.0001).
Model 2 controlled for both MVPA and percent of total time spent sedentary (Table 3). The one significant sedentary pattern was the CHAP median bout duration (OR = 1.15, 95% CI = 1.04, 1.28; p = 0.008).
Associations of Sedentary Patterns with MetS Stratified by Hispanic/Latino Ethnicity
Results for interaction analysis are found in Supplement Table 3. Interaction terms (sedentary pattern*Hispanic/Latino) are not significant for any model, and all likelihood ratio test results comparing each model and model b version (with the interaction term) are null. While the interactions were not significant, there were still qualitative differences in MetS odds ratios by Hispanic/Latino for sedentary patterns. For example, a one standard deviation increase in CHAP median bouts per day for Hispanic/Latinos was associated with 1.71 times the odds of MetS (p = 0.0004), whereas for non-Hispanic/Latinos the odds were less, 1.43 (p = 0.008) (Table 4). In general, CHAP sedentary pattern measures are more precise and more consistently associated with MetS for both Hispanics/Latinos and non-Hispanics compared to cutpoint measures.
Discussion
This study compared associations between movement-based cutpoint and posture-based CHAP sedentary measures with Metabolic Syndrome in a sample of 579 adults, with stratified analysis for Hispanic/Latino ethnicity. While CHAP and cutpoint measures estimate similar total amounts of sedentary time, CHAP estimated less interrupted patterning (half the number of breaks, double the length of bouts) of sedentary behavior, all of which were significantly different from cutpoint measures. One important finding is that these patterns held consistent when stratified by MetS or Hispanic/Latino, except for percent total sedentary time. In previous research in an older adult population, agreement for total sedentary time, hours in bouts ≥ 30 min, and breaks in sedentary time between methods had a Pearson correlation of 0.66, 0.78, and 0.51 respectively. [15] In a study of 1,457 people, Edwardson et al. saw a lower between-method correlation of total sedentary time (0.51) and for average number of breaks in sitting per day (0.42) [38]. Taken together, these findings build a body of evidence across age spectrums and health outcomes that while there is general agreement between movement- and posture-based measures in detecting total sedentary time and sedentary patterns, movement-based measures detect more breaks in sedentary time than posture-based measures [16]. This study adds that there may be differences in movement and postural patterns in Hispanics/Latinos that warrant further study.
Model results had expected direction of associations between both measurement methods with MetS. Both longer bout durations and hours in bouts ≥ 30 min were associated with greater odds of MetS, while increasing breaks per day lowered odds. Levels of PA are an important factor, independent of sedentary behaviors, in the study of sedentary behaviors and MetS [13, 39]. There is some debate as to the need for adjusting for PA in studies of sedentary behavior [40], however, time spent in PA and higher intensities of PA have been shown to lower odds of MetS [41,42,43]. Replacing sedentary time with PA was associated with greater MetS risk reduction than modifying either behavior alone [44]. Furthermore, breaking up sedentary time with PA breaks is associated with a reduction in some components of MetS [45]. To assess these two factors, model 1 controlled only for covariates and model 2 added MVPA and percent of time in sedentary. In model 2, only CHAP measured median bout duration was significant, indicating that sedentary bout duration may have a biomechanical pathway to MetS independent of total sedentary time and MVPA.
