Abstract
Studies of health care access and use among historically resilient populations, while common, often field a limited sample size and rarely ask the groups most impacted by health inequities to weigh in. This is especially so for research and programs that focus on the American Indian and Alaska Native (AIAN) population. The present study addresses this gap by examining data from a cross-sectional survey of AIANs in Los Angeles County. To better interpret project findings and generate culturally relevant contexts, qualitative feedback was gathered at a community forum held in Spring 2018. Because recruitment of AIANs has historically been challenging, purposive sampling was employed to strategically identify a larger eligible pool. Among those who were eligible, 94% completed the survey (n = 496). AIANs who were enrolled in a tribe were 32% more likely to use the Indian Health Service (IHS), compared with those who were not enrolled (95% CI: 20.4%, 43.2%; p < .0001). In multivariable modeling, the strongest factors influencing IHS access and use were: tribal enrollment, preference for culturally-specific health care, proximity of the services to home or work, having Medicaid, and having less than a high school education. Feedback from the community forum indicated cost and trust (of a provider) were important considerations for most AIANs. Study findings reveal heterogeneous patterns of health care access and use in this population, suggesting a need to further improve the continuity, stability, and the image of AIANs’ usual sources of care (e.g., IHS, community clinics).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health care access and use among the American Indian and Alaska Native (AIAN) population are often more nuanced than what has been documented in the greater body of health services research literature [1,2,3,4]. While such findings are typically based on data from large national or state surveys—e.g., the National Health Interview Survey, the Medical Expenditure Panel Survey, or the California Health Interview Survey—these data sources often lack sample size and may generate limited information about potential factors, such as tribal enrollment, preferences for culturally-specific health care and behaviors related to health, that may affect the population’s consumption of health care goods and services. Other studies have demonstrated that AIANs are more likely to be uninsured and have less health services utilization than non-Hispanic whites, frequently driven by unique, intended and unintended disparities in socioecological factors at multiple levels [5,6,7,8]. Given that AIANs are entitled to receive health care under the United States (U.S.) Constitution through the Indian Health Service (IHS) and are often underrepresented in health services decisions and policy planning, a deeper dive into how they seek and obtain care (e.g., level of health insurance coverage, patterns of IHS use, preferences for place of usual care) may help to reveal hidden gaps or meaningful facilitating circumstances that could be applied in medicine and public health to better foster and promote interventions that fit this population’s needs. Research and quality improvement projects that proactively elicit direct input from community members, for example, may represent a promising approach to improving health care for the AIAN population, especially if it could be incorporated as a routine process in federal, state, and local planning of health services.
Presently, Los Angeles County (LAC), California is the county with the largest AIAN population in the nation [9]. Compared to other racial/ethnic groups in the region [10, 11], marked health disparities in both morbidity and mortality exist for this institutionally underserved and historically resilient population. In particular, these and other disparities (social/class in origin) cluster among urban-dwelling AIANs in LAC. It is also important to note that although approximately 75% of the AIAN population resides in urban areas, urban AIAN healthcare receives only 1% of IHS funding. For accessing care, it is also important to note that LAC is home to only one Urban Indian Organization (UIO), contracted by the IHS; it provides limited ambulatory care services. Because there are requirements for providing services as a UIO provider, patients who visit a UIO must meet certain “Urban Indian” eligibility criteria to receive services. Broadly these eligibility criteria include being a member of a tribe, including those who were terminated since 1940, those who are now or in the future recognized by the state, is an Alaska Native, a California Indian, a descendent, and so on and so forth as defined by the IHS. There is otherwise no directly operated IHS facilities or tribally compacted clinics within LAC, beyond this UIO. AIAN within LAC otherwise have access to the same health care options within the county as other LAC residents depending on financial circumstances. To date, only a paucity of research has described or characterized access to care and IHS use in this group; no study has examined these issues by applying a local, indigenized lens to help interpret their health data and health needs.
