Abstract
Purpose
This study aimed to examine the impact of the COVID-19 lockdown on social determinants of health (SDOH) among Blacks with HIV and a comorbid diagnosis of hypertension or type 2 diabetes mellitus (T2DM).
Methods
This was a longitudinal survey study. The inclusion criteria were adults ≥ 18 years and the presence of hypertension and/or diabetes, along with a positive HIV diagnosis. This study enrolled patients in the HIV clinics and chain specialty pharmacies in the Dallas-Fort Worth (DFW) area. A survey of ten questions examining SDOH was conducted before, during, and after the lockdown. A proportional odds mixed effects logistic regression model was applied to assess differences between time points.
Results
A total of 27 participants were included. Respondents felt significantly safer in their living place post-lockdown than in the pre-lockdown period (odds ratio = 6.39, 95% CI [1.08–37.73]). No other statistically significant differences in the responses were found over the study timeframe. However, borderline p values indicated better SDOH status post-lockdown as compared to pre-lockdown.
Conclusion
Study participants feel safer one year after lockdown compared to pre-lockdown. The CARES Act and the moratorium on rent and mortgage are among the factors that may explain this increase. Future research should include designing and evaluating interventions for social equity enhancement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Black populations are disproportionately affected by chronic diseases, including human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS), hypertension (HTN), and type 2 diabetes mellitus (T2DM). More than 1.1 million people in the US live with HIV/AIDS; among these, 476,100 are Blacks [1, 2]. In 2018, 42% (16,002) of the 37,968 new HIV diagnoses in the US were among Blacks, while they are only 14.2% of the population living in the US [3].
The prevalence of diagnosed diabetes was 8.7% of the US population in 2019, 12.1% among Blacks, compared to approximately 9.5%, 11.8%, 14.5%, and 7.4% among Asians, Hispanics, American Indians, and Whites, respectively [4]. Similarly, 116 million, or almost half of the US population, have HTN. A higher prevalence is seen among historically oppressed race/ethnic groups. HTN is more prevalent in non-Hispanic Black adults (56%) than in non-Hispanic White adults (48%), non-Hispanic Asian adults (46%), or Hispanic adults (39%) [5]. A systematic review of chronic diseases among African Americans found that multiple simultaneous components of health affect African American families. In this study, outcomes related to chronic diseases such as HTN, DM, depression, psychosocial outcomes, and health behaviors were examined [6].
The cause for the health disparities is varied and complex but generally intersects systemic barriers such as economic instability, lack of healthcare access, structural racism, and discrimination [7]. These factors, termed social determinants of health (SDOH), are the primary drivers for health inequity [8]. One of the key elements of SDOH is safe housing, transportation, and neighborhoods [9]. Safety is a basic need and an influential human right, which directly and indirectly affects psychological and physical health [9, 10]. It is defined as protection from physical, social, or emotional harm and is considered a complex concept that various environmental factors and risk management abilities can impact [11].
The coronavirus disease 2019 (COVID-19) pandemic has further strained the healthcare system and exacerbated the burden of chronic diseases. The impact of COVID-19 has been harmful to all individuals; however, it poses an increased risk for individuals with chronic health conditions such as cardiovascular disease, T2DM, obesity, and HIV [12]. Research has shown disparities in COVID-19 outcomes among historically oppressed racial and ethnic populations compared to other groups [13]. A meta-analysis of 68 studies representing over 43 million patients in the United States showed that COVID-19 positivity and severity were higher among African Americans than their White counterparts. Additionally, a positive association between the percentage of the uninsured population and COVID-19 positivity was seen among African Americans [14].
A limited number of studies have examined the effects of non-pharmaceutical interventions (NPIs) such as lockdowns, shelter-in-place orders, and other government-mandated restrictions that limit people’s freedom of movement and activities on COVID-19 mortality. The controversial results of a systematic review concluded that lockdowns failed to affect COVID-19 mortality significantly yet imposed immense economic and social costs [15]. Critics of this paper argue that the conclusions drawn are highly flawed, given the vague characterization of inconclusive efficacy measures for NPIs [16]. These studies set the foundation for our research into how Blacks with chronic diseases were faring regarding the impact of the COVID-19 lockdown on their SDOH. On the other hand, the CARES Act was a stimulus bill passed by the US Congress in response to the economic consequence of the COVID-19 pandemic in the US. Associations between mental health and CARES availability are controversial in different studies [17, 18].
