Abstract
Background
The purpose of this study was to estimate COVID-19 vaccination rate among Medicare beneficiaries with cancer history and determine whether COVID-19 vaccine uptake is higher among non-Hispanic White beneficiaries compared with racially and ethnically minoritized beneficiaries.
Methods
We used US representative, cross-sectional data from the Medicare Current Beneficiary Survey COVID-19 Winter 2021 Rapid Response Community Supplement Survey. A total of 1,863 respondents with self-reported cancer history (other than skin cancer) were included. The outcome was self-reported receipt of at least one coronavirus vaccine dose since vaccines became available. The key independent variable of interest was self-reported race and ethnicity. We applied sample weights to account for the survey design and provide population estimates to 9.6 million beneficiaries with cancer history. Weighted descriptive statistics and multivariable logistic regression analyses were conducted.
Results
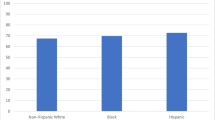
During the first 4 months of vaccine availability, 69.6% of beneficiaries received at least one vaccine dose of which 65.4% had two vaccine doses. A larger proportion of non-Hispanic White beneficiaries (71.9%) had at least one vaccine dose compared with non-Hispanic Black (60.4%) and Hispanic (57.4%) beneficiaries. An estimated 30.4% of beneficiaries were still unvaccinated, that represents approximately 2.9 million unvaccinated beneficiaries with cancer history. Hispanic beneficiaries were 42% (OR: 0.58; 95% CI: 0.33–0.99; p = .048) less likely to be vaccinated compared with non-Hispanic White beneficiaries.
Conclusions
Results indicate racial and ethnic differences in vaccine uptake among Medicare beneficiaries with cancer history. Effective strategies are needed to help increase vaccine confidence and uptake among adults with cancer history.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer remains the second leading cause of death in the USA, exceeded only by heart disease[1]. Given the major advances in cancer diagnosis and treatment, currently about 17 million Americans—5% of the total US population, live with a history of cancer diagnosis [1,2,3]. Individuals with a history of cancer diagnosis are considered as a high-risk, high-priority population group for coronavirus disease 2019 (COVID-19) vaccination for both primary and booster vaccinations, due to the fact that high morbidity and mortality of COVID-19 infection were reported among people with cancer history [4]. In fact, 30-day mortality rates of up to 62% have been reported among individuals with both cancer history and COVID-19 infection [5,6,7,8]. Individuals with cancer history and with COVID-19 not only have high mortality rate but also worse health outcomes compared to the general population with COVID-19 [9,10,11,12]. Furthermore, minoritized racial and ethnic groups with cancer history are disproportionately affected by COVID-19 in the USA. In fact, American Indian and Alaska Native, Black, and Latino individuals have substantially higher rates of COVID-19 infection, hospitalization, morbidity, and mortality compared to White individuals in the USA [8, 9, 13,14,15].
Given the high morbidity and mortality of COVID-19 among individuals with cancer history, vaccination is critical for mitigating the impact of the pandemic and its unequal effects on minoritized racial and ethnic groups. Highly effective vaccines against COVID-19 infection that significantly reduce adverse COVID-19-related outcomes are widely available in USA. As of July 2022, about 78% of the US population received at least one dose of COVID-19 vaccine [16,17,18]. Studies among the general population reported lower vaccination rates among minoritized racial and ethnic groups compared with White individuals [16]. While there is strong evidence for racial and ethnic disparities in COVID-19 vaccination uptake among the general population, whether these racial and ethnic differences exist in COVID-19 vaccination rates among adults with cancer history is currently unknown. Thus, the purpose of this study was to estimate COVID-19 vaccination rate among Medicare beneficiaries with cancer history and determine whether COVID-19 vaccine uptake is higher among non-Hispanic White beneficiaries compared with racially and ethnically minoritized beneficiaries using nationally representative, population-based US sample of adults with cancer history.
