Abstract
Purpose of Review
Consumption of wild game meat is traditionally associated with rural, remote and poor areas around the world, but there has been a recent rise in the consumption of wild game meat in urban and higher socio-economic regions such as Australia. Along with its unique animal fauna, Australia has a wide diversity of feral animals, many of which are hunted for food, although little is known about the levels of consumption of this meat across Australia. Corresponding with this is the lack of information on the parasites within these animals, particularly those of potential zoonotic concern through the consumption of raw or undercooked meat and organs. This review aimed to determine the level of knowledge of parasites of feral animals regularly consumed in Australia.
Recent Findings
Online databases were searched for publications on feral animals and their parasites. For the purpose of this review, only protozoal and helminth parasites that infest the muscle and organ systems and are infective to humans upon ingestion were considered as potential zoonotic parasites. A total of 5 records were found based on host and 27 based on parasite, showing a lack of information available.
Summary
Little information was available on the parasites of the major groups of feral animals hunted in Australia for food (pigs, deer, rabbits and hares, and goats) as well as on the parasites themselves, except for sparganosis caused by the cestode Spirometra erinaceieuropaei which has been widely reported in feral pigs. Sparganosis appears to be an underreported disease in Australia, with only 8 confirmed cases, highlighting the need for education of medical practitioners, especially in rural and remote areas, on the diagnosis of this infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Australia is well known for its unique animal fauna, but also has at least 25 species of exotic mammals, both domestic and wild [1]. A number of the domestic species escaped or were deliberately released into the wild and are now living as established feral populations, including pigs, goats, buffalo, camels and cattle. Although wild game meat is more commonly eaten in many rural, remote and/or poor areas around the world [2], there has been a recent increase in the consumption of wild game meat in urban and higher socio-economic regions [2,3,4,5] such as Australia. Wild game meat is considered rich in nutrients, low in fat and is usually sustainably sourced [3, 6, 7] which, along with the environmental benefits of removing feral species from the environment, has helped increase levels of consumption in Australia [3, 8].
Within Australia, however, the ecological impacts associated with feral animals are often considered of greater importance than the potential health risks via consumption and/or association with those animals [3, 4, 9], even though some, such as feral pigs, are known to be commonly infected with parasites [10]. Consumption of wild game in Australia has altered substantially over the last 250 years. Indigenous Australians have always hunted and consumed wild (native) game and adapted to the release of feral species with their inclusion in hunting practices [3, 9]. Following their arrival in Australia, early colonists were heavily reliant on wild game while livestock became established and subsequently released many of these (e.g. pigs) into the wild for hunting [3]. However, over time, meat from wild animals became “not socially acceptable” [11], especially following the 1930s Great Depression when wild-caught rabbits were a major food item and were subsequently stigmatised and associated with poverty [3]. Recent changes in Australian society, especially the arrival of immigrants and refugees from a wide variety of countries, many of whom consider rabbit, for example, a delicacy, has led to a return of rabbit meat to butchers in some areas [1, 3]. The different cultural traditions with different styles of food preparation which may involve minimal or no cooking of meat and/or organs [12] may, however, lead to increased risks of zoonotic parasites, such as that reported in parts of Europe in recent years [6, 7].
Zoonotic parasites and their associated diseases are well known throughout many parts of the world, where they are a major burden on public health and wellbeing [13,14,15,16], although there are limited data on the specific pathogens found in most wild game meat [5, 6]. Within Australia, the study of parasites of wild animals has an opportunistic and sporadic history, with the study of parasites of wildlife, in general, not perceived as being of great social benefit and generally limited to those only with potential impacts on livestock [17].
Outbreaks of illness and death from diseases caused by contaminated food are a constant threat but often go unrecognized, unreported or not investigated until they are a major visible public health or economic issue [18]. Australia (and its neighbouring countries in the Western Pacific) has a very low global burden of foodborne diseases [18] based on the available literature. The increased utilisation of feral game meat includes the potential risk of infection through the handling and butchering of the animal, as well as from the consumption of raw or poorly cooked meat and organs [2, 5, 19, 20]. Wildlife Health Australia listed various disease risks from feral animals in Australia, with feral pigs harbouring the majority of risks, but only the cestode Spirometra was listed as a risk able to be transmitted by the consumption of meat [21], although the Victorian Government stated that the diseases and pathogens of feral animals could present a food safety risk unless mitigating procedures were adopted and implemented [22]. However, recent research on zoonotic parasites in seafood in Australia has shown underreporting of human infections due to a combination of poor diagnostic techniques and lack of knowledge among members of the public as well as medical practitioners [23].