Studies have attempted to characterize the impact of COVID-19 on Black communities. These studies often did not consider individual differences in the severity and positivity of COVID-19 and were conducted at the ecological level; therefore, potential confounders can threaten their validity [19,20,21]. Our study is uniquely positioned to examine the impact of the lockdown on a particularly vulnerable segment of this community in a longitudinal design at the individual level. Keeping on the same page with Health People 2030 goals related to SDOH, our objectives add to upstream efforts to improve health and reduce disparities [22].
Methods
Study Design and Sample
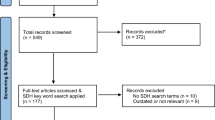
We employed a longitudinal survey as a part of an ongoing clinical trial (NCT03437694). The larger trial aims to assess the impact of medical record-based medication therapy management (MTM) on HIV-related health outcomes. Participants enrolled in the clinical trial were administered a survey and then interviewed. Following this, they received pharmacist-provided MTM services including, but not limited to, prioritization of medication lists, creation of action plans, discussion, and collaboration with a patient and medical provider if applicable, and recommendations for follow-up. The selection criteria for study participation were self-identification as Black, 18 years of age or older, diagnosed with HIV, and had HTN, T2DM, or both as comorbid conditions, as verified by their medical records.
A convenient sample of HIV clinic-recruited participants through multiple recruitment methods in Dallas-Fort Worth (DFW) area was obtained. Once enrolled in the study, participants were scheduled to meet with a pharmacist at a chain specialty pharmacy in the DFW area. For the data presented herein, participants had to have attended at least three study visits (in-person or virtual) from December 22, 2019, to June 22, 2021. This 1.75-year timeframe was subdivided into three periods, and every participant included in this analysis had at least one survey completed within each period. The first period, described here as the pre-lockdown period, was from December 22, 2019, to March 21, 2020. The second period, during the lockdown, heralded by the beginning of the Texas state-wide COVID pandemic restrictions, lasted for three months, from March 22, 2020, to June 23, 2020. One year after locking down, the third period began from March 21, 2021, to June 22, 2021. The study coordinator was present on all visits. He provided medical records to the pharmacist when the patient was in the active treatment arm and conducted the intake survey before the MTM session. The data reported herein were obtained from the intake surveys conducted by the study coordinator.
Survey Instrument
The original survey instrument comprised 43 questions of a quantitative assessment of barriers to care, health literacy, and medication adherence, among others. These items were developed from the literature review and adapted to address the objectives of the MTM clinical trial. It was a condensed version of the Medical Outcomes Study Scales (MOS) commonly used as a reliable tool in HIV populations [23].
In this study, the analysis was conducted on ten questions from the original survey questionnaire. Based on expert opinions and a review of relevant literature, these ten questions were deemed relevant to SDOH, and there were no additional questions on SDOH in the original questionnaire. All but the final item was measured on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree). The last question asked about the frequency of alcohol consumption in a week. This was also measured on a 5-point scale from 1(very often) to 5 (never). The survey questions addressed the following: whether the participant got enough sleep, whether pain interfered with their work or activities, whether their health interfered with their social activities, whether they spoke to someone they regularly trusted, whether they worried about running out of food, whether they rationed their food due to shortage, whether they had trouble getting their medications, whether their safety was threatened in the place they sleep or live or by someone whom they knew, whether they skipped taking their medications, and whether they consumed over 4–5 alcoholic drinks a day. Responses regarding enough sleep and speaking to someone regularly were reverse-coded for the analytical models and figure.
Data Analysis
Baseline participant characteristics were described as frequencies and percentages for categorical variables and means and standard deviations (SD) for continuous variables. The distribution of scores for each survey question in each period was evaluated, and medians, interquartile ranges, frequencies, and percentages were reported. To statistically assess whether participants’ responses to the questions changed over time, proportional odds mixed effects logistic regression models were used. Each model included a random participant-level intercept and time as a categorical variable. For each model, the proportional odds assumption was tested and met. Because more than 60% of participants gave the best possible response to each of the last six questions, a secondary analysis was conducted, in which the responses to these questions were dichotomized (5 vs. < 5). We fit binary mixed effects logistic regression models for this analysis, including a random participant-level intercept and time as categorical variables. SAS Enterprise Guide version 8.1 (SAS Institute Inc., Cary, NC) was used for all analyses.