Methods
Study Data Source
The current study used cross-sectional data from the Medicare Current Beneficiary Survey (MCBS) COVID-19 Winter 2021 Rapid Response Community Supplement Public Use File [19]. The MCBS is a nationally representative sample of Medicare population including beneficiaries aged ≥ 65 and ≤ 64 with certain disabling conditions residing in the USA. The MCBS COVID-19 Winter supplement is a cross-sectional telephone survey that collected data between February 28 through April 25, 2021 on the effects of the COVID-19 pandemic on Medicare beneficiaries. Specifically, it collected information on the availability of telemedicine visits, deferred medical care, social distancing and other preventive health behaviors, COVID-19 testing and vaccination, and other COVID-19 related variables. The MCBS COVID-19 Winter Community Supplement survey was conducted in either English or Spanish. Study participants were existing MCBS beneficiaries living in the community at the time of their interview [19]. The MCBS COVID-19 Winter supplement includes data on 11,107 community-dwelling Medicare beneficiaries weighted to be nationally representative of 57,387,274 beneficiaries enrolled in Medicare at any point in 2020 and continued to be enrolled through winter 2021. The response rate of the MCBS COVID-19 Winter supplement was 79.6%. Additional information about the survey is available elsewhere. Additional information about survey is available at the CMS MCBS website [19].
Study Participants
The MCBS COVID-19 Winter supplement surveyed Medicare beneficiaries either themselves or through proxy respondents. Overall, 2,182 participants self-reported cancer history (other than skin cancer) in the COVID-19 Winter 2021 Supplement. For the current study, we excluded observations responded by proxy (n = 224) and those who had incomplete data (missing values and refused to answer) on income (n = 78), unable to get medical care because of COVID-19 (n = 10), living alone status (n = 1), received vaccine (n = 1), and depression (n = 5). This yielded a final sample size of 1,863 respondents who did not respond by proxy, self-reported cancer history (other than skin cancer) and had complete data points on study variables. We used publicly available data and, therefore, did not require institutional review board approval in accordance with the exempt criteria under 45 Code of Federal Regulations part 46.102 [20].
Study Measures
The outcome variable of interest was a binary indicator of self-reported receipt of at least one vaccine dose since vaccines became available. Participants were asked “Since [DATE of COVID-19 vaccine availability] [have you/has (SP)] had a coronavirus vaccination?” with responses “Yes/No.” The MCBS COVID-19 Winter supplement used a reference date of December 2020 to align with when Emergency Use Authorization was issued. Participants also reported the number of coronavirus vaccination doses they received during the first 4 months of the vaccine availability. Participants were also asked the following question “How many coronavirus vaccination doses [have you/has (SP)] had?” with responses options “One vaccination dose” and “Two vaccination doses.”
The key independent variable of interest was self-reported race and ethnicity that was categorized as non-Hispanic Black, Hispanic, non-Hispanic White, and other that included American Indian or Alaska Native, Asian, Native Hawaiian or other Pacific Islander, two or more races, and unknown races. Based on current literature, a robust set of individual-level covariates that might influence the relationship between race and ethnicity and vaccine uptake were included in this study. The following self-reported covariates were included in the analysis age (65–74 and ≥ 75 years), sex (male and female), annual household income (< $25,000 and ≥ $25,000), residing area (non-metropolitan and metropolitan), US census regions (West, South, Northeast, Midwest), Medicare-Medicaid dual eligibility (no, fully eligible, partially eligible, and qualified Medicare beneficiary (QMB) eligible only), depression history (yes and no), unable to get medical care because of the COVID-19 (yes and no), and living status (not alone and alone).
Statistical Analysis
All statistical analyses were conducted on weighted data. We applied recommended sampling weights to account for the complex survey design provided by the MCBS to generate nationally representative results. Thus, the sample of 1,863 beneficiaries that were included in unweighted sample represent 9,632,778 community-dwelling Medicare beneficiaries with cancer history in the USA. We conducted descriptive statistics including unweighted frequencies, weighted percentages, and 95% confidence intervals (CI) of all variables to describe the study population overall and stratified by race and ethnicity. Weighted simple and multiple logistic regression models were used to evaluate the effect of race and ethnicity on COVID-19 vaccine uptake.
We examined potential of multicollinearity across all covariates before regression analyses with variation inflation factor (VIF). According to the general rule, VIFs exceeding 4 and 10 are warning further investigation and serious multicollinearity, respectively. Since all covariates have very low VIFs (< 1.5), we do not see any considerable multicollinearity in the model. Crude odd ratios (OR), adjusted odds ratio (AOR), and 95% CIs were estimated with 100 balanced repeated replications using Fay’s adjustment of 0.3. A 2-tailed p-value at a 0.05 level was considered statistically significant results. Analyses were conducted using Stata, version 17.0 (StataCorp).