The aim of this review is to identify what was known with regard to parasites of feral animals that are regularly consumed in Australia and any parasites that may be transmitted via consumption of their meat and/or organs to determine levels of potential risk.
Literature Review
Methodology
The four major feral animal types that are commonly consumed in Australia are pigs (Sus scrofa), deer (Cervus elaphus, Cervus timorensis, Cervus unicolor, Dama dama, Axis axis and Axis porcinus), rabbits (Oryctolagus cuniculus) and hares (Lepus capensis), and goats (Capra hircus). Although the meat of other feral animals, such as camels (Camelus dromedarius) [24] and water buffalo (Bubalus bubalis) [25], are also consumed in Australia, this is generally within limited community groups and were not considered within this review. For the purpose of this review, only protozoal and helminth parasites that infest the muscle and organ (e.g. heart, liver and kidney) systems and are infective to humans upon ingestion were considered as potential zoonotic parasites.
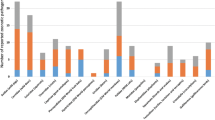
A review of publications on feral animals and their parasites was conducted using online databases (CAB, PubMed and Web of Science); a search of the disease reporting database, ProMed, did not return any results. The Boolean search phrase used included the host information (“pig OR Sus OR Suidae”; “deer OR Cervus OR Dama OR Axis OR Cervidae”; “rabbit OR hare OR Oryctolagus OR Lepus OR Leporidae”; “goat OR Capra OR Bovidae”) in combination with “AND zoono* (to cover zoonosis, zoonoses and zoonotic) AND parasit* (to cover parasite, parasitism and parasitic) AND Australia AND food”. The PRISMA guidelines were followed to remove duplicate records and records that could not be retrieved (Online Resource 1A-D). Of the remaining records eligible for assessment, records that did not report Australian feral animals were then excluded. Finally, the remaining records were read to assess their content for inclusion. This was conducted individually by host species group.
A subsequent review of publications on zoonotic parasites in Australia was conducted using the same three online databases. The five most important meat-borne zoonotic parasites around the world are Toxoplasma gondii, Sarcocystis spp., Trichinella spp., Spirometra spp. and Taenia spp. [18, 26]; recent research conducted by our laboratory has also reported infections of the zoonotic pentastome, Linguatula serrata, in Australia [27]. The Boolean search phrase used included the parasite or disease name (“Sarcocyst*” (to cover Sarcocystis and sarcocystiosis); “Toxoplasm*” (to cover Toxoplasma and toxoplasmosis); “Spirometra OR Spargan*” (to cover spargana, sparganid and sparganosis); “Trichin*” (to cover Trichinella and trichinosis); “Taenia OR cysticer*” (to cover cyticercus and cyticercosis); “Linguatula OR pentastom*” (to cover pentastome, pentasomid and pentastomiasis)) in combination with “AND Australia AND feral”. The PRISMA guidelines were followed as outlined above individually by parasite type (Online Resource 1E-I).
The hosts
Pigs
A total of 39 records were found across the three databases; following assessment, 8 records remained. Of these eight records, only one specifically dealt with zoonotic parasites of Australian wildlife [28]. Spratt [28] listed sparganosis (caused by Spirometra erinaceieuropaei), pentastomiasis (caused by pentastomes of the genera Armillifer and Linguatula) and toxoplasmosis (caused by T. gondii) as potential zoonotic parasites but did not list any known cases of infection. Kelly [29] reviewed potential zoonotic parasites in Australia, referring to sparganosis being of importance where feral pigs were fattened for human consumption with a high prevalence of infection in many areas. Taenia solium and Trichinella spiralis were also listed as potential problems but both, despite widespread global distributions, were not endemic in Australia [29]. Sporadic reports of T. solium in pigs (as Cysticercus cellulosae) at slaughter had been made, while human infections in Australia with T. spiralis were usually acquired from imported pork products [29]. The remaining records primarily dealt with reviews of trichinellosis and listed the few reports of Trichinella spp. previously reported in wildlife in Australia, with no human infections [30,31,32]. VanderWaal and Deen [33] provided information on the changing epidemiology of a variety of infectious diseases of swine worldwide, concentrating on farmed animals. Of the 40 pathogens identified, only 3 were zoonotic parasites transmitted via consumption of infected meat or organs: Trichinella spp., T. solium and T. gondii [33].
Deer
As only two records were obtained using the full search phrase, and both were deemed unsuitable, “food” was removed and the search re-run. A total of 23 records were obtained using this shortened search phrase; however, following assessment, no records were deemed suitable for inclusion.
