Abstract
The aim of this review is to examine the role of placental pathology in the understanding of singleton stillbirth. The placenta may be regarded as the “black box” of pregnancy and detailed examination may afford insight into the fetal and maternal events leading to this tragic outcome. In the UK, 1 in 200 to 1 in 240 pregnancies end in stillbirth whilst India accounts for the majority of global stillbirths. Between 2010 and 2013, India showed a decline in the stillbirth rate and it continues to fall–a recent report felt that the majority of deaths in the third trimester were preventable. However, in order to prevent such deaths we need to understand their cause. Postmortem studies may cast light on the many factors which lead to stillbirth or early neonatal death but there is anecdotal evidence that certain groups are reluctant to authorise postmortem examination and in a religiously diverse and observant country such as India, postmortem may not be acceptable to families. However, if the purpose of the postmortem study is properly explained, many families would agree to such an examination. In this paper the authors aim to look at how examination of the singleton placenta alone may provide valuable information regarding the causation of stillbirth and indicate potential treatment options for its prevention in future pregnanices. The authors will consider the more commonly encountered lesions, clinically and pathologically and provide guidelines for those less experienced in this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the UK, 1 in 200 to 1 in 240 pregnancies end in stillbirth [1, 2] whilst India accounts for the majority of global stillbirths, due to the high population, with 592,100 out of a total of 2.6 million of such births across the world. Between 2010 and 2013, India showed a decline in the stillbirth rate from 33 per 1000 to 25 per 1000 live births and it contiues to fall [3]–a recent report felt that the majority of deaths in the third trimester were preventable. However, in order to prevent such deaths we need to understand their cause. Postmortem studies may cast light on the many factors which lead to stillbirth or early neonatal death but there is anecdotal evidence that certain groups are reluctant to authorise postmortem examination [4]. Although if the benefits are properly explained, many families agree to such an examination.
There is increasing evidence to show that placental pathology may be the cause of singleton stillbirth in pregnancies at gestation of 24 week or more [5, 6]. The placenta sits at the interface between the mother and the fetus and serves to provide a record of intra uterine events both fetal and maternal – acting as the “black box” of pregnancy. It provides essential nutrients to the developing fetus whilst affording a protective environment. Nutrition of the fetus relies on the placental vascular tree continuing to grow and develop throughout the pregnancy in reponse to the demands of the fetus; whilst the protective function is derived from an ability to mount an inflammatory response in reponse to external factors. Such responses may occur at the maternal – fetal junction where organisms may enter the placental environment whilst fetal antigens may be presented to the maternal immune system allowing a response leading to the release of mediators of inflammation.
A number of conditions are known to be associated with stillbirth including cord abnormalities (insertion site, coiling index etc.) [7], implantation site abnormalities (placenta previa, placenta accreta, increta and percreta), infectious disease processes (maternal or fetal) and compromise to the circulation (maternal or fetal) [5, 6, 8]. Whilst some of these can be readily assessed by the obstetrician or midwife, some require detailed histopathological assessment. The aim of this review is to describe a systematic approach to placental pathology for the less experienced pathologist and a framework for obstetricians to understand the pathological changes described. It is important to recognise that the placenta gives insight into intrauterine events allowing focused care in subsequent pregnancies.
Macroscopic Lesions: Description and Significance
The clnical history and the macrosopic findings will help to guide the assessment of the placenta. Much can be gained from macroscopic examination in the delivery room [9] and the findings may inform the pathologist. The request form, submitted for placental examination, should in all cases include details relating to previous pregnancies, maternal body mass index (BMI), underlying maternal conditions e.g., Diabetes Mellitus or known thrombophilias (e.g., Factor V Leiden), gestational age, birth weight, mode of delivery, Apgar scores and complications, including whether the infant was admitted to the Neonatal Unit.
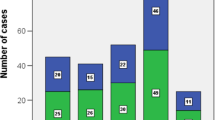
Prior to sampling the placenta the pathologist should give a detailed description of the umbilical cord, extraplacental membranes, placental disc and placental parenchyma. Figures 1 and 2 outline the various lesions which should be described and included in the report.