The present study addresses this gap in practice by using a combined quantitative and qualitative approach to attaining a deeper understanding of the factors that may impede or drive health care access and use among local AIANs in LAC. Guided by a framework based on the indigenist and decolonizing research methodology [12], the study team conducted a survey of eligible AIANs and convened a follow-up community forum to meaningfully integrate the interpretation of the results by members of LAC’s AIAN community into the final reporting. In both parts of the study, the team focused on two health equity indicators/outcomes of interest: (i) health care access as measured by health insurance coverage; and (ii) health services utilization as measured by IHS use and/or use of community clinics.
Methods
Conceptual Framing
The present study synthesizes and draws upon concepts from the indigenist and decolonizing research methodology [12], including but not limited to principles such as relationality, reciprocity, relational accountability, and honoring indigenous ways of knowing, to help guide the research design, data analysis, and interpretation of the results. For example, relationality was achieved by honoring all expertise and sharing power between institutions, community partners, a community advisory board that had oversight over many parts of the survey process, and community members. Reciprocity and relational accountability were accomplished by sharing results with community members. Indigenous ways of knowing were achieved by giving the AIAN community power to define some of the survey questions and shape the narrative around study results. Narrative construction was accomplished by garnering feedback through a community forum where AIAN community members, recruited by participating community-based organizations, were able to listen to a presentation of the results and provide insights during break-out groups. The Indigenous lens used to organize this study’s synthesis of the data shares similar underpinnings as those commonly valued in community-based participatory research: i.e., a strong focus on community strengths, equity, and systems change.
Survey Development and Quantitative Data Collection
A cross-sectional survey of AIANs was conducted June to October 2016 by the Los Angeles County Department of Public Health (DPH), in partnership with three large AIAN community-based organizations in LAC. Primary data collection was carried out at these organizations’ facilities and events using purposive sampling, whereby a systematic approach to recruitment and administration was undertaken and clear delineation of the eligible pool of AIANs were identified. This approach was necessary because survey research has historically fielded small sample sizes in this population principally as a result of the community itself being smaller than the general population, cost of reaching this hard-to-reach group, known trust issues with the government, among other barriers [4, 6].
A majority of the survey questions were adapted from large national, state, and/or local surveys (e.g., Behavioral Risk Factor Surveillance System, California Health Interview Survey, and the Los Angeles County Health Survey), with some of them being generated through community defined knowledge or Indigenous ways of knowing. For example, participants contributed questions that were more salient to their experiences with health care as an American Indian or Alaska Native person. This more transparent approach involving the AIAN community lends strength to the survey development process and was not seen as a bias or limitation.
The survey instrument was divided into four parts: (1) sociodemographic characteristics, including tribal enrollment status; (2) health insurance coverage and IHS eligibility and use; (3) opinions and preferences about AIAN clinics; and (4) questions that screened for depression. The instrument was written at a 7th grade Flesch-Kincaid Reading Level, with the Flesch Reading Ease score at 62% [13].
Acknowledging the need for trusted messengers in the research process, staff at the AIAN community-based organizations were trained to distribute the 4-page, self-administered instrument (paper questionnaire, see Supplemental material) to AIAN clients upon check-in at their facilities. Eligibility criteria included those who were 18 years and older, self-identified as AIAN, and resided in LAC. Exclusion criteria included those who were younger than 18 years of age, did not self-identify as AIAN, and were not a resident of LAC. The recruitment procedures accounted for seasonal, as well as daily variation in client volume. Additionally, recruitment occurred at periodic on- and off-site outreach/programmatic events. A gift card valued at $5.00, and a Healthy LA Native branded water bottle valued at $2.00 were given to all participants who enrolled and completed the survey. The survey completion rate was calculated based on the number of completed eligible surveys divided by the sum of completed, refused, incomplete, and/or missing surveys collected during a specified timeframe. Participants of the survey were drawn from a universe of those who attended or could attend the events/clinics and were available to complete the survey. Power to reach a large enough sample size was considered, in part, because recruiting AIAN participants in survey research has historically been difficult to do. Data were collected and initially entered into an Excel database, which was then cleaned and analyzed.
