Abstract
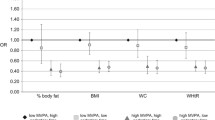
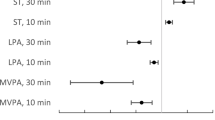
Previous studies suggest that the magnitude of morbidity/mortality reduction may differ between race-ethnic groups despite equated dose of physical activity (PA). The purpose of this study was to compare the potential racial-ethnic differences in cardiometabolic risk factors (CMRF) across quartiles of accelerometer-derived total activity counts/day (TAC/d) among US adults. The final sample (n=4144) included adults who participated in the 2003–2006 National Health and Nutrition Examination Survey (NHANES). CMRF included fasting glucose (FG), fasting insulin (FI), HOMA-IR, resting systolic (SBP) and diastolic blood pressure (DBP), waist circumference (WC), BMI, CRP, HDL-C, LDL-C, and triglycerides. Race-ethnic groups examined included non-Hispanic white (NHW), non-Hispanic black (NHB), and Mexican American (MA). In the highest quartile, NHW had significantly lower values of HOMA-IR, FI, SBP, BMI, WC, and HDL-C when compared to NHB. Compared to MA in the highest quartile, NHW had significantly lower values of HOMA-IR, FI, BMI, and triglycerides. Significant race-ethnic differences were found for several CMRF, especially among those who were in the top quartile of PA (e.g., the most active adults). It is probable that the protective effect of higher volumes of PA on CMRF is moderated by other non-PA factors distinct to NHB and MA.
Similar content being viewed by others
Data Availability
Data are publicly available online from https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
References
Pool LR, Ning H, Lloyd-Jones DM, Allen NB. Trends in racial/ethnic disparities in cardiovascular health among US adults from 1999-2012. J Am Heart Assoc. 2017;6(9). https://doi.org/10.1161/JAHA.117.006027.
Gasevic D, Ross ES, Lear SA. Ethnic differences in cardiovascular disease risk factors: a systematic review of North American evidence. Can J Cardiol. 2015;31(9):1169–79. https://doi.org/10.1016/j.cjca.2015.06.017.
Staiano AE, Harrington DM, Johannsen NM, Newton RL Jr, Sarzynski MA, Swift DL, et al. Uncovering physiological mechanisms for health disparities in type 2 diabetes. Ethn Dis. 2015;25(1):31–7 http://www.ncbi.nlm.nih.gov/pubmed/25812249.
Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010;51(Suppl):S15–27. https://doi.org/10.1177/0022146510383838.
Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. Jama-Journal of the American Medical Association. 2015;314(10):1021–9 https://jamanetwork.com/journals/jama/articlepdf/2434682/joi150096.pdf.
Murphy SL, Xu J, Kochanek KD, Curtin SC, Arias E. Deaths: final data for 2015. Natl Vital Stat Rep. 2017;66(6):1–75 https://www.ncbi.nlm.nih.gov/pubmed/29235985.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320:2020–8. https://doi.org/10.1001/jama.2018.14854.
Boyer WR, Churilla JR, Ehrlich SF, Crouter SE, Hornbuckle LM, Fitzhugh EC. Protective role of physical activity on type 2 diabetes: analysis of effect modification by race-ethnicity. J Diabetes. 2018;10(2):166–78. https://doi.org/10.1111/1753-0407.12574.
Gill JM, Celis-Morales CA, Ghouri N. Physical activity, ethnicity and cardio-metabolic health: does one size fit all? Atherosclerosis. 2014;232(2):319–33. https://doi.org/10.1016/j.atherosclerosis.2013.11.039.
Luke A, Dugas LR, Durazo-Arvizu RA, Cao G, Cooper RS. Assessing physical activity and its relationship to cardiovascular risk factors: NHANES 2003-2006. BMC Public Health. 2011;11:387. https://doi.org/10.1186/1471-2458-11-387.