Pathological examination of the placental disc. IUGR Intrauterine growth restriction; FGR Fetal growth restriction; IUFD Intrauterine fetal death; DM Diabetes mellitus; nRBC nucleated Red blood cells; VUE Villitis of unknown etiology; TORCH Toxoplasmosis, rubella, cytomegalovirus and herpes viruses; APH Antepartum hemorrhage
Umbilical Cord Lesions
Cord lesions may be of significance in causing the death of the fetus in-utero but unfortunately, though a few changes can be detected on ultrasound, it is unclear as how management could be altered to effect improved outcome in the next pregnancy. Indeed it is unclear whether hyper or hypo coiling recurs consistently in families [10,11,12].
The site of insertion is important when considering causation. Marginally inserted cords (< 1 cm from the nearest margin) and velamentous insertions are associated with adverse outcome, including in some studies, preterm labour. However, peripheral cords do not show such a relationship.
Thin cords tend to be associated with intrauterine growth restriction (IUGR) whilst thick cords tend to be related to maternal diabetes, raised BMI and fetal hydrops [13, 14]. Excessively long and excessively short cords tend to be asssociated with adverse outcome as do hyper and hypocoiled cords [10]. Assessment and examination of the cord may prove difficult particularly as assessment of length and degree of coiling relies on the whole cord being submitted for examination – which is often not the case. Therefore, although many studies have shown a relationship with adverse outcome, it can be difficult to achieve consistency in assessment of such lesions. However, in addition to hypocoiling of the cord, hypercoiled sections of cords with strictures or extreme points of narrowing along the length are associated with stillbirth and should be reported.
Placental Lesions
A number of lesions have been recognised in association with stillbirth ≥ 24 week gestation [15]. Placental weight is thought to reflect function and the feto-placental weight ratio has been suggested as a possible indicator of placental reserve capacity in IUGR. However, the functional reserve of the placenta may also be indicated by assessing the size of the disc which should be measured in 3 dimensions. The trimmed weight of the placenta should also be assessed – it may vary by up to 3% with fixation so it is important that the report states whether the placental disc was weighed in the fresh or fixed state. It is important to comment on lesions such as amnion nodosum over the fetal surface which may reflect diminished liquor volume either secondary to premature rupture of membranes (PROM) or to decreased placental reserve. Placental function may be compromised by ischemia and/or infarction and thus any infarct seen in the pre-term placenta or at term anything more than 5% or peripheral infarction should be described and evaluated by volume [8].
The form of the placenta is also crucial—circumvallation tends to be associated with bleeding in early pregnancy and may lead to discoloration of the membranes or to hemosiderin laden macrophages being discerned on histological examination. Including this in the macroscopic description may serve as an indicator to evaluate the membranes with PERLS (PBR) staining.
Retroplacental Hemorrhage
Catastrophic hemorrhage may lead to the death of an infant. Abruption is a clinical diagnosis but the presence or absence of a crater with depression of the maternal cotyledons should be noted and measured. Any clot received should be weighed. As indicated above where hemorrhage is suggested by examination of the membranes or the presence of crater formation or clinically diagnosed, PBR staining of the membranes will help to assess if there have been previous episodes of occult bleeding. Correlating with the Kleihauer-Betke test may also help the clinician to evaluate the size and significance of occult feto-maternal hemorrhage [16, 17] although some authors have suggested that in acute abruption KB testing may not be positive [18]. However chronic occult hemorrhage may occasionally be evident only on placental pathology where the histopathologist may see intervillous thrombi [19] or increased nucleated red cells within the fetal circulation and hemosiderin laden macrophages within the extraplacental membranes.
