Abstract
The purpose of this study is to identify statistically distinguishable trajectories of childhood body mass index (BMI), an important indicator of developmental status of children, and to provide a summary description of demographic characteristics of children based on these distinctive trajectories. Using data from the Healthy Communities Study (HCS), a large longitudinal dataset with oversamples of Hispanic and Black children across 130 communities in the USA, a group-based trajectory analysis approach was used to estimate trajectories of children based on their BMI-z scores. The three most distinguishable BMI trajectory groups identified for the HCS children show no marked increase or decrease in standardized BMI over an age range of 2 to 11. Approximately 28.5% of children were in a trajectory group with consistently obese BMI-z scores for their sex and age. The patterns of BMI trajectory groups identified for boys and girls are similar, but BMI-z scores for boys tend to be slightly higher than those for girls. These BMI trajectories are characterized by racial/ethnic and socioeconomic status disparities. Hispanic and Black children were more likely to be in the obese trajectory group than White children. Children with parents having less education, or children from low family income level, were more likely to be in the obese trajectory group than counterpart children. The findings suggest that BMI disparities exist from the early years of childhood and persist across childhood, with higher BMI associated with Black and Hispanic children as well as those from low socioeconomic status backgrounds.
Similar content being viewed by others
Introduction
Childhood obesity is a major public health concern in the USA with 19.3% of children and adolescents aged 2–19 years being obese in 2017–2018 [1]. It has been a consistent concern both before and during the COVID-19 pandemic [2]. Obesity can affect children’s psychological well-being as well as physical health. Children who have obesity are also more likely to become adults with obesity [3,4,5]. Adult obesity is associated with increased risk of several serious health conditions including heart disease, type 2 diabetes, and cancer [6, 7]. As such, childhood obesity has long-term negative health and quality of life consequences. The prevalence of obesity increased in children from the early 1960s through the late 2010s and has plateaued at an alarmingly high level [1, 8, 9].
Data from the National Health and Nutrition Examination Survey (NHANES) in 2017–2018 revealed the prevalence of obesity to be higher among children aged 6–11 years (20.3%) and adolescents aged 12–19 years (21.2%) compared with children aged 2–5 years (13.4%) [1]. The prevalence of obesity among non-Hispanic Black (24.2%) and Hispanic (25.6%) children and adolescents aged 2 to 19 years was higher than the prevalence among both non-Hispanic White (16.1%) and non-Hispanic Asian (8.7%) children and adolescents. In general, boys had a higher obesity prevalence (20.5%) than girls (18.0%). But the prevalence by sex varied when it was broken down by race/ethnicity. For boys, obesity prevalence was higher for Hispanic boys (28.1%) than for non-Hispanic Black boys (19.4%); for girls, it was higher for non-Hispanic Black girls (29.1%) than for Hispanic Black girls (23.0%). Obesity prevalence was lower for non-Hispanic White boys (17.4%) and non-Hispanic White girls (14.8%). Although these results shed light on the racial/ethnic disparities in obesity prevalence, the results are based on an analysis of cross-sectional body mass index (BMI) data using a variable-oriented statistical approach. In the present study, a person-oriented approach is applied to a rich longitudinal data set to estimate distinctive BMI trajectories based on the group membership, which contributes to providing a more comprehensive understanding of childhood obesity trajectories and their characteristics.
The relationships between childhood obesity and socioeconomic status are not entirely simple to understand. Based on the NHANES data between 2011 and 2014 [10], obesity prevalence increased in all subgroups examined as head of household education decreased. For the income group comparison, however, the pattern was complex. Obesity prevalence was lower in the highest income group (defined as > 350% of federal poverty line) among non-Hispanic White girls, Hispanic boys, and Hispanic girls, compared with the other income groups. But that was not the case among non-Hispanic Black girls, non-Hispanic Black boys, or non-Hispanic White boys. That is, the obesity prevalence among them was similar regardless of income groups. Similarly, other studies [11, 12] using various data sets have shown obesity continues to be highly prevalent among low socioeconomic status and non-Hispanic/non-White racial/ethnic groups, but the patterns seem to vary across subgroups.
These data trends from the previous studies are derived from aggregating information from cross-sectional data, providing an important snapshot of how different age groups during childhood fare in their BMI distribution in a given time period. However, given childhood obesity has long-term impacts, following the same children longitudinally to characterize distinct groups of BMI trajectories is needed to provide useful insights as to who is in certain BMI trajectory groups and what characteristics distinguish these groups. A better understanding of characteristics related to these developmental trajectories during childhood provides a fundamental step toward building long-term health intervention programs with the implications of improved life course outcomes. Therefore, a person-oriented approach used in the present study, in contrast to a variable-oriented approach, may prove more useful for identifying effective intervention strategies for targeted groups.
