Abstract
Background
COVID-19 revealed and broadened existing disparities in large cities. This article interprets the early impacts of COVID-19 on food insecurity (FI) in the Chicago and New York City (NYC) metropolitan areas for Black, Indigenous, and People of Color (BIPOC) and provides a study using a Social Determinants of Health (SDOH) framework.
Methods
A cross-sectional survey adapted from the National Food Access and COVID Research Team (NFACT) was deployed in Chicago (N = 680) and in NYC (N = 525) during summer 2020 and oversampled for race, ethnicity, and socioeconomic status. Multivariate binary logistic regression generated adjusted odds ratios (aOR) and 95% CIs for FI and select SDOH variables, which was conducted on each dataset.
Results
The prevalence of FI in NYC increased to 66.8% (from 57.8%) and in Chicago to 44.8% (from 41.0%). While higher income protected against FI before, protection was diminished or eliminated since COVID-19. FI declined for households with children in NYC while odds increased and became significant in Chicago. Respondents with chronic health conditions experienced increased odds of FI since COVID. In Chicago, this variable had the highest odds of FI. Respondents with depression or anxiety had increased odds of FI. In NYC, depression had the highest odds of FI. Females in NYC were protected against FI. Hispanics in NYC lost protection against FI from before to since COVID-19.
Conclusions
Results support the observed rise of FI for BIPOC and its association with health status. The analysis has multifaceted, structural policy implications for reducing FI in urban centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In public health, social inequities are examined across communities to understand the interlinkages between social structures and human well-being. Among diverse methods to better understand differential effects of the COVID-19 pandemic across communities, indices provide an assessment of household well-being useful in analyses [1]. Subsequent measures of health inequities during COVID-19 include access to quality healthcare, education, and food security [2,3,4]. In times of crisis such as the ongoing COVID-19 pandemic, pre-existing social inequalities lead to increased risks of infections, disease, disability, and mortality, especially among those of lower socioeconomic status. Even before COVID-19, historically marginalized communities experienced higher levels of unemployment, poor general health, poor nutritional status, and underlying chronic health conditions, such as diabetes mellitus and heart disease [5].
During a public health crisis, addressing health inequities requires the application of a Social Determinants of Health (SDOH) framework, which includes five social-economic indicators: economic stability (income, employment, and access to quality education), access to quality healthcare, neighborhood and built environment, and social and community context [6]. Debates around measuring and tracking inequity include alternatives that draw on SDOH for measuring inequity outside of strictly income-based variables. Examining inequality beyond income paints a more accurate picture of social inequality and, conversely, well-being [7].
As such, food security is a core SDOH [6]. Food insecurity (FI) is defined as having limited or no access to sufficient, nutritious food for living an active, healthy life. FI disproportionately impacts low-income communities and Black, Indigenous, and People of Color (BIPOC) [8] and is associated with poor health outcomes [9]. The United States Department of Agriculture (USDA) Six-Item Household Food Security Module offers a validated index to measure FI that we used to test hypotheses about the impacts of COVID-19 on BIPOC households across multiple sites [10].
The COVID-19 pandemic has revealed and broadened fractures in social structures, widening disparities globally across spheres of food security, health, and income. Pandemics affect humanity along the “fault lines of society—exposing and often magnifying power inequities that shape population health even in [less uncertain] times” [11, 12]. COVID-19 has resulted in the worsening of FI, which exacerbates worry and distress about not being able to meet basic household needs [13]. This chasm became severe for BIPOC in the USA—those who were already experiencing greater FI before the pandemic [8] and were sicker and living shorter lives than Whites [14,15,16,17]. These disparities of COVID-19 morbidity and mortality are “unjust, avoidable and… preventable” [16, 18].
COVID-19 is associated with greater FI among BIPOC and worse mental health outcomes [19,20,21]. Moreover, the US Census Bureau’s Household Pulse Survey reported that, although economic activity resumed in the USA around May 2020, the pandemic and subsequent social distancing restrictions led to family hardship, particularly food scarcity [22]. As a result, many individuals turned to safety net programs in their localities for help early in the pandemic, including food pantries and social assistance programs (i.e., Supplemental Nutrition Assistance Program (SNAP), Medicaid, and Temporary Assistance for Needy Families (TANF)), the $2.0 trillion Coronavirus Aid, Relief, and Economic Security (CARES) Act, and a more extensive relief package by the Trump administration [23].
While it is important to understand the breadth and depth of the impact of COVID-19 for building future resilience to public health crises [24, 25], few studies have reported empirical evidence about the impact of COVID-19 on FI in the USA [9, 26]. In addition to the inability to provide nutritious, affordable, available, and acceptable foods for a household, FI is associated with multiple adverse health outcomes, such as diabetes mellitus, hypertension, cardiovascular disease, depression, and increased risk of mortality [26]. With the continued threat of the COVID-19 pandemic, worsening economic conditions and financial instability adversely impact FI households [27] and BIPOC [9, 28].
Large metropolitan areas have great variability in terms of policies that can influence FI and health outcomes for residents. Two of the largest cities in the USA—Chicago and New York City (NYC)—have different welfare-oriented policies in place that may influence differences in FI outcomes. For example, pre-COVID-19, NYC’s safety net structure was heavily reliant on human services nonprofit organizations that, since the pandemic, have experienced large budget decreases from a lack of government funding [29]. Meanwhile, Chicago’s pre-COVID-19 support is reliant on federal and state welfare programs, such as SNAP and the Healthy Hunger-Free Kids Act of 2010 (implemented in Chicago Public Schools [CPS]), all of which received continuous support during the pandemic. The city of Chicago also partnered with community nonprofit organizations for food distribution, and although resources were available, social distancing and business closures made it difficult to access [30].
Leveraging the SDOH framework [6] in combination with the safety net response to COVID-19, our study examines FI in Chicago and in NYC [23, 31,32,33,34,35]. The aims of this paper are to (1) report and interpret the impacts of COVID-19 on BIPOC FI households in the greater Chicago and NYC metropolitan areas and (2) discuss how these findings reflect differing urban contexts and safety net policies for the purpose of narrowing and eliminating disparities in FI.
Methodology
Study Design
Our exploratory study began early in the pandemic. We recognized the need to collect data quickly to identify the early impacts of COVID-19 on FI for BIPOC across geographies and populations. As such, our study contributes to the efforts of a larger national collaborative, known as the National Food Access and COVID Research Team (NFACT). This group developed a survey to evaluate the early and ongoing impacts of COVID-19 on food security. That survey relies on the USDA Six-Item Food Security Module to generate a comparable measure of FI [10]. As of August 2020, the NFACT survey was administered across 18 sites and 15 states, including a national poll [19].
The Chicago and NYC studies adapted the NFACT survey to fit our respective contexts. The research team applied the SDOH Framework, with new measures on access to healthcare and mental health, among others [36,37,38], from a previously validated survey [26]. Our adaptations included shortening the survey administration time by streamlining the language and eliminating most comment fields, and adding health measures such as access to health care, mental health status, physical health status, and high risk medical conditions for COVID-19.