Sampling of Cord, Membranes and Placental Disc for Histology
In order to allow the maximum utility of the placental report we need to implement a consistent approach to sampling and description of lesions. The Amsterdam Placental Workshop Group in 2015 [20] promotes an agreed protocol for consistent, reproducible approach to examination with clear advice on sampling alongside improved classification and diagnostic criteria for placental lesions. This approach affords consistency across tertiary referral centres, community and district general hospital and helps to inform the scientific research community. It should give pathologists with less experience in placental pathology, confidence in reporting significant lesions and help to establish evidence-based recommendations for placental submission and facilitate global research of factors impacting on outcome. The criteria for sampling the placenta were agreed in order to ensure that the examination was cost-effective and thus likely to be more acceptable to the majority of centres.
Four blocks should be submitted as a minimum: 1 block to include a roll of extraplacental membranes from point of rupture to placental margin – this should include the marginal parenchyma and 2 cross-sections of umbilical cord, 1 from the fetal end and another approx. 5 cm from the placental insertion point. (The authors of this paper would prefer the cord and membranes to be placed in two cassettes in order to ensure that the examination is complete). Three other full thickness blocks should be taken each containing a random section of placental parenchyma derived from the central two-thirds of the disc and include one adjacent to the insertion site itself. If the transmural thickness is too great for the cassette, it should be divided in two and the upper part (subchorionic plate and subjacent tissue) and lower-third (basal aspect) should be placed in the cassette. Alternatively, the section can be divided in two and placed in two separate cassettes.
Detailed Histological Examination of the Placental Disc
Figure 2 provides a guide for the macroscopic and histological assessment of the placental disc. It should be recognised that many of these findings may co-exist; however, a number of patterns may be discerned. The authors have attempted to indicate those which may have a bearing on the the diagnosis of stillbirth and in which further investigations of the mother may be indicated in order to optimise care in the next pregnancy.
Maternal Vascular Malperfusion (MVM) (Fig. 3)
Clinical history and macroscopic examination of the placenta may afford insight into underlying conditions which might lead to maternal vascular malperfusion (previously referred to as maternal vascular underperfusion/ischemia) and guide the histopathological assessment. E.g., placental ischemia secondary to pregnancy induced hypertension (PIH) or pre-eclamptic toxemia (PET) may present with placental hypoplasia [weight low (<10th centile) for gestational age and/or a thin cord with diameter <8 mm at term], infarction and/or retroplacental hemorrhage. Thrombophilia may present with specific patterns of placental pathology [21]. The findings are summarised in Fig. 3 but it should be recognised that these findings may co-exist with other conditions and the figure is not fully comprehensive.
Clinically, the infant may show evidence of intrauterine growth restriction and such findings may indicate further testing to be undertaken by clinicians and possible treatment options to be considered in the next pregnancy. The basic evaluation to check for pre-eclampsia clinically would include baseline renal and liver functions, platelet and urate levels, checking for acquired thrombophilia e.g. lupus anticoagulant and anticardiolipin antibody [22]. These tests should be performed at the time of the fetal loss and if the anticardiolipin antibody or lupus anticoagulant is positive, then it must be repeated in 3 months to confirm the diagnosis. However, maternal vascular malperfusion may also be seen in inherited thrombophilias which have a recognised association with stillbirth [23]. Whilst the prevalence of these thrombophilias in the Indian population has not been extensively investigated, screening for these conditions may help complete the investigations and provide treatment options in the next pregnancy [24, 25].
Fetal Vascular Malperfusion (Fig. 4)
This is now the preferred term for Fetal Thrombotic Vasculopathy (FTV)/Stem Vessel Occlusion [26, 27]. It may arise secondary to a number of conditions which cause obstruction of fetal blood flow, including various cord lesions, hypercoaguability, complications of fetal cardiac dysfunction, hypoxia etc. At present it is defined by thrombosis, segmental avascular villi and stromal karyorrhexis.
Two forms of FVM are recognised: segmental – where the thrombotic obstruction may cause complete occlusion downstream and global – where partial obstruction of the umbilical vessels may lead to intramural fibrin deposition, and small clusters (<5 villi per cluster) of avascular or karyorrhectic villi. Such lesions may be distributed widely throughout the parenchyma. High grade FVM is defined as more than one focus of avascular villi with a cumulative total of ≥45 villi across three sections of parenchyma examined with or without thrombus or two or more occlusive thrombi in the chorionic plate or multiple non-occlusive thrombi, whilst scattered foci of avascular villi and/or stromal karyorrhexis may be used for less severe lesions.
