Abstract
Purpose of Review
We assessed the relation between environmental greenness and risk of dementia and cognitive impairment, based on a systematic review and meta-analysis up to March 30, 2022, characterizing whenever possible the shape of the association using dose–response meta-analysis.
Recent Findings
Twelve studies were included in this review, either using normalized difference vegetation index (NDVI) or land use/cover (LU/LC) methodology to assess greenness. Comparing the highest versus lowest exposure categories of greenness assessed using the NDVI (6 studies) or LU/LC (6 studies), we found no association with dementia. Dose–response meta-analysis of the association between greenness measured by LU/LC and dementia, based on only 3 studies, indicated a U-shaped association, but estimates were imprecise.
Summary
Our systematic review and meta-analysis provided some evidence of a slight inverse association between greenness and dementia at intermediate exposure levels, but not at high levels. Potential methodological limitations, such as exposure misclassification and unmeasured confounding, may have affected the results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia is a progressive neurodegenerative disease that results in major economic and social costs for both patients and their families. Approximately 50 million people in the world currently suffer from dementia; the estimated number of annual incident cases is 10 million, and approximately 150 million prevalent cases are predicted in 2050 [1]. For these reasons, dementia prevention is a key public health priority [2••]. Cognitive impairment is a clinical state that precedes dementia [3]. It is characterized by lower-than-expected performance in one or more cognitive domains considering the patient’s age and educational attainment; however, it does not substantially interfere in activities of daily living (ADLs). On the contrary, in dementia, more than one cognitive domain is affected, resulting in significant interference in ADL [3,4,5,6].
The causes of dementia remain unknown. Many potential risk factors have been investigated, such as reduced physical activity [7], poor diet [8], comorbidities such as diabetes, hypertension, and cardiovascular disease [9,10,11], and other environmental, clinical, and genetic factors. Environmental factors in particular, including exposure to air pollution, heavy metals, and metalloids [12], are increasingly considered as possible risk factors [13].
To date, there are no effective interventions to prevent, delay, or treat cognitive impairment and dementia, with the exception of preventive measures for vascular dementia [14, 15]. Therefore, the identification of environmental factors as risk factors for dementia could help prevent the disease, or its related disorders, either of the Alzheimer’s type or belonging to other clinical forms. Among the possible risk factors for dementia is the reduced availability of residential green space (“greenness”). Natural vegetation or green space/greenness surrounding residential and workplaces has been hypothesized to be protective towards dementia [16]. Potential beneficial effects of greenness on brain structure and function include greater cortical thickness [17, 18••, 19] and reduced ventricular size [20]. Research has shown a protective effect of residential greenness for a number of other outcomes including all-cause mortality, obesity, cardiovascular and respiratory diseases, poor sleep quality [21••, 22,23,24,25,26,27,28,29, 30••], pediatric anxiety and depression, and adverse birth outcomes [31, 32, 33••, 34•, 35].
The exposure indices most frequently used in literature to measure greenness are normalized difference vegetation index (NDVI) and land use and land cover (LU/LC). NDVI is obtained by satellite imagery and uses the characteristic of chlorophyll in leaves to absorb visible light for photosynthesis and reflect light near the infrared. NDVI is computed as the ratio of the difference between the near-infrared region and red reflectance to the sum of these two measures [36]. NDVI ranges from − 1 to 1, with more positive values representing higher greenness level, and negative values representing bodies of water [21••]. Other studies have instead relied on land use (LU), an indicator of land cover types, and land cover (LC), reflecting the physical and biological surface of land [37]. Studies based on LU/LC employed a land cover dataset to determine the percentage of land use around a predetermined buffer or area around the participant’s address, with specific reference to the presence of parks or urban green, forests, or crops/cultivations [38, 39]. Rarely used indices for exposure assessment include the enhanced vegetation index, based on land surface reflectance of light spectrum as NDVI but including adjustment for tree canopy background [40], and the vegetation continuous fields, relying on the percentage of land covered by tree canopies [41].
Given the growing number of studies assessing the relation between greenness and both cognitive impairment and dementia and the recent availability of new statistical tools for the assessment of non-linear relations [42, 43], we performed a systematic review of the literature and a dose–response meta-analysis to characterize the association between residential greenness and cognitive outcomes.
Methods
Study Identification
In this review, we applied the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [44, 45]. We performed a literature online search in the PubMed/MEDLINE and Embase databases until March 30, 2022 with no time restriction. Two authors (FZ and TF) independently screened publication titles and abstracts and evaluated full text for inclusion in the review. In case of conflicting evaluation, a third author (MV) was sought to resolve the disagreement.
According to the PECOS (Population, Exposure, Comparator, Outcome and Study design) guidelines [46], the specific research question is “In the adult population, what is the effect of greenness on risk of cognitive impairment or dementia from epidemiological studies?”.
Based on the research question, we selected epidemiological studies investigating exposure to greenness among adults (≥ 18 years old). We included research articles and not reviews, letters, or conference abstracts. We used search terms related to greenness, e.g., “green space,” “recreational parks,” “urban park,” “urban green,” and “vegetation,” as well as terms related to greenness measurement methods, i.e., “normalized difference vegetation index,” “land use,” “land cover,” and “vegetation index.” To investigate the outcome, we used terms related to dementia and cognitive impairment using MeSH terms and Explode terms for PubMed and Embase research, respectively. Only studies quantifying the prevalence, incidence, or mortality rate for dementia or cognitive impairment were considered, provided they used the International Classification of Disease (ICD), prescription of anti-dementia medication, hospital using scales for cognitive impairment diagnosis like Mini Mental State Examination (MMSE), and with dementia diagnosis during hospitalization. We included all types of observational studies with individual level data, i.e., cohort, case–control, cross-sectional, and ecological studies. From the original literature search, we excluded studies not reporting the aforementioned information. Supplemental Table S1 includes the details of our search strategies. No language restrictions were applied. If multiple studies used the same population, we considered the most recent report, which included the one the largest population, or the one specifically aimed at assessing dementia as outcome.
