Abstract
Background
Racialized communities, including Black Canadians, have disproportionately higher COVID-19 cases. We examined the extent to which SARS-CoV-2 infection has affected the Black Canadian community and the factors associated with the infection.
Methods
We conducted a cross-sectional survey in an area of Ontario (northwest Toronto/Peel Region) with a high proportion of Black residents along with 2 areas that have lower proportions of Black residents (Oakville and London, Ontario). SARS-CoV-2 IgG antibodies were determined using the EUROIMMUN assay. The study was conducted between August 15, 2020, and December 15, 2020.
Results
Among 387 evaluable subjects, the majority, 273 (70.5%), were enrolled from northwest Toronto and adjoining suburban areas of Peel, Ontario. The seropositivity values for Oakville and London were comparable (3.3% (2/60; 95% CI 0.4–11.5) and 3.9% (2/51; 95% CI 0.5–13.5), respectively). Relative to these areas, the seropositivity was higher for the northwest Toronto/Peel area at 12.1% (33/273), relative risk (RR) 3.35 (1.22–9.25). Persons 19 years of age or less had the highest seropositivity (10/50; 20.0%, 95% CI 10.3–33.7%), RR 2.27 (1.23–3.59). There was a trend for an interaction effect between race and location of residence as this relates to the relative risk of seropositivity.
Interpretation
During the early phases of the pandemic, the seropositivity within a COVID-19 high-prevalence zone was threefold greater than lower prevalence areas of Ontario. Black individuals were among those with the highest seroprevalence of SARS-CoV-2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and the illness that results (COVID-19) have resulted in a pandemic with profound consequences [1]. COVID-19 cases have been disproportionately concentrated within racialized communities. Among these groups, Black people have been profoundly affected in the UK, the USA and Canada [2,3,4].
COVID-19 cases are typically diagnosed by polymerase chain reaction (PCR) testing that is performed on nasopharyngeal swabs [5,6,7], and PCR testing protocols have largely been conducted only in those with symptoms of COVID-19. Given the significant rates of asymptomatic infections, PCR testing likely underestimates the prevalence of infection within communities, unless widespread testing of symptomatic and asymptomatic person is done. Serologic testing enables a more complete assessment of the extent to which SARS-CoV-2 infection and associated outcomes have affected communities [8, 9]. Furthermore, this enables risk factors that are associated with infection to be elucidated, including the presence of medical comorbidities and social determinants of health, including those that define material deprivation indices [10].
This study examined the use of serologic testing for SARS-CoV-2 infection in a community-based sample from Ontario, Canada, to determine the full extent to which SARS-CoV-2 has penetrated into the Black community, which cannot be captured by current PCR testing protocols. One of our goals was to establish feasibility of enrolling large number of Black Canadians, a population that has had a long history of mistrust of the health care system. We sought to determine the extent of community participation and the seroprevalence of SARS-CoV-2 antibodies in the study population. We compared the seropositivity rates among persons in lower socioeconomic settings with a large proportion of Black residents compared with more affluent settings with lower percentages of Black residents. We also examined risk factors that are associated with seropositivity for SARS-CoV-2 infection, including but not limited to the presence of medical comorbidities and the markers of the social determinants of health [11].
Our study was a prelude to a more extensive study of the seroprevalence of SARS-CoV-2 among Canadian communities with the largest proportions of Black residents. A goal was to get a truer sense of the actual prevalence of COVID-19 infection in these communities, in contrast to relying solely on PCR test results from symptomatic patients, prior to the start of COVID-19 vaccination campaigns. Furthermore, the study was intended to provide valuable data from the Black community, a group that is often not well represented in research projects, including community-based projects.
Methods
Study Design
We conducted a prospective cross-sectional study from August 15, 2020, to December 15, 2020, with a planned follow-up phase of up to 18 months after enrollment. The first phase of COVID-19 vaccination started on December 15, 2020 [12]. Thus, persons in this study would not have received vaccines at the time of blood sampling. In this report, we have addressed the cross-sectional component of the study.