It can be difficult to assign causation to FVM as many of the changes may be seen in involution of the placenta. However, thrombosis may be regarded as a pre-mortem process and investigations for acquired and inherited thrombophilia status of the mother have to be undertaken. Finding of a single discrete focus of avascular villi suggests involution rather than causative pathology [26].
Villitis of unknown etiology (VUE) with stem villitis and avascular villi (obliterative fetal vasculopathy) is regarded as a distinct process where the primary pathology relates to inflammation and damage of the vessel wall (see text below).
Inflammatory Lesions [28]
Ascending Infection
It is important to recognise that inflammation may reflect a fetal or maternal reponse and the nature, site and grade of these should be defined as indicated in Table 1 [29].
Acute chorioamnionitis is an acute inflammation of the membranes and chorion of the placenta generally to microbial infection. Although it is usually an ascending infection, intrauterine infections may also be secondary to spread from a contiguous infection or secondary to hematogenous spread. Histological chorioamnionitis does not always correlate with clinically diagnosed chorioamnionitis and it is therefore important when assigning causation, to have the clinical facts to hand. Confirmatory evidence of infection leading to stillbirth is not always possible as this requires seeing a fetal response within the lung parenchyma, for example. However, there is an association between the inflammatory response noted histologically and neurodevelopmental outcome in live born infants [30]. In such cases, clinical correlation becomes crucial and placental and fetal swabs should be sent fresh after delivery.
Though it may not be possible to diagnose fetal involvement when no autopsy is performed; maternal sepsis and acidosis are recognised high risk factors for stillbirth. Therefore, maternal high vaginal swabs at the time of presentation of an intrauterine death is imperative. The finding of an infection as a cause for stillbirth is important as the families can be reassured that the risk of recurrence is low.
Villitis of Unknown Etiology (VUE)
VUE is a common lesion occurring in approximately 3 to 5% of all term placentas [31, 32]. It is by definition a lymphohistiocytic lesion of the villi in which an infective etiology is excluded and is primarily a histological diagnosis. It has a variable distribution. Low grade refers to lesions with fewer than 10 villi affected and the lesions may be focal (one slide only) or multifocal (more than 1 slide) with high grade referring to multiple foci with more than 10 villi affected in each focus. The distinction is important as there is a relationship between high grade VUE and neurodevelopmental delay (it impairs the fetal circulation) and likelihood of recurrence.
In some instances, it is associated with vascular damage – when inflammatory cells are seen within the vascular walls – in this case both should be described using the term villitis with stem vessel occlusion [27]. It is also advisable to state in the report the site of the lesions in the hope of improved clinical understanding.
The precise cause of VUE is, by nature of the term, unclear but some authors [32] have suggested a relationship between this lesion and an autoimmune diathesis in the mother. Thus, clinically it is wise to screen for such disorders. The common diseases to be screened for include systemic lupus erythematosus, antiphospholipid antibody syndrome, autoimmune disease of the thyroid gland and other mixed connective tissue disorders. Whilst all these investigations could be onerous for the families to fund, the clinician can adopt a judicial approach based on history and examination. The routine clinical investigations, however, should ideally include screening for lupus anticoagulant and antiphospholipid antibody, which are quite prevalent and thyroid peroxidase antibody. Where applicable, check for extractable nuclear antigen antibodies (ENA screening).
Other lesions thought to have an underlying autoimmune basis include Eosinophilic/T cell vasculitis, chronic intervillositis and chronic deciduitis. All of these may have a recurrence risk and merit investigation of the mothers’ immune status – which may in turn lead to preventative treatment in subsequent pregnancies.
