Abstract
Purpose of review
The present article will describe the unique factors present in COVID-19 patients that predispose these individuals to develop mucormycosis with emphasis placed on the prevention and treatment of COVID-19-associated mucormycosis (CAM).
Recent findings
Viral specific factors, pre-existing diabetes mellitus, and COVID-19 treatments combine to facilitate the development of mucormycosis. There appears to be a gross overutilization of steroid and antibiotic therapy among COVID-19 patients. Appropriate stewardship of antibiotic and steroid therapy in conjunction with tight glucose control may prevent the development of CAM and facilitate effective treatment with pharmacologic and surgical therapy. Appropriate treatment for CAM has been extrapolated from traditional mucormycosis therapies, and high-level, empiric evidence regarding the efficacy of CAM-specific treatments does not exist.
Summary
Cellular impacts of COVID-19, poor diabetic management, and overuse of antibiotics and corticosteroids likely combine and increase the risk of mucormycosis in COVID-19 patients. Minimizing these risk factors should curb the development of CAM and facilitate the treatment of CAM. Current treatment of CAM has been borrowed from traditional mucormycosis therapy. Future prospective studies are needed to begin developing CAM-specific treatment regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
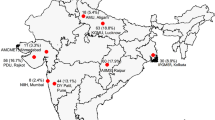
Mucormycosis is a rare, rapidly invasive, fungal infection caused by fungi in the order Mucorales that occurs primarily in immunocompromised individuals [1]. Rhizopus oryzae is the most common culprit responsible for mucormycosis [2]. The first confirmed report of COVID-19-associated mucormycosis (CAM) occurred in May 2020, and over 2000 additional cases of CAM have been identified since that time, representing a geographically disproportionate rise in mucormycosis during the COVID-19 pandemic with the majority of documented cases occurring in India [3, 4••, 5, 6].
Pre-existing comorbidities, viral specific effects, and COVID-associated treatments combine to facilitate the development of CAM. Mucormycosis can occur during or after COVID infection, and although the median duration between COVID infection and development of mucormycosis is between 13 and 18 days [4••, 7], invasive mucor was noted as early as 2 days and as late as 90 days after COVID diagnosis [8]. Other fungal species, including Aspergillus, have produced acute invasive fungal sinusitis in COVID patients,however, mucor has been found to be the causative agent over 90% of the time [9]. While significant disagreement [3] exists in the literature, CAM may represent a more deadly form of mucormycosis with mortality rates around 50%, while previous mortality rates reported for mucormycosis are closer to 33% [4••, 8, 10].
Mucormycosis is suspected following direct examination revealing pallor, eschar, or insensate mucosa and confirmed with fungal culture and tissue biopsy demonstrating invasive fungal organisms. Newer diagnostic options such as in situ hybridization and polymerase chain reaction are infrequently utilized alternatives that have the potential to improve the speed and accuracy of diagnosis in the future [11•, 12]. Effective treatment of mucormycosis involves a high degree of suspicion, prompt diagnosis, mitigation of exacerbating factors, and early initiation of antifungal therapy and surgical debridement (Table 1). Due to the poor outcomes associated with CAM even with prompt treatment, a strong emphasis should be placed on prevention of this devastating disease among COVID patients. This review will focus on the prevention and treatment of novel CAM.
Treatment
Prevention
A number of modifiable and non-modifiable risk factors combine in COVID patients that appear to facilitate the development of mucormycosis. Non-modifiable factors include COVID-19 viral specific effects, such as impaired ciliary clearance [23], hepcidin activation via viral mimicry leading to increased free iron to fuel fungal proliferation [24], free radical mediated endotheliitis [25], and upregulation of receptors like GRP78 and fungal ligand spore coating homolog protein that facilitates fungal angioinvasion [26].
Modifiable risks can be broken down into pre-existing factors, namely diabetes, and treatment-related factors including steroid and antibiotic use. Prior to the COVID-19 endemic, 40% of mucor patients were diabetic [1], while 77% of patients with CAM have pre-existing diabetes. Elevated blood sugar results in glycosylation of transferrin and ferritin, thereby decreasing iron binding and increasing free iron [27]. Abundant free iron stimulates mucor proliferation, and the acidotic environment present in diabetic ketoacidosis facilitates the germination of fungal spores [27].