Results
Table 1 presents unweighted frequencies and weighted percentages of sample characteristics. Approximately, 11.0% were younger than 65 years of age and 58.9% were women. The majority (80.2%) self-identified as non-Hispanic White, while 7.1% as Hispanic and 7.0% as non-Hispanic Black and 81.7% were living in Metropolitan areas. During the first 4 months of vaccine availability, 69.6% received at least one vaccine dose of which 65.4% had two vaccine doses (Table 1).
Table 2 presents sample characteristics by race and ethnicity. Compared to non-Hispanic Whites beneficiaries, racial and ethnic minority beneficiaries were more likely to be younger than 65 years of age (p = 0.02), have lower income (< $25,000) (p = < 0.001), report being unable to get medical care due to COVID-19 (p = 0.08), and be full dual or partial dual eligible for Medicare-Medicaid (p = < 0.001). A larger proportion of non-Hispanic White beneficiaries (71.9%) had at least one vaccine dose compared with non-Hispanic Black (60.4%) and Hispanic (57.4%) beneficiaries (p = 0.004) (Table 2). In simple logistic regression (Table 3), compared to non-Hispanic White beneficiaries, non-Hispanic Black (OR: 0.59; 95% CI: 0.38–0.93; p = 0.023) and Hispanic (OR: 0.53; 95% CI: 0.33–0.82; p = 0.006) beneficiaries were less likely to be vaccinated.
Table 3 shows the results of multiple logistic regression model. After adjusting for all covariates in the multiple logistic regression model, Hispanic beneficiaries were 42% (AOR: 0.58; 95% CI: 0.33–0.99; p = 0.048) less likely to be vaccinated compared with non-Hispanic White beneficiaries. No statistically significant difference was observed between non-Hispanic White and non-Hispanic Black beneficiaries. Adjusted for all covariates, Medicare beneficiaries with incomes less than $25,000 were less likely to be vaccinated compared to those with incomes exceeding $25,000 (AOR: 0.58; 95% CI; 0.41–0.80; p < 0.001). Beneficiaries living alone (AOR: 0.64; 95% CI; 0.48–0.84), those who were unable to get medical care (AOR: 0.57; 95% CI: 0.36–0.88; p = 0.012) and had history of depression (AOR: 0.75; 95% CI: 0.56–0.98; p = 0.042) had lower odds of being vaccinated compared to their counterparts. Those living in South were 31% less likely to be vaccinated compared with beneficiaries living in West (AOR: 0.69; 95% CI: 0.50–0.95; p = 0.024) (Table 3).
Discussion
In this paper, we estimate COVID-19 vaccination rate among Medicare beneficiaries with cancer history and determine whether COVID-19 vaccine uptake is higher among non-Hispanic White beneficiaries compared with racially and ethnically minoritized beneficiaries. The findings of this study suggest that during the first four months of the vaccine availability, an estimated 30.4% of beneficiaries were still unvaccinated, that represents approximately 2.9 million unvaccinated community-dwelling Medicare beneficiaries with cancer history. Across racial and ethnic groups, Hispanic beneficiaries had the lowest rate of having at least one vaccine dose followed by non-Hispanic Black beneficiaries. Hispanic beneficiaries were 42% less likely to have at least one vaccine dose compared to White beneficiaries after adjusting for all other factors in the model.
This is in line with previous research conducted among the general population that showed lower vaccination rate among racial and ethnic minority groups compared with White individuals.
As of July 2022, among people who have received at least one vaccine dose, 55% were White individuals, 21% Hispanic, 10% Black, and 7% Asian individuals[16]. However, it is difficult to have direct comparison between the findings of this report and our study because of differences in study population. Nonetheless, recent reviews have documented the various factors that influence rates of vaccine uptake among Black and Hispanic communities, including immigrant communities (which overlaps with Black and Hispanic-identified individuals) [21]. Moreover, even though these groups experienced early disparities in rates of COVID-10 vaccine uptake, there is evidence that they gained ground by the development and implementation locally-grounded, community-based strategies that we were resonant with their culture and responsive to the social and material conditions of their lives [22,23,24].