The study was deemed minimal risk to survey participants by the DPH Institutional Review Board (IRB). The same decision was reached by the UCLA IRB, as additional IRB review and approval from the latter institution became necessary when the primary investigator/primary author transitioned to the institution for fellowship. Based on guidance from the IRBs, written informed consent was not required, instead, implied informed consent was used if participants had read the embedded information in the introduction of the survey and proceeded to complete the questionnaire. The study received exempt status in accordance with the common rule, Title 45, Part 46 of the Code of Federal Regulations.
Quantitative Data Analysis
Descriptive analyses were conducted to identify and describe survey participant preferences for health care from a community perspective, tribal enrollment status, health insurance coverage status (e.g., Medi-Cal [California’s Medicaid program], Medicare, Veteran’s Affairs benefits, HMO, PPO insurance plan, or other health insurance obtained through the Affordable Care Act), IHS use (health services utilization), and sociodemographic characteristics (e.g., age, sex, education, income, housing status, transportation, and depression screening score).
Two different analytical approaches were used for the main analyses: (1) multivariable regression, and (2) best subsets regression. For both approaches, there were 2 primary dependent variables (outcomes): insurance coverage, and IHS use. Insurance coverage was defined as those who answered “yes” to having health insurance. Anyone who answered “no” or “I don’t know” to having health insurance coverage were classified as “uninsured.” IHS use was defined as those who answered “yes” to using the IHS in the survey. Those who answered “no” or “I don’t know” about whether they used the IHS were classified as not using IHS.
Multivariable regression models were constructed to examine the associations between the two independent variables of interest—i.e., enrollment in a tribe and health care preferences—and the dependent variables: health insurance coverage and IHS use. Potential confounders/control variables were identified using a priori information about known biologic or social causal relations and through the construction of directed acyclic graphs [14, 15].
Best subsets algorithms were also employed to explore and identify factors that may influence health insurance coverage (access to care) and the use of the IHS among the urban-dwelling AIANs in LAC. Best subsets algorithms applied all combinations of variables to find factors which most strongly impacted the dependent variables. Other variables considered in these models pertained to at least one of the following groupings: sociodemographics, perceived benefits and barriers to using the services, AIAN cultural experiences, and screening for depression. A score of 3 or more on the Patient Health Questionnaire-2 (PHQ-2) indicated a positive screening for likely depression or related depressive disorder [16]. The multiple imputations methodology was applied to help handle missing data, assuming missingness was not at random.
All analyses were carried out using STATA version 14.1 (StataCorp. 2015. Stata Statistical Software, Release 14. College Station, TX: StataCorp LP) and SAS version 9.4 (SAS Institute Inc., Cary, NC) software packages.
Community Forum—Qualitative Data Collection and Analysis
Recruitment
A one-time community forum was held in May of 2018 with the goals of sharing back survey findings, and eliciting community interpretation of results. Flyers were posted in participating community-based organization waiting rooms, websites, and social media accounts. Information was also shared with staff from the partnering local department of public health, as well as the partnering academic institution. A total of 66 participants attended the forum. For the convening, all participants were informed that there would be note-takers present at the meeting; they were given the opportunity to strike their comments from the record at any time if they chose. In addition, all participants were told that no personal identifying information was to be collected.