Our analysis examined datasets for Chicago and NYC separately. Both were collected using a similar survey and methodology. We did not merge the data or attempt to draw statistical comparisons between the cities. The Chicago survey covered the Chicago Metropolitan Statistical Area (Cook, DeKalb, DuPage, Grundy, Kane, Kankakee, Kendall, Lake, McHenry, and Will Counties in Illinois; and Lake, Newton, and Porter Counties in Indiana). The NYC survey included NYC proper (Manhattan County [NYC], Kings County [Brooklyn], Queens County [Queens], Richmond County [Staten Island], and Bronx County [Bronx]) and surrounding Hudson and Westchester Counties in New York, Bergen County in New Jersey, and Fairfield County in Connecticut.
We used a nested quota sampling design to meet specific targets for race, ethnicity, income, and education. Estimating outcomes for BIPOC in public health research is crucial and oversampling is a way to deliver more accurate estimates than what can be obtained from comparisons to the general population [39]. We oversampled in both cities using a similar design to capture self-reported low-income populations (less than $25,000 annual income before 2019 taxes) (50% Chicago, 50% NYC), Black (50% Chicago, 40% NYC), Native American (10% NYC), Hispanic (50% Chicago, 40% NYC), and those with a high school education or less (50% Chicago, 50% NYC). It is important to note that in our recently published NFACT multisite paper, three other studies also oversampled for BIPOC populations [19].
Both surveys used a cross-sectional design and were conducted independently at a single data collection time point during the summer of 2020. Respondents were asked about perceived differences in their state of living across two different time periods. Specifically, we asked participants to make a self-assessment of their state before COVID-19 versus their current state in real time since COVID-19. All “before CO13D-19” data were retrospective recalls by respondents at the same time they responded to items about “since COVID-19.” The start of the coronavirus outbreak was defined as March 2020. Responses to “before COVID-19” included the 12 months prior to March 2020, while “since COVID-19” included everything after the March 2020 onset of COVID-19 to the time of the survey.
Participants were recruited from a web-based consumer panel and screened based on age (18 and over), race, ethnicity, county of residence, income, and education levels [36]. Respondents were asked to provide information about their household which included all individuals who lived with them. Only one respondent per household participated. The consumer panel solicited participation from registered members and provided compensation for participation. Subsample quotas were achieved by targeting solicitations to members who met the demographic and socioeconomic criteria. Final de-identified datasets were delivered to the research team.
Variables
Food Security
We utilized the United States Department of Agriculture (USDA) Six-Item validated Food Security Module to measure FI (outcome) before COVID-19 and since COVID-19. The Six-Item Short Form [10] was adapted to ask about the time period both “in the year before the coronavirus outbreak” and “since the coronavirus outbreak,” defined in the survey instrument as “before COVID-19” and “since COVID-19,” respectively (Appendix 17). Scoring and classification used established procedures from the USDA Food Security Module (Appendix 17). According to the USDA, for reporting purposes a raw score of 0–1 is described as “food secure,” and the two categories “low food security” (2–4) and “very low food security” (5–6) in combination are referred to as FI [10]. The measure was used without modifications in the univariate analysis and represented as three categories: “food secure” (0–1), “low food security” (2–4), and “very low food security” (5–6). In the bivariate and multivariate analyses, food security was re-coded as a binary categorical variable where 0 corresponds to “food secure” and 1 corresponds to “FI.”
Household Determinants
This category has two variables: household income and household with children. Household income captures all income streams for the household to which the respondent belongs. Household income was categorized into seven subcategories, where 0 corresponds to “Less than $12,000 per year” and 6 corresponds to “$125,000 or greater per year.”
Respondents were asked to report the number of persons less than 18 years old living in their households. This variable was re-coded into a binary categorical variable where 0 corresponds to “No children living in the household” and 1 corresponds to “Children are living in the household.”
Individual Determinants
This category represents the respondent’s physical and mental health, in addition to their access to healthcare services. Respondents self-reported the presence of a health condition or multiple health conditions, including cancer, hypertension, diabetes, chronic respiratory disease, rheumatological disease, and cardiovascular disease. This variable was re-coded into a binary categorical variable, where 0 corresponds to “No health condition” and 1 corresponds to “Health condition present.” These specific chronic health conditions are a health burden, physically, mentally, and economically. These health conditions place individuals at a greater risk for developing serious illness when contracting COVID-19 [40].
Anxiety and depression were measured using the GAD-2 [41] and PHQ-2 [42] scales, respectively. Both screening tests use a score scale from 0 to 6. If a respondent’s score is higher than 3 (optimal cut point), the test is considered positive (positive GAD-2 and/or PHQ-2) and the respondent is at higher risk of having either anxiety or depression, respectively. Accordingly, these variables were coded as 0 which corresponds to “Negative” and 1 which corresponds to “Positive.”
Health insurance status was categorized into three subcategories, where 0 corresponds to “Private health insurance,” 1 corresponds to “Public health insurance,” and 2 corresponds to “No health insurance.”
This category of variables also represents the respondents’ self-identified demographics and educational attainment. Participants’ demographics consist of age, gender, race, and ethnicity. Age was categorized into three groups where 0 corresponds to ages “18 to 39,” 1 corresponds to ages “40 to 55,” and 2 corresponds to “56 years old and above.”
Gender had five categories: “Female,” “Male,” Non-binary,” “Transgender,” and “Other.” The gender variable was re-coded to a binary categorical variable where 0 corresponds to “Male” and 1 corresponds to “Female” in the bivariate and multivariate analyses. Other subcategories of gender were omitted from these analyses due to very low statistical power.
Race and ethnicity were re-coded into two categories. The first category has two subcategories, where 0 corresponds to “Non-Hispanic White” and 1 corresponds to “Black, Indigenous, People Of Color (BIPOC).” The second category has two subcategories, where 0 corresponds to “non-Hispanic” and 1 corresponds to “Hispanic.”
Respondents’ education was re-coded into three categories based on the level of their educational attainment in the statistical analyses. Respondents who received education after bachelor’s level were coded as 0. Those who attained education in a college (some college education, or associate degree) or a university degree (bachelor degree) were coded as 1. Finally, respondents who obtained education up to a high school level were coded as 2.
Statistical Analysis
Descriptive analysis was conducted to explore the frequencies of the USDA Six-Item validated Food Security Module. The independent variables were treated as categorical variables (nominal or ordinal) and examined using frequencies. The mode was calculated as a measure of central tendency and dispersion. A McNemar’s test was conducted to assess the statistically significant change in the proportions of food security status before COVID-19 and since COVID-19. Only respondents who answered all USDA Six-Item questions for before and since COVID-19 were included in the test (matched pairs pre-post test). Bivariate chi-square tests were conducted to examine the differences in FI prevalence when stratified by the indicator variables. To consider the results of the McNemar’s or chi-square tests to be statistically significant, the p-value must be less than 0.05.
The multivariate binary logistic regression model was developed using the SDOH framework. Our model includes variables for four of the five social-economic indicator categories: (1) economic stability: household income range; (2) access to quality education: education level; (3) access to quality healthcare: presence of a health condition, anxiety screen, depression screen, and health insurance status; and (4) social and community context: children in the household, age, gender, race, and ethnicity. We did not analyze variables for the neighborhood and built environment SDOH category [6]. The multivariate logistic regression model was applied to examine the associations between FI and all of the independent variables at the same time. The multivariate regression models’ results were reported as adjusted odds ratios. The confidence intervals (CI) were set at 95% which corresponds to a p-value of 5%. To consider an association significant, the reported ratios must have had a p-value < 0.05. The area under the receiver operating characteristic (ROC) curve was calculated to evaluate how well the adjusted binary logistic regression models classify positive and negative food security status outcomes at all possible cutoff points. The analysis was performed with Stata/BE 17.0.