Results
Respondent Demographics
Of the 117 participants enrolled to date (8/26/2022) in the trial, 27 participants met the criteria for inclusion in this analysis. Respondents were 52.9 ± 11.0 years of age, mostly female (51.9%), and diagnosed with diabetes and hypertension (51.9%), along with HIV. All patients with T2DM had HTN, too. Respondent characteristics are presented in Table 1.
Participant Survey Responses
Table 2 summarizes participant responses to the ten survey items. Generally, most survey respondents disagreed with not having enough food, not getting their medicines because of financial problems, feeling like their safety was threatened in the place they sleep or live, and having to skip medicines for more than one day in the last month. However, respondents were neutral regarding getting enough sleep, pain interfering with work or activities, and health interfering with social activities. Most respondents (> 70%) reported never consuming more than 4 or 5 alcoholic drinks a day within the past week.
Responses over Time
The proportional odds mixed effects logistic regression model results showed the odds ratios comparing during and one year after lockdown to the pre-lockdown time point (Table 3). A significant difference was found between one year after lockdown and pre-lockdown periods [OR = 6.39, 95% CI (1.08–37.73), p = 0.04] for responses to the statement “In the last month, I felt like my safety was threatened by the place I sleep or live” after dichotomization of these responses (strongly disagree vs. all others). In other words, a significantly greater proportion of participants reported a “strongly disagree” response on this question during the post-lockdown period compared to the pre-lockdown period. No other statistically significant differences in the responses were found over the study timeframe. As shown in Table 3, p values of odds ratios for the following questions were borderline and showed positive changes when comparing post-lockdown to pre-lockdown time points; “I skipped taking my medicines for more than one day”, “I felt like my safety was threatened by someone I knew”, and “I did not get my medicines because of financial problems”. As depicted in Fig. 1, there were positive changes in response to most survey questions during the study period. However, these changes were not often statistically significant.
Discussion
A significantly greater proportion of participants reported a “strongly disagree” response to the question “In the last month, I felt like my safety was threatened because of the place I sleep or live” during the post-lockdown period compared to the pre-lockdown period. In other words, patients felt less threatened in their living place post-lockdown compared to the pre-lockdown period. Additionally, despite a small sample size, there was still evidence of positive changes comparing post to pre-lockdown periods for the statements on being threatened by someone they knew, skipping taking medicine because of financial problems, and skipping taking medication more than one day. The significant positive change in feelings of safety in the vulnerable study participants and even the lack of negative changes in other SDOH question responses can be attributed to several factors. Among them, COVID-19-related economic policies like the CARES Act and the moratorium on rent and mortgage could play an important role. The Families First Coronavirus Response Act (FFCRA), CARES Act, and American Rescue Plan (ARP) Act were policies enacted by Congress to provide economic relief from COVID-19 [21]. These policies created moratoriums on foreclosures and evictions to prevent individuals from losing their homes during the pandemic and increase compliance with stay-at-home orders. Economic Impact Payments (EIPs) were also established to provide stimulus payments to low- and middle-income earners [24]. By implementing these policies, the basic needs of the community might be met, and the economic balance in society might be improved. This would reduce economic anxiety, which in turn would decrease instances of domestic violence and other crimes and raise safety levels. However, this hypothesis should be evaluated in future studies, as the studies that assessed the impact of the CARES Act on crime and violence rates have shown inconsistent results [25, 26]. These policies could also improve lifestyle management, including regular medication use.