Corticosteroids impair phagocytic clearance of fungi and increase blood sugar promoting development of mucormycosis [28]. Only critically ill COVID patients with ARDS, high oxygen requirements, or those receiving mechanical ventilation have been shown to benefit from corticosteroids (RECOVERY). In practice, however, a large proportion of non-critically ill COVID patients have received steroids, and these courses are often at higher doses and for longer durations than recommended even for critically ill COVID patients [29].
Antibiotic therapy suppresses normal, healthy bacterial flora leaving the host more vulnerable to invasion by fungus. Approximately 75% of COVID patients receive antibiotic courses despite estimates that bacterial co-infection with COVID-19 occurs in only 8.6% of patients, revealing a substantial overuse of antibiotics in this patient population [30, 31].
While viral specific effects of COVID-19 that predispose patients to the development of CAM may be difficult to combat, there should be close attention to tight glucose control, reservation of steroid therapy for critically ill COVID patients, and good stewardship of antibiotics to prevent the development of CAM. Similarly, for patients who have developed CAM, it is of the utmost importance to address the above modifiable risk factors to optimize the patient’s immune function and create the least hospitable environment possible for the Mucorales fungus.
Therapy
In an effort to avoid re-inventing the wheel, treatment for CAM has been extrapolated from the management of traditional mucormycosis. Currently, high-level, empiric evidence regarding the efficacy of CAM-specific treatments does not exist. Available CAM-specific literature consists of observational case reports, case series, and systematic reviews encompassing a myriad of complex treatment regimens with variable dosages, durations, and combinations of pharmacologic and surgical therapies. The extreme heterogeneity of existing data makes it exceedingly difficult to create meaningful comparisons between treatment regimens for CAM. The following treatment section will summarize the therapies that have been utilized in the management of CAM; however, it is important to note that findings specific to the treatment of CAM are based exclusively on Level V and VI evidence at this time.
Pharmacologic treatment
Amphotericin B
Intravenous amphotericin B (AmB) serves as the first-line medical therapy for treatment of mucormycosis and is the most commonly used treatment for CAM [32]. This drug serves as a broad-spectrum antifungal with a low incidence of clinical resistance among Mucorales strains [33]. AmB comes in a deoxycholate formulation, as well as lipidic formulations, including AmB lipid complex (ABLC) and liposomal AmB (L-AmB). The lipidic formulations tend to be preferred due to their lower risk of nephrotoxicity, increased central nervous system penetration, and decreased side effects like headache, fever, hypotension, dyspepsia, and pain at the injection site [34,35,36]. Of the lipidic options, L-AmB has been shown to induce less toxicity and produce fewer side effects than ABLC [37,38,39]. Due to the potential nephrotoxic effects of AmB, other antifungal options should be considered for patients with severe kidney disease. During AmB therapy, monitoring of hepatic and renal function, careful electrolyte repletion, and adequate hydration are important to recognize and address potential toxicities [35]. Dosing of L-AmB for CAM has ranged from 3 to 10 mg/kg/day [40]. Five to 10 mg/kg/day was recommended in the 2019 Global Guideline for the Diagnosis and Management of Mucormycosis [32],however, a randomized controlled trial evaluating treatment of pulmonary mucormycosis found 3 mg/kg/day dosing to be equally efficacious [41]. Ultimately, the patient’s clinical response and tolerance of the drug should guide dosing. AmB has been previously administered via nebulized solution for topical therapy [42] and has been injected intrathecally with success in mucormycosis patients, though available data is sparse [43, 44]. Intravenous AmB treatment should be continued until clinical improvement is noted, usually sometime between 2 and 4 weeks, before the patient is transitioned to step-down therapy with oral antifungals [45]. A lack of clinical response, progression of disease, or drug intolerance may necessitate earlier transition from AmB to an alternative antifungal. Of note, certain rarer Mucorales strains have not been shown to be sensitive to amphotericin B, including Cunninghamella and Apophysomyces [46].