Past studies using nationally representative US longitudinal cohort data from the Early Childhood Longitudinal Study (ECLS) have shown racial/ethnic disparities and socioeconomic factors in childhood BMI growth curves [13,14,15]. The primary findings are based on two cohorts: the ECLS-Birth Cohort and the ECLS-Kindergarten Class of 1998–99. The findings showed Hispanic and Black children compared to White and Asian children are at risk of being overweight or obese. Notably, Hispanic boys and Black girls had unfavorably higher BMI and obesity rates, compared to their White and Asian counterparts. These disparities related to weight status and growth trends are characterized by the earliest adiposity reboundFootnote 1 at around age 5 and steeper BMI growth velocity [13]. Low household socioeconomic status and household income had significant associations with high BMI and obesity. The findings from the ECLS data also revealed US children have relatively higher mean BMIs than those standards set by the Centers for Disease Control and Prevention (CDC) and the World Health Organization [13]. In the study using the ECLS-Birth Cohort, the conclusion was that disparities in children’s weight status were already present at 24 months and progressed through kindergarten entry [14]. While these previous longitudinal studies have provided important information on weight status and time/age trends in relation to their race/ethnic characteristics and socioeconomic measures, the studies’ estimates were based on the multilevel modelling framework where repeated BMI measures over time are nested within each child [17].
It is more informative, however, to group children based on their BMI trajectories, then examine and compare their characteristics among the trajectory groups. These trajectories can provide information on (1) how BMI levels change throughout childhood and (2) what child-level demographic and socioeconomic characteristics are associated with these longitudinal trajectories. Such information provides important long-term implications because childhood obesity links to adulthood obesity and its related health consequences [3,4,5]. A better understanding of the BMI trajectories and their associated groups could also inform intervention strategies to mitigate the risks associated with unhealthy weight trajectories during childhood, which is of paramount importance for the prevention or reduction of future chronic disease burdens.
The main purpose of this study is to identify distinctive group trajectories of childhood BMI, an important indicator of developmental status of children, and to provide a summary description of demographic characteristics of children based on their BMI trajectories. In contrast to previous studies, the present study uses a longitudinal childhood BMI dataset covering an age range between 2 (when BMI measure can be applied) and 11 (when early adolescence starts) and a person-oriented approach to estimate distinct BMI trajectories based on group membership. Notably, this study uses data from the national Healthy Communities Study (HCS), which contains a rich sample of US children from diverse racial, ethnic, and socioeconomic backgrounds. Capitalizing on the rich diversity in the HCS, follow-on univariate and multivariate analyses were conducted on these distinctive groups to understand what demographic and socioeconomic characteristics account for their distinctiveness.
Methods
Data
The HCS, implemented from 2013 to 2015, collected contemporary and historical data from 5138 children aged 4–15 and their parent/guardian from 130 study communities selected from a probability-based sample of census tracts (N = 102) and a certainty sample of communities known to have promising programs and policies targeting childhood obesity (N = 28). The study goal was to assess relationships between children’s BMI, dietary and physical activity behaviors, and characteristics of community programs and policies (CPPs) targeting childhood obesity [18]. Communities that participated in the HCS were diverse with respect to geographic region (42.3% South, 22.3% West, 20.0% Midwest, 15.4% Northeast); urbanicity (38.5% urban, 38.5% suburban, 23.1% rural). Although the study was not designed to be nationally representative, the sample design included an oversample of census tracts with a large proportion of non-Hispanic Black (26.2%), Hispanic (32.3%), and low-income residents (38.5%). Data were collected in a total of 438 schools: 227 elementary (52%), 53 elementary/middle (12%), and 158 middle schools (36%). The study recruited from area schools (one to two elementary and one to two middle schools per community). In each community, children attending the selected schools were given interest forms that asked parents/guardians to indicate whether they were interested in participating in the study. The information collected from the interest forms was compiled and used as the sampling frame for recruiting families. Children who were institutionalized or non-ambulatory, or whose families lived in the community for less than 1 year, were excluded. Eligible children were recruited following a stratified random selection process that maintained maximum balance among gender, grade, and race/ethnicity for each community, selecting one child per household. Data on 5138 child/parent pairs (children aged 4–15) were collected from home visits by trained field data collection personnel during 2013–2015. The HCS was approved by Battelle’s institutional review board. Detailed descriptions of the sample can be found elsewhere [18, 19].