Data Extraction
From each selected study, we extracted location, study design, total study population, number of cases, and number of controls if applicable, period of observation or year when the study data were collected, greenness evaluation methodology, type of outcome and its assessment method, and risk estimates with 95% confidence intervals (CI) taken from the fully adjusted model. We also extracted, whenever possible, all the details about the magnitude of greenness for each exposure category in which the study population was divided. When greenness was assessed using different areas or buffer diameters, we extracted data from the smallest area or buffer. We contacted the authors of the four publications in which detailed data were not provided [47,48,49,50] and obtained additional data needed to perform the analysis.
Risk of bias assessment
We assessed the risk of bias (RoB) of the included studies using the Risk of Bias in Non-Randomized Studies of Exposure (ROBINS-E) tool [51, 52]. Two investigators (FZ and TF) assessed the risk of bias. Any discrepancy was resolved by MV. Supplemental Table S2 reports criteria for RoB evaluation. Studies were considered “low RoB” if all domains were rated at low risk; they were considered “moderate” or “high” RoB if one or more domains was at moderate or high RoB, respectively.
Data Analysis
We performed a meta-analysis comparing the highest versus the lowest greenness categories or continuous increase of greenness (1 standard deviation or interquartile range or 0.1 unit or 10% increments) using a restricted maximum likelihood random effects model with inverse–variance estimation method. We also explored the shape of the association between greenness and risk of cognitive impairment or dementia through a dose–response meta-analysis using a one-stage approach in order to explore also non-linear association [53] as previously implemented in other fields [54,55,56]. For this purpose, we also extracted the mean value of greenness for each exposure category. If the mean was not available, we used the median or the midpoint of each exposure stratum. In case of highest and lowest open-ended exposure categories, we used a value 20% higher or lower than the boundary value, based on the ranges observed in studies with complete data [57, 58]. Studies that provided risk estimates only for continuous exposure were excluded from the dose–response analysis. We used a restricted cubic spline model with three knots at fixed percentiles (10th, 50th, and 90th) of greenness through the restricted maximum likelihood random effects model [59]. We provided a graphical overlay of study-specific trends using predicted curves showing the influence of variation across studies. Finally, we assessed the heterogeneity of included studies using the I2 statistics [60]. We used Stata software (v17.0, Stata Corp. College Station, TX, 2021) to perform all data analysis.
Results
Study Selection
Figure 1 shows the PRISMA flow chart for literature search and study identification. We identified 269 potentially eligible articles, after the exclusion of duplicates. After analyzing the title and abstract, we discarded 232 papers and we retrieved the full text of the remaining 37. After their in-depth evaluation, we further excluded two studies because they analyzed the same population [61, 62••], 17 studies because they did not evaluate the exposure or outcome of interest (such as the two measuring cognitive decline but not cognitive impairment [19, 40]), and six papers because they were not original research articles. Overall, 12 publications eventually met the inclusion criteria, i.e., they had individual-level data and reported the association of greenness with dementia and/or cognitive impairment [47,48,49,50, 63,64,65, 66••, 67, 68••, 69, 70].
Study Characteristics
Table 1 summarizes the main characteristics of included studies. The publication period ranged from 2015 to 2022. Three studies were conducted in Europe (two in UK [48, 67], one in the Netherlands [47]), five in North America (two in Canada [49, 66••] and three in US [68••, 69, 70]), three in Asia (one each in China [50], Taiwan [65], and Hong Kong [64]), and one in Australia [63]. Four studies had a cross-sectional design [48, 64, 67, 68••], one case–control [65], five cohort [47, 49, 63, 66••, 69], one including both cross-sectional and cohort design [50], and one ecological [70].
With regard to exposure assessment, six studies measured greenness using NDVI [49, 50, 64, 66••, 68••, 69], five used LU/LC with the corresponding datasets for the classification of green areas [48, 63, 65, 67, 70], and one study presented both LU/LC and NDVI [47]. Six studies compared the greenness of the smallest residential units of study participants based on the administrative subdivision of each country [48, 64, 65, 67, 68••, 70], defined by an average population (e.g., lower layer super output areas [48, 67]) or on natural or urban boundaries such as roads (e.g., census block [68••]). In the other studies, residential greenness was measured using the mean value of NDVI or LU/LC with various dimensions of buffer around the residential addresses: one study analyzed residential greenness around a 1.6-km area [63]; another measured greenness at 250-m and 500-m buffers from centroid city block of subject’s residence [66••]; one study assessed the areal greenness of 100 m surrounding residential address [49]. The area considered by another study is 500-m buffer size around participant’s residence [50]; one study analyzed the area of 300 m and 1000 m around the residence [47]; another study analyzed the greenness at 2000-m buffer around the residence [69]. For data analysis, we used the values related to the smallest buffers, in accordance with previous reviews [71, 72], that ranged from 100 m to 2 km across the different studies. The characteristics of exposure assessment are described in more detail in the Supplemental Table S3.
All the three studies of cognitive impairment were based on categorical definitions of greenness, while seven out of the 11 studies on dementia used continuous exposure data, and the remaining four used categorical data.
As shown in Table 1, two studies investigated the association between greenness and mortality from dementia [47, 64], while four studies explored the association with incidence [49, 63, 66••, 69], one with further subdivision into all-cause dementia, vascular dementia, and Alzheimer’s disease [69]. Similarly, one study evaluated the association between greenness and incidence of four neurodegenerative diseases, namely Parkinson’s disease, multiple sclerosis, Alzheimer’s disease, and non-Alzheimer’s dementia, although only the latter two were considered for the analysis [49]. In addition, two studies investigated the association between greenness and both cognitive impairment and dementia [48, 67], while one study assessed cognitive impairment specifically [50]. One study investigated the association with Alzheimer’s dementia using prevalent cases [65], while one study considered prevalent cases of “Alzheimer’s disease and related dementias” (ADRD) together and divided into “Alzheimer’s disease” (AD) and “non-Alzheimer’s dementia” (NAD) [68••]. One ecological study design [70] used Alzheimer’s disease rate by zip code.