Impaired Glucose Tolerance, Raised Maternal BMI and Diabetes Mellitus
Impaired glucose tolerance/diabetes mellitus is known to be associated with increased morbidity during pregnancy and an increased risk of stillbirth [33, 34]. There is a high incidence of impaired glucose tolerance in the Indian population and the condition is not always diagnosed during the antenatal period. Impaired glucose tolerance may be associated with raised BMI ≥ 35, which in itself is a known risk factor for stillbirth [34, 35]. However, it may be implied by the gross and histological findings within the placenta. Grossly the placenta may appear boggy and plethoric, especially in cases with poor control. Histological assessment of the placenta may show villous immaturity at term with poor development of vasculo-syncytial membranes and increased stromal cells – these findings are seen even when glucose control has been optimized. Villous edema and thickening of the basement membrane may also be seen and such lesions are highly significant.
Chorangiosis
Further, there may be evidence of chorangiosis. Although this may be a marker of hypoxia (it is seen more frequently in mothers living at high altitudes), it is often seen in association with diabetes or in women with raised BMI and also in cases with pre-eclampsia, drug ingestion and urinary tract infection. Chorangiosis is associated with villitis, abruption and umbilical cord anomalies. Chorangiosis is diagnosed when a × 10 ocular objective shows a minimum of 10 villi, each with 10 or more vascular channels, in 10 or more areas of 3 or more random, non-infracted and non-ischemic zones, as defined by Altshuler [36, 37]. Focal chorangiosis is defined as greater than 15 vascular channels within smaller groups of villi [37]. The differential diagnosis between chorangiosis and other vascular lesions can be difficult. Chorangioma refers to a nodular lesion composed entirely of small vascular channels (analogous to hemangiomas in other sites) whilst chorangiomatosis is a less well defined lesion with features between chorangiosis and chorangiomatosis. Further descriptions of this lesion can be found in the literature [38].
Massive Perivillous Fibrin Deposition (Previously Known as Glitter Infarct/Maternal Floor Infarction)
For completeness, one should include this lesion which has an association with fetal death, preterm birth and intrauterine growth restriction and may may recur in subsequent pregnancies [39]. It is characterized by extensive deposition of fibrin within the intervillous space resulting in secondary villous atrophy. It is thought that there may be an immunological basis for the activation of this process leading to platelet aggregation and fibrin deposition [40]. However, Sebire et al. reported an association with primary antiphospholipid syndrome [41].
Conclusions
Postmortem is considered by many to be the gold standard investigation for cause of death in stillbirths and there are a number of benefits that make it a very valuable investigation even in those infants with a prenatal diagnosis [42,43,44]. However, in some cultures postmortem examination may be refused for cultural or religious reasons or simply be too expensive. This refusal is in part confounded by the findings in a number of studies which show that even after a detailed postmortem, the cause of death may remain unknown in 57.9 to >70% though the number where cause of death is identified may rise to >90% when the placenta is examined in detail [5, 45,46,47]. Indeed, examination of the placenta alone may help to define causation and indicate treatment options in subsequent pregnancies. It is hoped that this review, which is not exhaustive, will stimulate interest among Indian pathologists to investigate the placenta whereever possible in the stillbirth population and thus gain more information about these tragic deaths. Consistency in sampling and reporting will not only help clinicians but also inform future research into stillbirth and thus decrease the stillbirth rate.
References
Smith GC, Fretts RC. Stillbirth. Lancet. 2007;370:1715–25.
Heazell AEP, Whitworth MK, Whitcombe J, et al. Research priorities for stillbirth: process overview and results from UK stillbirth priority setting partnership. Ultrasound Obstet Gynecol. 2015;46:641–7.
McClure EM, Saleem S, Goudar SS, et al. Stillbirth rates in low-middle income countries 2010–2013: a population-based, multi-country study from the Global Network. Reprod Health. 2015;12:S7.
Odendaal HJ, Elliott A, Kinney HC, et al. Consent for autopsy research for unexpected death in early life. Obstet Gynecol. 2011;117:167–71.
Pásztor N, Keresztúri A, Kozinszky Z, Pál A. Identification of causes of stillbirth through autopsy and placental examination reports. Fetal Pediatr Pathol. 2014;33:49–54.
Redline RW. Placental pathology: a systematic approach with clinical correlations. Placenta. 2008;29:S86–91.