Collection and Analysis of the Data
Community input was recorded via note-takers. These note-takers were self-identified AIAN graduate students recruited through a local university’s American Indian Studies Program listserv. Pre-determined questions were posed throughout the icebreaker, the data presentation, and subsequent breakout groups. Descriptive content and synopses from the note-takers were entered into Microsoft Excel, and analyzed using the thematic analysis method described by Braun and Clarke [17]. In short, thematic analysis is a systematic 6-phase method for identifying, analyzing and reporting patterns (themes) within data. Initial coding was completed on all data (feedback from forum participants). To ensure fidelity of the initial codes a modified process of synthesized member checking (SMC) was carried out with three community members who participated in the community forum. SMC is a method whereby interview data and interpreted data are returned to participants (usually in paper form) for review and feedback. SMC enables participants to add comments in writing which are then searched for confirmation or disconfirming resonance with the analyzed study data, thus, enhancing the credibility of the results. This process was modified by inviting participants to give their feedback orally after having interacted with the data in real-time. Codes were then reconciled with the primary author’s codes and synthesized into subsequent themes.
Results
Survey Findings
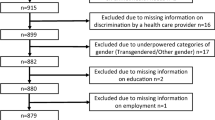
From June to October 2016, 533 prospective participants were approached and 501 of them completed the survey, yielding a completion rate of 94%. Five surveys were excluded as these participants were not AIAN, yielding a sample size of 496. Overall, 80.2% of the participants were enrolled in a tribe (Table 1). More than 90% were under 65 years of age, a majority were female (64.4%), and over three-fifths (62.4%) had some college experience or were college graduates. Despite a relatively high level of education, 55.4% had an income of less than $19,999. Over 60% reported they preferred being seen at an AIAN clinic, while about one-quarter were unsure. Approximately 90% had health insurance coverage and 44% used the IHS (Table 1). Nearly half of the AIAN survey participants screened positive for likely depression.
The top three services ranked by survey participants as “very important” to have in an AIAN clinic were dental services (72.7%), services for people with disabilities (65.5%), and specialty care, including any medical subspecialty beyond primary care (64.7%). The lower or bottom three services as ranked by the participants were traditional healers (57.1%), doctors and staff that are AIAN (45.5%), and doctors and staff that are not AIAN, but are culturally sensitive towards AIAN patients (44.1%). A majority of participants who used the IHS answered they also used the sole Urban Indian Organization (UIO) in LAC (a clinic at least partially funded by the IHS), but several indicated they traveled as far as Alaska, Arizona, Montana, New Mexico, and surrounding counties to access other sites (whether tribal, directly operated, or other urban sites).
The multivariable regressions provided adjusted prevalence differences for the two outcome variables: (1) health insurance coverage for those enrolled in a tribe versus those who were not enrolled in a tribe and (2) IHS use (Table 2). Health insurance coverage was similar for AIANs enrolled in a tribe as compared with those who were not enrolled in a tribe (prevalence difference −3.5%; 95% CI: −10.5%, 3.6%; p = .34). IHS use was 32% more frequent among AIANs who were enrolled in a tribe as compared with those who were not enrolled in a tribe (95% confidence interval [CI]: 20.4%, 43.2%; p < .0001).
When examining the effect of preference for culturally-specific health care, health insurance coverage was slightly less than anticipated, but not significantly different, for AIANs who preferred culturally-specific health care services compared with those who did not, after adjusting for other non-AIAN race/ethnicities, depression, IHS eligibility, enrollment in a tribe, homelessness, highest level of education, and unemployment (95% CI: −11.1%, 0.7%; p = .08) (Table 3). For patterns on utilization, AIANs were 13.4% more likely to use the IHS if they preferred culturally-specific health care versus if they did not, after adjusting for other non-AIAN race/ethnicities, depression, and IHS eligibility (95% CI: 5.6%, 21.2%; p = .0008).
Best subsets algorithms revealed several factors that had the strongest factors positively impacting health insurance coverage. They were having two or more children in the household, wanting to learn more about their AIAN culture, and being female. Younger ages (18–39) and self-reporting as Black in addition to AIAN negatively impacted having health insurance coverage (Tables 4 and 5).