Four studies used the International Classification of Disease, Injuries and Causes of Death (ICD versions 9 and 10) to measure outcome [47, 64, 68••, 70]. Another four studies used for the diagnosis of dementia, in addition to ICD, hospitalization and/or the first treatment with specific drugs and/or physician claims [49, 63, 65, 66••]. Three studies administered established cognitive tests (e.g., MMSE and geriatric mental status) [48, 50, 67], though one of them was based on an adapted version of the MMSE [50]. One study used a series of clinical and neuropsychological tests for diagnosis of dementia classified according to DSM-IV criteria [69].
Five studies included a study population of over 200,000 individuals [47, 49, 64, 66••, 68••], one between 100,000 and 200,000 [63], two between 10,000 and 100,000 [50, 65], and three studies analyzed a population less than 10,000 [48, 67, 69]. The total number of study participants included in this review was over 3,350,000, including over 275,000 and over 24,000 cases of dementia and cognitive impairment, respectively. The ecological study population comprised subjects aged > 65 years, who lived in the Mid-Atlantic USA and had Medicare insurance [70].
After assessing the risk of bias of the included studies (Supplemental Table S4), we evaluated five studies as being at low RoB [47, 48, 63, 67, 69]. Five studies had moderate RoB [49, 64, 65, 66••, 68••] due to lack of education data, lack of detailed information about the magnitude of greenness, or with more than 10% of the population excluded to missing data. Two studies had a high RoB: one analyzed the relation between LU/LC and self-reported cognitive impairment [50], and the second examined the relation between NDVI and dementia without controlling for age and sex [70]. We performed a sensitivity analysis excluding such studies with high RoB.
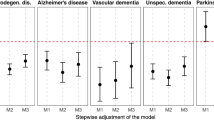
Greenness and Dementia
Figure 2 shows individual and summary risk ratios (RRs) of dementia comparing the highest to lowest greenness categories, or in case of continuous data for 1-unit exposure increase. We used a dose value 20% higher or lower of the boundary value in one study [63]. Overall, the summary RR for the association between greenness and dementia was 0.98 (95% CI 0.90–1.06) when greenness was measured with NDVI and 0.99 (95% CI 0.93–1.05) when LU/LC models were used. Stratification by types of study (e.g., longitudinal vs cross-sectional) and greenness measurement methodologies showed similar results (Supplemental Figure S1 and Supplemental Figure S2). The analysis restricted to Alzheimer’s disease as the outcome available in five studies yielded similar results: in the three studies [49, 68••, 69] using NDVI, the summary RR was 1.03 (95% CI 0.83–1.28), while in the two studies using LU/LC [65, 70], the summary RR was 0.96 (95% CI 0.87–1.06) (Supplemental Figure S3). Conversely, risk of non-Alzheimer’s dementia was reported in two studies only, one study [49] reporting a RR of 0.95 (95% CI 0.93–0.98) for interquartile increase of greenness and the second study [68••] reporting a RR of 0.95 (95% 0.89–1.02) in the intermediate exposure category and RR of 1.01 (95% CI 0.93–1.08) in the highest exposure group.
Risk ratio (RR) with 95% confidence interval (CI) between exposure to greenness measured by normalized difference vegetation index (NDVI) or land use/land cover (LU/LC) and dementia. The squares represent risk estimate, and horizontal lines represent their 95% CI. The area of each square is proportional with the weight of the study in the meta-analysis. The diamonds represent the combined risk for each type of exposure, and the solid line represents null value. The inverse-variance estimation method was used for study weighting. AD, Alzheimer’s disease; NAD, non-Alzheimer’s dementia
The association between dementia and greenness comparing the highest versus the lowest exposure categories, after excluding six studies based on 1-unit continuous exposure increase, showed a higher estimate compared with the overall result (Supplemental Figure S4). Similar results were also obtained after excluding the only study [70] at high risk of bias (Supplemental Figure S5).
The dose–response curve between dementia and greenness as measured by LU/LC showed a lower risk ratio for the “intermediate” range of exposure, between 0.2 and 0.8, with the lowest RR of around 0.8 at a greenness level of 0.5. At the highest levels of greenness, there was little evidence of protection, with the RR approaching and slightly exceeding 1 (Fig. 3). Two of the three included studies demonstrated a U-shaped relation while the other suggested no association [48, 63, 67] (Supplemental Figure S6). A dose–response meta-analysis between dementia and greenness based on the NDVI methodology could not be computed since only two studies were suitable for inclusion.
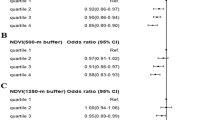
Greenness and Cognitive Impairment
The two studies that investigated greenness using LU/LC and cognitive impairment reported a summary RR of 1.47 (95% CI 1.22–1.76) when comparing the highest and lowest exposure categories (Fig. 4). Only one study, having high RoB, assessed greenness with NDVI [50], and reported an odds ratio of 0.92 (95% CI 0.84–1.01).
Risk ratio (RR) with 95% confidence interval (CI) between exposure to greenness measured by normalized difference vegetation index (NDVI) or land use/land cover (LU/LC) and cognitive impairment. The squares represent risk estimate, and horizontal lines represent their 95% CI. The area of each square is proportional with the weight of the study in the meta-analysis. The diamonds represent the combined risk for each type of exposure, and the solid line represents null value. The inverse–variance estimation method was used for study weighting
We could not compute a dose–response meta-analysis between greenness and cognitive impairment due to the small number of studies available, whether using NDVI (n = 1) or LU/LC (n = 2).
Discussion
Environmental greenness will have greater importance to humans given the progressive shift towards urbanization, with over 60% of the population projected to live in urban areas by 2030 [73]. The present systematic review and meta-analysis suggests that greenness may have a non-linear association with dementia. Specifically, the dose–response curve for greenness measured by LU/LC is consistent with the hypothesis that living in a place with an intermediate greenness value may protect against dementia. This U-shaped association may be related to possible counteracting effects and interplay of greenness-associated factors, both beneficial (reduced air pollution and noise annoyance, psychological factors, and increased physical activity) and adverse (greater social isolation, decreased interaction with neighbors, increased loneliness, and distance from medical and social services, particularly in rural areas) [16, 74,75,76]. However, such possible mediators and confounders were not adequately assessed in the available studies, and should be carefully considered in future investigations [77, 78]. The null findings from the categorical analysis do not necessarily contradict the dose–response analysis. Because the categories of exposure were defined independently in each study and were heterogeneous across studies, the pooled analysis is difficult to interpret and may be misleading. In addition, since the dose–response meta-analysis indicated comparable RRs in the highest and the lowest exposure ranges, the null results of the categorical analysis were not surprising as they could not capture the shape of the association between greenness and dementia at intermediate exposure levels.