Results
Descriptives
The characteristics and demographics of individual respondents and households are shown in Table 1. The descriptives relevant to the sampling design include income, race, ethnicity, and education. A similar percentage of households reported an annual income of less than $25,000 in Chicago and NYC (31.4% and 34.7%, respectively). Most respondents were 18 to 39 years old in Chicago and NYC (70%, 69.5%, respectively). The gender of respondents in Chicago was 46.2% female and 52.1% male, 0.9% non-binary, 0.7% transgender, and 0.1% other. In NYC, 52.6% of respondents were female, 45.5% male, 0.8% non-binary, 0.9% transgender, and 0.2% other. Most respondents in Chicago and NYC identified as BIPOC (74.4% and 92% respectively). Both Chicago and NYC had a similar percentage of respondents who identified as Hispanic (36.6% and 36.2% respectively). Respondents who have reported having up to a high school education in Chicago and NYC were 29.1% and 29.7% respectively.
Descriptives relevant to SDOH include the presence of children in the household, presence of a health condition, anxiety, depression, and health insurance status. In Chicago, 55.7% of respondents reported having children living in their household, and in NYC it was 60.4%. Respondents who reported a health condition were 32.9% in Chicago, and 51.2% in NYC. Most Chicago respondents screened positive for anxiety and depression (66.6% and 66.7%, respectively), while positive screens for anxiety and depression in NYC were 37.9% and 43.8%, respectively. A similar percentage of respondents reported having a type of health insurance in Chicago and NYC (85.7% and 86.7% respectively).
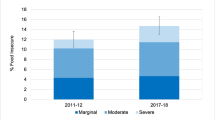
Food security assessments before and since COVID-19 in Chicago and NYC are shown in Table 2. Since COVID-19, the percentage of households classified as food secure (score 0–1) declined and FI households (score 2–6) increased in both cities. In Chicago, 44.8% of households were FI since COVID-19, compared to 41% before. In NYC, the percentage of FI households since COVID-19 was 66.8%, compared to 57.8% before. A greater percentage of households in Chicago and NYC reported very low food security since COVID-19 (20.6% and 28.7%, respectively) compared to before (14.6% and 22.7%, respectively).
Bivariate Analyses
Table 3 shows the food security status (food secure vs FI) of matched-pairs (before COVID-19 and since COVID-19) respondents in Chicago and NYC. We classified FI households that completed all Food Security Index questions for before and since COVID-19 into consistently FI (CFI) and newly FI (NFI) categories. Households that were FI before and since COVID-19 were categorized as CFI. Households were categorized as NFI when they were food secure before and FI since COVID-19 [26]. NFI is significant because it demonstrates the loss of food security since COVID-19. In Chicago, the number of CFI households was 200 (80%) and that of NFI households was 50 (20%). Similarly, in NYC, the number of CFI households was 272 (79.5%) and that of NFI households was 70 (20.5%).
Table 4 shows the FI status of respondents (matched-pairs) in Chicago and NYC before and since COVID-19. In Chicago, the difference in proportions of FI was 3.99% higher (p < 0.05, 95% CI: 0.01–0.07) since COVID-19 compared to before COVID-19. Likewise in NYC, the difference in proportions of FI was higher (p < 0.001, 95% CI: 0.05–0.13) since COVID-19 when compared with before COVID-19.
Chi-square analyses were conducted to test if there were differences in prevalence of FI when stratified by the indicators before and since COVID-19 in Chicago and NYC. There was a significant difference in the prevalence of FI between the subcategories of household income, anxiety and depression screens, health insurance, age, race, and education in Chicago before COVID-19 (Appendix 6). After COVID-19, FI prevalence remained significantly different across the previous variables in addition to children in a household and ethnicity (Appendix 7). In NYC, there was a significant difference in the prevalence of FI across children in a household, health condition, anxiety, depression, health insurance, age, gender, race, and ethnicity before COVID-19 (Appendix 8). Since COVID-19, FI prevalence remained significant for the previous variables except for age, race, and ethnicity (Appendix 9).
Multivariate Logistic Regression
Before COVID-19
Table 5 shows the multivariate binary logistic regression analyses before and since COVID-19 in Chicago and NYC. In Chicago, the adjusted model showed that the association of income was significant across almost all subcategories. When controlling for all covariates, the higher the income subcategory, the lower the odds to have reported FI. As such, income subcategory $125,000 or above had the least odds of reported FI (aOR = 0.11, 95% CI: 0.03–0.41). In NYC, all income subcategories except one ($100,000–$124,999) were significantly associated with FI after adjustment for covariates.
In NYC, households with children had more than two times the odds to have reported FI when compared to households without children (aOR = 2.62, 95% CI: 1.68–4.1). Respondents with health conditions had higher odds to have reported FI in Chicago and NYC (aOR = 1.76, 95% CI: 1.08–2.85, aOR = 1.95, 95% CI: 1.28–2.97, respectively). People with self-reported depression had greater odds to have reported FI in Chicago and NYC (aOR = 1.9, 95% CI: 1.08–3.34, aOR = 2.37, 95% CI: 1.45–3.87, respectively). Chicago respondents who had public health insurance had lower odds to have reported FI compared to respondents who had private health insurance (aOR = 0.56, 95% CI: 0.34–0.93). In NYC, the respondent’s type of health insurance had no significant association with FI. Respondents in Chicago over 56 years of age had fewer odds to have reported FI compared to those 18 to 39 years old (aOR = 0.34, 95% CI: 0.15–0.8). Females in NYC had lower odds to have reported FI (aOR = 0.59, 95% CI: 0.38–0.91) compared to males. Respondents in NYC who identified as Hispanic had fewer odds to have reported FI compared to non-Hispanic respondents (aOR = 0.44, 95% CI: 0.29–0.68). Educational attainment showed no association with FI in Chicago or NYC.
Since COVID-19
As shown in Table 5, income subcategories either lost their significant association with FI or had their association significance reduced in Chicago and NYC. Most respondents of different income subcategories had their reported FI adjusted odds reduced since COVID compared to before. Income subcategories ranging from $50,000 to $124,999 per year lost their significant association among NYC respondents and remained significant among Chicago respondents. In general, income subcategories remained significantly associated with lower adjusted odds of FI with various degrees in Chicago and NYC.
Households with children had higher odds to have reported FI in Chicago and NYC (aOR = 1.78, 95% CI: 1.15–2.76, aOR = 2.35, 95% CI: 1.48–3.72, respectively). Among respondents who reported living with chronic health conditions, there was an increase in the odds of reported FI since COVID-19. Respondents living with health conditions had higher odds to have reported FI in Chicago and NYC (aOR = 1.97, 95% CI: 1.23–3.15, aOR = 2.2, 95% CI: 1.43–3.39, respectively). Chicago respondents with a positive anxiety screen had higher odds to have reported FI (aOR = 1.97, 95% CI: 1.23–3.15). Respondents with a positive depression screen in NYC had more than two times the odds to have reported FI (aOR = 2.52, 95% CI: 1.52–4.18). Compared to respondents with private health insurance, NYC respondents with public health insurance or no health insurance were at increased odds to have reported FI (aOR = 2, 95% CI: 1.26–3.18, aOR = 2.22, 95% CI: 1.05–4.73, respectively). Having health insurance and the type of health insurance were significantly associated with FI in NYC since COVID-19 compared to before COVID-19. In Chicago, this factor lost its significant association with FI since COVID-19. Since COVID-19, respondents in Chicago over 56 years of age had fewer odds to have reported FI compared to those 18 to 39 years old (aOR = 0.39, 95% CI: 0.17–0.9). Females in NYC had lower odds to have reported FI (aOR = 0.6, 95% CI: 0.38–0.93). Being female in Chicago was not significantly associated with FI. NYC respondents who identified as Hispanic no longer had a significant association with lower odds of reported FI since COVID-19 compared to before COVID-19. Educational attainment was not significantly associated with FI in either city since COVID-19.