Medical Chart BMI Data
To develop a longitudinal history of BMI via medical record review and current anthropometric assessments (height, weight, BMI), a medical release form was signed by a subsample of participant families in the study to obtain retrospective BMI data from medical record review.
The height, weight, and BMI measurements collected from the in-person household visit (n = 3317 children with one data point per child) were appended to the data abstracted from the medical charts (n = 50,728 data points from n = 3317 children; multiple data points per child were available for age, weight, and height) resulting in a total of 54,045 initial data points for 3317 children. Because such abstracted, uncleaned longitudinal growth data are subject to recording errors or inconsistencies, a series of data cleaning steps were performed in the present work to detect and correct or remove those problems. The data cleaning steps employed in this secondary analysis study build on those implemented in prior HCS work [20]. First, records with negative ages or missing ages were removed, as well as subsequent records that were exact duplicates of a previous record. Height data and weight data were then examined separately for outliers, respectively. LOESS models and statistical process control with quantile regression were used to obtain fitted values and to identify outliers. Records were eliminated for a child if the records were major deviations from the series of other records for the child. If nearly all values were outliers or were corrected for a child, the child was excluded from analysis. Additional data cleaning steps were applied to resolve issues including potential data entry errors and inconsistent unit conversions (e.g., lb to kg for weight), which are common issues found in longitudinal chart abstraction. During this robust data quality control process, 20,911 data points for height or weight or both were dropped due to missing or negative ages, duplicate data, missing data, or outliers, resulting in a longitudinal medical chart BMI dataset containing a total of 29,817 data points for 3220 children. Demographic differences were minimal between those who were included in the final longitudinal medical chart BMI dataset versus those who were excluded. There were no significant differences by sex, family income less than $35 K, or maximum parent education; however, non-Hispanic White children were more likely to be included than non-Hispanic Black and Hispanic children, and those with family income greater than $100 K were more likely to be included than those with family income less than $20 K.
For this trajectory analysis, the longitudinal medical chart BMI dataset was merged with the data collected from the in-person household visit. Age was defined in years. For children with more than one BMI for a given age, the median BMI value at that age was used. Age range was restricted to between 2 and 11 for reliable estimates because a BMI z-score is not applicable to children younger than age 2 and few cases were available for ages older than 12. Trajectory analysis was only applied for children having at least 3 BMI records (mean ± SD: 4.9 ± 1.7). The final BMI trajectory analysis consisted of 2198 children aged 2–11 with 10,729 data points. This secondary analysis study was reviewed by the University of Michigan Institutional Review Board and the Battelle Memorial Institute Institutional Review Board.
Measures
For this descriptive trajectory analysis, major demographic measures were included to summarize the characteristics of the trajectories identified by the model: sex (boy; girl), race/ethnicity (White (non-Hispanic), Black (non-Hispanic), Hispanic, other (non-Hispanic), unknown/missing), parent education (less than high school, high school/some college, college, post college), family income (less than $20 K through greater than $100 K in 6 categories), and parent employment status (not employed, employed full- or part-time). These demographic variables were created from the data collected from home visits by in-person interviews between 2013 and 2015.
Obesity is most commonly defined by BMI. As a simple measure calculated as weight in kilograms divided by height in meters squared (kg/m2), BMI is used to classify obesity among adults, and is recommended for use with children and adolescents as well. The cutoff criteria for obesity classification among children are based on the sex-specific BMI-for-age CDC Growth Charts for the USA in the year 2000. Based on recommendations from expert committees, obesity in children and adolescents was defined as a BMI greater than or equal to the age- and sex-specific 95th percentile (equivalent to BMI z-score ≥ 1.645) while overweight [21] was defined as a BMI between the 85th and 95th percentiles (equivalent to 1.036 < BMI z-score < 1.645) of the 2000 CDC Growth Charts [21].
Using the HCS data on height and weight, BMI and BMI-z scores were calculated from the 2000 CDC Growth Charts. Despite its wide use, BMI z-score has been criticized as inaccurate for BMIs of 97th percentile or greater [22]. In response to this limitation, an extended BMI-z score was proposed [23], which used data that combined children with obesity in the CDC Growth Charts and more recent NHANES surveys to increase the sample size. Estimation of z-scores for very high BMIs was based on actual data from children with high BMIs. Because of its construction, the extended BMI-z score corresponds with current cutpoints for overweight and obesity. Because the HCS children were slightly heavier than the national population [9], our analyses also used extended BMI-z scores in addition to the standard BMI-z scores to provide a robust check of the data analysis.