NDVI and LU/LC were the greenness indices used in the papers that could be retrieved in this review. NDVI is an index obtained through satellite images [36] that cannot distinguish the type of “green,” while the LU/LC index, generated through regional databases, may better represent greenness typology. LU/LC has the additional advantage to reflect the presence of anthropogenic activities and related interactions with the natural ecosystem [38]. Therefore, while NDVI is an overall measure of green area, with no relation with greenspace use, LU/LC models may assess greenness as proximity of natural environments like forest and agricultural crops, owing to information generally yielded by regional datasets. Therefore, studies based on LU/LC might be able to provide more information than NDVI to investigate types of greenness. In addition, these studies may be affected by confounding, such as the different availability of facilities like recreational and social meeting places associated with proximity to green spaces, thus raising relevant methodological issues that have not been fully addressed in existing studies. These aspects may be particularly important in the study of dementia, since social isolation has been suggested as possible adverse effect of greenness when assessing its relation with cognition [77,78,79]. In this regard, LU/LC might be more valid than NDVI in providing an adequate characterization of green areas, accounting for these issues. Unfortunately, the number of studies based on LU/LC and addressing cognitive outcomes is limited.
The observational nature of included studies and the lack of detailed information for some potential mediators and/or confounders and their interactions represent major limitations of the studies on greenness and cognitive outcomes. In particular, it is difficult to identify the exact factors independently associated with greenness and that may mediate potential favorable effects on dementia, such as decreased stress levels [80, 81], lower air pollution [82•, 83, 84•], increased physical activity [23, 85], reductions in obesity [86], and improved mental health [87, 88].
Heterogeneity in the definition of greenness across studies, particularly in terms of area characteristics and size, could have hampered the detection of an association with cognitive impairment and dementia. For instance, to define greenness, some studies chose the buffer size area from residence [47, 49, 50, 63, 66••, 69], e.g., area of 1.6 km from the point of residence because it is the distance that a person can cover on foot and because long distances allow opportunities for contact with more green spaces [88]. In other studies [48, 64, 65, 67, 68••, 70], the area considered to assess greenness coincided with the smallest geographic unit used by the national demographic agency, e.g., the census block level NDVI for each study participants’ residential address in a Florida study [68••]. Similarly, the timing of exposure assessment differs across studies, since some of them assessed greenness at several time points during the follow-up [66••], or reported the average value of four seasons [50], or alternatively relied on a single measure, as done in most studies. In addition, timing of exposure assessment did not consider changes in greenness over time, before disease onset. Another source of exposure misclassification stems from the fact that greenness was generally measured surrounding the participants’ address of residence, while the time spent in other places (such as during working and recreational activities) was not taken into consideration. In addition, a source of heterogeneity across studies and of bias may have been the different confounders considered in the analyses. All studies except one [70] were adjusted for socio-economic status, which may be a relevant confounder [89], while only two studies [64, 66••] accounted for air pollution, also an important covariate. Air pollution has been associated with a large spectrum of neurological disorders including its ability to affect the incidence and mortality of dementia [90]. Considering the observation that green spaces, especially urban green spaces, may have the ability to reduce air pollutant levels [91], the latter can be both a mediator and a confounder [92,93,94] when addressing the role of greenness in the etiology of cognitive impairment and dementia. In the only study evaluating the association between greenness and dementia risk with and without air pollution in the multivariate model, the hazard ratio became weaker in the full adjusted model [66••].
With reference to outcome assessment, a potential source of heterogeneity was the different methodologies used across studies. For dementia diagnosis, some studies used ICD classification, while others used first anti-dementia medication, first hospitalization with dementia reported, and/or physicians’ diagnosis, or other tools such as Global Clinical Dementia Rating. In contrast, all studies used the MMSE for the diagnosis of cognitive impairment.
We acknowledge additional limitations of our review and the underlying studies on which it was based. The small number of available studies hampered our assessment, yielding statistically imprecise summary risk estimates and hampering the possibility to carry our subgroup analyses, including the exploration of potential effect modifiers such as sex, age, race, socioeconomic status, and the different associations with dementia types.
Conclusions
This systematic review and meta-analysis suggests that environmental greenness may have a non-linear association with dementia. Specifically, the data are consistent with the hypothesis that living in a place with an intermediate greenness value may protect against dementia. Given the limitations of previous studies in terms of exposure assessment, control of confounding, and lack of precision, future studies should address these methodological challenges to facilitate pooled analyses and to provide more reliable conclusions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
WHO. Risk reduction of cognitive decline and dementia: WHO Guidelines. World Health Organization, Geneva. 2019. https://www.who.int/publications/i/item/9789241550543
•• Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–46. https://doi.org/10.1016/S0140-6736(20)30367-6. This study outlines the modifiable risk factors for dementia and the possible preventive strategies.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
Knopman DS, Petersen RC. Mild cognitive impairment and mild dementia: a clinical perspective. Mayo Clin Proc. 2014;89(10):1452–9. https://doi.org/10.1016/j.mayocp.2014.06.019.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9. https://doi.org/10.1016/j.jalz.2011.03.008.
Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–94. https://doi.org/10.1111/j.1365-2796.2004.01388.x.
Beckett MW, Ardern CI, Rotondi MA. A meta-analysis of prospective studies on the role of physical activity and the prevention of Alzheimer’s disease in older adults. BMC Geriatr. 2015;15:9. https://doi.org/10.1186/s12877-015-0007-2.
Filippini T, Adani G, Malavolti M, Garuti C, Cilloni S, Vinceti G, et al. Dietary habits and risk of early-onset Dementia in an Italian case-control study. Nutrients. 2020;12(12):3682. https://doi.org/10.3390/nu12123682.
