Abstract
Purpose of Review
Although many environmental exposures (e.g., air pollution) are geographically patterned and persist as a result of historic economic policies (e.g., redlining), the impact of reproductive and social policies on maternal and child health remains incompletely understood. Reproductive and social policies are increasingly important for maternal and child health equity, particularly following the 2022 US Supreme Court decision in Dobbs v Jackson Women’s Health Organization (“Dobbs decision”), which restricted access to abortion. Here, we summarize the literature from original research studies examining influences of reproductive and social policy on maternal and child health, focusing on impacts on adverse birth outcomes and policies as sources of stress.
Recent Findings
Several studies suggest that those most impacted by the Dobbs decision are younger, non-white, socioeconomically disadvantaged, and living in states with less access to government safety net programs, all of which are compounded by environmental injustices. Further, studies conducted in the wake of the Dobbs decision find elevated stress levels among women of reproductive age. This may represent one pathway leading to adverse birth outcomes, as epidemiologic studies demonstrate that preterm birth rates increased following the 2016 election, a period of heightened stress.
Summary
Reproductive and social policies are understudied contributors to adverse outcomes for reproductive-aged women and their children. This has important implications for maternal and child health equity, as those who will be the most impacted by reproductive and social policies already experience the highest rates of adverse birth outcomes and environmental toxicant exposure.


Similar content being viewed by others
Data Availability
No datasets were generated or analyzed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Douthard RA, Martin IK, Chapple-McGruder T, Langer A, Chang SUS. Maternal mortality within a global context: historical trends, current state, and future directions. J Women’s Health. 2021;30(2):168–77.
Petersen EE, Davis NL, Goodman D, Cox S, Syverson C, Seed K, et al. Racial/Ethnic Disparities in pregnancy-related deaths - United States, 2007–2016. MMWR Morb Mortal Wkly Rep. 2019;68(35):762–5.
Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013/11/15 ed. 2013;10 Suppl 1(Suppl 1):S2–S2.
Hamilton BE, Martin JA, Osterman M. Births: Provisional Data for 2022. National Center for Health Statistics (U.S.), editor. 2023 Jun 1;(28). Available from: https://stacks.cdc.gov/view/cdc/127052
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84.
Burris Heather H, Lorch Scott A, Kirpalani Haresh, Pursley DeWayne M, Elovitz Michal A, Clougherty Jane E. Racial disparities in preterm birth in USA: a biosensor of physical and social environmental exposures. Arch Dis Child. 2019;104(10):931.
Bronstein JM, Wingate MS, Brisendine AE. Why is the U.S. preterm birth rate so much higher than the rates in Canada, Great Britain, and Western Europe? Int J Health Serv. 2018;48(4):622–40.
Tverskoi D, Senthilnathan A, Gavrilets S. The dynamics of cooperation, power, and inequality in a group-structured society. Sci Rep. 2021;11(1):18670.
Lane HM, Morello-Frosch R, Marshall JD, Apte JS. Historical redlining is associated with present-day air pollution disparities in US Cities. Environ Sci Technol Lett. 2022;9(4):345–50. This manuscript found that an economic policy (redlining) was associated with air pollution exposure decades later..
Krieger N, Van Wye G, Huynh M, Waterman PD, Maduro G, Li W, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. Am J Public Health. 2020;110(7):1046–53. This manuscript found that an economic policy (redlining) was associated with preterm birth decades later.
Wallace ME, Mendola P, Chen Z, Hwang BS, Grantz KL. Preterm birth in the context of increasing income inequality. Matern Child Health J. 2016;20(1):164–71.
Woolhandler S, Himmelstein DU, Ahmed S, Bailey Z, Bassett MT, Bird M, et al. Public policy and health in the Trump era. The Lancet. 2021;397(10275):705–53. This review article highlights how environmental policy changed during the Trump administration.
Casey JA, Karasek D, Ogburn EL, Goin DE, Dang K, Braveman PA, et al. Retirements of coal and oil power plants in California: association with reduced preterm birth among populations nearby. Am J Epidemiol. 2018;187(8):1586–94.
Lazzarini Z. The End of Roe v. Wade — States’ power over health and well-being. N Engl J Med. 2022;387(5):390–3.
Byron JJ, Avalos M, Amy Xiao K, Klein AA, Leheste JR. Health equity in a post ‘Roe Versus Wade’ America. Cureus. 2022;14(12):e32100.
