Abstract
Background
Sarcopenia, a condition marked by progressive muscle mass and function decline, presents significant challenges in aging populations and those with chronic illnesses. Current standard treatments such as dietary interventions and exercise programs are often unsustainable. There is increasing interest in pharmacological interventions like bimagrumab, a monoclonal antibody that promotes muscle hypertrophy by inhibiting muscle atrophy ligands. Bimagrumab has shown effectiveness in various conditions, including sarcopenia.
Aim
The primary objective of this meta-analysis is to evaluate the impact of bimagrumab treatment on both physical performance and body composition among patients diagnosed with sarcopenia.
Materials and methods
This meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We systematically searched PubMed, Ovid/Medline, Web of Science, and the Cochrane Library databases up to June 2024 using appropriate Medical Subject Headings (MeSH) terms and keywords related to bimagrumab and sarcopenia. Eligible studies were randomized controlled trials (RCTs) that assessed the effects of bimagrumab on physical performance (e.g., muscle strength, gait speed, six-minute walk distance) and body composition (e.g., muscle volume, fat-free body mass, fat body mass) in patients with sarcopenia. Data extraction was independently performed by two reviewers using a standardized form, with discrepancies resolved through discussion or consultation with a third reviewer.
Results
From an initial search yielding 46 records, we screened titles, abstracts, and full texts to include seven RCTs in our meta-analysis. Bimagrumab treatment significantly increased thigh muscle volume (mean difference [MD] 5.29%, 95% confidence interval [CI] 4.08% to 6.50%, P < 0.001; moderate heterogeneity χ2 = 6.41, I2 = 38%, P = 0.17) and fat-free body mass (MD 1.90 kg, 95% CI 1.57 kg to 2.23 kg, P < 0.001; moderate heterogeneity χ2 = 8.60, I2 = 30%, P = 0.20), while decreasing fat body mass compared to placebo (MD − 4.55 kg, 95% CI − 5.08 kg to − 4.01 kg, P < 0.001; substantial heterogeneity χ2 = 27.44, I2 = 89%, P < 0.001). However, no significant improvement was observed in muscle strength or physical performance measures such as gait speed and six-minute walk distance with bimagrumab treatment, except among participants with slower baseline walking speeds or distances.
Discussion and conclusion
This meta-analysis provides valuable insights into the effects of bimagrumab on sarcopenic patients, highlighting its significant improvements in body composition parameters but limited impact on functional outcomes. The observed heterogeneity in outcomes across studies underscores the need for cautious interpretation, considering variations in study populations, treatment durations, and outcome assessments. While bimagrumab shows promise as a safe pharmacological intervention for enhancing muscle mass and reducing fat mass in sarcopenia, its minimal effects on muscle strength and broader physical performance suggest potential limitations in translating body composition improvements into functional gains. Further research is needed to clarify its long-term efficacy, optimal dosing regimens, and potential benefits for specific subgroups of sarcopenic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The European Working Group on Sarcopenia in Older People-2 defines sarcopenia as reduced muscle mass and/or muscle strength as assessed via grip strength or gait speed by [1]. Whilst it affects 5–16% of elderly people as a whole, it is more commonly encountered in younger patients with significant medical conditions such as malignancies, chronic kidney disease, liver cirrhosis, heart failure or cerebrovascular disease [2]. Sarcopenia has been associated with poor quality of life, higher rates of morbidity and mortality, higher rates of hospitalizations, and higher risk of various medical comorbidities including osteoporosis, cognitive impairment, metabolic syndrome, hypertension and depression [2]. Currently, the available management options for sarcopenia include physical exercise programs such as aerobic exercise, resistance training, high-intensity interval training and whole-body vibration therapy as well as dietary modifications including high-protein nutritional supplements, supplementation with vitamin D and anti-oxidant agents [3]. Nevertheless, such physical therapy modalities may not be suitable for a large proportion of patients either due to reduced physical activity capacity or their general medical status. Therefore, with several clinical studies yielding neutral or disappointing results, there is growing interest in developing novel pharmacotherapeutic approaches for the management of sarcopenia [4, 5].
Bimagrumab is a monoclonal antibody that targets both the activin type 2A and B, which are mediators of several TGF-beta family proteins such as activins and myostatin. Blockage of these protein ligands is responsible for muscle atrophy. Activation of Act2RA and Act2RB supports differentiation of human myoblasts [6]. By doing so, it can promote muscle hypertrophy in animals [6] and humans [7] which has an impact on various conditions, including sarcopenia, body myositis, casting-induced disuse atrophy, recovery after hip fractures and chronic obstructive pulmonary disease [8,9,10,11,12]. Its effects are thought to result from the attenuation of negative regulators of muscle mass, such as myostatin [6, 7]. Myostatin, activin A, activin B, and growth and differentiation factor 11 are negative regulators that inhibit skeletal muscle mass through activin type 2 receptors [11]. It has been shown that both humans and animals with genetic mutations that reduce or eliminate myostatin have increased muscle mass, but are otherwise healthy [13, 14].
In the present systematic review and meta-analyzes we sought to evaluate, the efficacy of variable dosing regimens of bimagrumab in adult populations on the course of sarcopenia. Both age-related and medical condition-associated forms of sarcopenia were included in assessing measures of physical activity or muscle strength or techniques measuring muscle mass.