Goats
A total of 26 records were found across the three databases; following assessment, 2 records remained. Both dealt with infections within production animals [34, 35], rather than feral goats, but given that large numbers of feral goats are “domesticated” to become rangeland goats for future meat production, they were considered relevant to this review. A 34% antibody level in the population (in the State of South Australia) for Sarcocystis spp., which is a potential zoonotic parasite transmitted by ingestion of infected meat, was found in one study [34]. Echinoccocus and Fasciola were listed as potential zoonotic risks [35], but infection with both does not involve the consumption of infected goat meat. The only other zoonotic parasite mentioned was Trichinella and its absence from Australia [35].
Rabbits and Hares
As only three records were obtained using the full search phrase, of which two were deemed unsuitable and the third was unobtainable, “food” was removed and the search re-run. A total of 48 records were obtained using this shortened search phrase; following assessment, 2 records remained. Eight rabbits and a single European hare (as well as a feral pig and goat, but this reference did not appear in those searches) were examined for larval stages of the zoonotic pentastomid Linguatula serrata; none was infected [27]. The health impacts of feral mammals on humans were reviewed, including potential zoonotic parasites where hares were infected with Toxoplasma, but no specific details of the geographical location were provided [1].
The Parasites
Trichinella
A total of 8 records were obtained for infection with Trichinella in Australian feral animals; following assessment, three records remained, all of which were general reviews of Trichinella [32] or pig-borne diseases in general [4, 36]. Although the known zoonotic species, Trichinella spiralis, has yet to be reported from Australia, both T. pseudospiralis and T. papuae have been reported from various mammals, although only T. papuae was reported from pigs, but not from mainland Australia [32].
Previous reports of human infections within Australia by nematodes within muscle tissues were initially diagnosed as T. pseudospiralis [30]. However, this has been shown to be a misidentification, with Haycocknema perplexum the actual parasite [37]. This parasite has only been reported from Australia (either in northern Queensland or Tasmania) with 13 known cases, all with an unknown source of infection [37]. Each case had some association with wildlife, but not all consumed wild game meat, although this has not been ruled out as a potential risk factor [37].
Linguatula
Only three reports were obtained discussing infection with Linguatula serrata in feral animals [27, 38, 39]. After documenting the widespread occurrence of L. serrata in wild dogs and foxes in the highlands of southern Australia, but not being able to find infection within a range of potential intermediate hosts, including rabbits, hares and pigs [27], intermediate stages were subsequently found in the liver and lung tissues of rabbits [39] and the mesenteric lymph node of a feral goat (identified as Linguatula sp.; 38).
Spirometra (Sparganosis)
A total of 34 records were obtained for infection with Spirometra erinacei/erinaceieuropaei or sparganosis in feral animals in Australia; following assessment, 8 remained for inclusion. The majority of the references excluded were detailing the infection of Spirometra in definitive hosts (cats, foxes and wild dogs) without mention of hunted feral animals as prey items [40,41,42,43,44]. The remaining records all detailed sparganosis infection in feral pigs, with specific mention of potential human health risks from consumption.
Sparganosis in feral pigs occurs along the eastern edge of Australia (from tropical north Queensland to Victoria) [45,46,47]. Given that the distributions of foxes, wild dogs and feral cats overlap with pigs across most of their distribution, it is likely that spargana could occur in feral pigs wherever they are found in Australia. Indeed, carcasses of feral pigs were commonly condemned at abattoirs due to infection with spargana [10, 48]. Rates of condemnation were usually over 50%, but this differed between geographical location and year, with infection levels of spargana in adult feral sows corresponding with good seasonal conditions [49]. Standard meat inspection procedures, however, often failed to find spargana in deep muscles which would lead to an underreporting of infection levels [49].
The initial report of spargana in the muscle of feral pigs that had been caught and kept to be fattened for later slaughter was documented in further detail by Bearup [48] in a description of the life cycle. Spargana were most commonly found under the perinoneum of the abdominal wall and diaphragm but were also found in the connective tissue between muscles in almost every region of the body [45, 48].
Despite these high levels of infection in feral pigs, only 8 cases of human sparganosis have so far been reported in Australia, which is most likely due to misdiagnosis of infection [50]. Most cases reported in Australia are subcutaneous sparganosis in Australian-born people who have never travelled overseas [48, 50]. These cases were most likely acquired through the consumption of infected copepods (first intermediate hosts) in unfiltered water; however, one case reported consumption of wild pigs and rabbits [50]. Subcutaneous infections generally present as a small tumour or lump, which are often misdiagnosed [45, 48, 50] until excised and identified [50]. An experimental infection produced oedema and erythema accompanied by chills and fever caused by the migration of spargana [48]. Worldwide, cerebrospinal sparganosis is the most common infection, accounting for approximately 25% of all cases; the only report of cerebral sparganosis in Australia was from an East Timor refugee [50].