Despite federal provisions, there is skepticism surrounding whether these policy enactments adequately protected populations as initially designed [27]. A recent review asserted that low-income and historically oppressed racial and ethnic minority communities were disproportionately adversely affected by the pandemic and less likely to receive assistance. Structural inequities, including racism and capitalism, pervasive in our society were partly blamed for this occurrence [20]. It has been shown that these minorities were more likely to be significantly disrupted by COVID-19, possibly due to obstacles to receiving government relief packages [28]. The COVID-19 pandemic has shown social, racial, and economic health disparities and has accentuated effects on vulnerable populations. While we did not include an economic status assessment, our participant population generally represents a marginalized and particularly vulnerable population, especially during the COVID-19 pandemic. A systematic review of the association of racial/ethnic and socioeconomic status (SES) with health outcomes and access to healthcare services during the COVID-19 pandemic found that historically oppressed racial/ethnic minority groups had higher risks of COVID-19 infection and confirmed diagnosis, hospitalization, and death [19]. Factors such as low education level, poverty, poor housing conditions, low household income, speaking a language other than the national language in a country, and overcrowded households were cited as contributing factors [19]. Further, due to safety and effectiveness concerns, COVID-19 vaccination refusal is higher among Blacks than Whites [29].
The Census Bureau’s data revealed an assessment of the SDOH for millions of citizens in the United States during the pandemic. Approximately 7% of adults were not confident in their ability to pay for next month’s housing expenses, and 10.3% reported food insufficiency. Notable disparities exist among these measures for Black and Hispanic adults compared to White adults. As compared to 55.5% of White adults, approximately 75% of Black (74.4%) and Hispanic (75.2%) adults reported difficulty paying their household expenditures in early March 2022, but this survey did not provide pre-pandemic measures for comparison, and its finding showed that changes in SDOH did not follow economic indicators or pandemic trends; therefore, caution is warranted to consider the findings related to the COVID-19 pandemic [30]. Although most studies agree that Blacks and other historically oppressed racial/ethnic minorities in the US suffer the most from the COVID-19 pandemic, studies differ in terminology, outcome measures, inaccurate or incomplete race/ethnicity, and SES data [20].
To our knowledge, no studies have assessed housing security pre-, during, and post-lockdown. Studies have, however, associated housing insecurity with poor health status and stress. A study of a nationally representative sample of US adults reported an association between housing insecurity, higher psychological distress, and lower self-rated health during the COVID-19 pandemic. They also asserted that the CDC’s nationwide eviction moratorium may have mitigated these associations [31]. A study revealed that the CARES Act significantly decreased eviction rates across the US [32]. Therefore, the likely rationale for our findings over the study time includes policy measures enacted to mitigate the economic, social, and health issues, particularly those of low-income and racial/ethnic minority populations. Financial payments and mortgage and rent moratoriums may have contributed to perceived food, income, and housing security.
Limitations
This study has some limitations that may limit the generalizability of the findings. The major limitation of this study was the use of a regional survey sample for a specifically marginalized population as a nationally representative sample. The restricted geographic location of Dallas-Fort Worth, Texas, as well as the recruitment strategies for this sample, limits the generalizability of the study findings. Also, no measures of SES (income or education level) were collected; as such, no assumptions could be made regarding the respondents’ socioeconomic status baseline to infer any change. A small study sample size should also be considered as one of the reasons for not having statistically significant changes for some questions in this study. Besides, being a subset of a larger ongoing study created limitations related to research design and capabilities. The larger study was not designed specifically to answer the current research question; thus, there is the risk of selection and information biases. Moreover, given data collection in person or via phone, social desirability bias may have influenced participants to respond more positively. Many studies acknowledge social desirability bias as a limitation in interviews and surveys [33,34,35]. Additionally, the survey instrument used in this study was not validated for this population to address SDOH specifically.
Conclusions
The participants felt significantly safer where they slept or lived one year after lockdown than pre-lockdown. This change can be attributed to multiple social factors. One of the plausible explanations can be rent and mortgage moratoriums and housing protections provided by the CARES Act. Future research on a representative and large population size is recommended. Evaluating the CARES effect on health disparities will lead to improved awareness that drives policy and practice as we strive to narrow the gaps in health inequity. A multi-pronged approach to addressing the interconnected issues plaguing the healthcare sector and other social and economic sectors will be integral to closing this gap.
References
Centers for Disease Control and Prevention. National Center for HIV, Viral Hepatitis, STD, and TB Prevention Atlas Plus. www.cdc.gov/nchhstp/default.htm. October 1, 2021. Accessed 15 November 2022.
Centers for Disease Control and Prevention. HIV among African Americans. Fact sheet. www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-hiv-aa-508.pdf. Accessed 31 October 2022.
Kaiser Family Foundation. Black Americans and HIV/AIDS: the basics. Fact sheet. www.kff.org/hivaids/fact-sheet/black-americans-and-hivaids-the-basics/ .Accessed 19 May 2022.