Gudala K, Bansal D, Schifano F, Bhansali A. Diabetes mellitus and risk of dementia: a meta-analysis of prospective observational studies. J Diabetes Investig. 2013;4(6):640–50. https://doi.org/10.1111/jdi.12087.
Papanastasiou CA, Theochari CA, Zareifopoulos N, Arfaras-Melainis A, Giannakoulas G, Karamitsos TD, et al. Atrial fibrillation is associated with cognitive Impairment, all-cause dementia, vascular dementia, and Alzheimer’s disease: a systematic review and meta-analysis. J Gen Intern Med. 2021;36(10):3122–35. https://doi.org/10.1007/s11606-021-06954-8.
Li J, Wu Y, Zhang D, Nie J. Associations between heart failure and risk of dementia: a PRISMA-compliant meta-analysis. Medicine (Baltimore). 2020;99(5):e18492. https://doi.org/10.1097/MD.0000000000018492.
Jung CR, Lin YT, Hwang BF. Ozone, particulate matter, and newly diagnosed Alzheimer’s disease: a population-based cohort study in Taiwan. J Alzheimers Dis. 2015;44(2):573–84. https://doi.org/10.3233/JAD-140855.
Killin LO, Starr JM, Shiue IJ, Russ TC. Environmental risk factors for dementia: a systematic review. BMC Geriatr. 2016;16(1):175. https://doi.org/10.1186/s12877-016-0342-y.
Gale SA, Acar D, Daffner KR. Dementia. Am J Med. 2018;131(10):1161–9. https://doi.org/10.1016/j.amjmed.2018.01.022.
Knopman DS, Jones DT, Greicius MD. Failure to demonstrate efficacy of aducanumab: an analysis of the EMERGE and ENGAGE trials as reported by Biogen, December 2019. Alzheimers Dement. 2021;17(4):696–701. https://doi.org/10.1002/alz.12213.
Besser L. Outdoor green space exposure and brain health measures related to Alzheimer’s disease: a rapid review. BMJ Open. 2021;11(5):e043456. https://doi.org/10.1136/bmjopen-2020-043456.
Dzhambov AM, Bahchevanov KM, Chompalov KA, Atanassova PA. A feasibility study on the association between residential greenness and neurocognitive function in middle-aged Bulgarians. Arh Hig Rada Toksikol. 2019;70(3):173–85. https://doi.org/10.2478/aiht-2019-70-3326.
•• Min KD, Kim JS, Park YH, Shin HY, Kim C, Seo SW, et al. New assessment for residential greenness and the association with cortical thickness in cognitively healthy adults. Sci Total Environ. 2021;778:146129. https://doi.org/10.1016/j.scitotenv.2021.146129. This study demonstrates that higher greenness exposure is associated with increased cortical tickness of the frontal, parietal and occipital regions in subjects living in urban areas.
Crous-Bou M, Gascon M, Gispert JD, Cirach M, Sanchez-Benavides G, Falcon C, et al. Impact of urban environmental exposures on cognitive performance and brain structure of healthy individuals at risk for Alzheimer’s dementia. Environ Int. 2020;138:105546. https://doi.org/10.1016/j.envint.2020.105546.
Besser LM, Lovasi GS, Michael YL, Garg P, Hirsch JA, Siscovick D, et al. Associations between neighborhood greenspace and brain imaging measures in non-demented older adults: the Cardiovascular Health Study. Soc Psychiatry Psychiatr Epidemiol. 2021;56(9):1575–85. https://doi.org/10.1007/s00127-020-02000-w.
•• Fong KC, Hart JE, James P. A review of epidemiologic studies on greenness and health: updated literature through 2017. Curr Environ Health Rep. 2018;5(1):77–87. https://doi.org/10.1007/s40572-018-0179-y. This review presents a complete and updated overview of the methods available to assess greenness in epidemiological studies and related issues.
Gascon M, Triguero-Mas M, Martinez D, Dadvand P, Rojas-Rueda D, Plasencia A, et al. Residential green spaces and mortality: a systematic review. Environ Int. 2016;86:60–7. https://doi.org/10.1016/j.envint.2015.10.013.
McMorris O, Villeneuve PJ, Su J, Jerrett M. Urban greenness and physical activity in a national survey of Canadians. Environ Res. 2015;137:94–100. https://doi.org/10.1016/j.envres.2014.11.010.
Sarkar C. Residential greenness and adiposity: findings from the UK Biobank. Environ Int. 2017;106:1–10. https://doi.org/10.1016/j.envint.2017.05.016.
Yitshak-Sade M, Kloog I, Novack V. Do air pollution and neighborhood greenness exposures improve the predicted cardiovascular risk? Environ Int. 2017;107:147–53. https://doi.org/10.1016/j.envint.2017.07.011.
Sun S, Sarkar C, Kumari S, James P, Cao W, Lee RS, et al. Air pollution associated respiratory mortality risk alleviated by residential greenness in the Chinese Elderly Health Service Cohort. Environ Res. 2020;183:109139. https://doi.org/10.1016/j.envres.2020.109139
de Vries S, van Dillen SM, Groenewegen PP, Spreeuwenberg P. Streetscape greenery and health: stress, social cohesion and physical activity as mediators. Soc Sci Med. 2013;94:26–33. https://doi.org/10.1016/j.socscimed.2013.06.030.
James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124(9):1344–52. https://doi.org/10.1289/ehp.1510363.
Gianfredi V, Buffoli M, Rebecchi A, Croci R, Oradini-Alacreu A, Stirparo G, et al. Association between urban greenspace and health: a systematic review of literature. Int J Environ Res Public Health. 2021;18(10):5137. https://doi.org/10.3390/ijerph18105137.
•• Kasdagli MI, Katsouyanni K, de Hoogh K, Lagiou P, Samoli E. Investigating the association between long-term exposure to air pollution and greenness with mortality from neurological, cardio-metabolic and chronic obstructive pulmonary diseases in Greece. Environ Pollut. 2022;292(Pt B):118372. https://doi.org/10.1016/j.envpol.2021.118372. This study indicates the adverse effects of air pollution and the beneficial role of greenness on mortality from nervous system disease and other diseases.