Felix M, Sobel L, Salganicoff A. KFF Women’s Health Policy. 2023 [cited 2023 Dec 13]. Legal Challenges to state abortion bans since the Dobbs decision. Available from: https://www.kff.org/womens-health-policy/issue-brief/legal-challenges-to-state-abortion-bans-since-the-dobbs-decision/
Guttmacher Institute. Interactive map: US abortion policies and access After Roe [Internet]. 2023 [cited 2023 Dec 14]. Available from: https://states.guttmacher.org/policies/
Wheaton B, Young M, Montazer S, Stuart-Lahman K. Social stress in the twenty-first century. In: Handbook of the Sociology of Mental Health, 2nd ed. New York, NY, US: Springer Science + Business Media; 2013. p. 299–323. (Handbooks of sociology and social research.).
Frederiksen B, Ranji U, Gomez I, Salganicoff A. KFF Women’s Health Policy. 2023 [cited 2023 Dec 14]. A National Survey of OBGYNs’ Experiences After Dobbs. Available from: https://www.kff.org/womens-health-policy/report/a-national-survey-of-obgyns-experiences-after-dobbs/
Gupta S, Perry B, Simon K. Trends in abortion- and contraception-related internet searches after the US Supreme Court overturned constitutional abortion rights: how much do state laws matter? JAMA Health Forum. 2023;4(4):e230518–e230518.
Myers C. Forecasts for a post-Roe America: The effects of increased travel distance on abortions and births. Journal of Policy Analysis and Management [Internet]. 2023 Sep 13 [cited 2023 Nov 28];n/a(n/a). Available from: https://doi.org/10.1002/pam.22524
Gruber J, Levine P, Staiger D. Abortion legalization and child living circumstances: who is the “Marginal Child”? Q J Econ. 1999;114(1):263–91.
Miller S, Wherry LR, Foster DG. The economic consequences of being denied an abortion. Am Econ J Econ Pol. 2023;15(1):394–437.
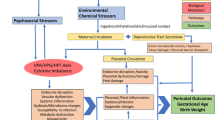
Padula AM, Monk C, Brennan PA, Borders A, Barrett ES, McEvoy CT, et al. A review of maternal prenatal exposures to environmental chemicals and psychosocial stressors-implications for research on perinatal outcomes in the ECHO program. J Perinatol. 2019/10/17 ed. 2020;40(1):10–24. This review article highlights the importance of considering both chemical and non-chemical exposures in maternal and child health research.
Barrett ES, Padula AM. Joint impact of synthetic chemical and non-chemical stressors on children’s health. Curr Environ Health Rep. 2019/10/23 ed. 2019;6(4):225–35. This review article highlights the importance of considering both chemical and non-chemical exposures in maternal and child health research.
Myers C, Bennett L, Vale F, Nieto A. Abortion access dashboard [Internet]. 2023 [cited 2023 Dec 13]. Available from: https://experience.arcgis.com/experience/6e360741bfd84db79d5db774a1147815
United States Environmental Protection Agency. EJ Screen: environmental justice screening and mapping tool [Internet]. 2023 [cited 2023 Dec 13]. Available from: https://www.epa.gov/ejscreen
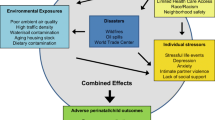
Olvera-Alvarez H, Appleton A, Fuller C, Belcourt A, Kubzansky L. An integrated socio-environmental model of health and well-being: a conceptual framework exploring the joint contribution of environmental and social exposures to health and disease over the life span. Current Environmental Health Reports. 2018;1:5.
Brenner AB, Zimmerman MA, Bauermeister JA, Caldwell CH. Neighborhood context and perceptions of stress over time: an ecological model of neighborhood stressors and intrapersonal and interpersonal resources. Am J Community Psychol. 2013;51(3–4):544–56.
Krieger Nancy, Huynh Mary, Li Wenhui, Waterman Pamela D, Van Wye Gretchen. Severe sociopolitical stressors and preterm births in New York City: 1 September 2015 to 31 August 2017. J Epidemiol Community Health. 2018;72(12):1147.
Chu DM, Aagaard J, Levitt R, Whitham M, Mastrobattista J, Rac M, et al. Cohort analysis of immigrant rhetoric on timely and regular access of prenatal care. Obstetrics & Gynecology [Internet]. 2019;133(1). Available from: https://journals.lww.com/greenjournal/fulltext/2019/01000/cohort_analysis_of_immigrant_rhetoric_on_timely.17.aspx
Gutierrez C, Dollar NT. Birth and prenatal care outcomes of Latina mothers in the Trump era: analysis by nativity and country/region of origin. PLoS ONE. 2023;18(3):e0281803.