Among AIANs participating in the survey, the strongest impact on increasing IHS use were the reported importance of working or living near an IHS clinic, tribal enrollment, preference for culturally-specific health care, Medicaid coverage (Medi-Cal in California), and having less than a high school education. Younger age (ages 18–39) negatively impacted IHS use. The largest prevalence difference for IHS use was between those who were enrolled in a tribe (51.5%) and those who were not enrolled in a tribe (11.5%) (adjusted prevalence difference = 32.3%; 95% CI: 22.4%, 42.2%; p < .0001).
Findings from the Community Forum
Despite the diversity of health insurance coverage (based on the survey data) and IHS use, a majority of the dialog at the community forum centered around IHS use and preferences for culturally-specific care. Thematic analyses of the qualitative data (feedback from forum participants) identified four primary themes: (1) quality of care, (2) scope of services, (3) trust/mistrust, and (4) system-based considerations (Fig. 1).
Quality of care was a major theme during the forum discussion. Content ranged from positive to negative perceptions about the quality of care within the IHS. Personal stories were shared as anecdotes, yet some community members expressed an agnostic view about preference for culturally-specific care or the IHS, citing they simply wanted the best care.
When it came to the scope of services offered, community members shared a polarized view. Some were of the opinion that care delivered by the IHS was not only comprehensive, but free. Others felt that there were certain things not covered. Not having dental and specialty care services were specifically referenced as limitations of the IHS. For instance, one community member said, “if you need a specialty doctor, make connections elsewhere.” Another noted, “dental services are not often covered or they’re more expensive.”
Perceptions of trust and mistrust were influenced by reputation and confidentiality. Several community members reported that IHS had “a bad reputation” and that “bad news travels fast.” There was additional mistrust when it came to IHS operating within small communities where “everybody talks,” which suggests there were issues with confidentiality. However, many cited “familiarity” as a reason to trust the IHS.
Lastly, community members reported multiple systems-based considerations that negatively or positively affected AIAN access to and use of the IHS. Negative perceptions included a lack of information and outreach as evidenced by many noting “I didn’t know this was the Indian Health Service,” referencing the Urban Indian Organization in which the community forum was held. Several community members also referenced limited hours, excessive paperwork, and a lack of transportation as barriers to accessing and using IHS. Conversely, positive system attributes included the fact that the service was perceived as “free,” and provided “all-in-one” services and transportation at some sites.
Discussion
To the best of our knowledge, this is the first study of its kind to include tribal enrollment status, preferences for culturally-specific health care, health insurance coverage, and IHS use as part of a more complex but pragmatic modeling of an urban AIAN population dataset. The study is also among the first to use a sample size that is larger than most surveys and sufficiently powered for quantitative analysis. As part of the qualitative data collection and analysis process, the study elicited the assistance of the AIAN community to jointly interpret and frame user perspectives on health care access and use in this population.
Tribal Enrollment
Having health insurance coverage was similar for AIANs who were enrolled in a tribe compared with those who were not enrolled in a tribe (−3.5%, 95% CI: −10.5%, 3.6%; p = .34). Interestingly, this seems to contrast the community forum interpretation which points to the likely circumstances in which insurance is perceived as being expensive compared with the “free” services that IHS offers (i.e., assuming the members are aware of, eligible for, and have enrolled in the system). Other forum members noted the process of signing up for health insurance as rather burdensome, and for a small group there was a general thought that there was no need to see a doctor.
In contrast to the patterns of health insurance coverage reported, AIANs who were enrolled in a tribe were found to be 31.9% more likely to use the IHS as compared with those who were not enrolled in a tribe. This finding is not entirely surprising given that the IHS website brands itself as a health care system for federally recognized American Indians and Alaska Natives in the US. Albeit, as echoed in the community forum, many eligible individuals may not be aware of their eligibility to receive care from the IHS. Implications exist for contracted IHS providers to educate about the intersection of obtaining insurance and IHS eligibility. At least for the UIO in this study, evidence points to the opportunity to aid in insurance enrollment as well as facilitate a low-barrier approach to potential eligible users.