Discussion
Overall, the results of the analyses for Chicago and NYC returned similar trends and associations. In both cities, FI increased since COVID-19, with minor deviations for unique scenarios in either Chicago or NYC. Increases in FI for NYC and Chicago have been reported elsewhere [43,44,45]. This is unsurprising considering the intensity with which the COVID-19 pandemic affected U.S. urban areas [46]. Chicago and NYC are two of the three largest metropolitan areas in the USA and urban research has confirmed the vulnerability of large cities to pandemics and infectious diseases [47]. However, our findings are higher compared to other sources, likely because we oversampled populations previously known to experience higher rates of FI [8, 16, 17].
Our study reports that, before COVID-19, income was significantly associated across nearly all subcategories across both cities, with higher income as a protective factor against FI in Chicago. Here, we used income as an indicator variable for economic stability in the Healthy People 2030 goals, as is common in the SDOH framework [48]. In the examined time period since COVID-19, high income subcategories did not appear to be protective against FI in NYC. Findings also reveal income’s relevance to FI as low-income populations saw higher odds of FI and, since COVID-19, the protective effects of income were reduced or eliminated in both cities [49].
Our results reported households with children under 18 years of age had higher odds of being FI in both Chicago and NYC. These results support other research that finds households with children experienced higher odds of FI than those without children [50]. A possible common explanation across the two cities could be the sudden loss of free school meals with school district closures. With schools closed, families would be expected to experience an increase in spending on food to account for any meals provided by the school, across each school-aged child in the household. For instance, there are 337,664 children attending 642 K-12 public schools in Chicago and 1.1 million children attending 1866 K-12 public schools in NYC [51]. In NYC public schools, 73 percent of 1.1 million students experience poverty and therefore qualify for free or reduced lunches [52].
Similarly, respondents living with chronic health conditions had higher odds of being FI in Chicago and NYC. Our findings corroborate with the literature indicating that people who live in FI households often face difficulties in managing diet-related chronic conditions, including being on a limited budget and restricted healthcare access [53]. These conditions also place them at a higher risk of COVID-19 infections and death, such as obesity, diabetes mellitus, hypertension, and heart disease [40]. Again, respondents living with chronic health conditions had higher odds of being FI since COVID-19 began, understandably, given the sudden and drastic decline in access to health care due to the immediate infrastructural and institutional shutdowns [2].
Since COVID-19, FI has been identified as a major predictor of depression, anxiety, and high stress among low-income Americans [20, 21]. Even prior to the pandemic, FI has been a well-known predictor for mental health factors, including major depression and anxiety [54]. However, it should be noted that there is a bidirectionality to the relationship between FI and mental health, and therefore, we cannot infer causality [55]. Depression had two times greater odds to be associated with FI in NYC and was associated with higher FI in Chicago. Research shows that financial insecurity and FI create feelings of sadness, hopelessness, shame, guilt, and anxiety [56]. It is possible that social isolation since COVID-19 exacerbated these feelings and increased depression and/or depression symptoms in individuals [2].
Furthermore, Chicago respondents who had public health insurance had fewer odds to be FI, while in NYC, the type of health insurance a respondent had showed no significant association with FI. This could be due to differences between access and affordability of health insurance in both cities, including public health insurance. Our findings differ from other studies, in particular research that shows Medicare enrollees to have higher odds to experience FI [57].
Age was inversely associated with the odds of being FI before COVID-19 in both cities, but age was only significant in Chicago since the onset of COVID-19. It is important to note that the study is limited in evaluating the relationship between age and FI, since age was measured as a categorical variable with three categories, and age of the participants is not representative of the population. Overall, our results confirm that age is a significant predictor for FI in Chicago, but there was no significance in NYC.
FI is most prevalent among females in a household with children [54]. Females had greater odds of being FI before COVID-19 began in NYC potentially due to the high cost of living, if women are assumed to earn lower incomes and bear greater care responsibilities [58, 59]. Female caregivers with children may also have gained access to school meal programs and other related programs before, but not early during, the COVID-19 pandemic. At the start of the pandemic, all Chicago Public School (CPS) students were eligible to receive meals. CPS increased food accessibility for children and families by providing “grab and go” family food packages that contained up to 3 days’ worth of food for breakfast and dinner [60]. In addition, CPS students received up to $450 distributed through a P-EBT card to meet food needs, increasing food accessibility [61]. The confluence of NYC’s higher population density, higher cost of living, greater relative poverty, and the public’s higher dependence on public transportation and therefore inability to avoid crowds may help explain some of the greater disparate effects across gender, caused by the early first wave of the pandemic when NYC was the epicenter [62]. However, further studies are needed with a larger sample size, to make such assessments.
Findings of earlier studies in Chicago support our findings that, pre-COVID, BIPOC households in Chicago had higher odds of experiencing FI [26, 63]. Notably, a larger proportion of BIPOC households, not Hispanic households, in NYC appeared to be better protected from FI since COVID-19 than before the pandemic. This pattern was not observed among BIPOC in Chicago. Because BIPOC households in NYC had differing results than the Hispanic population in NYC, as well as both BIPOC and Hispanic households in Chicago, the data suggests that we need a closer look at the local policies and programs in place as well as other potential factors influencing FI protections for historically marginalized communities in both cities [64]. Using slightly different nested quotas in the sampling designs for NYC and Chicago, as well as the different proportion of White respondents in the two cities, could have contributed to different outcomes for BIPOC and Hispanic respondents. It should be noted that our study was not powered to detect differences across specific race or ethnicity groups, except for Hispanic, despite our intention to oversample households affected by FI.
Finally, educational attainment served as a proxy variable for quality access to education in the SDOH framework [6]. While not unimportant to conversations about economic instability, our findings showed that educational attainment had no significant association with self-reported FI status, when comparing the periods before COVID-19 and since the onset of COVID-19 in March 2020.
Conclusion
Our study found that FI increased since COVID-19 in both Chicago and NYC for BIPOC populations known to be vulnerable to FI. While FI increased since COVID-19 in both Chicago and NYC, SDOH factors across the two cities did not show substantially different effects on FI since COVID-19, aside from specific cases such as females and Hispanics in NYC. Our study was exploratory in nature, conducted in the early months of the COVID-19 pandemic, cross-sectional in design, and oversampled for BIPOC.
These urban centers are densely populated and often experience “staggering income inequalities” among a heterogeneous population with a mix of diverse races, cultures, and backgrounds [62, 65]. Population density in NYC (26,403 people per square mile) is over 2.2 times greater than Chicago (11,783 people per square mile). Manhattan alone, the borough with the highest population density at more than 66,000 people per square mile, is 5.6 times greater than Chicago [66]. In turn, the dense social composition of NYC impacted people across all income brackets, helping to explain that in our study, high income was not a protective factor in NYC. Beyond general population density, overcrowding has been linked to COVID-19 risks of exposure, regardless of geography [67].