Posaconazole
Posaconazole is an azole antifungal utilized as a step-down therapy, a salvage therapy following initial treatment with AmB, a first-line therapy in patients who cannot take AmB, or as a mucormycosis prophylactic in at-risk patients [45, 47, 48••]. Posaconazole is the second most commonly used drug for the treatment of CAM after AmB [40]. Despite its use for prophylaxis in immunocompromised patients, mucormycosis has been shown to develop in patients taking posaconazole, which has led providers to primarily use this drug as a second-line treatment [49, 50]. Intravenous dosing is 300 mg BID on the first day followed by 300 mg QD, and oral dosing is 200 mg QID followed by 400 mg BID after stabilization of disease [45]. Therapeutic drug monitoring is recommended, a number of drug interactions exist, and side effects include hepatotoxicity, QTc prolongation, nausea, vomiting, diarrhea. and headache [45].
Isavuconazole
Isavuconazole is an extended-spectrum azole with similar indications as posaconazole for the treatment of CAM [48••]. Although acting via the same mechanism as posaconazole, isavuconazole offers the advantage of a unique formulation that decreases nephrotoxicity and side effects, including hepatotoxicity and QT prolongation, in comparison to other azoles [51]. Additionally, mortality rates in mucormycosis patients treated with first-line isavuconazole therapy have been shown to be equivalent to mortality rates in patients treated with AmB, making this oral medication an excellent alternative for patients who cannot tolerate or do not respond to amphotericin B [52]. Intravenous and oral dosing is 372 mg TID for 2 days, followed by 372 mg “”QD [45]. Therapeutic drug monitoring is not required for isavuconazole [45].
Echinocandins
Echinocandins including caspofungin and anidulafungin have been used in combination with amphotericin B for the treatment of CAM [48••]. While echinocandins alone have poor activity against mucormycosis, in vitro studies have demonstrated synergism between amphotericin B and echinocandins via an unknown mechanism [53, 54]. A study by Reed et al. [55] evaluating 41 patients with rhino-orbital-cerebral mucormycosis found that patients treated with combined amphotericin B and caspofungin therapy had improved survival that was most pronounced in patients with cerebral involvement [55]. Side effects of echinocandins tend to be much milder than those associated with AmB and the azole medications,however, patients can experience fever, rash, edema, nausea, vomiting, diarrhea, bronchospasm, dyspnea, and hypotension [56]. Side effects can often be managed by simply reducing the rate of infusion [57].
Cytokines
Cytokines including interferon gamma (IFN-gamma), granulocyte colony-stimulating factor (GCS-F), and granulocyte-monocyte colony-stimulating factor (GM-CSF) have been utilized in an attempt to bolster the host immune response against mucormycosis. In vitro work has shown both CM-CSF and IFN-gamma may boost the natural immune response against certain Mucorales strains [58, 59]. IFN-gamma is active against the broadest range of fungal organisms [60], and although clinical data is limited, IFN-gamma in combination with nivolumab successfully treated mucormycosis refractory to standard therapies [61], and this drug combination has been used successfully in a CAM patient.
Surgical debridement
Mucormycosis is an angioinvasive process leading to infarction and necrosis of involved tissues. Effective treatment requires surgical debridement to remove devitalized tissue harboring the fungus that cannot be penetrated by systemic antifungal therapy. The combination of antifungal therapy and surgical debridement has been shown to improve survival compared with antifungal therapy alone in CAM patients [62, 63]. An endoscopic endonasal approach provides excellent access and visualization for thorough debridement in the majority of cases; however, when facing frank orbital invasion, exenteration can be considered [10, 64]. Recent evidence suggests that patients with orbital involvement who undergo less invasive treatments, such as retrobulbar amphotericin B injections, may achieve equivalent rates of survival compared to patients who undergo orbital exenteration [65]. Successful debridement usually requires multiple trips to the operating room with targeted biopsies to guide further debridement to ensure clear margins [66].
Hyperbaric oxygen
Hyperbaric oxygen therapy (HBOT) has been shown to inhibit fungal growth, enhance tissue healing and angiogenesis, and correct lactic acidosis, which promotes the efficacy of amphotericin B [67, 68]. Limited evidence from small case series suggests that the addition of HBOT to standard antifungal and surgical therapy may improve survival in mucormycosis patients, especially for diabetic patients [69,70,71]. HBOT used as adjunctive therapy with antifungal and surgical treatment has been successfully utilized in a kidney transplant patient with CAM [72].