Cohen-Cline H, Turkheimer E, Duncan GE. Access to green space, physical activity and mental health: a twin study. J Epidemiol Community Health. 2015;69(6):523–9. https://doi.org/10.1136/jech-2014-204667.
Hu CY, Yang XJ, Gui SY, Ding K, Huang K, Fang Y, et al. Residential greenness and birth outcomes: a systematic review and meta-analysis of observational studies. Environ Res. 2021;193: 110599. https://doi.org/10.1016/j.envres.2020.110599.
•• Jimenez MP, Shoaff J, Kioumourtzoglou MA, Korrick S, Rifas-Shiman SL, Hivert MF, et al. Early-life exposure to green space and mid-childhood cognition in the project Viva Cohort. Massachusetts Am J Epidemiol. 2022;191(1):115–25. https://doi.org/10.1093/aje/kwab209. This study reports a nonlinear association between greenness exposure in early childhood and cognition, highlighting the relevance of dose-response assessment through the entire range of exposure.
• Zhan Y, Liu J, Lu Z, Yue H, Zhang J, Jiang Y. Influence of residential greenness on adverse pregnancy outcomes: a systematic review and dose-response meta-analysis. Sci Total Environ. 2020;718:137420. https://doi.org/10.1016/j.scitotenv.2020.137420. This review reports the inverse association between residential greenness and adverse pregnancy outcomes and it includes a dose-response assessment.
Dadvand P, Nieuwenhuijsen MJ, Esnaola M, Forns J, Basagana X, Alvarez-Pedrerol M, et al. Green spaces and cognitive development in primary schoolchildren. Proc Natl Acad Sci U S A. 2015;112(26):7937–42. https://doi.org/10.1073/pnas.1503402112.
Tucker CJ. Red and photographic infrared linear combinations for monitoring vegetation. Remote Sens Environ. 1979;8(2):127–50. https://doi.org/10.1016/0034-4257(79)90013-0.
Watson RT, Noble IR, Bolin B, Ravindranath NH, Verardo DJ, Dokken DJ. Land use, land use change, and forestry: a special report of the Intergovernmental Panel on Climate Change. Cambridge University Press, UK. 2000. https://www.ipcc.ch/report/land-use-land-use-change-and-forestry/
Du X, Zhao X, Liang S, Zhao J, Xu P, Wu D. Quantitatively assessing and attributing land use and land cover changes on China’s Loess plateau. Remote Sens Environ. 2020;12(3):353. https://doi.org/10.3390/rs12030353.
Vinceti M, Filippini T, Violi F, Rothman KJ, Costanzini S, Malagoli C, et al. Pesticide exposure assessed through agricultural crop proximity and risk of amyotrophic lateral sclerosis. Environ Health. 2017;16(1):91. https://doi.org/10.1186/s12940-017-0297-2.
de Keijzer C, Tonne C, Basagana X, Valentin A, Singh-Manoux A, Alonso J, et al. Residential surrounding greenness and cognitive decline: a 10-year follow-up of the Whitehall II cohort. Environ Health Perspect. 2018;126(7):077003. https://doi.org/10.1289/EHP2875.
de Keijzer C, Basagana X, Tonne C, Valentin A, Alonso J, Anto JM, et al. Long-term exposure to greenspace and metabolic syndrome: a Whitehall II study. Environ Pollut. 2019;255(Pt 2):113231. https://doi.org/10.1016/j.envpol.2019.113231.
Filippini T, Hatch EE, Rothman KJ, Heck JE, Park AS, Crippa A, et al. Association between outdoor air pollution and childhood leukemia: a systematic review and dose-response meta-analysis. Environ Health Perspect. 2019;127(4):46002. https://doi.org/10.1289/EHP4381.
Filippini T, Torres D, Lopes C, Carvalho C, Moreira P, Naska A, et al. Cadmium exposure and risk of breast cancer: a dose-response meta-analysis of cohort studies. Environ Int. 2020;142:105879. https://doi.org/10.1016/j.envint.2020.105879.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89. https://doi.org/10.1016/j.jclinepi.2021.03.001.
Morgan RL, Whaley P, Thayer KA, Schunemann HJ. Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int. 2018;121(Pt 1):1027–31. https://doi.org/10.1016/j.envint.2018.07.015.
Klompmaker JO, Hoek G, Bloemsma LD, Marra M, Wijga AH, van den Brink C, et al. Surrounding green, air pollution, traffic noise exposure and non-accidental and cause-specific mortality. Environ Int. 2020;134:105341. https://doi.org/10.1016/j.envint.2019.105341.
Wu YT, Prina AM, Jones AP, Barnes LE, Matthews FE, Brayne C, et al. Community environment, cognitive impairment and dementia in later life: results from the Cognitive Function and Ageing Study. Age Ageing. 2015;44(6):1005–11. https://doi.org/10.1093/ageing/afv137.
Yuchi W, Sbihi H, Davies H, Tamburic L, Brauer M. Road proximity, air pollution, noise, green space and neurologic disease incidence: a population-based cohort study. Environ Health. 2020;19(1):8. https://doi.org/10.1186/s12940-020-0565-4.
Zhu A, Wu C, Yan LL, Wu CD, Bai C, Shi X, et al. Association between residential greenness and cognitive function: analysis of the Chinese Longitudinal Healthy Longevity Survey. BMJ Nutr Prev Health. 2019;2(2):72–9. https://doi.org/10.1136/bmjnph-2019-000030.
Morgan RL, Thayer KA, Santesso N, Holloway AC, Blain R, Eftim SE, et al. A risk of bias instrument for non-randomized studies of exposures: a users’ guide to its application in the context of GRADE. Environ Int. 2019;122:168–84. https://doi.org/10.1016/j.envint.2018.11.004.
Morgan RL, Thayer KA, Santesso N, Holloway AC, Blain R, Eftim SE, et al. Evaluation of the risk of bias in non-randomized studies of interventions (ROBINS-I) and the ’target experiment’ concept in studies of exposures: Rationale and preliminary instrument development. Environ Int. 2018;120:382–7. https://doi.org/10.1016/j.envint.2018.08.018.