Moreover, there may be wider social and economic disparities in NYC, as evidenced by higher costs of living and greater relative poverty. In fact, NYC has continued to be reported as being the most expensive city in the USA, compared to other large American cities such as San Francisco, Boston, Chicago, and Los Angeles [68]. In NYC, higher costs of living (i.e., out-of-pocket rent expenses) are often associated with not only lower levels of economic achievement, but also worse self-reported health conditions and a higher likelihood of postponing medical services for financial reasons [69]. In NYC, the cost of living index data is 1.6 times higher than Chicago: based on a Composite Index of 100%, 116.9% for Chicago, and 185.8% for NYC (combined average of Manhattan [216.7%], Brooklyn [181.7%], and Queens [159%]) [70]. Despite these differences, we did not find substantial differences in FI before and since COVID-19 for the two cities.
Income inequality was associated with FI before COVID-19 in both cities. However, since COVID-19, increasing annual income was either lost or diminished in its association with FI. Aside from income, employment and access to quality education are components of economic instability within the SDOH framework. Ultimately, employment was not included in this study as income and education have been sufficient proxy variables across COVID-19 FI studies [44, 45, 71]. However, we believe there is a complex relationship surrounding the type and nature of employment that needs future exploration. Access to quality education, through the educational attainment variable, was not significant in our study.
This study shows that beyond income, other structural, social, and health inequities had a greater impact on predicting FI since COVID-19 in both cities. When accounted for, such factors diminished the protective effect of increasing annual income against FI. We recognize the limitations of using income as an indicator of economic standing. Future studies will expand beyond income to discuss variables such as educational attainment, employment status, and types of employment as additional indicators of economic well-being.
Age is a characteristic often linked to or dependent on other factors such as gender, race and ethnicity, and social class, building on what Estes [72] calls an interlocking system of oppression that is interactional in nature. Similar to the conclusions drawn from our BIPOC results, future studies need to be larger to capture the nature of age, which may have adverse effects on young populations (i.e., teenagers), in addition to any elderly-related results. In order to truly understand the impact of an emergency or crisis on FI, we need to further study the intersectionality of race, ethnicity, gender, and low-income populations.
Our study is useful for understanding how SDOH influence COVID-19’s impacts on FI among BIPOC populations in general. While we oversampled for specific race and ethnicity groups, the study was not sufficiently powered to detect differences among groups. Since our study design is cross-sectional, findings indicate associations and cannot determine causality or temporality. Despite the limitations of our study, higher rates of FI were reported for our sample population across both sites. Additionally, similar studies confirm not only the continuation of FI since COVID-19, but also suggest amplified outcomes on households with children as well as widening dietary inequities across low-income and BIPOC households [43,44,45]. These results underscore the early impact of the pandemic on existing socioeconomic inequities affecting BIPOC populations, as well as the higher prevalence of FI among these communities before the pandemic [26]. Similarly, our transgender, non-binary, and other gender categories did not have sufficient statistical power to be tested as their own category.
As the world rapidly urbanizes, studying urban centers can ultimately unlock the key to future public health solutions [73]. Despite observed differences between Chicago and NYC, the magnitude of the results does not change the overall rise of FI reported in all US cities studied by NFACT publications. Singularly testing each variable for its predictive capacity on FI may have overlooked interlocking influences, also referred to as syndemics theory [74]. As we do more research at the intersection of income, food, and health security, we can discover more commonalities across insecure communities and account for emerging insecure groups.
Future studies should address the intersectionality of demographic characteristics on outcomes like FI instead of relying on the predictive power of any single factor. Further evidence on the drivers of FI, and how we can predict and combat further increases in FI, can enable us to better alleviate the issue via policy solutions. From a policy perspective, Chicago continues to increase accessibility through the new “Food Equity Agenda,” a multi-year project to transform the food system in Chicago. The goals of the agenda are to eliminate barriers for food pantry expansions, eliminate barriers to urban farming, market nutrition programs and benefits, support local BIPOC food business, and increase funding for BIPOC food producers and businesses [75].
The results have multifaceted, structural policy implications insofar as income does not necessarily indicate food security, which could question the means-tested approach of social policies in the USA. For example, along with demographic and employment information, applications for programs such as SNAP require disclosure of income. As applications for benefits become more user-friendly, accounting for categories like chronic health conditions or health insurance status can better address issues of FI. This study corroborates other recent publications that call for a paradigmatic shift in our policies by taking a human rights framework to address upstream social and economic determinants of health that create health disparities to eliminate FI [26]. Moreover, further studies that include food security as a SDOH are necessary to inform targeted improvements in social protection policies and programs.
References
Hacker JS, Huber GA, Nicholas A, Rehm P, Schlesinger M, Valletta R, et al. The economic security index: a new measure for research and policy analysis. Rev Income Wealth [Internet]. 2014 May [cited 2021 Dec 21]; 60(S1):S5-S32. Available from: https://doi.org/10.1111/roiw.12053.
Leddy A, Weiser S, Palar K, Seligman H. A conceptual model for understanding the rapid COVID-19–related increase in food insecurity and its impact on health and healthcare. Am J Clin Nutr [Internet]. 2020 [cited 2022 Jan 5]; 112(5),1162–1169. Available from: https://doi.org/10.1093/ajcn/nqaa226.
Morales D, Morales A, Beltran T. Racial/ethnic disparities in household food insecurity during the COVID-19 pandemic: a nationally representative study. J Racial Ethn Health Disparities [Internet]; 2020 [cited 2022 Jan 5]; 8:1300–1314. https://doi.org/10.1007/s40615-020-00892-7.
Marmot M. The Health Gap: The Challenge of an Unequal World. London: Bloomsbury Press; 2015. p. 400.
Burstrom B, Tao W. Social determinants of health and inequalities in COVID-19. EUR J Public Health [Internet]. 2020 August [cited 2021 Dec 21]; 30(4):617–618. Available from: https://doi.org/10.1093/eurpub/ckaa095.
Office of Disease Prevention and Health Promotion. Social Determinants of Health (SDOH) [Internet]. Rockville MD; [updated 2021 Nov 4; cited 2022 April 22]. Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health.
Boushey H. Unbound: how inequality constricts our economy and what we can do about it. Cambridge: Harvard University Press; 2019. p. 304.
Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018. Washington DC: US Department of Agriculture, Economic Research Service; 2019. 47 p. Report No.:270.
Wolfson J, Leung CW. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients [Internet]. 2020 May 15 [cited 2021 Dec 21]; 12 (6): 1648. Available from: https://doi.org/10.3390/nu12061648.
US Department of Agriculture (USDA). U.S. Household Food Security Survey Module: Six-Item Short Form Economic Research Service [Internet]. USDA; 2012 [updated 2012 Sep, cited 2022 Jan 13]. Available from: https://www.ers.usda.gov/media/8282/short2012.pdf.
Gravlee CC. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making. AM J Hum Biol [Internet]. 2020 Aug 4 [cited 2021 Dec 21]; 32(5):1–8. Available from: https://doi.org/10.1002/ajhb.23482.