Pinar H, Carpenter M. Placenta and umbilical cord abnormalities seen with stillbirth. Clin Obstet Gynecol. 2010;53:656–72.
Pinar H, Goldenberg RL, Koch MA, et al. Placental findings in singleton stillbirths. Obstet Gynecol. 2014;123:325–36.
Baergen RN. Macroscopic examination of the placenta immediately following birth. J Nurse Midwifery. 1997;42:393–402.
Machin GA, Ackerman J, Gilbert-Barness E. Abnormal umbilical cord coiling is associated with adverse perinatal outcomes. Pediatr Dev Pathol. 2000;3:462–71.
De Laat MWM, Franx A, Nikkels PGJ, Visser GHA. Prenatal ultrasonographic prediction of the umbilical coiling index at birth and adverse pregnancy outcome. Ultrasound Obstet Gynecol. 2006;28:704–9.
Ernst LM, Minturn L, Huang MH, Curry E, Su EJ. Gross patterns of umbilical cord coiling: correlations with placental histology and stillbirth. Placenta. 2013;34:583–8.
Milnerowicz-Nabzdyk E, Zimmer M, Tlolka J, Michniewicz J, Pomorski M, Wiatrowski A. Umbilical cord morphology in pregnancies complicated by IUGR in cases of tobacco smoking and pregnancy-induced hypertension. Neuroendocrinol Lett. 2010;31:842–7.
Binbir B, Yeniel AO, Ergenoglu AM, Kazandi M, Akercan F, Sagol S. The role of umbilical cord thickness and HbA1c levels for the prediction of fetal macrosomia in patients with gestational diabetes mellitus. Arch Gynecol Obstet. 2012;285:635–9.
Miller ES, Minturn L, Linn R, Weese-Mayer DE, Ernst LM. Stillbirth evaluation: a stepwise assessment of placental pathology and autopsy. Am J Obstet Gynecol. 2016;214:115.e1–6.
Pelikan DM, Scherjon SA, Mesker WE, et al. Quantification of fetomaternal hemorrhage: a comparative study of the manual and automated microscopic Kleihauer–Betke tests and flow cytometry in clinical samples. Am J Obstet Gynecol. 2004;191:551–7.
Emery CL, Morway LF, Chung-Park M, Wyatt-Ashmead J, Sawady J, Beddow TD. The Kleihauer–Betke test: clinical utility, indication, and correlation in patients with placental abruption and cocaine use. Arch Pathol Lab Med. 1995;119:1032–7.
Atkinson AL, Santolaya-Forgas J, Matta P, Canterino J, Oyelese Y. The sensitivity of the Kleihauer–Betke test for placental abruption. J Obstet Gynaecol. 2015;35:139–41.
Benirschke K, Burton GJ, Baergen RN. Transplacental hemorrhage, cell transfer, trauma. In: Pathology of the human placenta. 6th ed. Berlin: Springer; 2012. p. 461–85.
Yee Khong T, Mooney EE, Ariel I, et al. Sampling and definitions of placental lesions Amsterdam placental workshop group consensus statement. Arch Pathol Lab Med. 2016;140:698–713.
Vora S, Shetty S, Khare M, Ghosh K. Placental histomorphology in unexplained foetal loss with thrombophilia. Indian J Med Res. 2009;129:144–9.
Gogia N, Machin GA. Maternal thrombophilias are associated with specific placental lesions. Pediatr Dev Pathol. 2008;11:424–9.
Saade GR, McLintock C. Inherited thrombophilia and stillbirth. Semin Perinatol. 2002;26:51–69.
Vora S, Shetty S, Salvi V, Satoskar P, Ghosh K. Thrombophilia and unexplained pregnancy loss in Indian patients. Natl Med J India. 2008;21:116–9.
Kumar N, Ahluwalia J, Das R, et al. Inherited thrombophilia profile in patients with recurrent miscarriages: experience from a tertiary care center in north India. Obstet Gynecol Sci. 2015;58:514–7.