Spargana left in situ in a pig carcass for 24 h at room temperature were viable and infective to dogs and cats and could remain viable for up to 14 days in a domestic refrigerator [45]. Freezing at − 8 °C for 24 h [45] or cooking at a temperature of at least 80 °C for a few minutes [49] was considered sufficient to kill sparagana in tissues. Infection in people in Australia is likely to be low risk due to most Australians cooking pig meat thoroughly, although “immigrants from some European countries are accustomed to eating raw pork in various dishes” and would be more susceptible to infection [45].
Sparganosis is likely an under-recognised zoonotic disease in the Australian population and, as all the native Australian cases occurred in rural settings, this highlighted the need for rural and remote health practitioners to be aware of this disease [50].
Taenia solium
A total of 32 records were obtained for Taenia infection; following assessment, 1 remained for inclusion which did not include T. solium as a parasite of feral pigs in Australia [49]. Most of the references that were obtained dealt with other species of Taenia that utilise dogs and cats as definitive hosts.
Toxoplasma gondii
A total of 73 records were obtained for T. gondii infection; following assessment, 3 remained for inclusion. The majority of records that were excluded were only reporting prevalence of infection in feral cats in different regions of Australia, mostly showing high prevalence of infection in areas where cat populations are high [51, 52]. The records that did mention feral animals that are consumed by humans all had negative results for the presence of T. gondii and/or its antibodies, although for most studies, numbers of examined animals were usually low, and the study took place in a single geographical location. Rabbits were found to be uninfected in Western Australia (n = 57) [53] and Queensland (n = 4) [54], while fallow deer (n = 2) and feral goats (n = 5) were also uninfected in Tasmania and Queensland, respectively [55].
Sarcocystis
A total of 17 records were obtained for Sarcocystis in feral animals in Australia; following assessment, 9 remained for inclusion. The majority of these references did not refer to feral game for consumption but were detailing prevalence of infection in definitive hosts (primarily cats) which presents information on risk of infection in local animals exposed to infective stages [44, 56,57,58,59,60]. A survey of feral goats slaughtered at abattoirs in South Australia found that there were a significant proportion of the goats, from all regions in South Australia, infected with the microscopic sarcocysts in a variety of tissues, including skeletal muscles [61]. Although the cost of Sarcocystis infection to the production animal industry is large (almost AU$2 million annually from carcass condemnation and meat trimming), no human infections have yet been reported [60]. As there are a number of species of Sarcocystis that infect animals in Australia, it is possible that none is pathogenic to people; however, only one study appears to have tested this hypothesis [62]. Human volunteers were fed either microscopic or macroscopic Sarcocystis cysts collected from sheep muscle, but all tested negative for infection after 60 days [62]. In comparison, macroscopic cysts were found to infect cats, and microscopic cysts were found to infect dogs and foxes after the same time period [62]. Areas with high cat densities correlate to areas with high levels of infection in production animals [59, 60]; however, there has been no corresponding survey of wildlife in these areas to determine impacts of cat density on levels of infection.
Conclusions
There are currently large gaps in the knowledge regarding zoonotic parasites in feral game meat and offal in Australia due to insufficient surveillance of wild animals [1, 14, 17, 63]. This partial and fragmentary knowledge of the potential impacts of consuming introduced and feral animals on human health prevents a proper evaluation of the potential risks and the identification of priorities for managing and preventing them to be undertaken [1]. Changes in the environment and livestock production processes present new risks for the emergence of parasitic zoonoses [13, 15, 32, 36, 63]. Globalization of food supply, increased international travel, increase of population of highly susceptible persons and changes in culinary habits have led to increased diagnoses of food-borne parasitic diseases worldwide [1, 18, 26, 63].
Although there are several wild animals, both native and introduced, that are regularly harvested, either recreationally or commercially, for consumption in both domestic and international markets, little is known about the levels of wildlife harvesting in Australia [8]. Environmental and welfare concerns regarding production animal practices and the ecological benefits of the removal of feral animals from the environment are large reasons that have helped increase levels of consumption of feral game in some areas of Australia [3, 8]. Confusingly, each state and territory within Australia has different regulations depending on the “status” of the animal in question. For example, in Victoria, feral deer are recognised as “game” species and are subject to harvest monitoring by the Victorian State Government, whereas other feral mammals, such as pigs, goats and rabbits, are considered as “pests” and are thus not monitored as stringently [8]. Although there are quite strict regulations for the export of feral game meat, with required levels of formal meat inspection, there are fewer restrictions on the movement and consumption of feral game meat within Australia, where it may be banned from sale but can be given away [4]. As such, families and friends of recreational hunters are the people most likely to consume feral game meat on a regular basis [6, 7]. The processing of carcasses, which usually occurs in the field (20% of surveyed hunters in Spain; [7]) or under home conditions can lead to an increased risk of infection due to the time elapsed between animal death and butchering as well as the conditions of dressing and cooling impacting meat health [7, 46].