Study Setting
We conducted a community-based study in three regions of Ontario during a period prior to the start of the provincial COVID-19 vaccination efforts. The primary area of focus had a higher proportion of Black residents than most areas of Canada. In Toronto, this was an area that had a higher proportion of Black residents (> 15–30%) compared to the provincial proportion for the province of Ontario, Canada (4.7%) [13]. Thus, we focused on the northwest quadrant of the Greater Toronto Area (GTA) and nearby suburban area of Peel, Ontario. We also aimed to enroll participants from areas that covered a spectrum of the socioeconomic levels across the province given that socioeconomic status might be associated with the likelihood of exposure to SARS-CoV-2. Thus, additional regions of focus included the suburban city of Oakville, Ontario, and London, Ontario. These areas have predominantly White residents in contrast to the northwest quadrant of the GTA. The northwest quadrant of the GTA and Peel are known to be COVID-19 hot spots (high case counts) based on the COVID-19 cases reported, whereas Oakville and London, Ontario, are regarded as lower incidence areas.
Northwest quadrant of the Greater Toronto Area and Peel Region: The northwest quadrant of the Greater Toronto Area is an expansive region in southern Ontario, Canada. The northwest quadrant lies to the north of the Toronto city centre, a major economic and cultural hub. It is situated to the east of Hamilton, a city known for its industrial and waterfront districts. Within the northwest quadrant, the area where the study was focussed has 29% Black residents. Adjoining this area is the suburban area of Peel Region with 15.3 Black residents [14]. The median household income of the northwest quadrant of the GTA is Can $66,000 [15].
Oakville, Ontario, is a suburban town located to the southwest of Toronto along the shores of Lake Ontario. It is recognized for its picturesque waterfront and affluence relative to neighbouring communities. The median household income is Can $128,000, which is well above the Ontario provincial figure of $91,000 [16, 17]. It is positioned to the south of Toronto, east of Hamilton, Ontario. The proportion of Black residents in this area is 2.9% [16].
London, Ontario, is a city in southwestern Ontario, known for its educational institutions. It is located to the west of Toronto and approximately 120 miles northwest of Niagara Falls, which is on the border of Ontario and New York State. The proportion of Black residents in London is 3.5% [18]. The median household income is Can $76,500 [18].
Study Population and Sample
Participants consisted of Black Canadians and non-Black Canadians (White, South Asian, East Asian, Middle East, Hispanic, Other) residing in the areas where the study was conducted. We recruited participants using different promotional approaches that included social media, a study website, conventional media (radio interviews) and promotion using flyers and information sheets that were distributed to potential participants within the communities. Flyers were distributed at community social events, churches and health centres. The promotional material encouraged the participation of Black Canadians to obtain enough of these participants for meaningful analyses and generalizability. Persons were eligible for inclusion if they were greater than 2 years of age. We excluded persons who had symptomatic COVID-19 at the time of enrollment to ensure the safety of the research team. Participants were invited to participate at the study enrollment sites and written informed consent was obtained. In addition, we obtained assent for age-appropriate children. Participants received gift certificates as approved by the Research Ethics Board and no financial compensation was provided.
Study Procedure
Participants were administered a questionnaire that included items relating to clinical, epidemiologic, demographic and socioeconomic variables. Clinical data included age, gender, chronic medical conditions and medications that could potentially affect the immune responses to SARS-CoV-2. Epidemiologic, socio-economic, demographic data and ethno-racial information were collected. The race/ethnicity categories used were adapted from those used by Statistic Canada [19]. Types of occupation were categorized as frontline versus non-frontline, where the former include but are not limited to persons working as teachers, health care workers, protective service workers (e.g. police, fire, and emergency medical services), personal support workers, taxi drivers and cashiers. Each participant provided a 10-cc venous blood sample which was stored at 4°C followed by processing within 7 days. Separated sera were stored at −20°C or colder prior to the performance of the immunoassay.
We established a community advisory group (CAG) to facilitate community engagement [20]. The group included members from a cross-section of the Black Canadian community primarily and included non-Black Canadians working or living within the Black community. Regular meetings were held between the research team and the CAG who were all unpaid volunteers. Besides the CAG, the research team worked closely with leaders from the communities where enrollment occurred.
Primary Outcome Measurement
Testing was performed at the Hospital for Sick Children, Toronto. SARS-CoV-2 IgG antibodies were determined using the EUROIMMUN assay which is a Health Canada-approved enzyme-linked immunoassay (EUROMMUN, Lubeck, Germany) [21]. This is a semi-quantitative assay that targets recombinant S1 protein of SARS-CoV-2. The interpretation of results was based on the signal to cutoff ratios of < 0.8 being reported as negative, ≥ 0.8 to < 1.1 as borderline and ≥ 1.1 as positive [21]. The sensitivity of the assay is reported to be 94.4% with a specificity of 99.6% among persons who are > 10 days after the onset of symptoms [21].