Data Analysis
A linear trajectory analysis approach [24, 25] was used to estimate trajectories of children based on their BMI-z scores calculated from the 2000 CDC Growth Charts [21]. This semi-parametric group-based modeling approach is intended to focus on the development of “person-based” approaches to analyzing developmental trajectories [24,25,26]. This approach assumes a mixture of distinct groups defined by their developmental trajectories within the target population. By identifying groups of individuals with similar trajectories, the group-based trajectory method provides a valuable tool for summarizing and communicating complex patterns in longitudinal data [21]. Stata version 15 was used to estimate the models and graphically depict the trajectories [27]. The dependent variable was BMI-z score. BMI-z scores were computed at different ages for each child, ranging from 2 to 11 years of age.
The model included age entered as an independent variable matched at each BMI measure. Missing data was handled using full information maximum likelihood estimation. Goodness of model fit was assessed by the Bayesian information criterion (BIC). A series of group-based trajectory models were evaluated ranging from two to five trajectory groups using the complete sample as well as separate models for girls and boys. This process established the optimal number of trajectory groups.
Based on the selected trajectory groups, chi-square analyses were used to examine the differences among the identified trajectory groups in terms of demographic and socioeconomic characteristics. Generalized ordinal logistic regression analyses were also performed to examine the combined association of these characteristics on group membership. Odds ratios (ORs) and 95% confidence intervals were estimated.
Results
A three-trajectory model was selected from the linear trajectory analysis using BMI-z scores over the age span of 2–11. The optimal model was identified on the basis of a large BIC statistic and interpretability of the distinctive trajectories [24].
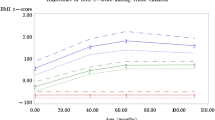
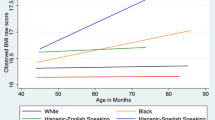
As Fig. 1 shows, each of these BMI-z score trajectories is relatively “flat,” without marked increasing or decreasing trends. These three trajectory groups and accompanying fraction of children within each trajectory group were designated: (1) Lower (25.9%; n = 569), (2) Mid (45.6%; n = 1003), and (3) Upper (28.5%; n = 626). For example, children of the Upper group had high BMI-z scores throughout their developmental period. The same patterns were found for the Mid and Lower groups, which were still within the normal BMI-z category. Using the extended BMI-z scores, the estimated trajectories were almost identical (Lower 24.3%, n = 533; Mid 46.0%, n = 1010; Upper 29.8%, n = 655; figures are not shown). The patterns of three distinct trajectories based on the BMI-z scores for boys and girls were similar, but the BMI-z levels of the Upper and Mid trajectories for boys were slightly higher than for those trajectories for girls (Fig. 2). The BMI-z scores of the Upper trajectory were slightly higher than 2.00 for boys around ages 4–10, whereas they were relatively flat and just below 2.00 for girls across all ages.
Table 1 summarizes demographic and socioeconomic characteristics of children by these three trajectory groups. From separate chi-square analyses, the table shows the Upper BMI-z group consisted of a higher proportion than the expected proportion of Hispanic or Black children; children whose parents had less than a college education; children whose families had an income less than $35 K (all P < 0.001); and children whose parents who were unemployed (P = 0.012). Conversely, the Lower BMI-z group had a higher proportion than the expected proportion of White children or children of another race; children whose parents had a college or post-college education; children whose families had an income greater than $100 K (all P < 0.001); and children who had at least one parent who was employed (P = 0.012). The proportions of boys and girls were more or less equal across these trajectory groups (P = 0.150), although the proportion of boys in the Upper trajectory group was slightly higher than the proportion of girls.