It is apparent from this review that there is little information available on the parasites of most of the feral animals regularly consumed in Australia. And, for those that do have information, most is out-dated in terms of their current distributions and potential risks. Rabbits and hares were relatively well studied for parasites as potential biological control agents [17], and feral pigs have had sporadic and generally localised reports of parasites [47], but there has been no systematic survey of pigs in areas of hunting in recent years, although the risk of introduction of diseases such as African Swine Fever has led to an increased interest in diseases of feral pigs [64, 65]. Feral deer and goats have had very limited studies with respect to parasite infections, although deer are increasingly hunted for game meat [8] and goats are routinely captured for consumption either domestically or internationally [38]. Priority needs to be directed towards systematic surveys of these animals, in collaboration with local hunter and pest control groups, to determine zoonotic parasite risk from consumption of meat, especially if undercooked.
Although the range of known zoonotic parasites identified from feral animals in Australia is low, this does not preclude risks of infection from the consumption of feral game meat. The presence of the zoonotic pentastome, L. serrata, was considered rare until recent work showed high levels of infection in definitive hosts in south-eastern Australia [27], an area of high populations of hunters of feral game. Thus, it should not be assumed that lack of information equates to a lack of infection as many wildlife species have not been systematically surveyed for parasites across large areas of Australia.
There are a number of known zoonotic parasites that do not yet appear to be endemic in Australia, including T. solium and species of Trichinella, although they are endemic in neighbouring countries [66]. There are various reports of T. solium being introduced to Australia via immigrants, but it has never established [67]. Trichinella papuae has been reported from feral pigs on islands in the Torres Strait between Australia and Papua New Guinea [32]; travel between these islands and the Australian mainland is not well regulated, and the risk of introduction to mainland Australia remains constant. Stringent border control preventing the illegal importation of meat [68] and increased awareness of these parasites and their associated diseases [50] are needed to prevent their introduction to Australia.
Similar to the pleas regarding seafood, education is needed with respect to potential zoonotic parasites in feral animals consumed for food in Australia [23]. Hunters and consumers need to be aware of safe meat hygiene and potential risks, and medical practitioners need to be educated about meat-borne parasitic diseases for diagnosis of possible infections. The Game Hunters Association of Australia and the Australian Deer Association, for example, run courses for recreational hunters which includes break down of carcasses as well as meat care. However, Government-level public health authorities should increase interest in topics regarding consumption of feral game meat and provide formal training in good hygiene practices during all steps of feral game meat preparation and handling [7]. In addition, diagnostic tests and laboratory personnel need to be educated for accurate diagnosis and identification of these parasites. Infection with T. gondii is often under-diagnosed and underreported, although there are some indications that it is more common in remote Indigenous communities [60]. Toxoplasma gondii is common and widely distributed among Australian native fauna, isolated from over 25 species of native mammals and birds with prevalence ranging from 40 to 100% and a number of different strains [15]; infection levels in feral wildlife remains unknown.
An increased consumption of feral game meat in Australia has exacerbated the zoonotic potential of parasites of wildlife [8, 28]. In Spain, hunters of game animals must have a veterinary inspection of their meat if they are selling it, but they do not yet require one for self-consumption [7]. Traditional post mortem inspection techniques in Australian abattoirs were adapted from techniques developed in Europe and North America to control important zoonotic diseases including taeniasis and trichinosis [69]. However, considerable improvement in animal health status among production animals has led to eradication of many of these significant zoonoses within production animals, leading to modifications in post-mortem inspection techniques [69]. However, these may need to be reintroduced for examination of feral game meat carcasses.
Data Availability
Data is available from the corresponding author upon reasonable request.
References
Capizzi D, Monaco A, Genovesi P, Scalera R, Carnevali L. Impact of alien mammals on human health. In: Mazza G, Tricarico E, editors. Invasive Species and Human Health. 10. Wallingford: CAB International; 2018. p. 190–215.
Kurpiers L, Schulte-Herbruggen B, Ejotre I, Reeder D. Bushmeat and emerging infectious diseases: lessons from Africa. In: Angelici F, editor. Problematic wildlife a cross-disciplinary approach. Switzerland: Springer International Publishing; 2016. p. 507–52.