Research Ethics
Research Ethics approval was obtained from Clinical Trials Ontario (CTO; Project ID CTO 3274), the Hospital for Sick Children (3274-CIA-Aug/2020-42457) and the London Health Sciences Centre (reference 3274-CIA-Nov/2020-45486).
Statistical Analyses
We estimated that a sample size of 300 participants would produce greater than a 95% confidence interval equal to the sample proportion plus or minus 0.02 when the estimated seropositivity proportion is 0.03. Data were descriptively summarized, and proportions compared using chi-square of Fisher’s exact test, as appropriate. Seropositivity estimates were expressed as proportions with 95% confidence interval (Binomial exact estimates). Continuous variables were compared using Student’s T test or a non-parametric procedure, as appropriate. Risk ratios (relative risk) were determined for different SARS-CoV-2 exposure categories. The relationship between seropositivity and different variables is examined using univariate analyses and a multiple logistic regression approach including the interaction between variables such as race and location of residence. For the multivariable analyses, we included variables that were primarily aligned with our main objectives (location of residence and race) and others achieving the lowest P values on univariate analyses. 95% confidence intervals were provided where appropriate. There were very few missing data (1%) and we proceeded with analysis as if we had a complete dataset.
Results
Descriptive Characteristics (Table 1)
We recruited 388 participants from across the study sites; however, one participant withdrew from the study without providing a reason. Most of the participants we enrolled were from the northwest quadrant of the Greater Toronto Area and adjoining areas of Peel Ontario, where 70.5% (273/387) participants were enrolled. The proportions of participants enrolled from Oakville and London were 15.5% (60/387) and 13.2% (51/387)), respectively. Most participants were at or above the age of 19 years (87.1%), with 57.9% in the 31–65 years age group. Participants less than 19 years accounted for 12.9% of enrollees. The breakdown according to race indicated that we were successful in recruiting Black Canadians: Black Canadians 65.9% (255/387), non-Black Canadian 33.9% (131/387; race/ethnicity unknown for 1 participant) and among non-Black persons, those identifying as White accounted for 15.3% (59/387), representing the second largest racial group of participants enrolled.
Table 2 shows a comparison between the study population and general population groups in three areas of Ontario, Canada. We had deliberately focused on enhancing participation of Black Canadians. The study group had proportionately more women relative to men compared with the general population. The study population had a median age of 45 years compared with the three general population groups with median ages of 38, 39.5 and 41.6 years, respectively.
To examine the extent to which participants might have been motivated to enter our study to determine their antibody status following previous COVID-19 infection, we evaluated a subset of participants. Thus, among a subset of participants for whom there were complete data on COVID-19 exposures and diagnosis, 14.2% (27/190) indicated that they felt that they had COVID-19 respiratory symptoms prior to serological testing. Among these persons, 4.2% (8/190) tested positive for COVID-19 antibodies. From among 150 subjects who provided complete data on prior PCR testing, two participants who were previously PCR-positive for COVID-19 were also seropositive in our study.
Seropositivity
Table 3 shows that the seropositivity for the overall study population was 9.6% (95% CI 7.1–13.3). Seropositivity values for London and Oakville were comparable (3.9% (2/51; 95% CI 0.5–13.5) and 3.3% (2/60; 95% CI 0.4–11.5), respectively). Using, the Oakville/London estimate as the reference, the seropositivity for the GTA northwest region was 3.5-fold greater (RR 3.5, 95% CI 1.3–9.8), seropositivity 12.3% (95% CI 8.1–17.6). Black persons in the Northwest quadrant of Toronto had a seropositivity of 14.4% (95% CI 9.4–19.5). The seropositivity rate for Black participants residing in London/Oakville was 1.5% (95% CI 0.04–8.0). Among 59 participants who identified as White (50.9% of whom resided in Oakville/London), the seropositivity was 3.4% (95% CI 0.41–11.7). As shown in Table 3, the highest seropositivity values were observed in the < 19 years age group 22.0% (95% CI 11.5–36.0). Pairwise comparisons showed a statistically significant difference between the seropositivity among the latter age group compared with the 31–65 years age groups (P < 0.01) with no significant difference when compared with the 19–30 age group P = .09).