Our study findings did not show statistically significant difference in vaccination rate between non-Hispanic White and non-Hispanic Black beneficiaries with cancer history in the adjusted regression model which is not consistent with current literature. Thus, future studies are needed with large and diverse sample to explore this relationship comprehensively. The insignificant finding after adjusting for the socio-economic factors may imply that the lower rate of vaccination in non-Hispanic Black beneficiaries could be explained by socio-economic status. Other factors that may explain this finding are participants’ age distribution and Medicare-Medicaid dual eligibility distribution. In our study, non-Hispanic Black individuals were more likely to be younger than 65 years of age compared to non-Hispanic White individuals (16.2% vs. 10.2%). In adjusted model, we found that older individuals were more likely to be vaccinated compared to younger individuals. Future studies with equal distribution by age are needed. By contrast, studies conducted in the general population showed racial and ethnic disparities in vaccination uptake for both Hispanic and Black individuals [17, 25]. Further studies are needed to investigate racial and ethnic differences in COVID-19 vaccination rate among individuals living with cancer history. Better understanding the factors associated with vaccination rate may help to improve the vaccine uptake. Equitable receipt of COVID-19 vaccination among racial and ethnic individuals with cancer history are critical to reduce inequities in COVID-19-related adverse outcomes.
We found a significant impact of socioeconomic markers including income and living alone on vaccination rate among Medicare beneficiaries. Specifically, beneficiaries with cancer history who lived alone and resided in low-income housing were less likely to be vaccinated compared to their counterparts. Our findings are consistent with the fact that individuals with lower income are more likely to be unvaccinated [25,26,27]. In our study, racially and ethnically minoritized beneficiaries were more likely to have lower income compared to White beneficiaries. One explanation of the differences in the vaccination uptake may be that beneficiaries with lower income are more likely to rely on public transportation and have less access to vaccination sites. Increasing the number of vaccinations sites in areas with higher proportion of low income racially and ethnically minoritized groups might help to improve the vaccination uptake in these groups. We also observed lower likelihood of vaccination within Medicare beneficiaries residing within the South. The South is characterized by a differential racial composition that is higher in the proportion of Black and impoverished regions [28]. Given the overlap between these factors, it is not possible to delineate the individual contribution of each to variation in vaccination rates. Lastly, it is possible that geographic variation in political support of vaccination may have resulted in lower vaccination rates within the South. This is consistent with early reports that the geographic distribution of COVID-19 morbidity and mortality were higher in states that did not expand Medicaid under the Affordable Care Act, many of which were states that also had political resistance to public health response measures to minimize viral transmission, such as use of face masks and maintenance of physical distance [29].
The current study has several limitations that need to be acknowledged. The study sample included only community-dwelling Medicare beneficiaries aged 65 years or older and those aged 64 and younger with certain disabling conditions, thus, the results may not be generalized to beneficiaries living in long-term care facilities and to non-Medicare persons with cancer history. We excluded observations completed by proxy which might have an impact on the results. These participants may have more chronic complications of COVID-19 (including cancer) and their demographic and clinical characteristics may be different from the participants who responded by themselves. In addition, majority of the sample were non-Hispanic White (80.2%), therefore, future studies with more diverse and larger sample of individuals with a history of cancer are needed. The data rely on self-reported endpoints and are therefore subject to potential reporting bias and measurement errors. Some important variables were not included in the MCBS COVID-19 Winter supplement surveyed such as education attainment that may have an impact on the outcome of interest, COVID-19 vaccine uptake. The dataset did not include detailed information on the distribution of racial and ethnic participants which is identified as a common limitation when using publicly available survey datasets [30,31,32]. The dataset also did not include other critical confounding factors such as cultural behaviors, perception of health, racism that also contribute to disparity in vaccination uptake. Therefore, future studies with diverse sample and detailed information on race and ethnicity and other critical factors are needed to better understand racial and ethnic variation in vaccine uptake.
Conclusions
In conclusion, large proportion of Medicare beneficiaries with cancer history were unvaccinated. non-Hispanic White beneficiaries had higher rates of vaccination compared to racial and ethnic beneficiaries. Interventions should be developed to optimize vaccine uptake among low-income racial and ethnic individuals with cancer history.