An important contribution is the stratified analysis focusing on the Hispanic/Latino participants compared to non-Hispanic participants. Hispanic/Latino participants were 1.7 times more likely to have MetS for every 1 standard deviation increase in median sedentary bout duration compared to non-Hispanics. However, Hispanic/Latino participants spent fewer hours in bouts ≥ 30 min (mean = 2.3) compared to non-Hispanic/Latino participants (mean = 3.1) and a lower percent of overall time sedentary, 58.2% compared to 63.3%, respectively. The significant finding was the discrepancy in the CHAP posture-based method’s sensitivity to significant associations in the Hispanic/Latino population compared to the cutpoint movement-based method. It is unclear if this is due to ethnic differences in posture-based sedentary behaviors, differences in the relationship between behaviors with MetS, or if perhaps the lower rates of sedentary time and more disrupted sedentary patterns in the Hispanic/Latino population necessitate more accurate measurement of each postural change. This is an area of needed further study, as our ability to accurately measure differences in behavioral patterns and their associations with MetS may be an important aspect of accounting for and intervening on metabolic health disparities in Hispanics/Latinos. In Chang et al. interaction analysis showed that association between movement-based mean sitting bout duration and fasting glucose concentration was significantly stronger among Hispanic/Latina women than non-Hispanic women [26]. Larsen et al., found that Hispanics/Latinos self-reported sitting significantly less than non-Hispanic whites, yet had more than double the odds of having diabetes after adjusting for total sitting time [24]. They concluded that differences in sedentary time likely do not contribute to ethnic disparities in type 2 diabetes, but were unable to explore sedentary patterns due to self-report measurement. Our findings indicate that sedentary patterns did have stronger associations with MetS in Hispanics/Latinos compared to non-Hispanics, and posture-based measures captured this association more consistently and precisely than movement-based measures.
As research into intervening on sedentary behaviors increases, several studies are finding replacing sitting time with walking and standing yields similar and even better improvements in glucose response, insulin resistance, triacylglycerol measures, and MetS than MVPA [45,46,47,48]. In Hispanics/Latinos, less sedentary time, but not MVPA was associated with improved cardiovascular risk factors [49]. However, many of these studies are being designed around movement-based assessment of sedentary behaviors. This study provides further evidence that not only are movement-based assessments potentially overestimating postural changes associated with sedentary behavior, but they may also not be able to precisely estimate relationships to MetS. We found this risk to be even higher in Hispanics/Latinos, where movement-based measures consistently missed associations between MetS and sedentary patterns that were significant when using posture-based measures. This is particularly relevant when designing interventions for Hispanics/Latinos. Lassalle et al. argue that targeting reduction of sedentary behaviors may be more achievable than increasing physical activity, particularly in minority populations who may enjoy fewer resources and less access to physical activity promoting environments [50]. As we move toward the development of quantitative sedentary behavior guidelines [51], it will be essential to increase our understanding of movement- and posture-based associations with MetS outcomes with a focus on minority populations.
Application of the CHAP algorithm to accelerometer data to produce posture-based measures of sedentary patterns was a key strength of the study. Use of CHAP allows for reliable, validated, objective measures of posture-based sedentary behaviors in previously collected studies using hip accelerometry. A limitation of this study was that the Hispanic/Latino population was comprised of almost all individuals from Mexico or of Mexican heritage, thus is not representative of the more diverse Hispanic/Latino population in the US. Another limitation was modeling MetS as a dichotomous variable, which may be problematic because it does not consider the risk gradient based on the individual components. Further limitations include a cross-sectional study design, where causality relationships between sedentary patterns measures and MetS cannot be determined. The positive association between increased sedentary behavior and MetS has been established by other prospective studies, affirming our findings [52, 53]. The two-week accelerometer monitoring period may not capture all usual behavior patterns of individuals, although less than two-weeks of accelerometer data has been shown to produce stable estimates of group-level means of sedentary behaviors [54, 55]. Hip-worn accelerometers may not adequately capture resistance training (e.g., weight lifting) as would wrist-worn accelerometers [56], but resistance training is likely complimentary to and does not replace aerobic activity to lower risk of MetS [57]. Finally, the role of daily accelerometer wear time in this sample (mean = 14.4 h per day) may bias the associations between sedentary time and MetS towards the null, though we attempted to account for this by adjusting models for wear time. On days with less than 14 h of wear, each hour less of wear time was associated with a lower percentage of sedentary time captured [58, 59].
Conclusion
This study is an important contribution to a growing evidence base that not only is overall sedentary time a risk factor for MetS, but sedentary patterns play a role in MetS beyond MVPA and total sedentary time. The role of sedentary pattern measurement, using movement- or posture-based methods, impacted the strength and precision of measured associations. In stratified analyses we found that for Hispanics/Latinos posture-based measures were more sensitive to significant associations compared to movement-based measures. Further evidence investigating posture-based sedentary pattern associations with MetS in Hispanics/Latinos is needed.