Factors Associated with Seropositivity
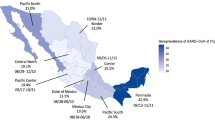
We found that three postal code neighbourhoods in Toronto and Peel accounted from greater than 50% of all seropositive cases (M3N, L6A and L4T) and were the areas with > 10% of participants being seropositive. Univariate analysis indicated that being a resident of the GTA/Peel area was more than three times likely to as associated with seropositivity when compared with residence in London/Oakville (RR 3.43 (95% CI 1.30–8.03). Using White as the reference, there was a statistical trend for Black persons to be more likely to be seropositive compared with White persons (RR 3.24 95% CI 0.79–13.22; P = .07); similar estimates for the other groups were as follows: South Asian RR 4.4 (95% CI .80–24.6; P = 0.1); East Asian 3.5 (.53–22.84; P = .21); and Hispanics 2.46 (.37–16.46; P = .58). The seropositivity estimates among Black versus South Asian, East Asian and Hispanics were not statistically significantly different. Being a frontline worker compared to a non-frontline worker was associated with a greater risk of seropositivity (RR 2.69 (95% CI 1.0–7.23), P = 0.04. There were no significant differences in seropositivity among males versus females; RR 1.08 (95% CI 0.58–2.01), P = 0.82, while having a link with schools (teachers or students) showed a trend to be associated with seropositivity RR 1.85 (95% CI 0.96–3.57), P = 0.06.
Multivariable Model
Table 4 shows univariate analyses and variables that were included in multivariable analyses. We examined the association between seropositivity and age, race and location of residence and the interaction between race and location of residence (model 1) and age, race and location of residence (model 2). Persons < 19 years were 2.5 times more likely to be seropositive compared with their older counterparts, RR 2.5 (95% CI 1.26–4.78). Residence in the GTA/Peel area was associated with a greater risk of seropositivity, RR 3.5 (95% CI 1.26–9.53). With respect to the interaction between race and location of residence, for Black Canadians compared with non-Black, the adjusted RR for seropositivity for residence in the GTA/Peel region was 1.70 (95% CI 0.72–4.04), and in contrast for the Oakville/London location, the RR was 0.17 (95% CI 0.02-1.59); therefore, the RR increased approximately tenfold for Black participants residing in the GTA/Peel Region; however, this increase was not statistically significant (P = 0.06; RR = 9.75 (CI 9.3 to 105.25).
Discussion
In the USA, during the early phases of the pandemic, SARS-CoV-2 seroprevalence varied across states between 5 and 25% [22,23,24]. In Canada, the seroprevalence for the general population was estimated to be less than 5% based on data derived from blood donors [25]. Data are limited on the SARS-CoV-2 seroprevalence for Black communities in North America. Our report provides insight into such estimates in Ontario, Canada, during the second wave of COVID-19. Overall, the results show that the seroprevalence detected among persons in a COVID-19 hot zone was several times greater than estimates derived from blood donors across Canada [25]. This confirms that certain communities were been disproportionately affected by the virus.
This study directs its primary focus towards the Black community within a North American context, acknowledging the alarming disparities in the impact of COVID-19. However, it is essential to underscore that this focus on the Black community does not diminish the recognition that other racialized groups have also experienced significant disparities in the face of the pandemic. For instance, research has shown that Hispanic populations in the USA also faced higher rates of COVID-19 infection and hospitalization compared to non-Hispanic white populations [26,27,28]. Additionally, Indigenous communities have experienced disproportionate impacts, including but not limited to the challenges related to unmet health needs [29]. Furthermore, South Asian communities in Ontario have encountered notable disparities, as evidenced by research illustrating heightened vulnerability and infection rates within this demographic [30].
Among White participants, the seroprevalence was < 4%, with a tendency for a higher rate among Black Canadians (11%). Seropositivity among Black persons was not statistically different from those among South Asian, East Asians and Hispanics, although it should be noted that the confidence intervals for the seropositivity rates among latter groups were wide due to the smaller sample sizes of these subgroups. The study acknowledges the smaller sample sizes of other groups, such as South Asians, East Asians and Hispanics and recognizes the need for further research to understand the seroprevalence rates among these subgroups. Additionally, by addressing the specific concerns and experiences of the Black community, the study can contribute to broader discussions on health disparities and equity that may benefit all populations.