Data Availability
The data that support the findings of this study are openly available in Centers for Medicare & Medicaid Services at https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/MCBS-Public-Use-File.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. https://doi.org/10.3322/caac.21590.
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, et al editors. SEER Cancer Statistics Review, 1975–2011. Bethesda, MD: National Cancer Institute; 2014.
American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2019-2021. Atlanta: American Cancer Society; 2019. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancertreatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2019-2021.pdf.
Fendler A, de Vries EGE, GeurtsvanKessel CH, et al. COVID-19 vaccines in patients with cancer: immunogenicity, efficacy and safety. Nat Rev Clin Oncol. 2022. https://doi.org/10.1038/s41571-022-00610-8.
Saini KS, Tagliamento M, Lambertini M, et al. Mortality in patients with cancer and coronavirus disease 2019: A systematic review and pooled analysis of 52 studies. Eur J Cancer. 2020;139:43–50. https://doi.org/10.1016/j.ejca.2020.08.011.
Kalinsky K, Accordino MK, Hosi K, et al. Characteristics and outcomes of patients with breast cancer diagnosed with SARS-Cov-2 infection at an academic center in New York City. Breast Cancer Res Treat. 2020;182(1):239–42. https://doi.org/10.1007/s10549-020-05667-6.
He W, Chen L, Chen L, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637–45. https://doi.org/10.1038/s41375-020-0836-7.
Wang Q, Berger NA, Xu R. Analyses of Risk, Racial Disparity, and Outcomes Among US Patients With Cancer and COVID-19 Infection. JAMA Oncol. 2021;7(2):220–7. https://doi.org/10.1001/jamaoncol.2020.6178.
Grivas P, Khaki AR, Wise-Draper TM, et al. Association of clinical factors and recent anticancer therapy with COVID-19 severity among patients with cancer: a report from the COVID-19 and Cancer Consortium. Ann Oncol. 2021;32(6):787–800. https://doi.org/10.1016/j.annonc.2021.02.024.
Kuderer NM, Choueiri TK, Shah DP, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907–18. https://doi.org/10.1016/S0140-6736(20)31187-9.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. https://doi.org/10.1136/bmj.m1198.
Chavez-MacGregor M, Lei X, Zhao H, Scheet P, Giordano SH. Evaluation of COVID-19 Mortality and Adverse Outcomes in US Patients With or Without Cancer. JAMA Oncol. 2022;8(1):69–78. https://doi.org/10.1001/jamaoncol.2021.5148.
Gu T, Mack JA, Salvatore M, et al. Characteristics Associated With Racial/Ethnic Disparities in COVID-19 Outcomes in an Academic Health Care System. JAMA Netw Open. 2020;3(10):e2025197. https://doi.org/10.1001/jamanetworkopen.2020.25197.
Lara OD, Smith MJ, Wang Y, et al. Racial disparities in patients with coronavirus disease 2019 infection and gynecologic malignancy. Cancer. 2021;127(7):1057–67. https://doi.org/10.1002/cncr.33335.
Newman LA, Winn RA, Carethers JM. Similarities in Risk for COVID-19 and Cancer Disparities. Clin Cancer Res. 2021;27(1):24–7. https://doi.org/10.1158/1078-0432.CCR-20-3421.
Kaiser Family Foundation (KFF). Based on KFF analysis of vaccinations using the Centers for Disease Control and Prevention, Demographic Characteristics of People Receiving COVID-19 Vaccinations in the United States data and total population data using KFF analysis of the 2019 American Community Survey data. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/. Accessed 30 July 2022.
Siegel M, Critchfield-Jain I, Boykin M, et al. Racial/Ethnic Disparities in State-Level COVID-19 Vaccination Rates and Their Association with Structural Racism. J Racial Ethn Health Disparities. 2021. https://doi.org/10.1007/s40615-021-01173-7.
Agarwal R, Dugas M, Ramaprasad J, Luo J, Li G, Gao GG. Socioeconomic privilege and political ideology are associated with racial disparity in COVID-19 vaccination. Proc Natl Acad Sci U S A 2021;118(33). https://doi.org/10.1073/pnas.2107873118.