References
Grundy SM, et al. Diagnosis and management of the metabolic syndrome. Circulation. 2005;112(17):2735–52.
Edwardson CL, et al. Association of Sedentary Behaviour with Metabolic Syndrome: A Meta-Analysis. PLoS ONE. 2012;7:e34916.
Amirfaiz S, Shahril MR. Objectively Measured Physical Activity, Sedentary Behavior, and Metabolic Syndrome in Adults: Systematic Review of Observational Evidence. Metab Syndr Relat Disord. 2019;17:1–21.
Gardiner PA, et al. Associations Between Television Viewing Time and Overall Sitting Time with the Metabolic Syndrome in Older Men and Women: The Australian Diabetes Obesity and Lifestyle Study. J Am Geriatr Soc. 2011;59:788–96.
Dempsey PC, et al. Associations of context-specific sitting time with markers of cardiometabolic risk in Australian adults. Int J Behav Nutr Phys Act. 2018;15:1–11.
Bellettiere J, et al. Associations of sitting accumulation patterns with cardio-metabolic risk biomarkers in Australian adults. PLoS ONE. 2017;12: e0180119.
Scheers T, Philippaerts R, Lefevre J. SenseWear-determined physical activity and sedentary behavior and metabolic syndrome. Med Sci Sports Exerc. 2013;45:481–9.
Tremblay MS, et al. Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:1–17.
Boerema ST, van Velsen L, Vollenbroek MMR, Hermens HJ. Pattern measures of sedentary behaviour in adults: a literature review. Digit Health. 2020;6.
Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 200306. Eur Heart J. 2011;32:590–7.
Healy GN, et al. Breaks in Sedentary TimeBeneficial associations with metabolic risk. Diabetes Care. 2008;31:661–6.
Henson J, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56:1012–20.
Bankoski A, et al. Sedentary Activity Associated With Metabolic Syndrome Independent of Physical Activity. Diabetes Care. 2011;34:497–503.
Carlson, J. A. et al. Day-level sedentary pattern estimates derived from hip-worn accelerometer cut-points in 8–12-year-olds: Do they reflect postural transitions? 37;(2019), 1899–1909 .https://doi.org/10.1080/02640414.2019.1605646
Bellettiere J, et al. Agreement of Sedentary Behavior Metrics Derived From Hip- and Thigh-Worn Accelerometers Among Older Adults: With Implications for Studying Physical and Cognitive Health. J Meas Phys Behav. 2021;4:79–88.
Barreira TV, Zderic TW, Schuna JM, Hamilton MT, Tudor-Locke C. Free-living activity counts-derived breaks in sedentary time: Are they real transitions from sitting to standing? Gait Posture. 2015;42:70–2.
van der Berg JD, et al. Associations of total amount and patterns of sedentary behaviour with type 2 diabetes and the metabolic syndrome: The Maastricht Study. Diabetologia. 2016;59:709–18.
Heiss G, et al. Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014;37:2391–9.
Umpierrez GE, Gonzalez A, Umpierrez D, Pimentel D. Diabetes Mellitus in the Hispanic/Latino Population: An Increasing Health Care Challenge in the United States. Am J Med Sci. 2007;334:274–82.
Schneiderman N, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37:2233–9.
Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the Metabolic Syndrome in the United States, 2003–2012. JAMA. 2015;313:1973–4.
Silfee V, Lemon S, Lora V, Rosal M. Sedentary Behavior and Cardiovascular Disease Risk Factors among Latino Adults. J Health Care Poor Underserved. 2017;28:798.
Qi Q, et al. Objectively measured sedentary time and cardiometabolic biomarkers in US Hispanic/Latino adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Circulation. 2015;132:1560–9.
Larsen BA, Martin L, Strong DR. Sedentary behavior and prevalent diabetes in Non-Latino Whites, Non-Latino Blacks and Latinos: findings from the National Health Interview Survey. J Public Health (Bangkok). 2015;37:634–40.