Table 2 reports the results, odds ratios (ORs), and 95% confidence intervals (CIs) of the ordered logistic regression analyses using these same characteristics as predictors of BMI trajectories, except for parent employment, across participants aged 2–11. Parent employment was dropped because it was not a statistically significant predictor in the model (P = 0.573 using BMI-z score) and because it had missing values on about 13% of children. The estimates compared results from these four separate models using the following independent variables: (1) BMI-z scores; (2) extended BMI-z scores for combined boys and girls; (3) BMI-z scores for boys; and (4) BMI-z scores for girls. One of the assumptions for ordered logistic regression, the proportional odds/parallel-lines assumption, is that the relationship between each pair of outcome groups (i.e., Upper trajectory vs. Mid/Lower trajectories and Lower trajectory vs. Mid/Upper trajectories) is the same. This assumption was not always met in our data. For example, when the model was fit using the data for all children combining boys and girls, three categories of race/ethnicity, and one category of parent education the model did not meet the assumption. In that case, generalized ordered logistic regression was used, which relaxes the assumption only on those predictors that did not pass the assumption test, allowing estimation of different ORs for group comparisons [28, 29]. Because the assumptions were met in most predictor variables across the four models, and because ORs for the predictors that met the proportional odds assumptions are the same between the two sets of group comparisons (i.e., Upper trajectory vs. Mid/Lower trajectories and Lower trajectory vs. Mid/Upper trajectories), Table 2 presents the results only for Upper trajectory vs. Mid/Lower trajectories comparisons. The overall conclusion of the analyses was consistent, however, regardless of the model employed.
The first part of the estimated ORs in Table 2 reports model 1 results using BMI-z scores for all children. For racial/ethnicity characteristics, the proportional ORs of comparing each racial/ethnic group to non-Hispanic White children (reference group) on the trajectory membership are reported, given other variables in the model held constant. For non-Hispanic Black children, the odds of being in the Upper trajectory versus the Mid/Lower trajectory were 2.04 times higher than for non-Hispanic White children (P < 0.001), holding the other variables constant. For Hispanic children, the odds of being in the Upper trajectory versus the Mid/Lower trajectory were 2.16 times higher than for non-Hispanic White children (P < 0.001), holding other variables constant. For children in the non-Hispanic Other racial category, the odds were 1.64 times higher than for non-Hispanic White children (P = 0.026). In terms of parent’s education, for children whose parents had a college or post-college education, the odds of being in the Upper trajectory versus the Mid/Lower trajectory were 0.69 times (P = 0.010) and 0.64 times lower (P = 0.014), respectively, than for children whose parents had less than a high school education (reference group), holding other variables constant. For children whose family income level was greater than $100 K, compared to those whose family income was less than $20 K (reference group), the odds were significantly lower (OR = 0.64, P = 0.008). The odds of being in the Upper trajectory versus the Mid/Lower trajectory were 0.84 times lower for girls than for boys (P = 0.032), holding the other variables constant.
Because the HCS children were slightly heavier than the national population [9], trajectories were also estimated using the extended BMI-z in model 2. Results from both the regular and extended measures were very similar, and only 71 children changed their trajectory group membership in the extended BMI-z analysis compared to the standard BMI-z analysis. The results of the ordered logistic regression based on the extended BMI-z were similar to the results based on the standard BMI-z, but the odds associated race/ethnicity categories were slightly lower for the extended BMI-z than the odds associated race/ethnicity categories for the standard BMI-z as reported in Table 2. The odd ratio of being in the Upper trajectory versus the Mid/Lower trajectory for Other racial category compared to non-Hispanic White children was not statistically significant.
Additional analyses were conducted separately for boys and girls in model 3 and model 4 to determine whether there were any notably different patterns between boys and girls in terms of demographic and socioeconomic status associations with the trajectories. The results show that although racial/ethnic characteristics were statistically significantly associated with trajectories for both boys and girls, the degree of association was lower for girls, with statistical significance not always observed. For boys, the odds of being in the Upper trajectory versus the Mid/Lower trajectory were higher for non-Hispanic Black or Hispanic boys than for non-Hispanic White boys (ORs = 1.70 and 1.80, P = 0.011 and P < 0.001, respectively). For girls, however, the odds of being in the Upper trajectory versus the Mid/Lower trajectory were higher only for Hispanic girls than for non-Hispanic White girls (OR = 1.41, P = 0.046). For boys with parent education of college or post-college, compared to boys with parent education less than high school education, the odds of being in the Upper trajectory were significantly lower (OR = 0.60, P = 0.013 and 0.56, P = 0.024, respectively). But for girls, the odds of being in the Upper trajectory were significantly lower for girls with parents who had an education of high school or some college than for girls with parents who had less than a high school education (OR = 0.70, P = 0.037). For the family income factor, the odds of being in the Upper trajectory were significantly lower (OR = 0.52, P = 0.006) for girls from the highest family income level compared to girls from the lowest family income level. No statistically significant association was found with family income for boys.