Importantly, the seroprevalence rates detected in our study align with published information on the median household incomes of the communities studied [14,15,16]. This is consistent with the reported cases of COVID-19 based on income categories in Toronto, where individuals in lower-income categories were disproportionately affected by the virus compared to households with higher annual incomes [4]. These findings highlight the inequities in the impact of COVID-19 on different socioeconomic groups [4].
Our results suggest that persons less than 19 years of age were among those most likely to be seropositive. There is potential for younger individuals living in lower socioeconomic areas to contribute to the spread of COVID-19 in settings such as multigenerational homes. Higher seropositivity among persons less than 19 years has implications on strategies aimed at reducing the risk of COVID-19 among persons in school environments, including ways to enhance access to COVID-19 vaccines coupled with specially targeted educational measures, particularly within COVID-19 high-prevalence areas.
An accomplishment of the study is the successful enrollment of participants from the communities studied. Particularly within the Black community, there is often reluctance to participate in research studies due to various reasons, such as historical mistreatment and mistrust. However, the Community Advisory Group (CAG) recognized the importance of community engagement and trust building in overcoming these barriers. Through targeted outreach efforts and community partnerships, the study was able to establish a sense of trust and rapport with the Black community. This was crucial in encouraging individuals to participate and contribute to the study. The involvement of the CAG, which consisted of community leaders and representatives, played a vital role in bridging the gap between the researchers and the community. This facilitated oversampling of Black participants with proportionately more Black persons enrolled compared with the general population, as our results have indicated.
The successful enrollment from the communities studied not only allowed for a relatively high proportion of Black participants, but also ensured that the study findings were more relevant and meaningful to these communities. It also laid the foundation for future research collaborations and community-based interventions aimed at addressing health disparities and promoting health equity.
Limitations
This report is limited because of the use of a convenience sample. It is likely that our ability to show differences between some ethno-racial groups was limited by the sample size. Some participants could have been exposed but had not yet seroconverted at the point of blood sampling. However, the effect of this potential bias would be to underestimate the rates of infection in the groups studied. It is possible that some persons who participated were more motivated to do so because of concerns regarding previous exposure to COVID-19. However, as shown in the results, this bias was likely present in about 14% of the study population. We did not examine some variables that might be of relevance, including but not limited to household density. The study covered a period of approximately 4 months during year 1 of the pandemic and the second wave of COVID-19; therefore, no conclusions can be drawn about subsequent waves of COVID-19.
One issue is the extent to which seroprevalence data might inform progress toward optimal community immunity [31,32,33,34]. It is possible that communities with higher levels of seropositivity (e.g. hot zones) could achieve herd immunity at lower levels of vaccine coverage than what is required in COVID-19 low incidence areas. This might be of relevance in some racialized communities with low vaccine uptake, where a lower percentage of vaccine coverage coupled with higher background seropositivity rates might be sufficient to achieve a high level of community immunity. This observation is not intended to inform policy, but rather to acknowledge the potential beneficial role of the combination of immunity from SARS-CoV-2 infection and vaccination [35].
Conclusion
We have provided insights into the seroprevalence of SARS-CoV-2 infection among persons, including Black Canadians residing in COVID-19 high-prevalence zones in Ontario. This study examined the feasibility of a more extensive enrollment strategy within the Black community, while simultaneously providing insight into SARS-CoV-2 seroprevalence within a COVID-19 high-prevalence zone in Ontario. Overall, the study’s achievement in enrolling participants from the Black community demonstrates the feasibility of overcoming research participation barriers through community engagement and trust building. It serves as a stepping stone for future studies to continue fostering community partnerships and inclusivity in research. The sample size represents the largest report of SARS-CoV-2 seroprevalence among Black Canadians and one of few such reports in North America. We observed a tendency of greater seropositivity among individuals less than 19 years of age. There appears to be a tendency for Black Canadians who resided in a lower socioeconomic region (the northwest region of the Greater Toronto Area and Peel area) to more likely to be seropositive when compared with their White Canadian counterparts.
Data Availability
The data and material are not available to the public.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China. NEJM. 2020;382(8):727–33. https://doi.org/10.1056/NEJMoa2001017.