Centers for Disease Control and Prevention. National diabetes statistics report. Estimates of diabetes and its burdens in the United States. www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed 1 December 2022.
Centers for Disease Control and Prevention. Facts about hypertension in the United States. https://www.cdc.gov/bloodpressure/facts.htm. Accessed 1 December 2021.
Ellis KR, Hecht HK, Young TL, et al. Chronic disease among African American families: a systematic scoping review. Prev Chronic Dis. 2020;17:E167. https://doi.org/10.5888/pcd17.190431.
Noonan AS, Velasco-Mondragon HE, Wagner FA. Improving the health of African Americans in the USA: an overdue opportunity for social justice. Public Health Rev. 2016;37:12. https://doi.org/10.1186/s40985-016-0025-4.
Centers for Disease Control and Prevention. Frequently asked questions. What is health equity? www.cdc.gov/nchhstp/socialdeterminants/faq.html. Accessed 10 December 2019.
Healthy People 2030. Social determinant of health. https://health.gov/healthypeople/priority-areas/social-determinants-health. Accessed 12 April 2023.
Mohan D. People’s right to safety. Introduction: safety as a human right. Health and human rights. President and Fellows of Harvard College. 2003;6(2). https://www.hsph.harvard.edu/hhrjournal/wp-content/uploads/sites/2469/2014/04/10-Mohan.pdf. Accessed 12 April 2023
Mohammadinia L, Khorasani-Zavareh D, Gharibzadeh S, Roshanfekr P, Malekafzali H. Social determinants of health and home safety for under-five children in a neighbor’s Tehran. Iran Int J Prev Med. 2018;9:109. https://doi.org/10.4103/ijpvm.IJPVM_60_17.
Centers for Disease Control and Prevention. Underlying medical conditions associated with higher risk for severe COVID-19: information for healthcare professionals. 2022. www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html. Accessed 11 October 2022.
Centers for Disease Control and Prevention. Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Accessed 10 November 2022.
Magesh S, John D, Li WT, Li Y, Mattingly-App A, Jain S, Chang EY, Ongkeko WM, et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw Open. 2021;4(11):e2134147. https://doi.org/10.1001/jamanetworkopen.2021.34147.
Herby J, Jonung L, Hanke S. A literature review and meta-analysis of the effects of lockdowns on COVID-19 mortality. The Johns Hopkins Institute for Applied Economics, Global Health, and the Study of Business Enterprise. https://sites.krieger.jhu.edu/iae/files/2022/01/A-Literature-Review-and-Meta-Analysis-of-the-Effects-of-Lockdowns-on-COVID-19-Mortality.pdf. Accessed 31 August 2022.
Banholzer N, Lison A, Vach W. Comment on ‘A literature review and meta-analysis of the effects of lockdowns on COVID-19 mortality’. https://ssrn.com/abstract=40324772022. Access 11 Febrary 2022.
Chu L, Teng L. Does stimulus check payment improve people’s mental health in the COVID-19 pandemic? Evidence from U.S. household pulse survey. J Ment Health Policy Econ. 2022;25(4):133–42.
Tsai J, Huang M, Rajan SS, Elbogen EB. Prospective association between receipt of the economic impact payment and mental health outcomes. J Epidemiol Community Health. 2022;76(3):285–92. https://doi.org/10.1136/jech-2021-216661.
Khanijahani A, Iezadi S, Gholipour K, Azami-Aghdash S, Naghibi D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health. 2021;20(1):248. https://doi.org/10.1186/s12939-021-01582-4.
Vasquez RM. The disproportional impact of COVID-19 on African Americans. Health Hum Rights. 2020;22(2):299–307.
Cyrus E, Clarke R, Hadley D, et al. The impact of COVID-19 on African American communities in the United States. Health Equity. 2020;4(1):476–83. https://doi.org/10.1101/2020.05.15.20096552.
Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Accessed 3 December 2022.
Bozzette S, Hays R, Berry S, Kanouse DE, Wu AW. Derivation and properties of a brief health status assessment instrument for use in HIV disease. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8(3):253–65. https://doi.org/10.1097/00042560-199503010-00006.