Wade L. An unequal blow. Science [Internet]. 2020 May 15 [cited 2021 Dec 21]; 362(6492):700–703. Available from: https://doi.org/10.1126/science.368.6492.700.
Tomsik PE, Smith S, Mason MJ, Zyzanski SJ, Stange KC, Werner JJ, et al. Understanding and measuring healthcare insecurity. J Health Care Poor Underserved [Internet]. 2014 November 4 [cited 2021 Dec 21]; 25(4):1821–1832. Available from: https://doi.org/10.1353/hpu.2014.0180.
Chotiner I. The interwoven threads of inequality and health [Internet]. New York NY: The New Yorker; 2020 [updated 2020 Apr 14; cited 2022 Jan 12]. Available from: https://www.newyorker.com/news/q-and-a/the-coronavirus-and-the-interwoven-threads-of-inequality-and-health.
Eligon J, Burch ADS, Searcey D, Oppel RA Jr. Black Americans face alarming rates of coronavirus infection in some states [Internet]. New York NY: The New York Times; 2020 [updated 2020 Apr 14; cited 2022 Jan 12]. Available from: https://www.nytimes.com/2020/04/07/us/coronavirus-race.html.
Krieger N. ENOUGH: COVID-19, structural racism, police brutality, plutocracy, climate change- and a time for health justice, democratic governance, and an equitable and sustainable future. Am J Public Health [Internet]. 2020 Oct 7 [cited 2021 Dec 21]; 110(11):1620–1623. Available from: https://doi.org/10.2105/AJPH.2020.305886.
Krieger N, Rowley Dl, Herman AA, Avery B, Philips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Public Health [Internet]. 1993 Dec [cited 2021 Dec 21]; 9(6):81–122. Available from: https://doi.org/10.1016/S0749-3797(18)30666-4.
Whitehead M. The concept and principles of equity and health. Int J Health Serv [Internet]. 1992 July 1 [cited 2021 Dec 21]; 22(3):429–445. Available from: https://doi.org/10.2190/986L-LHQ6-2VTE-YRRN.
Niles MT, Beavers AW, Clay LA, Dougan MM, Pignotti, GA, Rogus S, et al. A multi-site analysis of the prevalence of food security in the United States, before and during the COVID-19 pandemic. Curr Dev Nutr [Internet]. 2021 [cited 2022 Jan 27]; 5(12):nzab135. Available from: https://doi.org/10.1101/2021.07.23.21260280.
Wolfson JA, Garcia T, Leung CW. Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity [Internet]. 2021 [cited 2022 Jan 13]; 5(1):64–71. Available from: https://doi.org/10.1089/heq.2020.0059.
Fang D, Thomsen MR, Nayga Jr RM. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health [Internet]. 2021 Mar 29 [cited 2022 May 3]; 21:607. Available from: https://doi.org/10.1186/s12889-021-10631-0.
United States Census Bureau. Household Pulse Survey Data Tables [Internet]; 2020 [updated 2021 Dec 22, cited 2022 Jan 12]. Available from: www.census.gov/programs-surveys/household-pulse-survey/data.html.
Saloner B, Gollust SE, Planalp C, Blewett. LA. Access and enrollment in safety net program in the wake of COVID-19: a national cross-sectional survey. PLos One [Internet]. 2020 Oct 6 [cited 2021 Dec 21]; 15(10):1–11. Available from: https://doi.org/10.1371/journal.pone.0240080.
Fernandez AA, Shaw GP. Academic leadership in a time of crisis: the coronavirus and COVID-19. J Leadersh Organ Stud [Internet]. 2020 Apr 4 [cited 2021 Dec 21]; 14(1):39–45. Available from: https://doi.org/10.1002/jls.21684.
Gevorkyan A, Gadhoke P, Freidberg T. A path to global social and economic resiliency [Internet]. New York NY: Henry George School of Social Science; 2020 [cited 2021 Dec 21]. Available from: https://www.hgsss.org/a-path-to-global-social-and-economic-resilience/.
Niles MT, Bertmann F, Belarmino EH, Wentworth T, Biehl E, Neff R. The early food insecurity impacts of COVID-19. Nutrients [Internet]. 2020 July 15 [cited 2022 Jan 12]; 12(7):2096. Available from: https://doi.org/10.3390/nu12072096.
Feeding America. The impact of coronavirus on food insecurity in 2020. Chicago IL; 2020 Oct. 14 p. Available from: https://www.feedingamerica.org/sites/default/files/2020-10/Brief_Local%20Impact_10.2020_0.pdf.
Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska Natives: a national profile using the current population survey-food security. J Hunger Environ Nutr [Internet]. 2016 Oct 25 [cited 2022 Jan 12]; 12(1):1–10. Available from: https://doi.org/10.1080/19320248.2016.1227750.
Amandolare S. New York’s Safety Net in Jeopardy [Internet]. New York NY: Center for an Urban Future; 2021 [updated 2021 Apr, cited 2022 Jan 12]. Available from: from https://nycfuture.org/research/new-yorks-safety-net-in-jeopardy.
Durden K. The pandemic highlights food insecurity [Internet]. Chicago IL: Chicago Defender; 2020 [updated 2020 Nov 24, cited 2022 Jan 13]. Available from: https://chicagodefender.com/the-pandemic-highlights-food-insecurity/.
Bitler M, Hoynes H, Schanzenbach, DW. Why the safety net might not respond as effectively to COVID-19 as it should [Internet]. New York NY: The Milbank Quarterly; 2020 [updated 2020 Apr 30, cited 2022 Jan 12]. Available from: https://www.milbank.org/quarterly/opinions/why-the-safety-net-might-not-respond-as-effectively-to-covid-19-as-it-should/.
Bryan MS, Jiehuan S, Jyotsna J, Horton DE, Montgomery A, Sargis R, et al. Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago. Ann Epidemiol [Internet]. 2021 April [cited 2021 Dec 21]; 56:47-54. Available from: https://doi.org/10.1016/j.annepidem.2020.10.011.
Gu T, Mack JA, Salvatore M. Disparities in COVID-19 outcomes in an academic healthcare system. JAMA Nethttps://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_3.pdf. Open [Internet]. 2021 Oct 21 [cited 2022 Jan 13]; 19(6):1–5. Available from: https://doi.org/10.1001/jamanetworkopen.2020.25197.
Karpman M, Zuckerman S, Gonzalez D, Kenney GM. The COVID-19 pandemic is straining families’ abilities to afford basic needs [Internet]. Washington DC: Urban Institute; 2020 [updated 2020 Apr 21, cited 2022 Jan 13]. Available from: https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_3.pdf.
Rosenberg ES, Dufort EM, Blog DS, Hall EW, Hoeder D, Backenson BP, et al. COVID-19 testing, epidemic features, hospital outcomes, and household prevalence, New York State-March 2020. Clin Infect Dis [Internet]. 2020 May 8 [cited 2022 Jan 13]; 71(8):1953–1959. Available from: https://doi.org/10.1093/cid/ciaa549.
Gadhoke P, Brenton B, Clay L. COVID-19 revealed racial disparities in healthcare insecurity in NY City (Jul-Aug 2020). National Food Access and COVID-19 Research Team (NFACT) [Internet]. 2021 Jan 22 [cited 2022 Jan 13]. Available from: https://doi.org/10.17603/ds2-wp13-z439.