Orsini N. Weighted mixed-effects dose–response models for tables of correlated contrasts. Stand Genomic Sci. 2021;21:330–47. https://doi.org/10.1177/1536867X211025798.
Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: dose-response meta-analysis of experimental studies. Circulation. 2021;143(16):1542–67. https://doi.org/10.1161/CIRCULATIONAHA.120.050371.
Filippini T, Hatch EE, Vinceti M. Residential exposure to electromagnetic fields and risk of amyotrophic lateral sclerosis: a dose-response meta-analysis. Sci Rep. 2021;11(1):11939. https://doi.org/10.1038/s41598-021-91349-2.
Filippini T, Malavolti M, Whelton PK, Vinceti M. Sodium intake and risk of hypertension: a systematic review and dose-response meta-analysis of observational cohort studies. Curr Hypertens Rep. 2022;24/59:133–44. https://doi.org/10.1007/s11906-022-01182-9.
Vinceti M, Filippini T, Crippa A, de Sesmaisons A, Wise LA, Orsini N. Meta-analysis of potassium intake and the risk of stroke. J Am Heart Assoc. 2016;5(10):e004210. https://doi.org/10.1161/JAHA.116.004210.
Filippini T, Wise LA, Vinceti M. Cadmium exposure and risk of diabetes and prediabetes: a systematic review and dose-response meta-analysis. Environ Int. 2022;158:106920. https://doi.org/10.1016/j.envint.2021.106920.
Crippa A, Discacciati A, Bottai M, Spiegelman D, Orsini N. One-stage dose-response meta-analysis for aggregated data. Stat Methods Med Res. 2019;28(5):1579–96. https://doi.org/10.1177/0962280218773122.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Brown SC, Perrino T, Lombard J, Wang K, Toro M, Rundek T, et al. Health disparities in the relationship of neighborhood greenness to mental health outcomes in 249,405 U.S. medicare beneficiaries. Int J Environ Res Public Health. 2018;15(3):430. https://doi.org/10.3390/ijerph15030430.
•• Jin X, Shu C, Zeng Y, Liang L, Ji JS. Interaction of greenness and polygenic risk score of Alzheimer’s disease on risk of cognitive impairment. Sci Total Environ. 2021;796:148767. https://doi.org/10.1016/j.scitotenv.2021.148767. This study reports an inverse association between greenness exposure and cognitive impairment in subjects with low genetic risk for Alzheimer’s disease, indicating that the protective effect of grenness may not overcome genetic predisposition.
Astell-Burt T, Navakatikyan MA, Feng X. Urban green space, tree canopy and 11-year risk of dementia in a cohort of 109,688 Australians. Environ Int. 2020;145:106102. https://doi.org/10.1016/j.envint.2020.106102.
Ho HC, Fong KNK, Chan TC, Shi Y. The associations between social, built and geophysical environment and age-specific dementia mortality among older adults in a high-density Asian city. Int J Health Geogr. 2020;19(1):53. https://doi.org/10.1186/s12942-020-00252-y.
Liu CC, Li CY, Kung SF, Kuo HW, Huang NC, Sun Y, et al. Association of environmental features and the risk of Alzheimer’s dementia in older adults: a nationwide longitudinal case-control study. Int J Environ Res Public Health. 2019;16(16):2828. https://doi.org/10.3390/ijerph16162828.
•• Paul LA, Hystad P, Burnett RT, Kwong JC, Crouse DL, van Donkelaar A, et al. Urban green space and the risks of dementia and stroke. Environ Res. 2020;186: 109520. https://doi.org/10.1016/j.envres.2020.109520. This study provide evidence for an inverse association between greenness and dementia incidence, taking into account the role of air pollution.
Wu YT, Prina AM, Jones A, Matthews FE, Brayne C, Medical Research Council Cognitive F, et al. The built environment and cognitive disorders: results from the Cognitive Function and Ageing Study II. Am J Prev Med. 2017;53(1):25–32. https://doi.org/10.1016/j.amepre.2016.11.020.
•• Aitken WW, Lombard J, Wang K, Toro M, Byrne M, Nardi MI, et al. Relationship of neighborhood greenness to Alzheimer’s disease and non-Alzheimer’s dementia among 249,405 U.S. Medicare beneficiaries. J Alzheimers Dis. 2021;81(2):597–606. https://doi.org/10.3233/JAD-201179. This study carried out in a large population suggest that neighborhood greenness is associated with lower risk of Alzheimer’s dementia, but not of other dementias.
Slawsky ED, Hajat A, Rhew IC, Russette H, Semmens EO, Kaufman JD, et al. Neighborhood greenspace exposure as a protective factor in dementia risk among U.S. adults 75 years or older: a cohort study. Environ Health. 2022;21(1):14. https://doi.org/10.1186/s12940-022-00830-6.
Wu J, Jackson L. Greenspace inversely associated with the risk of Alzheimer’s disease in the Mid-Atlantic United States. Earth (Basel). 2021;2(1):140–50. https://doi.org/10.3390/earth2010009.
Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37(5):455–63. https://doi.org/10.1016/j.amepre.2009.06.022.
Zhao YL, Qu Y, Ou YN, Zhang YR, Tan L, Yu JT. Environmental factors and risks of cognitive impairment and dementia: a systematic review and meta-analysis. Ageing Res Rev. 2021;72:101504. https://doi.org/10.1016/j.arr.2021.101504.
Population Division of the Department of Economic and Social Affairs. World Urbanization Prospects - The 2018 Revision. United Nations, New York. 2019. https://population.un.org/wup/publications/Files/WUP2018-Report.pdf
Burgess S. Social isolation experienced by older people in rural communities. Commission for Rural Communities, Gloucester, UK. 2012. https://www.basw.co.uk/system/files/resources/basw_111815-1_0.pdf
Clarke PJ, Ailshire JA, House JS, Morenoff JD, King K, Melendez R, et al. Cognitive function in the community setting: the neighbourhood as a source of “cognitive reserve”? J Epidemiol Community Health. 2012;66(8):730–6. https://doi.org/10.1136/jech.2010.128116.