Cox K, Jacoby S, Marr C. Stimulus payments, child tax credit expansion were critical parts of successful COVID-19 policy response. https://www.cbpp.org/research/federal-tax/stimulus-payments-child-tax-credit-expansion-were-critical-parts-of-successful. Access 22 June 2022.
Pritchard D. The impact of the 2020 CARES Act stimulus payments on crime. Texas A&M University. 2022. http://people.tamu.edu/~davidpritchard/David%20JMP.pdf. Accessed 13 April 2023.
Erten B, Keskin P, Prina S. Social distancing, stimulus payments, and domestic violence: evidence from the U.S. during COVID-19. 2021. https://pinarkeskin.com/onewebmedia/EKP_Mar2021.pdf. Accessed 13 April 2023.
Sontan O. Care Ethics versus the CARES Act. Hastings Cent Rep. 2021;51(4):7–8. https://doi.org/10.1002/hast.1266.
Gutkowski V. Racial and ethnic disparities in access to COVID-19 Relief. 2022. https://www.stlouisfed.org/on-the-economy/2022/jul/racial-ethnic-disparities-access-covid19-relief. Accesed 20 October 2022.
Callaghan T, Moghtaderi A, Lueck JA, et al. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med. 2021;272:113638. https://doi.org/10.1016/j.socscimed.2020.113638.
Drake P, Rudowitz R. Tracking social determinants of health during the COVID-19 pandemic. www.kff.org/coronavirus-covid-19/issue-brief/tracking-social-determinants-of-health-during-the-covid-19-pandemic/ . Accessed 22 April 2021.
Himmelstein G, Desmond M. Eviction and health: a vicious cycle exacerbated by a pandemic. Health Affairs Health Policy Brief. 2021. https://doi.org/10.1377/hpb20210315.747908.
Jeff Ernsthausen J, Simani E, The eviction ban worked, but it’s almost over. Some landlords are getting ready. The Pandemic Economy. ProPublica. https://www.propublica.org/article/the-eviction-ban-worked-but-its-almost-over-some-landlords-are-getting-ready . Access 24 July 2020.
Latkin CA, Edwards C, Davey-Rothwell MA, Tobin KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. 2017;73:133–6. https://doi.org/10.1016/j.addbeh.2017.05.005.
Latkin CA, Vlahov D, Anthony JC. Socially desirable responding and self-reported HIV-infection risk behaviors among intravenous-drug-users. Addiction. 1993;88(4):517–26. https://doi.org/10.1111/j.1360-0443.1993.tb02058.x.
Goh GS, Khow YZ, Tay DK, Lo NN, Yeo SJ, Liow MHL. Preoperative mental health influences patient-reported outcome measures and satisfaction after revision total knee arthroplasty. J Arthroplasty. 2021;36(8):2878–86. https://doi.org/10.1016/j.arth.2021.03.026.
Acknowledgements
The authors would like to acknowledge the participating pharmacists that conducted MTM for this study and the Student Research Assistants (Funmilayo Yesufu, Ying Qin, Jenna Ference, Yesha Patel, and Goke Sule) that facilitated data entry.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium This work was supported by the National Institutes of Health [5U54MD006882-08].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
The study was approved by the North Texas Regional Institutional Review Board (NTRIRB approval # 2018–094).
Competing Interests
The authors declare no competing interests.
Disclaimer
The funding source was not involved in the study design, collection, analysis, interpretation of data, the writing of the report, nor the decision to submit the article for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
At the time of the study, Deidra Lee was a Postdoctoral Research Fellow, Department of Pharmacotherapy, University of North Texas Health Science, Center College of Pharmacy, Fort Worth, Texas.
At the time of the study, Jennifer Cooper is at The Ohio State University and The Research Institute at Nationwide Children’s Hospital, Columbus, OH, USA.
At the time of the study, Kathleen Borgmann was an Assistant Professor at the University of North Texas Health Science Center, School of Biomedical Sciences, Fort Worth, Texas.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fleming, M., Lee, D., Oranu, C. et al. Positive Changes in Safety Perception Among Blacks with HIV and Comorbidities: Assessment of Social Determinants of Health During COVID-19. J. Racial and Ethnic Health Disparities 11, 1578–1586 (2024). https://doi.org/10.1007/s40615-023-01633-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01633-2