Culturally-Specific Health Care
The present study found that AIAN survey participants who preferred culturally-specific health care were 13.4% more likely to use the IHS (95% CI: 5.6%, 21.2%; p = .008). However, AIANs who preferred culturally-specific care were only slightly, and not significantly less likely to have health insurance (−5.2%, 95% CI: −11.1%, 0.7%; p = .08). Based on data collected from the community forum, there was some evidence to suggest that some AIANs may believe having health insurance and obtaining culturally-specific services were mutually exclusive. There was also some confusion about how health insurance is or is not connected to IHS operation (e.g., a community member asked if billing insurance goes to help IHS clinics). Regardless, the expectation that culturally-specific health care could be delivered by the diverse clinical settings lumped into the IHS umbrella (UIOs, tribally compacted clinics, or directly operated facilities) may not be consistent with reality.
Given the well-documented underfunding of the IHS, particularly the dramatic underfunding of UIOs [18], it can be helpful for AIAN patients to obtain health insurance in addition to using the IHS. This not only serves as a way to generate revenue for UIOs but may introduce a broader range of services that may not otherwise be available.
A recent study found that persistent perceptions of health care insecurity were a major barrier to AIAN well-being [19]. Almost half of the participants in the present survey screened positive on the depression screener, suggesting further evaluation is warranted to see if they meet criteria for more severe depressive disorders. Feedback from the community forum seems to corroborate this finding. Psychological distress may not only emanate from health care insecurity, but could also be associated with the well-documented historical mistrust of government and health care institutions. For local providers, this again underscores the importance of having culturally appropriate care available and trauma-informed environments that people can go to address or alleviate these common problems and concerns.
Despite over 60% of the participants stating a preference to be seen in an AIAN clinic presumably because of its culturally relevant service options, key preferences such as seeing traditional healers, having doctors and staff that are AIAN or are at least culturally sensitive were ranked lower than preferences having to do with providing comprehensive care. This finding, however, is not entirely unanticipated since a more immediate need to address basic medical needs makes practical sense. Feedback from the community forum offered additional insights on this, revealing that there were more nuanced concerns not captured by the survey. Prominent among them were concerns about the quality of care, trust, and scope of services that were offered by the IHS.
IHS Performance and Funding Support
The IHS has had performance challenges, which unfortunately has garnered more attention than its unique innovations [20,21,22]. Given that implementation of services can range from directly operated facilities to tribally operated facilities to UIOs, the range of opinions expressed at the community forum was not surprising. Even though the US government is legally obligated to provide health care for AIANs, the IHS is only funded at 56% of need, with its per capita spending being significantly lower than those of other agencies within the US Department of Health and Human Services [18]. Clearly, access to essential health services and quality of care will continue to be affected if federal funding does not increase.
Factors that Influence Health Care Access and IHS Use
Factors that had the strongest positive impact on having health insurance coverage included having two or more children in the household, female gender, and considering learning more about their culture as “extremely important” or “very important” by the survey participants. Factors which had the strongest negative impact on having health insurance coverage were, in addition to being AIAN descent, self-identified as being Black and younger in age (< 40 years of age). These results were not surprising, as those who want to learn more about their culture may be more connected to community organizations that typically provide trusted outreach to AIANs; in turn, these organizations may be more primed to describe how and why it is important to obtain health insurance coverage.
In contrast, factors that had the strongest positive impact on IHS use were tribal enrollment, preference for culturally-specific health care, proximity to clinic access, level of education, age over 39, and Medicaid enrollment. While the results were not entirely unexpected, they do point to a need for better engagement of the AIAN population and to identify ways that can help increase the use of IHS in LAC.
Limitations
The present study has several limitations. First, although purposive sampling was the most efficient way and the only feasible method of obtaining a sufficiently powered AIAN sample in LAC, this approach limits the generalizability of the results (i.e., the sample is more representative of AIANs who sought culturally-specific services at AIAN community-based organizations than other AIANs in the region).