Chen X, Lee C, Huang H. Neighborhood built environment associated with cognition and dementia risk among older adults: a systematic literature review. Soc Sci Med. 2022;292:114560. https://doi.org/10.1016/j.socscimed.2021.114560.
Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. 2017;158:301–17. https://doi.org/10.1016/j.envres.2017.06.028.
Zijlema WL, Triguero-Mas M, Smith G, Cirach M, Martinez D, Dadvand P, et al. The relationship between natural outdoor environments and cognitive functioning and its mediators. Environ Res. 2017;155:268–75. https://doi.org/10.1016/j.envres.2017.02.017.
Astell-Burt T, Hartig T, Eckermann S, Nieuwenhuijsen M, McMunn A, Frumkin H, et al. More green, less lonely? A longitudinal cohort study. Int J Epidemiol. 2022;51(1):99–110. https://doi.org/10.1093/ije/dyab089.
Roe JJ, Thompson CW, Aspinall PA, Brewer MJ, Duff EI, Miller D, et al. Green space and stress: evidence from cortisol measures in deprived urban communities. Int J Environ Res Public Health. 2013;10(9):4086–103. https://doi.org/10.3390/ijerph10094086.
Sindi S, Hagman G, Hakansson K, Kulmala J, Nilsen C, Kareholt I, et al. Midlife work-related stress increases dementia risk in later life: the CAIDE 30-year study. J Gerontol B Psychol Sci Soc Sci. 2017;72(6):1044–53. https://doi.org/10.1093/geronb/gbw043.
• Balboni E, Filippini T, Crous-Bou M, Guxens M, Erickson LD, Vinceti M. The association between air pollutants and hippocampal volume from magnetic resonance imaging: a systematic review and meta-analysis. Environ Res. 2022;204(Pt A): 111976. https://doi.org/10.1016/j.envres.2021.111976. This review suggests that in adults air pollution may adversely affect hippocampal volume, with consequent detrimental effects on the risk of cognitive decline and dementia.
Shi L, Steenland K, Li H, Liu P, Zhang Y, Lyles RH, et al. A national cohort study (2000–2018) of long-term air pollution exposure and incident dementia in older adults in the United States. Nat Commun. 2021;12(1):6754. https://doi.org/10.1038/s41467-021-27049-2.
• Weuve J, Bennett EE, Ranker L, Gianattasio KZ, Pedde M, Adar SD, et al. Exposure to air pollution in relation to risk of dementia and related outcomes: an updated systematic review of the epidemiological literature. Environ Health Perspect. 2021;129(9):96001. https://doi.org/10.1289/EHP8716. This review shows that the epidemiological evidence supports a positive association between air pollution and risk of dementia.
Ngandu T, Lehtisalo J, Solomon A, Levalahti E, Ahtiluoto S, Antikainen R, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–63. https://doi.org/10.1016/S0140-6736(15)60461-5.
Kivipelto M, Mangialasche F, Ngandu T. Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease. Nat Rev Neurol. 2018;14(11):653–66. https://doi.org/10.1038/s41582-018-0070-3.
Kessing LV. Depression and the risk for dementia. Curr Opin Psychiatry. 2012;25(6):457–61. https://doi.org/10.1097/YCO.0b013e328356c368.
Sturm R, Cohen D. Proximity to urban parks and mental health. J Ment Health Policy Econ. 2014;17(1):19–24.
Besser LM, McDonald NC, Song Y, Kukull WA, Rodriguez DA. Neighborhood environment and cognition in older adults: a systematic review. Am J Prev Med. 2017;53(2):241–51. https://doi.org/10.1016/j.amepre.2017.02.013.
Fu P, Guo X, Cheung FMH, Yung KKL. The association between PM2.5 exposure and neurological disorders: a systematic review and meta-analysis. Sci Total Environ. 2019;655:1240–8. https://doi.org/10.1016/j.scitotenv.2018.11.218.
Nowak DJ, Crane DE, Stevens JC. Air pollution removal by urban trees and shrubs in the United States. Urban For Urban Green. 2006;4(3–4):115–23. https://doi.org/10.1016/j.ufug.2006.01.007.
Crouse DL, Pinault L, Balram A, Brauer M, Burnett RT, Martin RV, et al. Complex relationships between greenness, air pollution, and mortality in a population-based Canadian cohort. Environ Int. 2019;128:292–300. https://doi.org/10.1016/j.envint.2019.04.047.
Hood RB, James P, Fong KC, Minguez-Alarcon L, Coull BA, Schwartz J, et al. The influence of fine particulate matter on the association between residential greenness and ovarian reserve. Environ Res. 2021;197:111162. https://doi.org/10.1016/j.envres.2021.111162.
Kasdagli MI, Katsouyanni K, de Hoogh K, Lagiou P, Samoli E. Associations of air pollution and greenness with mortality in Greece: an ecological study. Environ Res. 2021;196:110348. https://doi.org/10.1016/j.envres.2020.110348.
Acknowledgements
We thank the authors who provided additional data on request: Klompmaker JO, Zhu A, Wu YT, and Brauer M.
Funding
This study was supported by the “Dipartimenti di Eccellenza 2018–2022” grant to the UNIMORE Department of Biomedical, Metabolic, and Neural Sciences from the Italian Ministry of Education, University, and Research, by grants “UNIMORE FAR 2019, 2020 and 2021 Mission Oriented Linea FOMO-Fondazione di Modena” to Dr. Vinceti and Dr. Filippini, by a grant of Local Health Authority of Reggio Emilia to Dr. Vinceti, and by grant no. R00AG066949 from the National Institute of Health to Dr. Jimenez. These funding sources had no role in the design and execution of this study.
Author information
Authors and Affiliations
Contributions
FZ, TF, and MV designed the original study. FZ, TF, and MV analyzed the data and draft the manuscript, and with the contribution of MPJ, LAW, and EEH interpreted the data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the topical collection on FOOD, HEALTH, AND THE ENVIRONMENT.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zagnoli, F., Filippini, T., Jimenez, M.P. et al. Is Greenness Associated with Dementia? A Systematic Review and Dose–Response Meta-analysis. Curr Envir Health Rpt 9, 574–590 (2022). https://doi.org/10.1007/s40572-022-00365-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-022-00365-5