Conclusion
Cellular impacts of the COVID-19 virus, uncontrolled diabetes mellitus, overutilization of corticosteroids, and poor stewardship of antibiotics combine in COVID-19 patients to increase their risk of developing mucormycosis. Addressing these modifiable risk factors is crucial for both prevention and successful treatment of CAM. Existing treatment strategies for CAM have been borrowed from traditional mucormycosis therapy. Literature specifically addressing the treatment of CAM is sparse and largely observational. Additionally, the vast heterogeneity among the described treatment regimens utilized for CAM makes meaningful comparisons between specific therapies challenging. Future prospective studies are needed to begin developing evidence-based, CAM-specific treatment regimens.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25(1):26–34. https://doi.org/10.1016/j.cmi.2018.07.011.
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634–53. https://doi.org/10.1086/432579.
Pal R, Singh B, Bhadada SK, Banerjee M, Bhogal RS, Hage N, Kumar A. COVID-19-associated mucormycosis: an updated systematic review of literature. Mycoses. 2021;64(12):1452–9. https://doi.org/10.1111/myc.13338.
•• Sen M, Honavar SG, Bansal R, Sengupta S, Rao R, Kim U, et al. Members of the Collaborative OPAI-IJO Study on Mucormycosis in COVID-19 (COSMIC) Study Group. Epidemiology, clinical profile, management, and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India - collaborative OPAI-IJO study on mucormycosis in COVID-19 (COSMIC), Report 1. Indian J Ophthalmol. 2021;69(7):1670–1692. https://doi.org/10.4103/ijo.IJO_1565_21. Provides key epidemiologic and demographic information on the largest series of COVID-19-associated mucormycosis patients to date.
Fouad YA, Abdelaziz TT, Askoura A, Saleh MI, Mahmoud MS, Ashour DM, et al. Spike in rhino-orbital-cerebral mucormycosis cases presenting to a tertiary care center during the COVID-19 pandemic. Front Med (Lausanne). 2021;8:645270. https://doi.org/10.3389/fmed.2021.645270.
Sharma S, Grover M, Bhargava S, Samdani S, Kataria T. Post coronavirus disease mucormycosis: a deadly addition to the pandemic spectrum. J Laryngol Otol. 2021;135(5):442–7. https://doi.org/10.1017/S0022215121000992.
Patel A, Agarwal R, Rudramurthy SM, Shevkani M, Xess I, Sharma R, et al. Multicenter epidemiologic study of coronavirus disease-associated mucormycosis. India Emerg Infect Dis. 2021;27(9):2349–59. https://doi.org/10.3201/eid2709.210934.
Nagalli S, Kikkeri NS. Mucormycosis in COVID-19: a systematic review of literature. Infez Med. 2021;29(4):504–512. https://doi.org/10.53854/liim-2904-2.
Baghel SS, Keshri AK, Mishra P, Marak R, Manogaran RS, Verma PK, et al. The spectrum of invasive fungal sinusitis in COVID-19 patients: experience from a tertiary care referral center in Northern India. J Fungi (Basel). 2022;8(3):223. https://doi.org/10.3390/jof8030223.
Bhatt K, Agolli A, Patel MH, Garimella R, Devi M, Garcia E, et al. High mortality co-infections of COVID-19 patients: mucormycosis and other fungal infections. Discoveries (Craiova). 2021;9(1):e126. https://doi.org/10.15190/d.2021.5.
• Narayanan S, Chua JV, Baddley JW. Coronavirus disease 2019-associated mucormycosis: risk factors and mechanisms of disease. Clin Infect Dis. 2022;74(7):1279–1283. https://doi.org/10.1093/cid/ciab726. Thorough discussion of the mechanisms driving the development of COVID-19 associated mucormycosis.
Samson R, Dharne M. COVID-19 associated mucormycosis: evolving technologies for early and rapid diagnosis. 3 Biotech. 2022;12(1):6. https://doi.org/10.1007/s13205-021-03080-4.