Gresier C. Going feral: wild meat consumption and the uncanny in Melbourne Australia. Aust J Anthropol. 2015;27:49–65.
Gibbs EPJ. The public health risks associated with wild and feral swine. Revue Scientifique et Téchnique - Office International des Épizooties. 1997;16:594–8.
Engel L, Hamedy A, Koethe M. Direct detection and quantifcation of Toxoplasma gondii in meat samples from feral raccoons (Procyon lotor) in Germany by magnetic-capture real-time PCR. Parasitol Res. 2023;122:307–13.
Bundesinstitut für Risikobewertung. Game meat: health assessment of human-pathogenic parasites. German Federal Institute for Risk Assessment; 2018. p. 42pp. Available from https://www.bfr.bund.de/cm/349/game-meat-health-assessment-of-human-pathogenic-parasites.pdf.
Lizana V, Muniesa A, Cardells J, López-Ramon J, Aguiló-Gisbert J, Lomillos JM, et al. Safe game: hygienic habits in self-consumption of game meat in eastern Spain. Foods. 2022;11:368.
Moloney PD, Gormley AM, Toop SD, Flesch JS, Forsyth DM, Ramsey DSL, et al. Bayesian modelling reveals differences in long-term trends in the harvest of native and introduced species by recreational hunters in Australia. Wildl Res. 2022;49:673–85.
Koichi K, Sangha K, Cottrell A, Gordon I. Aboriginal Ranger’s perspectives on feral pigs: are they a pest or a resource? A case study in the Wet Tropics World Heritage Area of northern Queensland. J Aust Indigenous Issues. 2013;15:2019.
Baldock FC, Hopkins TJ. Spirometra erinacei in cats and dogs in Australia. Proceedings of the 53rd Annual Conference of the Australian Veterinary Association 1976:87–8.
Izac A-M, O’Brien P. Conflict, uncertainty and risk in feral pig management: an Australian approach. J Environ Manage. 1991;32:1–18.
Davies N. The zoonotic potential of Tasmanian wildlife [Master of Medical Science]. Department of Pathology: University of Tasmania; 1995.
Conlan JV, Sripa B, Attwood S, Newton PN. A review of parasitic zoonoses in a changing Southeast Asia. Vet Parasitol. 2011;182:22–40.
Cantlay J, Ingram D, Meredith A. A review of zoonotic infection risks associated with the wild meat trade in Malaysia. EcoHealth. 2017;14:361–88.
Thompson RCA, Conlan JV. Emerging issues and parasite zoonoses in the SE Asian and Australasian region. Vet Parasitol. 2011;181:69–73.
Mathison BA, Sapp SGH. An annotated checklist of the eukaryotic parasites of humans, exclusive of fungi and algae. Zookeys. 2021;1069:1–313.
Spratt DM, Beveridge I. Wildlife Parasitology in Australia: past, present and future. Aust J Zool. 2018;66:286–305.
Havelaar AH, Kirk MD, Torgerson PR, Gibb HJ, Hald T, Lake RJ, et al. World Health Organization global estimates and regional comparisons of the burden of foodborne disease in 2010. Plos Med. 2015;12(12):e1001923.
Meng X, Lindsay D, Sriranganatham N. Wild boars as sources for infectious diseases in livestock and humans. Philos Trans R Soc B. 2009;364:2697–707.
Khan S, Atanasova K, Krueger W, Ramirez A, Gray G. Epidemiology, geographical distribution, and economic consequences of swine zoonoses: a narrative review. Emerg Microbes Infect. 2013;2:1–11.
Wildlife Health Australia. Disease agents reported in feral animals in Australia. Wildlife Health Australia; 2013. p. 10. Available from https://wildlifehealthaustralia.com.au/FactSheets.
Chief Veterinary Officer's Unit. Review of of diseases and pathogens of invasive animals that may present food safety and human health risks. Agriculture Victoria; 2016. p. 26pp.
Shamsi S, Sheorey H. Seafood-borne parasitic diseases in Australia: are they rare or underdiagnosed? Intern Med J. 2018;48(5):591–6.
Tan ETT, Ng JC, Al Jassim R, D’Arcy BR, Netzel G, Fletcher MT. Emerging food safety risk of hepatoxic indospicine in feral Australian camel meat. Food Control. 2020;113:107205.
Lemcke B. Water buffalo handling: property to abattoir. Part 1. General Principles. Report No. J63. Northern Territory Government. Darwin; 2015. p 4.
Dorny P, Praet N, Deckers N, Gabriel S. Emerging food-borne parasites. Vet Parasitol. 2009;163:196–206.
