Abstract
Objective
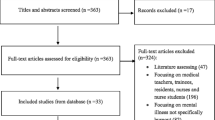
The authors conducted a systematic review of the published literature to identify interventions to prevent and/or reduce burnout among medical students and residents.
Methods
The authors searched 10 databases (from the start of each through September 21, 2016) using keywords related to burnout, medical education, and prevention. Teams of two authors independently reviewed the search results to select peer-reviewed, English language articles describing educational interventions to prevent and/or reduce burnout among medical students and/or residents that were evaluated using validated burnout measures. They assessed study quality using the Medical Education Research Study Quality Instrument and the Cochrane Risk of Bias Tool.
Results
Fourteen studies met inclusion criteria and all used the Maslach Burnout Inventory as at least one measure of burnout. Four were single group pre-post studies, 6 non-randomized two-group studies, and 4 randomized controlled trials. None of the studies were designed specifically to target burnout prevention. In 12 studies, residents were the targeted learners. Six of the 14 studies reported statistically significant changes in burnout scores: 5 reported improvement and 1 reported worsening of burnout. Of the 5 studies that reported statistically significant benefit, 1 studied a complementary and alternative medicine elective, 1 studied the Respiratory One Meditation method, and 3 studied duty hour changes.
Conclusions
This review highlights the need for rigorously designed studies in burnout prevention and reduction among residents and especially medical students.

Similar content being viewed by others
References
Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463–71.
Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85.
Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–13.
Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006;44:234–42.
Murray A, Montgomery JE, Chang H, Rogers WH, Inui T, Safran DG. Doctor discontent. A comparison of physician satisfaction in different delivery system settings, 1986 and 1997. J Gen Intern Med. 2001;16:452–9.
Buchbinder SB, Wilson M, Melick CF, Powe NR. Primary care physician job satisfaction and turnover. Am J Manag Care. 2001;7:701–13.
Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among american surgeons. Arch Surg. 2011;146:54–62.
Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149:334–41.
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488–91.
West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302:1294–300.
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000.
Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manag Rev. 2007;32:203–12.
Dyrbye LN, Massie FS Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–80.
West CP, Tan AD, Shanafelt TD. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87:1138–44.
Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325-6963-14-325.
West CP, Shanafelt TD. Physician well-being and professionalism. Minn Med. 2007;90:44–6.
Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91:422–31.
Noseworthy J, Madara J, Cosgrove D, et al. Physician burnout is a public health crisis: a message to our fellow health care CEOs. 2017.
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–51.
Rothenberger DA. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017;60:567–76.
Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements <http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements>. Accessed 27 Feb 2018.
Linzer M, Poplau S, Brown R, Grossman E, Varkey A, Yale S, et al. Do work condition interventions affect quality and errors in primary care? Results from the healthy work place study. J Gen Intern Med. 2017;32:56–61.
Sikka R, Morath JM, Leape L. The quadruple aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24:608–10.
Moss M, Good V, Gozal D, Kleinpell R, Sessler C. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. Am J Respir Crit Care Med. 2016;194:106–13.
Dzau V, Kirch D, Nasca T. To care is human — collectively confronting the clinician-burnout crisis. N Engl J Med. 2018;378:312–4.
Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39:47–54.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–81.
Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9:294–301.
Shanafelt TD, Gorringe G, Menaker R, Storz KA, Reeves D, Buskirk SJ, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90:432–40.
Wasson LT, Cusmano A, Meli L, Louh I, Falzon L, Hampsey M, et al. Association between learning environment interventions and medical student well-being: a systematic review. JAMA. 2016;316:2237–52.
Landrigan CP, Fahrenkopf AM, Lewin D, Sharek PJ, Barger LK, Eisner M, et al. Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122:250–8.
Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243:864–71.
Barrack RL, Miller LS, Sotile WM, Sotile MO, Rubash HE. Effect of duty hour standards on burnout among orthopaedic surgery residents. Clin Orthop Relat Res. 2006;449:134–7.