Gemmill A, Catalano R, Alcalá H, Karasek D, Casey JA, Bruckner TA. The 2016 presidential election and periviable births among Latina women. Early Human Dev. 2020;1(151):105203.
Bell SO, Stuart EA, Gemmill A. Texas’ 2021 Ban on abortion in early pregnancy and changes in live births. JAMA. 2023;330(3):281–2.
Redd SK, Mosley EA, Narasimhan S, Newton-Levinson A, AbiSamra R, Cwiak C, et al. Estimation of multiyear consequences for abortion access in Georgia under a law limiting abortion to early pregnancy. JAMA Netw Open. 2023;6(3):e231598–e231598.
Nehme L, Ye P, Huang JC, Kawakita T. Decision and economic analysis of hostile abortion laws compared with supportive abortion laws. Am J Obstet Gynecol MFM. 2023;5(8):101019.
McCarty AT. Child poverty in the United States: a tale of devastation and the promise of hope. Sociol Compass. 2016;10(7):623–39.
Centers for Disease Control and Prevention. Maternal deaths and mortality rates: each state, the District of Columbia, United States 2018–2021 [Internet]. 2022 [cited 2023 Dec 14]. Available from: https://www.cdc.gov/nchs/maternal-mortality/MMR-2018-2021-State-Data.pdf
Robert Wood Johnson Foundation. State of childhood obesity [Internet]. 2023 [cited 2023 Dec 14]. Available from: https://stateofchildhoodobesity.org/demographic-data/ages-10-17/
Foster DG, Biggs MA, Ralph L, Gerdts C, Roberts S, Glymour MM. Socioeconomic outcomes of women who receive and women who are denied wanted abortions in the United States. Am J Public Health. 2022;112(9):1290–6.
Jones K, Pineda-Torres M. Trap’d Teens: Impacts of abortion provider regulations on fertility & education. SSRN. 2022 May 19;IZA Discussion Paper No. 14837. This article shows how a social and reproductive policy can impact population health.
Kleven H, Landais C, Posch J, Steinhauer A, Zweimüller J. Child penalties across countries. AEA Papers Proc. 2019;109:122–6.
Kleven H, Landais C, Søgaard JE. Children and gender inequality: evidence from Denmark. Am Econ J Appl Econ. 2019;11(4):181–209.
Hanauer A. Institute on Taxation and Economic Policy. 2022 [cited 2023 Dec 14]. Abortion-restricting states do least for children. Available from: https://itep.org/abortion-restricting-states-do-least-for-children/
Jacobs David E, Clickner Robert P, Zhou Joey Y, Viet Susan M, Marker David A, Rogers John W, et al. The prevalence of lead-based paint hazards in U.S. housing. Environ Health Perspect. 2002;110(10):A599-606.
Muñoz I, Colacino JA, Lewis RC, Arthur AE, Meeker JD, Ferguson KK. Associations between school lunch consumption and urinary phthalate metabolite concentrations in US children and adolescents: results from NHANES 2003–2014. Environ Int. 2018;1(121):287–95.
Biggs MA, Upadhyay UD, McCulloch CE, Foster DG. Women’s mental health and well-being 5 years after receiving or being denied an abortion: A prospective, longitudinal cohort study. JAMA Psychiat. 2017;74(2):169–78.
Dave D, Fu W, Yang M. Mental distress among female individuals of reproductive age and reported barriers to legal abortion following the US Supreme Court decision to overturn Roe v Wade. JAMA Netw Open. 2023;6(3):e234509–e234509. This article shows that stress levels increased among women in the US following the Dobbs decision.
Rajkumar RP. The relationship between access to abortion and mental health in women of childbearing age: analyses of data from the Global Burden of Disease Studies. Cureus. 2022;14(11):e31433.
Clark EA, Cordes S, Lathrop E, Haddad LB. Abortion restrictions in the state of Georgia: anticipated impact on people seeking abortion. Contraception. 2021;103(2):121–6.
Post SM, Jobe MC, Malekzadeh AN, AuBuchon KE, Hoffman RK, Stock ML, et al. Watching the fall of Roe v. Wade: media exposure relates to U.S. women’s alcohol use intentions. Psychol Addict Behav. 2023
American Psychological Association. Stress in AmericaTM. 2020. (A National Mental Health Crisis.).
Wiley KS, Knorr DA, Chua KJ, Garcia S, Fox MM. Sociopolitical stressors are associated with psychological distress in a cohort of Latina women during early pregnancy. J Community Psychol. 2023;51(7):3044–59.
Ramos IF, Campos B, Schetter CD. Pregnancy anxiety and beliefs surrounding motherhood in Latinas: a qualitative study. J Lat Psychol. 2022;10(4):277–90.