Shamsi S, McSpadden K, Baker S, Jenkins DJ. Occurrence of tongue worm, Linguatula cf. serrata (Pentastomida: Linguatulidae) in wild canids and livestock in south-eastern Australia. Int J Parasitol: Parasites Wildlife. 2017;6:271–7.
Spratt DM. Zoonotic tissue parasites of Australian wildlife (Special Issue: Parasitic infections.). Microbiology Australia. 2016;37(1):12–4.
Kelly JD. Anthropozoonotic helminthiases in Australia: the role of animals in disease transmission. Part 1. Meat and offal-borne anthropozoonoses. Part 2. Anthropozoonoses associated with domesticated and domiciliated vertebrates. Int J Zoonoses. 1974;1(1):1–12.
Pozio E. Trichinella pseudospiralis an elusive nematode. Vet Parasitol. 2016;231:97–101.
Borza C, Kundnani NR, Darabus G, Mederle N, Pascu C, Abhinav S, et al. Trichinellosis: A constant presents worldwide involved in the public health. Revista Romana De Medicina Veterinara. 2021;31(2):92–6.
Crisostomo-Jorquera V, Landaeta-Aqueveque C. The genus Trichinella and its presence in wildlife worldwide: a review. Transbound Emerg Dis. 2022;69(5):e1269–79.
VanderWaal K, Deen J. Global trends in infectious diseases of swine. Proc Natl Acad Sci USA. 2018;115:11495–500.
Murrell TG, O’Donoghue PJ, Ellis T. A review of the sheep-multiple sclerosis connection. Med Hypotheses. 1986;19(1):27–39.
Adams DB, Butler RJ, Nicholls TJ. Public health hazards of meat from small ruminants: the perspective of Australia. Revue Scientifique et Téchnique - Office International des Épizooties. 1997;16(2):433–40.
Pappas G. Socio-economic, industrial and cultural parameters of pig-borne infections. Clin Microbiol Infect. 2013;19:605–10.
Pritt BS, Mathison BA, Bradbury RS, Liewluck T, Nicolau S, O’Horo JC, et al. Imported Haycocknema perplexum Infection, United States. Emerg Infect Dis. 2022;28:2281–4.
Barton DP, Shackelford B, Shamsi S, Jenkins D. Are feral goats intermediate hosts for Linguatula (Pentastomida) in Australia? Int J Parasitol: Parasites Wildlife. 2022;18:283–6.
Barton DP, Baker A, Porter M, Zhu X, Jenkins DJ, Shamsi S. Verification of rabbits as intermediate hosts for Linguatula serrata (Pentastomida) in Australia. Parasitol Res. 2020;119:1552–62.
Coman BJ. Helminth parasites of the dingo and feral dog in Victoria with some notes on the diet of the host. Aust Vet J. 1972;48(8):456–61.
Coman BJ. A survey of the gastro-intestinal parasites of the feral cat in Victoria. Aust Vet J. 1972;48(4):133–6.
Coman BJ, Jones EH, Driesen MA. Helminth parasites and arthropods of feral cats. Aust Vet J. 1981;57(7):324–7.
Ryan GE. Gastro-intestinal parasites of feral cats in New South Wales. Aust Vet J. 1976;52(5):224–7.
O’Callaghan M, Reddin J, Lehmann D. Helminth and protozoan parasites of feral cats from Kangaroo Island. Trans Royal Soc South Austr Inc. 2005;129(1):81–3.
Gordon HM, Forsyte BA, Robinson M. Sparganosis in feral pigs in New South Wales. Aust Vet J. 1954;30:135–8.
Appleton PL, Norton JH. Sparganosis: a parasitic problem in feral pigs. Queensland Agric J. 1976;102(4):339–43.
Pavlov PM. Health risks to humans and domestic livestock posed by feral pigs (Sus scrofa). Proc Vertebr Pest Conf No. 1988;13(13):141–4.
Bearup AJ. Life history of a spirometrid tapeworm, causing sparganosis in feral pigs. Aust Vet J. 1953;29:217–24.
Giles JR. Public health, pathology and parasitology of feral pigs. Australian Veterinary Association Yearbook. 1981:289–92.
Tran Q, Tran MC, Mehanna D. Sparganosis: an under-recognised zoonosis in Australia? BMJ Case Rep. 2019;12(5):4.
Adriaanse K, Firestone SM, Lynch M, Rendall AR, Sutherland DR, Hufschmid J, et al. Comparison of the modified agglutination test and real-time PCR for detection of Toxoplasma gondii exposure in feral cats from Phillip Island, Australia, and risk factors associated with infection. Int J Parasitol: Parasites Wildlife. 2020;12:126–33.