Discussion
Using longitudinal data collected from early childhood through the beginning of adolescence, the goal of the present study was to characterize distinctive childhood BMI trajectories and to describe how the trajectories are characterized by their race/ethnicity and socioeconomic factors. This study provides insights into subgroups that are meaningfully distinctive in their BMI trajectories and the related characteristics that persist throughout the critical period of development and may subsequently determine children’s healthy or unhealthy weight paths. This person-based approach is useful in identifying distinctive subgroups and understanding factors accounting for their distinctiveness. Such information may provide a basis for developing more targeted intervention programs and for testing the effects of the targeted programs.
Previous longitudinal studies [13,14,15] based on growth curve analyses found similar patterns of racial/ethnic disparities in children’s development of obesity starting in early ages. Those studies estimated BMI trajectories by racial/ethnic groups. Our analyses, however, identified groups of children who shared distinctive developmental trajectories for BMI-z. Follow-on analyses then revealed who these children were in terms of their characteristics. This person-based approach provides information about (a) distinctive trajectories (obese or normal) and (b) characteristics of group membership. Therefore, while similar trajectory patterns and conclusions can be drawn from the results obtained using two different approaches, i.e., variable-based and person-based approaches, the present study provides additional information to form a more comprehensive picture of BMI trajectories in childhood. Based on the person-based approach, our key findings can be summarized in the following manner: (a) one of the BMI trajectories remained in the obese category group consistently from early childhood through the beginning of adolescence, and (b) children in the obese trajectory group were characterized by racial/ethnic and low socioeconomic status backgrounds. These findings help identify target populations for intervention strategies.
Notably, the BMI trajectories identified in this study do not markedly increase or decrease over age. The trajectories include groups of children who stayed in the obese category, and who stayed in two normal categories between ages 2 and 11. Taken collectively, the HCS children maintained their BMI trajectory group membership from early childhood through the beginning of adolescence. Alarmingly, the Upper trajectory group fell in the obese category and was consistently high without any markedly increasing or decreasing trend. The Upper trajectory did not cross or overlap with the Mid or Lower trajectories. Even more concerning, this study found membership in the Upper trajectory was highest among low-socioeconomic status and non-Hispanic Black and Hispanic children. This means that the unhealthy BMI status of HCS children was established at an early age, continued in that unhealthy BMI category across childhood, and was characterized by racial/ethnic disparities and low socioeconomic status backgrounds.
Previous studies using longitudinal data estimating growth curves also concluded that racial/ethnic disparities in US children’s weight status and growth curves emerge at different ages for different racial groups, and the disparities are generally well established by kindergarten age [13,14,15]. In particular, a study by Isong and colleagues using the ECLS-Birth Cohort from age 9 months through kindergarten age concluded that disparities in children’s weight status were already present at 24 months and progressed through kindergarten entry [14]. Specifically, their findings showed that mean BMI z-scores for Hispanic boys at 24 months and for Black girls at 36 months were significantly higher than their White counterparts, and those trends continued. Their findings provided valuable insights into obesity trends for particular racial/ethnic subgroups by boys and girls.
Our findings provide a comprehensive picture of childhood BMI trajectories based on group membership. The Upper, obese, trajectory group included not just Hispanic (56.4%) and Black (17.4%) children, but also White children (17.9%) and children of “Other” racial group (5.9%). The Upper trajectory group was mostly characterized by low socioeconomic status. This means that although significant proportions of Hispanic and Black children are at risk of having a distinct obesity trajectory from early age through early adolescence, a non-insignificant proportion of White children are at risk as well. They are likely from low socioeconomic status backgrounds. An additional analysis was conducted to show that disproportionately higher fractions of White children in the Upper obese trajectory group were from lower levels of parent education and family income (results not shown). As such, the value of our approach and findings is that both are “group-person” focused, which may be more informative in identifying targeted children groups based on their trajectories and in distinguishing them with their specific subgroup characteristics.
Additionally, the present study used longitudinal data covering ages 2 through 11, which revealed that while HCS children developed their obese BMI trajectory as early as ages 2–3, the trajectories of HCS children continued through early adolescence, maintaining similar levels of BMI z-scores. While previous studies using ECLS cohorts were also longitudinal data, theirs included data from two different cohorts: ECLS-Birth Cohort which include children ages 9 months through kindergarten or ECLS-Kindergarten which included children from kindergarten to middle school [13,14,15].
Therefore, the findings from the present study, which are based on the rich longitudinal data from HCS using a person-oriented approach, not only provide an important confirmation of the evidence of early emergence as well as persistence of a BMI disparity throughout early adolescence, but also provide a comprehensive understanding toward a targeted obesity prevention strategy. Future studies that help identify distinct groups of BMI pathways throughout the life course would be informative to understand who remains obese throughout their adulthood, and who and when, if applicable, becomes obese later in their life.