Schuh LA, Khan MA, Harle H, Southerland AM, Hicks WJ, Falchook A, et al. Pilot trial of IOM duty hour recommendations in neurology residency programs: unintended consequences. Neurology. 2011;77:883–7.
Parshuram CS, Amaral AC, Ferguson ND, Baker GR, Etchells EE, Flintoft V, et al. Patient safety, resident well-being and continuity of care with different resident duty schedules in the intensive care unit: a randomized trial. CMAJ. 2015;187:321–9.
Eckleberry-Hunt J, Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med. 2018;93:367–70.
Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:195–205.
Kemper KJ, Larrimore D, Dozier J, Woods C. Impact of a medical school elective in cultivating compassion through touch therapies. Complement Health Pract Rev. 2006;11:47–56.
de Vibe M, Solhaug I, Tyssen R, et al. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Med Educ. 2013;13:107-6920-13-107.
Anonymous. Deploying an interactive machine learning system in an evidence-based practice center: abstrackr. Proceedings of the Association for Computing Machinery International Health Informatics Symposium, 2012.
Reed DA, Beckman TJ, Wright SM, Levine RB, Kern DE, Cook DA. Predictive validity evidence for medical education research study quality instrument scores: quality of submissions to JGIM’s medical education special issue. J Gen Intern Med. 2008;23:903–7.
Kirkpatrick D, Kirkpatrick J. Evaluating training programs. San Francisco: Berrett-Koehler Publishers; 1994.
Covidence <https://www.covidence.org/reviews/active>. Accessed 27 Feb 2018.
Gunasingam N, Burns K, Edwards J, Dinh M, Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J. 2015;91:182–7.
McCue JD, Sachs CL. A stress management workshop improves residents’ coping skills. Arch Intern Med. 1991;151:2273–7.
Milstein JM, Raingruber BJ, Bennett SH, Kon AA, Winn CA, Paterniti DA. Burnout assessment in house officers: evaluation of an intervention to reduce stress. Med Teach. 2009;31:375–8.
Palamara K, Kauffman C, Stone VE, Bazari H, Donelan K. Promoting success: a professional development coaching program for interns in medicine. J Grad Med Educ. 2015;7:630–7.
Runyan C, Savageau JA, Potts S, Weinreb L. Impact of a family medicine resident wellness curriculum: a feasibility study. Med Educ Online. 2016;21:30648.
Weight CJ, Sellon JL, Lessard-Anderson CR, Shanafelt TD, Olsen KD, Laskowski ER. Physical activity, quality of life, and burnout among physician trainees: the effect of a team-based, incentivized exercise program. Mayo Clin Proc. 2013;88:1435–42.
Ospina-Kammerer V, Figley CR. An evaluation of the respiratory one method (ROM) in reducing emotional exhaustion among family physician residents. Int J Emerg Ment Health. 2003;5:29–32.
Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual. 3rd ed. Palo Alto: Consulting Psychologists Press; 1996.
Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–11.
Linzer M, Levine R, Meltzer D, Poplau S, Warde C, West CP. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. 2014;29(1):18–20.
Shanafelt TD, Dyrbye LN, Sinsky C, Hasan O, Satele D, Sloan J, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836–48.
Trockel M, Bohman B, Lesure E, Hamidi MS, Welle D, Roberts L, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. 2018;42(1):11–24.
Ripp JA, Privitera MR, West CP, Leiter R, Logio L, Shapiro J, et al. Well-being in graduate medical education: a call for action. Acad Med. 2017;92:914–7.
Funding/Support
This project was made possible with a Mapping the Landscape, Journeying Together grant from the Arnold P. Gold Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors determined that IRB approval was not applicable as this is a systematic review of previously published studies.
Disclosures
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Walsh, A.L., Lehmann, S., Zabinski, J. et al. Interventions to Prevent and Reduce Burnout Among Undergraduate and Graduate Medical Education Trainees: a Systematic Review. Acad Psychiatry 43, 386–395 (2019). https://doi.org/10.1007/s40596-019-01023-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40596-019-01023-z