Ballard PJ, Hoyt LT, Yazdani N, Kornbluh M, Cohen AK, Davis AL, et al. Election-related sociopolitical stress and coping among college students in the United States. J Am Coll Health. 2022;9:1–11.
Latendresse G. The interaction between chronic stress and pregnancy: preterm birth from a biobehavioral perspective. J Midwifery Womens Health. 2008/12/31 ed. 2009;54(1):8–17
Shahid Z, Asuka E, Singh G. Physiology, hypothalamus. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024
Kogler L, Müller VI, Chang A, Eickhoff SB, Fox PT, Gur RC, et al. Psychosocial versus physiological stress — meta-analyses on deactivations and activations of the neural correlates of stress reactions. Neuroimage. 2015;1(119):235–51.
Thau L, Gandhi J, Sharma S. Physiology, Cortisol. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024
Dahlerup BR, Egsmose EL, Siersma V, Mortensen EL, Hedegaard M, Knudsen LE, et al. Maternal stress and placental function, a study using questionnaires and biomarkers at birth. PLoS ONE. 2018;13(11):e0207184.
Giurgescu C. Are maternal cortisol levels related to preterm birth? J Obstet Gynecol Neonatal Nurs. 2009;38(4):377–90.
Hoyt LT, Zeiders KH, Chaku N, Niu L, Cook SH. Identifying diurnal cortisol profiles among young adults: physiological signatures of mental health trajectories. Psychoneuroendocrinology. 2021;1(128):105204.
Stanton SJ, LaBar KS, Saini EK, Kuhn CM, Beehner JC. Stressful politics: voters’ cortisol responses to the outcome of the 2008 United States Presidential election. Psychoneuroendocrinology. 2010;35(5):768–74.
Blanton H, Strauts E, Perez M. Partisan identification as a predictor of cortisol response to election news. Polit Commun. 2012;29(4):447–60.
Filardi T, Panimolle F, Lenzi A, Morano S. Bisphenol A and Phthalates in diet: an emerging link with pregnancy complications. Nutrients. 2020;12(2)
Eick SM, Goin DE, Cushing L, DeMicco E, Smith S, Park JS, et al. Joint effects of prenatal exposure to per- and poly-fluoroalkyl substances and psychosocial stressors on corticotropin-releasing hormone during pregnancy. J Exposure Sc Environ Epidemiol [Internet]. 2021; https://doi.org/10.1038/s41370-021-00322-8
Barrett ES, Corsetti M, Day D, Thurston SW, Loftus CT, Karr CJ, et al. Prenatal phthalate exposure in relation to placental corticotropin releasing hormone (pCRH) in the CANDLE cohort. Environ Int. 2022;1(160):107078.
Appleton AA, Jackson BP, Karagas M, Marsit CJ. Prenatal exposure to neurotoxic metals is associated with increased placental glucocorticoid receptor DNA methylation. Epigenetics. 2017;12(8):607–15.
Chen X, Xu S, Tan T, Lee ST, Cheng SH, Lee FW, et al. Toxicity and estrogenic endocrine disrupting activity of phthalates and their mixtures. Int J Environ Res Public Health. 2014;11(3):3156–68.
James-Todd T, Senie R, Terry MB. Racial/ethnic differences in hormonally-active hair product use: a plausible risk factor for health disparities. J Immigr Minor Health. 2012;14(3):506–11.
Richman LS, Jonassaint C. The effects of race-related stress on cortisol reactivity in the laboratory: implications of the Duke Lacrosse scandal. Ann Behav Med. 2008;35(1):105–10.
Dench D, Pineda-Torres M, Myers C. The effects of the Dobbs decision on fertility. SSRN. 2023 Nov 27;IZA Discussion Paper No. 16608,. This article shows the preliminary impact of the Dobbs decision on the birth rate.
Funding
Stephanie M Eick was supported by the JPB Environmental Health Fellowship and by grants K01ES035082 and P30ES019776 from the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
SME was responsible for the conceptualization and wrote the main manuscript text. JAE prepared Fig. 1 and contributed to writing, reviewing, and editing. MC prepared Fig. 2, contributed to the literature review and to writing, reviewing, and editing. NRB prepared Fig. 2 and contributed to writing, reviewing, and editing.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eick, S.M., Eatman, J.A., Chandler, M. et al. Reproductive and Social Policies, Sociopolitical Stress, and Implications for Maternal and Child Health Equity. Curr Envir Health Rpt (2024). https://doi.org/10.1007/s40572-024-00443-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s40572-024-00443-w