Moon JY, et al. Objectively Measured Physical Activity, Sedentary Behavior, and Genetic Predisposition to Obesity in U.S. Hispanics/Latinos: Results From the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes. 2017;66:3001–12.
Chang YJ, et al. Total sitting time and sitting pattern in postmenopausal women differ by hispanic ethnicity and are associated with cardiometabolic risk biomarkers. J Am Heart Assoc. 2020;9(4).
Diaz KM, et al. Prolonged, Uninterrupted Sedentary Behavior and Glycemic Biomarkers among US Hispanic/Latino Adults. Circulation. 2017;136:1362–73.
Xue X, et al. A new measure to quantify sedentary behavior using accelerometer data: Application to the Hispanic Community Health Study/Study of Latinos. Stat Methods Med Res. 2022;31:612–25.
Nakandala S et al. Application of Convolutional Neural Network Algorithms for Advancing Sedentary and Activity Bout Classification. J Measur Phys Behav 2;(2021) https://doi.org/10.1123/jmpb.2020-0016.
Greenwood-Hickman MA et al. The CNN Hip Accelerometer Posture (CHAP) method for classifying sitting patterns from hip accelerometers: a validation study. Med Sci Sports Exerc In Press, (2021)
Jankowska MM, et al. Protocol for a cross sectional study of cancer risk, environmental exposures and lifestyle behaviors in a diverse community sample: The Community of Mine study. BMC Public Health. 2019. https://doi.org/10.1186/s12889-019-6501-2.
Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43:357–64.
Matthews CE, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81.
Troiano RP, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8.
Bellettiere J, et al. CHAP-Adult: A Reliable and Valid Algorithm to Classify Sitting and Measure Sitting Patterns Using Data From Hip-Worn Accelerometers in Adults Aged 35+. J Meas Phys Behav. 2022;5:215–23.
ADALabUCSD/DeepPostures: Deep learning methods for identifying human postures from hip-worn accelerometer data. https://github.com/ADALabUCSD/DeepPostures. Accessed 11 Jan 2023.
Hibbing P. PBpatterns. 2022. Preprint at https://github.com/paulhibbing/PBpatterns. Accessed 25 Jan 2022.
Edwardson CL, et al. ActivPAL and ActiGraph Assessed Sedentary Behavior and Cardiometabolic Health Markers. Med Sci Sports Exerc. 2020;52:391–7.
Strasser B. Physical activity in obesity and metabolic syndrome. Ann N Y Acad Sci. 2013;1281:141–59.
Page A, Peeters G, Merom D. Adjustment for physical activity in studies of sedentary behaviour. Emerg Themes Epidemiol. 2015;12:1–4.
Serrano-Sánchez JA, et al. Domain and intensity of physical activity are associated with metabolic syndrome: A population-based study. PLoS ONE. 2019;14:e0219798.
Sisson SB, et al. Leisure time sedentary behavior, occupational/domestic physical activity, and metabolic syndrome in U.S. men and women. Metab Syndr Relat Disord. 2009;7:529–36.
Jefferis BJ, et al. Does duration of physical activity bouts matter for adiposity and metabolic syndrome? A cross-sectional study of older British men. Int J Behav Nutr Phys Act. 2016;13:1–11.
De la Cámara MA, et al. Associations of Mutually Exclusive Categories of Physical Activity and Sedentary Time With Metabolic Syndrome in Older Adults: An Isotemporal Substitution Approach. J Aging Phys Act. 2021;30:323–31.
Loh R, Stamatakis E, Folkerts D, Allgrove JE, Moir H J Effects of Interrupting Prolonged Sitting with Physical Activity Breaks on Blood Glucose, Insulin and Triacylglycerol Measures: A Systematic Review and Meta-analysis. Sports Med 2019 50:2 50, 295–330
Van Der Berg JD, et al. Replacement Effects of Sedentary Time on Metabolic Outcomes: The Maastricht Study. Med Sci Sports Exerc. 2017;49:1351–8.
Remie CME, et al. Sitting less elicits metabolic responses similar to exercise and enhances insulin sensitivity in postmenopausal women. Diabetologia. 2021;64:2817–28.