Centers for Medicare & Medicaid Services. 2021 Medicare current beneficiary survey COVID-19 winter supplement public use file. (https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/MCBS-Public-Use-File). Accessed 15 Jan 2022.
Department of Health and Human Services. Code of Federal Regulations. Title 45 Public Welfare. Part 46 Protection of Human Subjects. Dep Health Human Serv 2009. Retrieved from https://www.hhs.gov/ohrp/sites/default/files/ohrp/policy/ohrpregulations.pdf.
McFadden SM, Demeke J, Dada D, et al. Confidence and Hesitancy During the Early Roll-out of COVID-19 Vaccines Among Black, Hispanic, and Undocumented Immigrant Communities: a Review. J Urban Health. 2022;99(1):3–14. https://doi.org/10.1007/s11524-021-00588-1.
Demeke J, Ramos SR, McFadden SM, et al. Strategies That Promote Equity in COVID-19 Vaccine Uptake for Latinx Communities: a Review. J Racial Ethn Health Disparities. 2022. https://doi.org/10.1007/s40615-022-01320-8.
Demeke J, McFadden SM, Dada D, et al. Strategies that Promote Equity in COVID-19 Vaccine Uptake for Undocumented Immigrants: A Review. J Community Health. 2022;47(3):554–62. https://doi.org/10.1007/s10900-022-01063-x.
Dada D, Djiometio JN, McFadden SM, et al. Strategies That Promote Equity in COVID-19 Vaccine Uptake for Black Communities: a Review. J Urban Health. 2022;99(1):15–27. https://doi.org/10.1007/s11524-021-00594-3.
Nguyen KH, Anneser E, Toppo A, Allen JD, Scott Parott J, Corlin L. Disparities in national and state estimates of COVID-19 vaccination receipt and intent to vaccinate by race/ethnicity, income, and age group among adults >/= 18 years. United States Vaccine. 2022;40(1):107–13. https://doi.org/10.1016/j.vaccine.2021.11.040.
Hamel L, Lopes L, Sparks G, et al. KFF COVID-19 Vaccine Monitor: September 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-september-2021/view/footnotes/. Accessed 10 Mar 2022.
Hughes MM, Wang A, Grossman MK, et al. County-Level COVID-19 Vaccination Coverage and Social Vulnerability — United States. MMWR Morb Mortal Wkly Rep. 2021;70:431–6.
Pew Research Center. The growing diversity of Black America 2021 https://www.pewresearch.org/social-trends/2021/03/25/the-growing-diversity-of-black-america/. Accessed 30 Mar 2022.
Poteat T, Millett GA, Nelson LE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann Epidemiol. 2020;47:1–3. https://doi.org/10.1016/j.annepidem.2020.05.004.
Hahn RA, Stroup DF. Race and ethnicity in public health surveillance: criteria for the scientific use of social categories. Public Health Rep 1994;109(1):7–15. (https://www.ncbi.nlm.nih.gov/pubmed/8303018).
Krieger N. Refiguring, “race”: epidemiology, racialized biology, and biological expressions of race relations. Int J Health Serv. 2000;30(1):211–6. https://doi.org/10.2190/672J-1PPF-K6QT-9N7U.
Foster MW. Looking for race in all the wrong places: analyzing the lack of productivity in the ongoing debate about race and genetics. Hum Genet. 2009;126(3):355–62. https://doi.org/10.1007/s00439-009-0674-1.
Funding
Dr. Poghosyan is partially funded by the NIH/NCI 5R01CA258269.
Author information
Authors and Affiliations
Contributions
HP designed the study and acquired the data. HP and SJ analyzed the data. HP drafted the article. HP, MAD, GT, LN, and SJ reviewed and revised the article. All authors critically edited the article for intellectual content and approved the final article.
Corresponding author
Ethics declarations
Ethics Approval
We used publicly available data and, therefore, did not require institutional review board approval in accordance with the exempt criteria under 45 Code of Federal Regulations part 46.102.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Poghosyan, H., Dinan, M.A., Tamamyan, G. et al. Racial and Ethnic Variation in COVID-19 Vaccination Uptake Among Medicare Beneficiaries with Cancer History. J. Racial and Ethnic Health Disparities 10, 2354–2362 (2023). https://doi.org/10.1007/s40615-022-01415-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01415-2