Ibrahim AS, Gebermariam T, Fu Y, Lin L, Husseiny MI, French SW, et al. The iron chelator deferasirox protects mice from mucormycosis through iron starvation. J Clin Invest. 2007;117:2649–57.
Spellberg B, Ibrahim AS, Chin-Hong PV, Kontoyiannis DP, Morris MI, Perfect JR, et al. The Deferasirox-AmBisome Therapy for Mucormycosis (DEFEAT Mucor) study: a randomized, double-blinded, placebo-controlled trial. J Antimicrob Chemother. 2012;67:715–22.
Watkins TN, Gebremariam T, Swidergall M, Shetty AC, Graf KT, Alqarihi A, et al. Inhibition of EGFR signaling protects from mucormycosis. mBio 2018;9:e01384–18.
Vellanki S, Billmyre RB, Lorenzen A, Campbell M, Turner B, Huh EY, et al. A novel resistance pathway for calcineurin inhibitors in the human-pathogenic mucorales Mucor Circinelloides. mBio 2020;11:e02949–19.
Lewis RE, Ben-Ami R, Best L, Albert N, Walsh TJ, Kontoyiannis DP. Tacrolimus enhances the potency of posaconazole against Rhizopus oryzae in vitro and in an experimental model of mucormycosis. J Infect Dis. 2013;207:834–41.
Chamilos G, Lewis RE, Kontoyiannis DP. Lovastatin has significant activity against zygomycetes and interacts synergistically with voriconazole. Antimicrob Agents Chemother. 2006;50:96–103.
Naeimi Eshkaleti M, Kordbacheh P, Hashemi SJ, Falahati M, Zaini F, Mirhendi H. In vitro activity of amphotericin B in combination with statins against clinical and environmental Rhizopus oryzae strains. Iran J Public Health. 2019;48:943–8.
Liu M, Spellberg B, Phan QT, Fu Y, Fu Y, Lee AS, et al. The endothelial cell receptor GRP78 Is required for mucormycosis pathogenesis in diabetic mice. J Clin Investig. 2010;120:1914–24.
Shirazi F, Pontikos MA, Walsh TJ, Albert N, Lewis RE, Kontoyiannis DP. Hyperthermia sensitizes Rhizopus oryzae to posaconazole and itraconazole action through apoptosis. Antimicrob. Agents Chemother.
Liu Z, Tang J, Sun Y, Gao L. Effects of photodynamic inactivation on the growth and antifungal susceptibility of Rhizopus oryzae. Mycopathologia. 2019;184:315–9.
Koparal M, Kurt E, Altuntas EE, Dogan F. Assessment of mucociliary clearance as an indicator of nasal function in patients with COVID-19: a cross-sectional study. Eur Arch Otorhinolaryngol. 2021;278(6):1863–8. https://doi.org/10.1007/s00405-020-06457-y.
Cavezzi A, Troiani E, Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin Pract. 2020;10(2):1271. https://doi.org/10.4081/cp.2020.1271.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–8. https://doi.org/10.1016/S0140-6736(20)30937-5.
Ibrahim IM, Abdelmalek DH, Elshahat ME, Elfiky AA. COVID-19 spike-host cell receptor GRP78 binding site prediction. J Infect. 2020;80(5):554–62. https://doi.org/10.1016/j.jinf.2020.02.026.
Mitaka H, Kuno T, Takagi H, Patrawalla P. Incidence and mortality of COVID-19-associated pulmonary aspergillosis: a systematic review and meta-analysis. Mycoses. 2021;64(9):993–1001. https://doi.org/10.1111/myc.13292.
Moorthy A, Gaikwad R, Krishna S, Hegde R, Tripathi KK, Kale PG, et al. SARS-CoV-2, Uncontrolled diabetes and corticosteroids-an unholy trinity in invasive fungal infections of the maxillofacial region? A retrospective, multi-centric analysis. J Maxillofac Oral Surg. 2021;20(3):418–25. https://doi.org/10.1007/s12663-021-01532-1.
Gandra S, Ram S, Levitz SM. The “black fungus” in India: the emerging syndemic of COVID-19-associated mucormycosis. Ann Intern Med. 2021;174(9):1301–2. https://doi.org/10.7326/M21-2354.