Redline RW, Pappin A. Fetal thrombotic vasculopathy: the clinical significance of extensive avascular villi. Hum Pathol. 1995;26:80–5.
Faye-Petersen OM, Reilly SD. Demystifying the pathologic diagnoses of villitis and fetal thrombotic vasculopathy. Neoreviews. 2008;9:e399–410.
Katzman PJ. Chronic inflammatory lesions of the placenta. Semin Perinatol. 2015;39:20–6.
Redline RW, Faye-Petersen O, Heller D, Qureshi F, Savell V, Vogler C; Society for Pediatric Pathology, Perinatal Section, Amniotic Fluid Infection Nosology Committee. Amniotic infection syndrome: nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol. 2003;6:435–48.
Anblagan D, Pataky R, Evans MJ, et al. Association between preterm brain injury and exposure to chorioamnionitis during fetal life. Sci Rep. 2016;6:37932.
Derricott H, Jones RL, Heazell AEP. Investigating the association of villitis of unknown etiology with stillbirth and fetal growth restriction—a systematic review. Placenta. 2013;34:856–62.
Derricott H, Jones RL, Greenwood SL, Batra G, Evans MJ, Heazell AEP. Characterizing villitis of unknown etiology and inflammation in stillbirth. Am J Pathol. 2016;186:952–61.
Mathiesen ER, Ringholm L, Damm P. Stillbirth in diabetic pregnancies. Best Pract Res Clin Obstet Gynaecol. 2011;25:105–11.
Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA. 2014;311:1536–46.
Salihu HM. Maternal obesity and stillbirth. Semin Perinatol. 2011;35:340–4.
Altshuler G. An important placental sign of neonatal morbidity and mortality. Arch Pathol Lab Med. 1984;108:71–4.
Caldarella A, Buccoliero AM, Taddei GL. Chorangiosis: report of three cases and review of the literature. Pathol Res Pract. 2003;199:847–50.
Bagby C, Redline RW. Multifocal chorangiomatosis. Pediatr Dev Pathol. 2011;14:38–44.
Al-Sahan N, Grynspan D, Von Dadelszen P, Gruslin A. Maternal floor infarction: management of an underrecognized pathology. J Obstet Gynaecol Res. 2014;40:293–6.
Romero R, Whitten A, Korzeniewski SJ, et al. Maternal floor infarction/massive perivillous fibrin deposition: a manifestation of maternal antifetal rejection? Am J Reprod Immunol. 2013;70:285–98.
Sebire NJ, Backos M, Goldin RD, Regan L. Placental massive perivillous fibrin deposition associated with antiphospholipid antibody syndrome. BJOG. 2002;109:570–3.
Chichester M. Requesting perinatal autopsy. Am J Matern Nurs. 2007;32:81–6.
Stock SJ, Goldsmith L, Evans MJ, Laing IA. Interventions to improve rates of post-mortem examination after stillbirth. Eur J Obstet Gynecol Reprod Biol. 2010;153:148–50.
Downe S, Kingdon C, Kennedy R, Norwell H, McLaughlin MJ, Heazell AEP. Post-mortem examination after stillbirth: views of UK-based practitioners. Ireland: Elsevier Ireland Ltd; 2012. p. 33–7.
Hospital G, Street T, Gard T, Hoge EA, Kerr C. Causes of death among stillbirths. The stillbirth collaborative research network writing group. JAMA. 2011;306:2459–68.
Dudley DJ, Goldenberg R, Conway D, et al. A new system for determining the causes of stillbirth. Obstet Gynecol. 2010;116:254–60.
Man J, Hutchinson JC, Heazell AE, Ashworth M, Levine S, Sebire NJ. Stillbirth and intrauterine fetal death: factors affecting determination of cause of death at autopsy. Ultrasound Obstet Gynecol. 2016;48:566–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kulkarni, A.D., Palaniappan, N. & Evans, M.J. Placental Pathology and Stillbirth: A Review of the Literature and Guidelines for the Less Experienced. J. Fetal Med. 4, 177–185 (2017). https://doi.org/10.1007/s40556-017-0133-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40556-017-0133-3