Boyer W, Churilla J, Miller A, Gillum T, Penny M. The independent and combined effects of aerobic physical activity and muscular strengthening activity on all-cause mortality: an analysis of effect modification by race-ethnicity. J Phys Act Health. 2020;17:1–8. https://doi.org/10.1123/jpah.2019-0581.
Iliodromiti S, Ghouri N, Celis-Morales CA, Sattar N, Lumsden MA, Gill JM. Should physical activity recommendations for South Asian adults be ethnicity-specific? Evidence from a cross-sectional study of South Asian and white European men and women. PLoS One. 2016;11(8):e0160024. https://doi.org/10.1371/journal.pone.0160024.
Zhao M, Veeranki SP, Magnussen CG, Xi B. Recommended physical activity and all cause and cause specific mortality in US adults: prospective cohort study. BMJ. 2020;370:m2031. https://doi.org/10.1136/bmj.m2031.
Boyer WR, Ehrlich SF, Crouter SE, Churilla JR, Fitzhugh EC. Leisure-time aerobic physical activity and the risk of diabetes-related mortality: an analysis of effect modification by race-ethnicity. J Diabetes Complicat. 2021;35(1):107763. https://doi.org/10.1016/j.jdiacomp.2020.107763.
Bassett DR, Troiano RP, McClain JJ, Wolff DL. Accelerometer-based physical activity: total volume per day and standardized measures. Med Sci Sports Exerc. 2015;47(4):833–8. https://doi.org/10.1249/MSS.0000000000000468.
Wolff DL, Fitzhugh EC, Bassett DR, Churilla JR. Waist-worn actigraphy: population-referenced percentiles for total activity counts in U.S. adults. J Phys Act Health. 2014. https://doi.org/10.1123/jpah.2013-0464.
Boyer WR, Wolff-Hughes DL, Bassett DR, Churilla JR, Fitzhugh EC. Accelerometer-derived total activity counts, bouted minutes of moderate to vigorous activity, and insulin resistance: NHANES 2003-2006. Prev Chronic Dis. 2016;13:E146. https://doi.org/10.5888/pcd13.160159.
Wolff DL, Fitzhugh EC, Bassett DR, Churilla JR. Total activity counts and bouted minutes of moderate-to-vigorous physical activity: relationships with cardiometabolic biomarkers using 2003-2006 NHANES. J Phys Act Health. 2014;12:694–700. https://doi.org/10.1123/jpah.2013-0463.
National Center for Health Statistics, Centers for Disease Control and Prevention. NHANES Analytic and Reporting Guidelines. 2013. https://wwwn.cdc.gov/nchs/data/nhanes/analyticguidelines/99-10-analytic-guidelines.pdf
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. https://doi.org/10.1249/mss.0b013e31815a51b3.
Welk GJ, Schaben JA, Morrow JR Jr. Reliability of accelerometry-based activity monitors: a generalizability study. Med Sci Sports Exerc. 2004;36(9):1637–45 http://www.ncbi.nlm.nih.gov/pubmed/15354049.
National Health and Nutrition Examination Survey (NHANES). Laboratory Procedures Manual. 2011 https://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/2011-12_laboratory_procedures_manual.pdf.
Matthew CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(11 Suppl):S512–22 http://www.ncbi.nlm.nih.gov/pubmed/16294114.
American DA. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–31. https://doi.org/10.2337/dc20-S002.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;71:e127–248. https://doi.org/10.1016/j.jacc.2017.11.006.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–52. https://doi.org/10.1161/CIRCULATIONAHA.105.169404.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499–511 https://www.ncbi.nlm.nih.gov/pubmed/12551878.
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285(19):2486-97. 10.1001/jama.285.19.2486
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Gaillard TR, Osei K. Racial disparities in the pathogenesis of type 2 diabetes and its subtypes in the African diaspora: a new paradigm. J Racial Ethn Health Disparities. 2016;3(1):117–28. https://doi.org/10.1007/s40615-015-0121-z.
Aguayo-Mazzucato C, Diaque P, Hernandez S, Rosas S, Kostic A, Caballero AE. Understanding the growing epidemic of type 2 diabetes in the Hispanic population living in the United States. Diabetes Metab Res Rev. 2019;35(2):e3097. https://doi.org/10.1002/dmrr.3097.
Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the national health and nutrition examination survey. Hypertension. 2011;57(3):383–9. https://doi.org/10.1161/HYPERTENSIONAHA.110.161950.
Pereira MA, Folsom AR, McGovern PG, Carpenter M, Arnett DK, Liao D, et al. Physical activity and incident hypertension in black and white adults: the Atherosclerosis Risk in Communities Study. Prev Med. 1999;28(3):304–12. https://doi.org/10.1006/pmed.1998.0431.
Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. 2019;51(6):1314–23. https://doi.org/10.1249/MSS.0000000000001943.
Liu K, Ruth KJ, Flack JM, Jones-Webb R, Burke G, Savage PJ, et al. Blood pressure in young blacks and whites: relevance of obesity and lifestyle factors in determining differences. The CARDIA Study. Coronary Artery Risk Development in Young Adults. Circulation. 1996;93(1):60–6. https://doi.org/10.1161/01.cir.93.1.60.
Bassett DR Jr, Fitzhugh EC, Crespo CJ, King GA, McLaughlin JE. Physical activity and ethnic differences in hypertension prevalence in the United States. Prev Med. 2002;34(2):179–86. https://doi.org/10.1006/pmed.2001.0969.
Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393–423. https://doi.org/10.1161/CIR.0000000000000534.
Palazon-Bru A, Hernandez-Lozano D, Gil-Guillen VF. Which physical exercise interventions increase HDL-cholesterol levels? A systematic review of meta-analyses of randomized controlled trials. Sports Med. 2020;51:243–53. https://doi.org/10.1007/s40279-020-01364-y.
Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch Intern Med. 2007;167(10):999–1008. https://doi.org/10.1001/archinte.167.10.999.
Vella CA, Nelson MC, Unkart JT, Miljkovic I, Allison MA. Skeletal muscle area and density are associated with lipid and lipoprotein cholesterol levels: the Multi-Ethnic Study of Atherosclerosis. J Clin Lipidol. 2020;14(1):143–53. https://doi.org/10.1016/j.jacl.2020.01.002.
Carroll M, Kit B, Lacher D. Trends in elevated triglyceride in adults: United States, 2001-2012. NCHS Data Brief. 2015;198:198 https://www.ncbi.nlm.nih.gov/pubmed/25973997.
Frank AT, Zhao B, Jose PO, Azar KM, Fortmann SP, Palaniappan LP. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014;129(5):570–9. https://doi.org/10.1161/CIRCULATIONAHA.113.005757.
Yu SS, Castillo DC, Courville AB, Sumner AE. The triglyceride paradox in people of African descent. Metab Syndr Relat Disord. 2012;10(2):77–82. https://doi.org/10.1089/met.2011.0108.
Lin SX, Carnethon M, Szklo M, Bertoni A. Racial/ethnic differences in the association of triglycerides with other metabolic syndrome components: the Multi-Ethnic Study of Atherosclerosis. Metab Syndr Relat Disord. 2011;9(1):35–40. https://doi.org/10.1089/met.2010.0050.
Wolff-Hughes DL, Fitzhugh EC, Bassett DR, Churilla JR. Total activity counts and bouted minutes of moderate-to-vigorous physical activity: relationships with cardiometabolic biomarkers using 2003-2006 NHANES. J Phys Act Health. 2015;12(5):694–700. https://doi.org/10.1123/jpah.2013-0463.
Code Availability
Custom Code
Author information
Authors and Affiliations
Contributions
All authors contributed significantly.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Disclaimer
All views are of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boyer, W.R., Bassett, D.R., Fitzhugh, E.C. et al. Accelerometer-Measured Physical Activity and Cardiometabolic Risk Factors by Race-Ethnicity: 2003–2006 NHANES. J. Racial and Ethnic Health Disparities 9, 1607–1615 (2022). https://doi.org/10.1007/s40615-021-01100-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01100-w