Centers for Disease Control and Prevention. COVID data tracker: trends in cases and deaths by race/ethnicity, age, sex. [Internet]. Atlanta, GA: US Department of Health and Human Services. Available from: https://covid.cdc.gov/covid-data-tracker/#demographicsovertime. Accessed 25 Apr 2021.
Public Health England. Disparities in the risk and outcomes of COVID-19 [Internet]. London UK: Wellington House. 2020. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf. Accessed 26 Apr 2021.
City of Toronto. COVID19: ethno-racial identity & income. [Internet]. Toronto Canada: Available from: https://www.toronto.ca/community-people/health-wellness-care/health-programs-advice/respiratory-viruses/covid-19/covid-19-pandemic-data/covid-19-archived-dashboards/covid-19-ethno-racial-identity-income/.
LeBlanc JJ, Gubbay JB, Li Y, Needle R, Arneson SR, Marcino D, et al. Real-time PCR-based SARS-CoV-2 detection in Canadian Laboratories. J Clin Virol. 2020;128:104433. https://doi.org/10.1016/j.jcv.2020.104433.
World Health Organization (WHO). Laboratory testing for 2019 novel coronavirus (2019 nCoV) in suspected human cases. [Internet]. 2020. Available from: https://www.who.int/publications/i/item/10665-331501.
Chan JF, Yip CC, Toss KK, Tang TH, Wong SC, Leung K, et al. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol. 2020;58(5):e00310–20. https://doi.org/10.1128/JCM.00310-20.
Doi A, Iwata K, Kuroda H, Hasuike T, Nasu S, Kanda A, et al. Seroprevalence of novel coronavirus disease (COVID-19) in Kobe, Japan: A cross-sectional study. Clin Epidemiol Glob Health. 2021;11:100747. https://doi.org/10.1016/j.cegh.2021.100747.
Ward H, Cooke G, Whitaker M, Redd R, Eales O, Brown JC, et al. React-2 round 5: Increasing prevalence of SARS-CoV-2 antibodies demonstrate impact of the second wave and of vaccine roll-out in England. https://doi.org/10.1101/2021.02.26.21252512.
Public Health Ontario. COVID-19 in Ontario: a focus on neighbourhood material deprivation, February 26, 2020 to December 13, 2021. Toronto, ON: Queen’s Printer for Ontario, 2022. Available from: https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/06/covid-19-epi-material-deprivation.pdf?la=en.
Government of Canada. COVID-19 epidemiology update: key updates. [Internet]. Available from: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html.
https://news.ontario.ca/en/release/59607/ontario-begins-rollout-of-covid-19-vaccine.
https://www150.statcan.gc.ca/n1/pub/89-657-x/89-657-x2019002-eng.htm.
https://www.areavibes.com/toronto-on/jane+and+finch/employment/.
https://www150.statcan.gc.ca/n1/pub/12-581-x/2022001/sec3-eng.htm.
The Hospital for Sick Children. The seroMARK project: understanding COVID-19 immunity among Black Canadians. http://immunityseromark.ca/.
EUROIMMUN Medizinische Labordiagnostika AG. SARS-CoV-2 ELISA test systems from EUROIMMUE. Luebeck, Germany. Available from https://www.coronavirus-diagnostics.com/antibody-detection-tests-for-covid-19.html. Accessed 2020 April 23.
Bajema KL, Wiegand RE, Cuffe K, Patel SV, Iachan R, Lim T, et al. Estimated SARS-CoV-2 seroprevalence in the US as of September 2020. JAMA Intern Med. 2021;181(4):450–60. https://doi.org/10.1001/jamainternmed.2020.7976.
COVID-19 Immunity Task Force. Seroprevalence in Canada.[Internet] Available from: https://www.covid19immunitytaskforce.ca/seroprevalence-in-canada/.
Ng DL, Goldgof GM, Shy BR, Levine AG, Balcerek J, Bapat SP, et al. SARS-CoV-2 seroprevalence and neutralizing activity in donor and patient blood. Nat Commun. 2020;11(1):4698. https://doi.org/10.1038/s41467-020-18468-8.
Saeed S, Drews SJ, Pambrun C, Yi Q, Osmond L, O’Brien SF. SARS-CoV-2 seroprevalence among blood donors after the first COVID-19 wave in Canada. Transfusion. 2021;61(3):862–72.