Gadhoke P, Brenton B, Clay L, Gu S. Racial disparities in food insecurity in NYC summer 2020. National Food Access and COVID Research Team (NFACT) [Internet]. 2021 Jan 22 [cited 2022 Jan 13]. Available from: https://doi.org/10.17603/ds2-wp13-z439.
Pemberton S, Gadhoke P, Brenton B, Kavouras I. COVID-19 widened food insecurity in households with and without children in NYC City (July-August 2020). New York NY: National Food Access and COVID Research Team (NFACT); 2021. 5 p. Available from: https://drive.google.com/file/d/1D5vTItjiNz9foIa1eEIMo7UJXjnjpIit/view.
Vaughan R. Oversampling in health surveys: why, when, and how?. Am J Public Health [Internet]. 2017 Aug [cited 2022 May 3]; 107(8):1214–1215. Available from: https://doi.org/10.2105/AJPH.2017.303895.
Centers for Disease Control and Prevention. COVID-19: people with certain medical conditions [Internet]. Atlanta GA; 2020 [updated 2021 Dec 14, cited 2022 Jan 13]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
Kroenke K, Spitzer RL, Williams, JB, Monahan PO, Löwe B. (2007). Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Internal Med [Internet]. 2007 Mar 6 [cited 2022 May 4]; 146(5):317–325. Available from: https://doi.org/10.7326/0003-4819-146-5-200703060-00004.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care [Internet]. 2003 Nov [cited 2022 May 4]; 41(11): 1284–1292. Available from: https://doi.org/10.1097/01.MLR.0000093487.78664.3C
CUNY Graduate School of Public Health and Health Policy (CUNY SPH). Week 12 - Part 1: Food Insecurity [Internet] New York NY; 2020 [cited 2022 May 3]. Available from: https://sph.cuny.edu/research/covid-19-tracking-survey/week-12/.
Schanzenbach D, Pitts A. Food Insecurity in the Census Household Pulse Survey Data Tables [Report on the Internet]. Evanston IL: Northwestern University Institute for Policy Research; 2020 June 1 [cited 2022 May 3]. 16 p. Available from: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-1-june-2020.pdf.
Schanzenbach D, Pitts A. How much has food insecurity risen? Evidence from the Census Household Pulse Survey [Report on the Internet]. Evanston IL: Northwestern University Institute for Policy Research; 2020 June 10 [cited 2022 May 3]. 10 p. Available from: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-10-june-2020.pdf.
Sharifi A, Khavarian-Garmsir AR. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci Total Environ [Internet]. 2020 [cited 2022 Apr 22]; 749:142391. Available from: https://doi.org/10.1016/j.scitotenv.2020.142391.
Connolly C, Harris Ali S, Keil R. On the relationships between COVID-19 and extended urbanization. Dialogues Hum Geogr [Internet]. 2020 [cited 2022 Apr 22]; 10(2):213–216. Available from: https://doi.org/10.1177/2043820620934209.
Office of Disease Prevention and Health Promotion. Economic stability [Internet]. Rockville MD; [updated 2021 Nov 4, cited 2022 April 22]. Available from: https://health.gov/healthypeople/objectives-and-data/browse-objectives/economic-stability
Hunt BR, Benjamins MR, Khan S, Hirschtick JL. Predictors of food insecurity in selected Chicago community areas. J Nutr Edu [Internet]. 2019 Mar [cited 2022 Jan 13]; 51(3):287–299. Available from: https://doi.org/10.1016/j.jneb.2018.08.005.
Parekh N, Ali SH, O’Connor J, Tozan Y, Jones AM, Capasso A, Foreman J, DiClemente RJ. Food insecurity among households with children during the COVID-19 pandemic: results from a study among social media users across the United States. Nutr J [Internet]. 2021 Aug 30 [cited 2022 May 3]; 20(1):73. Available from: https://doi.org/10.1186/s12937-021-00732-2.
McLoughlin GM, McCarthy JA, McGuirt JT, Singleton CR, Dunn P, Gadhoke P. Addressing food insecurity through a health equity lens: a case study of large urban school districts during the COVID-19 pandemic. J Urban Health [Internet]. 2020 Sep 21 [cited 2022 Jan 13]; 97(6):759–775. Available from: https://doi.org/10.1007/s11524-020-00476-0.
Lynch TL, Mader N. Equity means all not some: lessons from the past 20 years of education reform in New York City and what should come next. New York NY: Center for New York City Affairs; 2021 Apr. 37 p. Available from: http://www.centernyc.org/s/April19_FinalReport_IS.pdf.
Tarasuk V, Cheng J, de Oliveira C, Dachner N, Gundersen C, Kurdyak P. Association between household food insecurity and annual health care costs. CMAJ [Internet]. 2015 Oct 6 [cited 2022 Jan 13]; 187(14):1031–1032. Available from: https://doi.org/10.1503/cmaj.150234.
Siefert K, Heflin CM, Corcoran ME, William DR. Food insecurity and the physical and mental health of low-income women. Women & Health [Internet]. 2008 Oct 22 [cited 2022 Jan 13]; 32(1–2):159–177. Available from https://doi.org/10.1300/j013v32n01_08.
Van der Pols JC. Nutrition and mental health: bidirectional associations and multidimensional measures. Public Health Nutr [Internet]. 2018 Apr [cited 2022 May 3]; 21(5):829–830. Available from: https://doi.org/10.1017/S1368980017003974. PMID: 29517473.
Knowles M, Rabinowich J, Ettinger de Cuba S, Cutts DB, Chilton M. Do you wanna breathe or eat?: Parent perspectives on child health consequences of food insecurity, trade-offs, and toxic stress. Matern Child Health J [Internet]. 2016 [cited 2022 Jan 13]; 20(1): 25–32. Available from: https://doi.org/10.1007/s10995-015-1797-8.
Madden JM, Shetty PS, Zhang F, Briesacher BA, Ross-Degnan D, Soumerai SB et al. Risk factors associated with food insecurity in the Medicare population. Jama Intern Med [Internet]. 2019 Sep 30 [cited 2022 Jan 13]; 180(1):144–147. Available from: https://doi.org/10.1001/jamainternmed.2019.3900.
Freiberg T. Effects of care leave and family social policy: spotlight on the United States. Am J Econ Sociol [Internet]. 2019 Sep 29 [cited 2022 Jan 13]; 78(4):1009–1037. Available from: https://doi.org/10.1111/ajes.12293.
Mandel H, Semyonov M. Family policies, wage structures, and gender gaps: sources of earning inequality in 20 countries. Am Sociol Rev [Internet]. 2005 Sep 1 [cited 2022 Jan 13]; 70(6):949–967. Available from: https://doi.org/10.1177/000312240507000604.
Mayor’s Press Office. Citadel mobilizes to address food insecurity in Chicago amid the ongoing COVID-19 outbreak with $2.5 million in support [Internet]. Chicago IL: City of Chicago; 2020 [updated 2020 Mar 19, cited 2022 Jan 13]. Available from: https://www.chicago.gov/city/en/depts/mayor/press_room/press_releases/2020/march/CitadelAddressFoodInsecurity.html.
Issa N. Every CPS student to get $450 for food through federal program that will benefit 1 million Illinois Children [Internet]. Chicago IL: Chicago Sun Times; 2021 [updated 2021 Mar 2, cited 2022 Jan 13]. Available from: https://chicago.suntimes.com/education/2021/3/1/22303912/cps-public-schools-p-ebt-food-snap-lunch-free-reduced-illinois-pandemic-electronic-benefits-transfer.