Second, self-administered surveys are subject to problems due to missing data. To address this issue, the study used multiple imputations prior to performing best subsets algorithms modeling. Third, as a cross-sectional study, the results can only be used to examine associations between factors and the prevalence of health insurance coverage and IHS use.
Lastly, the qualitative data (feedback) from the community forum was recorded by hand per participant preference, as opposed to using technology, such as voice or video recording. The latter could have improved the capacity to capture more precise and accurate data with less chance for human errors.
Conclusions
The present study utilized a research process that involved AIAN community participation, an important step towards using data to inform health policy and practice in a more meaningful, culturally congruent way. This model of practice has the potential to ensure that community voice and participation are consistently included in research and used strategically to inform health policy and health services decisions that may influence health care access and use among AIANs at the federal, state, and local level.
References
Andersen R. Behavioral model of families’ use of health services. Chicago (IL): University of Chicago, Center for Health Administration Studies; 1968.
Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–302.
Penchansky R, Thomas J. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40.
Derose KP, Gresenz CR, Ringel JS. Understanding disparities in health care access—and reducing them through a focus on public health. Health Aff (Millwood). 2011;30:1844–51.
Zuckerman S, Haley J, Roubideaux Y, Lillie-Blanton M. Health service access, use, and insurance coverage among American Indians/Alaska Natives and Whites: what role does the Indian Health Service play? Am J Public Health. 2004;94(1):53–9.
American Indian Studies Center at UCLA. Access to care among American Indians and Alaska Natives in Los Angeles.; 2016. Available at: https://www.aisc.ucla.edu/research/pb4.aspx. Accessed September 2018.
Sommerfield DH, Jaramillo ET, Lujan E, Haozous E, Willging CE. Health care access and utilization for American Indian Elders: a concept-mapping study. J Gerontol B Psychol Sci Soc Sci. 2021;76(1):141–51.
Kim G, Bryant AN, Goins RT, Worley CB, Chiriboga DA. Disparities in health status and health care access and use among older American Indians and Alaska natives and non-Hispanic Whites in California. J Aging Health. 2012 Aug;24(5):799–811.
United States Department of Commerce, Bureau of the Census, American Fact Finder: 2012-2016 American Community Survey 5-Year Estimates. Accessed September 2018. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF
Los Angeles County Department of Public Health, Office of Women’s Health. Health indicators for women in Los Angeles County: highlighting disparities by ethnicity and poverty level, 2017. Los Angeles, CA: U.S.
Jacobs-Wingo JL, Espey DK, Groom AV, Phillips LE, Haverkamp DS, Stanley SL. Causes and disparities in death rates among urban American Indian and Alaska Native populations, 1999-2009. Am J Public Health. 2016;106(5):906–14.
Rix EF, Wilson S, Sheehan N, et al. Indigenist and decolonizing research methodology. In: Handbook of Research Methods in Health Social Sciences. P. Liamputtong. Singapore: Springer Singapore; 2018. p. 1–15.
Kincaid JP, Fishburne RP, Rogers RL, et al. Derivation of new readability formulas (automated readability index, fog count, and Flesch reading ease formula) for Navy enlisted personnel. Research Branch Report 8–75. Chief of Naval Technical Training: Naval Air Station Memphis, 1975.
VanderWheele TJ, Hernan MA, Robins JM. Causal directed acyclic graphs and the direction of unmeasured confounding bias. Epidemiol. 2008;19(5):720–8.
Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int J Epidemiol. 2016;45(6):1887–94.
Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item pression screener. Med Care. 2003;41:1284–92.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psych. 2006;3(2):77–101.