Taggart PL, Caraguel CGB, McAllister MM. Fractional seroprevalence rates in common prey species can cause more than half of feral cats to be exposed to Toxoplasma gondii annually. Vet Parasitol. 2020;288:109306.
Jakob-Hoff RM, Dunsmore JD. Epidemiological aspects of toxoplasmosis in southern Western Australia. Aust Vet J. 1983;60(7):217–8.
Ross AK, Lowry J, Elphinstone A, Lawes JC. Toxoplasma gondii seroprevalence in endangered bridled nailtail wallabies and co-occurring species. Austr Mammal. 2020;42(2):167–70.
Smith ID, Munday BL. Observations on the incidence of Toxoplasma gondii in native and introduced feral fauna in eastern Australia. Aust Vet J. 1965;41:285–6.
Gregory GG, Munday BL. Internal parasites of feral cats from the Tasmanian Midlands and King Island. Aust Vet J. 1976;52(7):317–20.
Munday BL, Mason RW, Hartley WJ, Presidente PJA, Obendorf D. Sarcocystis and related organisms in Australian wildlife: I. Survey findings in mammals. J Wildl Dis. 1978;14(4):417–33.
Archer JF, Walker KH. Sarcosporidiosis - research sheds new light on an old problem in the sheep industry. Agric Gazette. 1979;90(3):11–3.
Taggart PL, Stevenson MA, Firestone SM, McAllister MM, Caraguel CGB. Spatial analysis of a cat-borne disease reveals that soil pH and clay content are risk factors for sarcocystosis in sheep. Front Vet Sci. 2019;6:00127.
Legge S, Taggart PL, Dickman CR, Read JL, Woinarski JCZ. Cat-dependent diseases cost Australia AU$6 billion per year through impacts on human health and livestock production. (Special Issue: Cat ecology, impacts and management in Australia.). Wildlife Res. 2020;47(7/8):731-46.
Hein WR, Cargill CF. An abattoir survey of diseases of feral goats. Aust Vet J. 1981;57(11):498–503.
Ford GE. Role of the dog, fox, cat and human as carnivore vectors in the transmission of the Sarcosporidia that affect sheep meat production. Aust J Agric Res. 1986;37(1):79–88.
Lustigman S, Prichard RK, Gazzinelli A, Grant WN, Boatin BA, McCarthy JS, et al. A Research Agenda for Helminth Diseases of Humans: The Problem of Helminthiases. Plos Negl Trop Dis. 2012;6(4):13.
Bengsen A, Gentle M, Mitchell J, Pearson H, Saunders G. Feral pig management in Australia: current trends and future directions. In: Timm R, O'Brien J, editors. 26th Vertebrate Pest Conference: University of California, Davis; 2014. p. 281–6.
Bengsen A, West P, Krull C. Feral pigs in Australia and New Zealand: range, trend, management, and impacts of an invasive species. In: Melletti M, Meijaard E, editors. Ecology, Conservation and Management of Wild Pigs and Peccaries. Part III - Conservation and Management: Cambridge University Press; 2017. p. 325–38.
Owen IL. Parasites of animals in Papua New Guinea recorded at the National Veterinary Laboratory: a catalogue, historical review and zoogeographical affiliations. Zootaxa. 2011;3143:10163.
Sandars DF. Taenia solium, the pork tapeworm, Australia. Med J Aust. 1958;45(18):607–8.
Beltran-Alcrudo D, Falco J, Raizman E, Dietze K. Transboundary spread of pig diseases: the role of international trade and travel. BMC Vet Res. 2019;15:64.
Pointon A, Hamilton D, Kiermeier A. Assessment of the post-mortem inspection of beef, sheep, goats and pigs in Australia: approach and qualitative risk-based results. Food Control. 2018;90:222–32.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study concept and design. Initial literature search and review undertaken by Diane Barton; secondary literature review undertaken by Shokoofeh Shamsi. The first draft of the manuscript was written by Diane Barton, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This is a review paper. No ethical approvals and informed consent is required.
Conflict of Interest
Shokoofeh Shamsi is a section editor for this Journal. There are no competing interests among the remaining authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
40588_2023_193_MOESM1_ESM.pdf
Supplementary file1 (PDF 209 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barton, D.P., Fahey, H., Jenkins, D.J. et al. Zoonotic Parasites in Feral Animals Commonly Consumed in Australia — Is There a Risk?. Curr Clin Micro Rpt 10, 66–73 (2023). https://doi.org/10.1007/s40588-023-00193-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40588-023-00193-7