Calderón-Parra J, Muiño-Miguez A, Bendala-Estrada AD, Ramos-Martínez A, Muñez-Rubio E, Fernández Carracedo E, et al. Inappropriate antibiotic use in the COVID-19 era: factors associated with inappropriate prescribing and secondary complications. Analysis of the registry SEMI-COVID. PLoS One. 2021;16(5):e0251340. https://doi.org/10.1371/journal.pone.0251340.
Langford BJ, So M, Raybardhan S, Leung V, Soucy JR, Westwood D, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27(4):520–31. https://doi.org/10.1016/j.cmi.2020.12.018.
Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405–21. https://doi.org/10.1016/S1473-3099(19)30312-3.
Sun QN, Fothergill AW, McCarthy DI, Rinaldi MG, Graybill JR. In vitro activities of posaconazole, itraconazole, voriconazole, amphotericin B, and fluconazole against 37 clinical isolates of zygomycetes. Antimicrob Agents Chemother. 2002;46(5):1581–2. https://doi.org/10.1128/AAC.46.5.1581-1582.2002.
Mishra V, Bansal KK, Verma A, Yadav N, Thakur S, Sudhakar K, Rosenholm JM. Solid lipid nanoparticles: emerging colloidal nano drug delivery systems. Pharmaceutics. 2018;10(4):191. https://doi.org/10.3390/pharmaceutics10040191.
Laniado-Laborín R, Cabrales-Vargas MN. Amphotericin B: side effects and toxicity. Rev Iberoam Micol. 2009;26(4):223–7. https://doi.org/10.1016/j.riam.2009.06.003.
Borba HHL, Steimbach LM, Riveros BS, Tonin FS, Ferreira VL, Bagatim BAQ, et al. Cost-effectiveness of amphotericin B formulations in the treatment of systemic fungal infections. Mycoses. 2018;61(10):754–63. https://doi.org/10.1111/myc.12801.
Hamill RJ. Amphotericin B formulations: a comparative review of efficacy and toxicity. Drugs. 2013;73(9):919–34. https://doi.org/10.1007/s40265-013-0069-4.
Johnson PC, Wheat LJ, Cloud GA, Goldman M, Lancaster D, Bamberger DM, et al. Safety and efficacy of liposomal amphotericin B compared with conventional amphotericin B for induction therapy of histoplasmosis in patients with AIDS. Ann Intern Med. 2002;137(2):105–9. https://doi.org/10.7326/0003-4819-137-2-200207160-00008.
Sidhu R, Lash DB, Heidari A, Natarajan P, Johnson RH. Evaluation of amphotericin B lipid formulations for treatment of severe coccidioidomycosis. Antimicrob Agents Chemother. 2018;62(7):e02293-e2317. https://doi.org/10.1128/AAC.02293-17.
Dilek A, Ozaras R, Ozkaya S, Sunbul M, Sen EI, Leblebicioglu H. COVID-19-associated mucormycosis: case report and systematic review. Travel Med Infect Dis. 2021;44:102148. https://doi.org/10.1016/j.tmaid.2021.102148.
Muthu V, Agarwal R, Dhooria S, Sehgal IS, Prasad KT, Aggarwal AN, et al. Has the mortality from pulmonary mucormycosis changed over time? A systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(4):538–49. https://doi.org/10.1016/j.cmi.2020.12.035.
Raj P, Vella EJ, Bickerton RC. Successful treatment of rhinocerebral mucormycosis by a combination of aggressive surgical debridement and the use of systemic liposomal amphotericin B and local therapy with nebulized amphotericin–a case report. J Laryngol Otol. 1998;112(4):367–70. https://doi.org/10.1017/s0022215100140484.
Grannan BL, Yanamadala V, Venteicher AS, Walcott BP, Barr JC. Use of external ventriculostomy and intrathecal anti-fungal treatment in cerebral mucormycotic abscess. J Clin Neurosci. 2014;21(10):1819–21. https://doi.org/10.1016/j.jocn.2014.01.008.