Joseph A, Pratt B, Joseph V. The National Tribal Budget Formulation Workgroup’s Recommendations on the Indian Health Service Fiscal Year 2021 Budget. National Indian Health Board. Ending the health crisis in Indian Country; a path to fulfill the trust and treaty obligations. Available at: https://www.nihb.org/docs/04242019/307871_NIHB%20IHS%20Budget%20Book_WEB.PDF. Published 2019. Accessed July 1, 2021.
Jaramillo ET, Willging CE. Producing insecurity: healthcare access, health insurance, and wellbeing among American Indian elders. Soc Sci Med. 2021;268:113384.
Indian Health Service: actions needed to improve oversight and quality of care. Gov Acc Office. 2017;17:181.
Sequist TD, Cullen T, Bernard K, Shaykevich S, Orav EJ, Ayanian JZ. Trends in quality of care and barriers to improvement in the Indian Health Service. J Gen Intern Med. 2011;26(5):480–6.
Carroll M, Cullen T, Ferguson S, Hogge N, Horton M, Kokesh J. Innovation in Indian healthcare: using health information technology to achieve health equity for American Indian and Alaska Native populations. Perspect Health Inf Manag. 2011;1(8):1d.
Acknowledgements
The authors thank the Rapid Assessment, Training, and Evaluation Unit at the Office of Health Assessment and Epidemiology in the Los Angeles County Department of Public Health for their technical support and contributions to the data collection. The authors also thank the Community Advisory Board, the three community-based organizations, and the Los Angeles American Indian and Alaska Native community members for their logistical support of this project. Finally, the authors thank Dr. Lori Fischbach for her review and data checking of this paper prior to submission and publication.
Availability of Data and Materials
Not available.
Code Availability
Not available.
Funding
This project was completed as part of Dr. Andrea Garcia’s work as a fellow at the National Clinician Scholars Program at UCLA.
Author information
Authors and Affiliations
Contributions
A.N.G. conceptualized the fellowship thesis for the National Clinician Scholars Program at UCLA, which included the study design, community engagement protocol, and preparation of the initial paper. A.V-M. and A.M-H. assisted A.N.G. in the thesis project and preparation of the initial/preliminary paper. L.V.S. organized and operationalized the data collection protocol and field work. K.W. and MS.V.H. served as A.N.G.’s fellowship advisors and helped in the planning of the overall project including mobilization of university resources. In the latter stages of the project, L.F. finalized the design of the analysis plan, performed several of the model analyses, assisted with the interpretation of the data, and helped draft the methods and tables for the final paper. P.L.C. also assisted with the design of the analysis plan, interpreted the data, and drafted one of the initial versions of the paper. T.K. served as an advisor to A.N.G. during her fellowship. He helped conceptualize and operationalize of the overall study design, provided institutional resources to assist with data collection and analysis, gave input on the interpretation of the data, and revised the paper critically for intellectual content. All authors participated in the writing of the article and approved the final version for publication.
Corresponding author
Ethics declarations
Ethics Approval
All study protocols and materials were reviewed by the University of California, Los Angeles and the Los Angeles County Department of Public Health Institutional Review Boards. The study received exempt status in accordance with the Common Rule, Title 45, Part 46 of the Code of Federal Regulations.
Consent to Participate
For the survey and the community forum, implied and verbal consent, respectively, were obtained from all study participants.
Consent for Publication
Not available.
Competing Interests
The authors declare no competing interests.
Disclaimer
The content of or any views expressed in this paper are those of the authors and do not necessarily reflect the opinion(s) or the position(s) of the National Clinician Scholars Program, the University of California, Los Angeles, the Los Angeles County Departments of Mental Health and Public Health, or any agencies/organizations mentioned in the text.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garcia, A.N., Venegas-Murrillo, A., Martinez-Hollingsworth, A. et al. Patterns of Health Care Access and Use in an Urban American Indian and Alaska Native Population. J. Racial and Ethnic Health Disparities 11, 1478–1488 (2024). https://doi.org/10.1007/s40615-023-01624-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01624-3