Thompson CN, Baumgartner J, Pichardo C, Toro B, Lan L, Arciuolo R et al. COVID-19 Outbreak - New York City, February 29-June 1, 2020 [Internet]. Atlanta GA; 2020 Nov 20 [updated 2020 Dec 17, cited 2022 Jan 12]. Available from: https://doi.org/10.15585/mmwr.mm6946a2external icon.
Center on Budget and Policy Priorities. Tracking the COVID-19 recession’s effects on food, housing, and employment hardships [Analysis in brief on the Internet]. Washington DC: Center on Budget and Policy Priorities; 2020 [cited 2022 May 3]. 19 p. Available from: https://www.cbpp.org/sites/default/files/atoms/files/8-13-20pov.pdf.
Rodriguez C, Crowder SL, Rodriguez M, Redwine L, Stern M. Food insecurity and the Hispanic population during the COVID-19 pandemic. Ecol Food Nutr [Internet]. 2021 Sep-Oct [cited 2022 May 3]; 60(5):548–563. Available from: https://doi.org/10.1080/03670244.2021.1974014.
Olmo J, Sanso-Navarro M. Modeling the spread of COVID-19 in New York City. Pep Reg Sci [Internet]. 2021 May 11 [cited 2022 Jan 13]; 100(5)1–37. Available from: https://doi.org/10.1111/pirs.12615.
World Population Review. World population by country [Internet]. 2020; [updated 2021 Dec 21, cited 2021 Dec 21]. Available from: https://worldpopulationreview.com
Maru D, Maru S, Bass E, Masci J. To stem the spread of COVID-19 address the challenges of crowded housing. Health Aff [Internet]. 2020 May 26 [cited 2022 Jan 12]. Available from: https://doi.org/10.1377/hblog20200521.144527/full/.
Mogull RG. A Contrast of U.S. Metropolitan Demographic Poverty: Chicago, Los Angeles, and New York. Int J Popul Res [Internet]. 2011 Oct 18 [cited 2022 Jan 12]; 2011:1-5. Available from: https://doi.org/10.1155/2011/860684.
Meltzer R, Schwartz A. Housing affordability and health: evidence from New York City. House Policy Debate [Internet]. 2015 Apr 27 [cited 2022 Jan 12]; 26(1):80–104. Available from: https://doi.org/10.1080/10511482.2015.1020321.
U.S. Census Bureau. Cost of living index—selected urban areas [Internet]. Washington DC; 2010 [updated 2011 Sep 30, cited 2022 Jan 12]. Available from: https://www2.census.gov/library/publications/2011/compendia/statab/131ed/tables/12s0728.xls
CUNY Graduate School of Public Health and Health Policy (CUNY SPH). COVID-19 Tracking Survey Methodology [Internet]. New York NY; 2020 [cited 2022 May 3]. Available from: https://sph.cuny.edu/research/covid-19-tracking-survey/methodology.
Estes CL. Social policy and aging: a critical perspective. Thousand Oaks CA: Sage; 2001. p. 30.
Liu A, Berube A. Big cities aren’t dividing America, they hold the key to our collective future. Brookings [Internet]. 2021 Nov 9 [cited 2022 Apr 22]. Available from: https://www.brookings.edu/blog/the-avenue/2021/11/09/big-cities-arent-dividing-america-they-hold-the-key-to-our-collective-future/.
Singer M. Introduction to syndemics: a critical systems approach to public and community health. San Francisco: John Wiley & Sons; 2009. p. 306.
Chicago Food Equity Council. Chicago Food Equity Agenda. Chicago IL: City of Chicago; 2020. 8 p. Available from: https://www.chicago.gov/content/dam/city/sites/food-equity/pdfs/City_Food_Equity_Agenda.pdf.
Acknowledgements
This research is conducted as part of the National Food Access and COVID Research Team (NFACT). NFACT is a national collaboration of researchers across 18 sites who are committed to rigorous and timely food access research during the time of COVID-19. To learn more, visit: www.nfactresearch.org. We would like to acknowledge Victoria Rivkina for her assistance with project management for the Chicago study. We would like to acknowledge the sponsorship by the Vincentian Institute for Social Action at St. John’s University, Queens, for the New York City study.
Funding
This work was supported by DePaul University, University Research Council, Competitive Research Grant, Project Number 602101, and DePaul University, College of Liberal Arts and Social Sciences, Undergraduate Research Assistantship Program.
This study was approved by the IRBs of DePaul University & St. John’s University. Informed consent was obtained from all participants for being included in this study.
Author information
Authors and Affiliations
Contributions
J.M. contributed to the design of the study, collected and interpreted the data, and contributed to the production of the final manuscript. Z.Q. analyzed and interpreted the data and contributed to the production of the final manuscript. P.G. contributed to the design of the study, collected and interpreted the data, and contributed to the production of the final manuscript. T.F. interpreted the data and contributed to the production of the final manuscript. B.B. contributed to the design of the study, collected and interpreted the data, and contributed to the production of the final manuscript. A.S. analyzed and interpreted the data and contributed to the production of the final manuscript. A.T. contributed to the production of the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1 USDA Six-Item Food Security Questionnaire and Scoring and Classification
Six-Item Food Security Module [10]
Before COVID-19 | Before COVID-19 | |||||||
|---|---|---|---|---|---|---|---|---|
Often true | Sometimes true | Never true | Don’t know | Often true | Sometimes true | Never true | Don’t know | |
The food that my household bought just didn't last, and I/we didn't have money to get more | ||||||||
I/we couldn't afford to eat balanced meals | ||||||||
Did you or others in your household ever CUT the size of meals or SKIP meals because there wasn't enough money for food?* | ||||||||
Did you ever eat less than you felt you should because there wasn't enough money for food? | ||||||||
Were you ever hungry but didn't eat because there wasn't enough money for food? | ||||||||
Before COVID-19 | Since COVID-19 | |||||||
|---|---|---|---|---|---|---|---|---|
Almost every month | Some months but not every month | In only 1 or 2 months | Don’t know | Almost every month | Some months but not every month | In only 1 or 2 months | Don’t know | |
How often did this happen? | ||||||||
Scoring and Classification [10]
Each response of “often true,” “sometimes true,” “almost every month,” and “some months but not every month” is coded as affirmative (yes). The sum of affirmative responses to the six questions in the module is the household’s raw score on the scale.
Household food security status is assigned as follows:
Raw score 0–1—“Food Secure”: High or marginal food security (raw score 1 may be considered marginal food security, but a large proportion of households that would be measured as having marginal food security using the household or adult scale will have raw score zero on the six-item scale)
Raw score 2–4—Low food security
Raw score 5–6—Very low food security
For some reporting purposes, the food security status of households with raw score 0–1 is described as food secure and the two categories “low food security” and “very low food security” in combination are referred to as FI.
Appendix 2
Appendix 3
Appendix 4
Appendix 5
Rights and permissions
About this article
Cite this article
Mazzeo, J., Al Abdeen Qusair, Z., Gadhoke, P. et al. A Tale of Two Cities During the COVID-19 Pandemic: Evaluating Food Insecurity in Chicago and New York City. J. Racial and Ethnic Health Disparities 10, 1703–1720 (2023). https://doi.org/10.1007/s40615-022-01355-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-022-01355-x