Nau R, Blei C, Eiffert H. Intrathecal antibacterial and antifungal therapies. Clin Microbiol Rev. 2020;33(3):e00190-e219. https://doi.org/10.1128/CMR.00190-19.
Malhotra HS, Gupta P, Mehrotra D, Dandu H, Kohli N, Verma V, et al. COVID-19 associated mucormycosis: staging and management recommendations (Report of a multi-disciplinary expert committee). J Oral Biol Craniofac Res. 2021;11(4):569–80. https://doi.org/10.1016/j.jobcr.2021.08.001.
Alastruey-Izquierdo A, Castelli MV, Cuesta I, Monzon A, Cuenca-Estrella M, Rodriguez-Tudela JL. Activity of posaconazole and other antifungal agents against Mucorales strains identified by sequencing of internal transcribed spacers. Antimicrob Agents Chemother. 2009;53(4):1686–9. https://doi.org/10.1128/AAC.01467-08.
Sipsas NV, Gamaletsou MN, Anastasopoulou A, Kontoyiannis DP. Therapy of mucormycosis. J Fungi (Basel). 2018;4(3):90. https://doi.org/10.3390/jof4030090.
•• Madhavan Y, Sai KV, Shanmugam DK, Manimaran A, Guruviah K, Mohanta YK, et al. Current treatment options for COVID-19 associated mucormycosis: present status and future perspectives. J Clin Med. 2022;11(13):3620. https://doi.org/10.3390/jcm11133620. Description of current and possible future treatment options for COVID associated mucormycosis
Schlemmer F, Lagrange-Xélot M, Lacroix C, de La Tour R, Socié G, Molina JM. Breakthrough Rhizopus infection on posaconazole prophylaxis following allogeneic stem cell transplantation. Bone Marrow Transplant. 2008;42(8):551–2. https://doi.org/10.1038/bmt.2008.199.
Lerolle N, Raffoux E, Socie G, Touratier S, Sauvageon H, Porcher R, et al. Breakthrough invasive fungal disease in patients receiving posaconazole primary prophylaxis: a 4-year study. Clin Microbiol Infect. 2014;20(11):O952–9. https://doi.org/10.1111/1469-0691.12688.
Falci DR, Pasqualotto AC. Profile of isavuconazole and its potential in the treatment of severe invasive fungal infections. Infect Drug Resist. 2013;22(6):163–74. https://doi.org/10.2147/IDR.S51340.
Castrejón-Pérez AD, Welsh EC, Miranda I, Ocampo-Candiani J, Welsh O. Cutaneous mucormycosis. An Bras Dermatol. 2017;92(3):304–11. https://doi.org/10.1590/abd1806-4841.20176614.
Drogari-Apiranthitou M, Mantopoulou FD, Skiada A, Kanioura L, Grammatikou M, Vrioni G, et al. In vitro antifungal susceptibility of filamentous fungi causing rare infections: synergy testing of amphotericin B, posaconazole and anidulafungin in pairs. J Antimicrob Chemother. 2012;67(8):1937–40. https://doi.org/10.1093/jac/dks137.
Arikan S, Lozano-Chiu M, Paetznick V, Rex JH. In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother. 2002;46(1):245–7. https://doi.org/10.1128/AAC.46.1.245-247.2002.
Reed C, Bryant R, Ibrahim AS, Edwards J Jr, Filler SG, Goldberg R, et al. Combination polyene-caspofungin treatment of rhino-orbital-cerebral mucormycosis. Clin Infect Dis. 2008;47(3):364–71. https://doi.org/10.1086/589857.
Mroczyńska M, Brillowska-Dąbrowska A. Review on current status of echinocandins use. Antibiotics (Basel). 2020;9(5):227. https://doi.org/10.3390/antibiotics9050227.
Denning DW. Echinocandin antifungal drugs. Lancet. 2003;362(9390):1142–51. https://doi.org/10.1016/S0140-6736(03)14472-8.
Gil-Lamaignere C, Simitsopoulou M, Roilides E, Maloukou A, Winn RM, Walsh TJ. Interferon- gamma and granulocyte-macrophage colony-stimulating factor augment the activity of polymorphonuclear leukocytes against medically important zygomycetes. J Infect Dis. 2005;191(7):1180–7. https://doi.org/10.1086/428503.