Duvivier BMFM, et al. Breaking sitting with light activities vs structured exercise: a randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia. 2017;60:490–8.
Wang X, et al. Objectively measured sedentary time and cardiovascular risk factor control in US Hispanics/Latinos with diabetes mellitus: results from the hispanic community health study/study of Latinos (HCHS/SOL). J Am Heart Assoc. 2017;6(6).
Lassalle PP, et al. Targeting sedentary behavior in minority populations as a feasible health strategy during and beyond COVID-19: on behalf of ACSM-EIM and HL-PIVOT. Transl J Am Coll Sports Med. 2021;6(4).
Stamatakis E, et al. Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. Br J Sports Med. 2019;53:377–82.
Greer AE, Sui X, Maslow AL, Greer BK, Blair SN. The Effects of Sedentary Behavior on Metabolic Syndrome Independent of Physical Activity and Cardiorespiratory Fitness. J Phys Act Health. 2015;12:68–73.
Honda T, et al. Sedentary bout durations and metabolic syndrome among working adults: A prospective cohort study. BMC Public Health. 2016;16:1–9.
Keadle SK, et al. Reproducibility of Accelerometer-Assessed Physical Activity and Sedentary Time. Am J Prev Med. 2017;52:541–8.
Wolff-Hughes DL, McClain JJ, Dodd KW, Berrigan D, Troiano RP. Number of accelerometer monitoring days needed for stable group-level estimates of activity. Physiol Meas. 2016;37:1447.
Stec MJ, Rawson ES. Estimation of resistance exercise energy expenditure using triaxial accelerometry. J Strength Cond Res. 2012;26:1413–22.
Liang M, Pan Y, Zhong T, Zeng Y, Cheng ASK. Effects of aerobic, resistance, and combined exercise on metabolic syndrome parameters and cardiovascular risk factors: a systematic review and network meta-analysis. Rev Cardiovasc Med. 2021;22:1523–33.
Herrmann SD, Barreira TV, Kang M, Ainsworth BE. How Many Hours Are Enough? Accelerometer Wear Time May Provide Bias in Daily Activity Estimates. J Phys Act Health. 2013;10:742–9.
Herrmann SD, Barreira TV, Kang M, Ainsworth BE. Impact of accelerometer wear time on physical activity data: a NHANES semisimulation data approach. Br J Sports Med. 2014;48:278–82.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. The Community of Mine study was supported by a National Institutes of Health grant, National Cancer Institute R01CA179977. This research was supported by NIH National Institute of Diabetes and Digestive and Kidney Diseases R01DK114945 and by the Population Facing Research Shared Resource of the City of Hope Cancer Center (National Cancer Institute Cancer Center Support Grant P30CA033572).
Author information
Authors and Affiliations
Contributions
Marta M. Jankowska: Conceptualization, Methodology, Data Curation, Writing, Review and Editing, Supervision. Calvin P. Tribby: Methodology, Software, Formal Analysis, Writing, Review and Editing, Visualization. Paul R. Hibbing: Conceptualization, Methodology, Software, Review and Editing. Jordan Carlson: Conceptualization, Methodology, Review and Editing. Mikael Anne Greenwood-Hickman: Conceptualization, Methodology, Review and Editing. Dorothy D. Sears: Conceptualization, Methodology, Investigation, Resources, Funding acquisition, Review and Editing. Andrea Z. LaCroix: Conceptualization, Methodology, Funding acquisition, Supervision, Review and Editing. Loki Natarajan: Conceptualization, Methodology, Resources, Funding acquisition, Supervision, Review and Editing.
Corresponding author
Ethics declarations
Ethics Approval
Ethics approval was obtained from the University of California San Diego Institutional Review Board (protocol #140510).
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Consent to Participate
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jankowska, M.M., Tribby, C.P., Hibbing, P.R. et al. Movement- and Posture-based Measures of Sedentary Patterns and Associations with Metabolic Syndrome in Hispanic/Latino and non-Hispanic Adults. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02114-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-02114-w