Am C, Garg S, Pham H, et al. Racial and ethnic disparities in rates of COVID-19–associated hospitalization, intensive care unit admission, and in-hospital death in the United States from March 2020 to February 2021. JAMA Netw Open. 2021;4(10):e2130479.
Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: a systemic review. Ann Intern Med. 2021;174(3):362–73. https://doi.org/10.7326/M20-6306. Epub 2020 Dec 1
Magesh S, John D, Li WT, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status. A systematic review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147. https://doi.org/10.1001/jamanetworkopen.2021.34147.
Hahmann T, Kumar MD. COVID-19: data to insights for a better Canada - unmet health care needs during the pandemic and resulting impacts among First Nations people living off reserve, Métis and Inuit. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2022001/article/00008-eng.htm.
Anand SS, Arnold C, Bangdiwala SI, et al. Seropositivity and risk factors for SARS-CoV-2 infection in a South Asian community in Ontario: a cross-sectional analysis of a prospective cohort study. CMAJ Open. 2022. https://doi.org/10.9778/cmajo.20220031.
Randolph HE, Barreiro LB. Herd immunity: understanding COVID-19. Immunity. 2020;52(5):737–41. https://doi.org/10.1016/j.immuni.2020.04.012.
Kwok KO, Lai F, Wei WI, Wong SYS, Tang JWT. Herd immunity – estimating the level required to halt the COVID-19 epidemics in affected countries. J Inf Secur. 2020;80(6):e32–3. https://doi.org/10.1016/j.jinf.2020.03.027.
Dong M, He F, Deng Y. How to understand herd immunity in the context of COVID-19. Viral Immunol. 2021;34(3):174–81. https://doi.org/10.1089/vim.2020.0195.
Kadkhoda K. Herd Immunity to COVID-19. Am J Clin Pathol. 2021;155(4):471–2. https://doi.org/10.1093/ajcp/aqaa27.
Jones J. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2023-06-21-23/03-COVID-Jones-508.pdf.
Acknowledgements
Biostatistician: Mr. Derek Stephens
We appreciate the contributions by the participants. The seroMARK team is supported by a Community Advisory Group, as follows: Dr. Pamela Appelt (chair), Oakville, Ontario; Dr. Mark Awuku, Windsor, Ontario; Mr. Paul Bailey, Toronto, Ontario; Dr. Janet Collins, London, Ontario; Mr. Liben Gebremikael, Toronto, Ontario; Ms. Jenny Gumb, Toronto, Ontario; Mr. Tesfai Mengesha, Toronto, Ontario; Ms. Adaoma Patterson, Toronto, Ontario; Dr. Cheryl Prescod, Toronto, Ontario; Ms. Noelle Richardson, Toronto, Ontario; Dr. Sylvanus Thompson, Toronto, Ontario; Ms. Nicole Welch, Toronto, Ontario.
Code Availability
Not applicable.
Funding
The Hospital for Sick Children Foundation; University of Toronto COVID-19 Action Initiative and the Office of Equity Diversity and Inclusion, Faculty of Medicine, University of Toronto; the COVID-19 Immunity Task Force, Canada
Author information
Authors and Affiliations
Consortia
Contributions
UA conceptualized and designed the study with contributions from MB, JU, AB, CJ, NK and PW. MA performed analyses. J-PJ, AC and JG provided key interpretation of the laboratory results. All authors contributed to the addressing of revisions and have approved of the final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics Approval
Research Ethics approval was obtained from Clinical Trials Ontario, the Hospital for Sick Children, and the London Health Sciences Centre.
Consent to Participate
Informed consent was obtained from participants.
Consent for Publication
Participants were aware that the results of the study would be prepared for publication. All authors approved the final version of the manuscript for publication.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Michelle Barton, Julia Upton, Annette Bailey and Aaron Campigotto share joint second authorship.
Mariana Abdulnoor, Jean-Philippe Julien, Jonathan Gubbay, Niranjan Kissoon, Alice Litosh, Maria-Rosa La Neve and Peter Wong share joint third authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Allen, U.D., Barton, M., Upton, J. et al. Disproportionate Rates of COVID-19 Among Black Canadian Communities: Lessons from a Cross-Sectional Study in the First Year of the Pandemic. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-023-01903-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01903-z