Roilides E, Antachopoulos C, Simitsopoulou M. Pathogenesis and host defence against Mucorales: the role of cytokines and interaction with antifungal drugs. Mycoses. 2014;57(Suppl 3):40–7. https://doi.org/10.1111/myc.12236.
Abzug MJ, Walsh TJ. Interferon-gamma and colony-stimulating factors as adjuvant therapy for refractory fungal infections in children. Pediatr Infect Dis J. 2004;23(8):769–73. https://doi.org/10.1097/01.inf.0000134314.65398.bf.
Grimaldi D, Pradier O, Hotchkiss RS, Vincent JL. Nivolumab plus interferon-γ in the treatment of intractable mucormycosis. Lancet Infect Dis. 2017;17(1):18. https://doi.org/10.1016/S1473-3099(16)30541-2.
Hussain S, Baxi H, Riad A, Klugarová J, Pokorná A, Slezáková S, et al. COVID-19-associated mucormycosis (CAM): an updated evidence mapping. Int J Environ Res Public Health. 2021;18(19):10340. https://doi.org/10.3390/ijerph181910340.
Hoenigl M, Seidel D, Carvalho A, Rudramurthy SM, Arastehfar A, Gangneux JP, et al. Perfect JR, White PL, Chakrabarti A; ECMM and ISHAM collaborators. The emergence of COVID-19 associated mucormycosis: a review of cases from 18 countries. Lancet Microbe. 2022;3(7):e543-e552. https://doi.org/10.1016/S2666-5247(21)00237-8.
Ravani SA, Agrawal GA, Leuva PA, Modi PH, Amin KD. Rise of the phoenix: mucormycosis in COVID-19 times. Indian J Ophthalmol. 2021;69(6):1563–8. https://doi.org/10.4103/ijo.IJO_310_21.
Ashraf DC, Idowu OO, Hirabayashi KE, Kalin-Hajdu E, et al. Outcomes of a modified treatment ladder algorithm using retrobulbar amphotericin b for invasive fungal rhino-orbital sinusitis. Am J Ophthalmol. 2022;237:299–309.
Alekseyev K, Didenko L, Chaudhry B. Rhinocerebral mucormycosis and COVID-19 pneumonia. J Med Cases. 2021;12(3):85–89. https://doi.org/10.14740/jmc3637.
Gudewicz TM, Mader JT, Davis CP. Combined effects of hyperbaric oxygen and antifungal agents on the growth of Candida albicans. Aviat Space Environ Med. 1987;58(7):673–8.
Siddiqui A, Davidson JD, Mustoe TA. Ischemic tissue oxygen capacitance after hyperbaric oxygen therapy: a new physiologic concept. Plast Reconstr Surg. 1997;99(1):148–55. https://doi.org/10.1097/00006534-199701000-00023.
Ferguson BJ, Mitchell TG, Moon R, Camporesi EM, Farmer J. Adjunctive hyperbaric oxygen for treatment of rhinocerebral mucormycosis. Rev Infect Dis. 1988;10(3):551–9. https://doi.org/10.1093/clinids/10.3.551.
John BV, Chamilos G, Kontoyiannis DP. Hyperbaric oxygen as an adjunctive treatment for zygomycosis. Clin Microbiol Infect. 2005;11(7):515–7. https://doi.org/10.1111/j.1469-0691.2005.01170.x.
Yohai RA, Bullock JD, Aziz AA, Markert RJ. Survival factors in rhino-orbital-cerebral mucormycosis. Surv Ophthalmol. 1994;39(1):3–22. https://doi.org/10.1016/s0039-6257(05)80041-4.
Arana C, Cuevas Ramírez RE, Xipell M, Casals J, Moreno A, Herrera S, et al. Mucormycosis associated with COVID-19 in two kidney transplant patients. Transpl Infect Dis. 2021;23(4):e13652. https://doi.org/10.1111/tid.13652.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grafmiller, K.T., Lee, J.T. Prevention and Treatment of COVID-19-Associated Mucormycosis. Curr Treat Options Allergy 10, 83–92 (2023). https://doi.org/10.1007/s40521-023-00339-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40521-023-00339-4