Note that the use of extended BMI-z scores did not change the conclusions in the present study. Although the HCS children were slightly heavier than the national population [1], the extended measure incorporating more recent NHANES surveys to increase the sample size did not influence our results significantly. An additional analysis was conducted to examine the extent of the changes in the BMI-z scores compared to the extended BMI-z scores. About 34% of children (754 from 2198 children) had changes in at least one BMI-z score value when comparing standard BMI-z score values to extended BMI-z scores values, but only 71 children from the data changed their trajectory group membership in the extended BMI-z analysis as compared to the standard BMI-z analysis.
Previous research has reported childhood obesity predicts obesity in adulthood [3,4,5], and thus there are long-term, potentially life-long health implications, particularly for the children of the Upper trajectory group with the high BMI-z scores. Since obesity disparities are associated with multiple factors, from biological, social, psychological, and behavioral, to geographic and social-environmental, it may also mean intervention strategies for healthy weight need to be multi-faceted and start as early as possible. Application of a life course approach [30] to the findings yields a combined view of the critical-period model and the accumulation-of-risk model. Such an approach could target a range of specific factors such as physical growth, social mobility, physical environment, and behavior changes with the emphasis on the timing of risk exposure. Our findings support the observation that developmental trajectories of children’s BMI start early and do not change course significantly. Because the current study is mainly descriptive using a limited number of demographic and socioeconomic characteristics, investigation of other potential factors underlying the complex mechanism lies beyond the scope of the current study goal. However, the information about these trajectories can identify subgroups that share these particular characteristics (e.g., non-Hispanic Black and Hispanic boys, children whose parents have less than college education), which could be useful in developing more targeted intervention programs. It may be that interventions that introduce protective factors at a very early age could help alleviate obesity risk in children, as well as help alleviate risk factors accumulating throughout childhood. Future research can expand to incorporate more extensive personal or environmental risk and protective factors that may further delineate their BMI trajectories.
Two important limitations of the present work are noted. First, the presented results might be limited in their generalizability to the national population due to the sampling design being based on the community characteristics and the inclusion of higher proportions of Hispanic children in the HCS. This does not, however, change the interpretation of the findings that children maintained their BMI trajectory group membership from early childhood through the beginning of adolescence. Second, although BMI was based on objective measurements, reporting errors may have been present such as confounding units of measure. This is not an uncommon problem in longitudinal BMI datasets. In the present work, a series of established steps were undertaken to ensure a robust longitudinal data set.
Overall, these results provide insights into childhood obesity trends that point to pathways determined early in life. The three most distinguishable trajectory groups identified for the HCS children showed no marked increase or decrease in standardized BMI over an age range of 2 to 11. One of the trajectory groups consisted of nearly 30% of children whose BMI-z scores were categorized as obese. While the patterns of BMI trajectory groups identified for boys and girls were similar, BMI-z scores for boys tended to be slightly higher than for girls. These BMI trajectories were characterized by racial/ethnic and socioeconomic status disparities. The findings suggest that BMI disparities exist from the early years of childhood and persist across childhood, with higher BMI associated with non-Hispanic Black and Hispanic children and those who are from low socioeconomic status backgrounds. Study findings underscore the importance of longitudinal data of BMI history. Findings also highlight the importance of investigating the role of specific risk and protective factors at early ages so as to further understand, strategize, and implement policies that can impact the health of children over their life course. Future studies involving sub-populations of increasing or decreasing BMI trajectories might provide information on potential differences in risk and protective factors to inform intervention programs.
Notes
The adiposity rebound is the second rise in adiposity, body fatness, as measured by BMI, which occurs between 5 and 7 years of age [16]. Typically, BMI increases during the first year of life, then subsequently decreases and reaches a nadir at around 6 years of age.
References
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats. 2020.
Lange SJ. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years — United States, 2018–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1278–1283. https://doi.org/10.15585/mmwr.mm7037a3
Krueger PM, Reither EN. Mind the gap: race\ethnic and socioeconomic disparities in obesity. Curr Diab Rep. 2015;15(11):95.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17(2):95–107.
Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. 2017;377(22):2145–53.
De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. J Obes. 2013;2013: 291546.
Dehghan M, Akhtar-Danesh N, Merchant AT. Childhood obesity, prevalence and prevention. Nutr J. 2005;2(4):24.
Sanyaolu A, Okorie C, Qi X, Locke J, Rehman S. Childhood and adolescent obesity in the United States: a public health concern. Glob Pediatr Health. 2019;6:2333794X19891305. https://doi.org/10.1177/2333794X19891305
Ogden CL, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8.
Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, Li X, et al. Prevalence of obesity among youths by household income and education level of head of household — United States 2011–2014. Morb Mortal Wkly Rep. 2018;67(6):186–9.
Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev. 2016;17(3):276–95.
Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early life risk factors for childhood obesity. Pediatrics. 2010;125(4):686–95. https://doi.org/10.1542/peds.2009-2100
Min J, Wen X, Xue H, Wang Y. (2018) Ethnic disparities in childhood BMI trajectories and obesity and potential causes among 29,250 US children: Findings from the Early Childhood Longitudinal Study-Birth and Kindergarten Cohorts. Int J Obes. 2005;42(9):1661–70.
Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865.
Guerrero AD, Mao C, Fuller B, Bridges M, Franke T, Kuo AA. Racial and ethnic disparities in early childhood obesity: growth trajectories in body mass index. J Racial Ethn Health Disparities. 2016;3(1):129–37.
Rolland-Cachera MF, Deheeger M, Bellisle F, Sempé M, Guilloud-Bataille M, Patois E. Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr. 1984;39(1):129–35.
Curran PJ, Obeidat K, Losardo D. Twelve frequently asked questions about growth curve modeling. J Cogn Dev Off J Cogn Dev Soc. 2010;11(2):121–36.
Arteaga SS, Loria CM, Crawford PB, Fawcett SB, Fishbein HA, Gregoriou M, et al. The Healthy Communities Study: its rationale, aims, and approach. Am J Prev Med. 2015;49(4):615–23.
Strauss WJ, Sroka CJ, Frongillo EA, Arteaga SS, Loria CM, Leifer ES, et al. Statistical design features of the Healthy Communities Study. Am J Prev Med. 2015;49(4):624–30.
Strauss WJ, Nagaraja J, Landgraf AJ, Arteaga SS, Fawcett SB, Ritchie LD, et al. The longitudinal relationship between community programmes and policies to prevent childhood obesity and BMI in children: the Healthy Communities Study. Pediatr Obes. 2018;13(Suppl 1):82–92.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190.
Freedman DS, Davies AJG, Kompaniyets L, Lange SJ, Goodman AB, Phan TLT, et al. A Longitudinal comparison of alternatives to body mass index Z-scores for children with very high body mass indexes. J Pediatr. 2021;235:156–62.
Wei R, Ogden CL, Parsons VL, Freedman DS, Hales CM. A method for calculating BMI z-scores and percentiles above the 95th percentile of the CDC growth charts. Ann Hum Biol. 2020;47(6):514–21.
Daniel S. Nagin. Group-based modeling of development: Harvard University Press; 2005.
Nagin DS. Group-based trajectory modeling: an overview. Ann Nutr Metab. 2014;65(2–3):205–10.
Bergman LR. A pattern-oriented approach to studying individual development: snapshots and processes. In R. B. Cairns, L. R. Bergman, & J. Kagan (Eds.), Methods and models for studying the individual (pp. 83–122). Sage Publications, Inc.
StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017.
Williams, R. Generalized Ordered Logit/Partial Proportional Odds Models for Ordinal Dependent Variables. The Stata Journal. 2006;6(1):58–82. https://doi.org/10.1177/1536867X0600600104
Williams R. Understanding and interpreting generalized ordered logit models. J Math Sociol. 2016;40(1):7–20.
Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–93.
Funding
Research reported in this manuscript was supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH) under award number R01HL137731. The original Healthy Communities Study was funded by the NHLBI, in collaboration with the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Diabetes and Digestive and Kidney Diseases, National Cancer Institute, and Office of Behavioral and Social Sciences Research, under award number HHSN268201000041C. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data cleaning, and analysis were performed by Hyoshin Kim and Alisha Rajbhandari. The first draft of the manuscript was written by Hyoshin Kim, and all authors commented on subsequent versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was reviewed by the Battelle Institutional Review Board and received the status of exemption. The study was also reviewed and approved by the University of Michigan Intuitional Review Board.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Classification Code
MSC= 62P25 Application of Statistics to Social Sciences.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, H., Rajbhandari, A., Krile, R. et al. Body Mass Index Trajectories among the Healthy Communities Study Children: Racial/Ethnic and Socioeconomic Disparities in Childhood Obesity. J. Racial and Ethnic Health Disparities 11, 203–215 (2024). https://doi.org/10.1007/s40615-023-01511-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-023-01511-x