Materials and methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) standards were followed for conducting this meta-analysis [15]. There were no deviations from the search strategy and pre-established methods by authors, emphasizing a full transparency.
Data source and search strategy
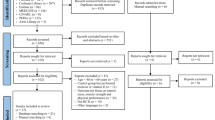
PubMed, Ovid/Medline, Web of Science and Cochrane Library databases were used with the search strategies outlined in Fig. 1. The search was limited to studies published between 1960 through June 2024. Studies published in a peer-reviewed journal in English were included. Additionally, the selected keywords and steps during the search in each database are in detail in Supplementary Table 1. The search criteria were designed and performed by two authors (M.K., S.C.).
Inclusion and exclusion criteria
We included randomized controlled trials (RCTs) that focused on patients diagnosed with sarcopenia and investigated the effects of bimagrumab administration. Eligible studies reported outcomes related to either body composition, such as thigh muscle volume, fat-free body mass, or fat body mass, or physical performance measures like voluntary knee extension strength, hand grip strength, gait speed, and six-minute walk distance. Studies had to be published in peer-reviewed journals and available in English to ensure comprehensive coverage of relevant literature and facilitate clear synthesis of findings.
We excluded non-randomized studies, including observational studies, retrospective or prospective cohort studies, case reports, case series, reviews, and meta-analyses, as they do not provide the rigorous evidence necessary for this systematic review. Studies involving patients who did not meet the diagnostic criteria for sarcopenia or included individuals under the age of 18 were also excluded. Additionally, studies that did not administer bimagrumab as part of their intervention or did not report outcomes related to body composition or physical performance were not considered. Non-English language publications and duplicate reports of the same study were also excluded to maintain clarity and consistency in the review process and to focus on the most relevant and robust evidence available.
Two investigators (M.K. and S.C.) independently screened abstracts and titles of the studies that were reached through the search platforms mentioned above. Bibliographies of the reviews and studies were additionally screened for relevant publications. Discrepancies were resolved by consensus third author D.S.. The selected studies were further investigated by two investigators (M.K. and S.C.) in full text, according to the criteria specified, and were reviewed by M.K. Further, references listed on selected studies and reviews were assessed manually for additional relevant studies. After the preliminary selection, the full texts of the selected studies were evaluated by authors independently. Details of the study selection procedures are depicted in Fig. 1.
Systematic reviews conducted exclusively in English, like in our case, offer several compelling advantages over reviews that include multiple languages. Firstly, focusing on English-only literature ensures a comprehensive coverage of studies from leading academic journals and databases where English is predominantly used. This approach minimizes the risk of missing key research findings that might be less accessible or indexed differently in other languages. Secondly, standardizing the language of publication enhances the consistency and clarity of the review process, facilitating a more coherent synthesis of evidence. This clarity not only improves the accessibility of findings to a wider audience but also enhances the reliability and reproducibility of the review's conclusions. Indeed, limiting systematic reviews to English-language publications has been already shown to exert minimal influence on the effect estimates and overall conclusions drawn from them [16].
Two authors (M.K. and S.C.) were responsible for collecting data from the studies. They extracted various information related to the studies, including their characteristics such as the year of performing and publishing the study, first author, and study design, as well as population characteristics such as age, sex, body mass index (BMI) and HbA1c levels. The authors collected information on thigh muscle volume, fat-free body mass and fat body mass, voluntary knee extension strength, hand grip strength, gait speed, and six-minute walk distance. The collected information is presented in Table 1 and Table 2.
Risk of bias assessment
Risk of bias within included studies was systematically assessed using the Cochrane Collaboration's tool, evaluating random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential sources of bias (Supplementary Table 2). Any discrepancies in data extraction or risk of bias assessments were resolved through consensus or consultation with a third reviewer.
Study objective
Our investigation must include studies in which bimagrumab was administered to individuals with sarcopenia along with assessments of either physical performance or body composition.
Data analysis
We investigated the effect of Bimagrumab on continuous outcomes using a two-tailed variance analysis in samples with known arithmetic means and standard deviations. Generic inverse variance based on calculating absolute differences of mean changes between the experimental and control groups and standard deviations for each comparison within each study were used. We converted the standard error and 95% confidence interval (CI) to standard deviation by using a standard formula [17].
If data were reported at more than one-time point during the study, we used the end-of-treatment data. If a study had more than two intervention arms, the control group sample size was split by the number of subgroup comparisons for that study. The treatment effect was significant if p < 0.05. We assessed for heterogeneity in treatment estimates using the Cochrane Q test and the χ2 statistic (with substantial heterogeneity defined as values > 50%). We conducted a sensitivity analysis to assess the contribution of each study to the pooled treatment effect by excluding each study one at a time and recalculating the pooled treatment effect for the remaining studies (leave-one-out meta-analysis).
Analyses were performed with the Review Manager (Version 5.3, The Cochrane Collaboration 2012).
Results
Selection and description of studies
Our analysis included seven RCTs. The total number of patients included was 660 (minimum 24 [8, 18] and maximum 250 [12] patients) with a follow-up period between 12 [8] and 48 weeks [19]. Except for one study [8] which included only men, all other studies assessed both sexes. Three studies were performed in the USA [7, 8, 18] and 4 were multicentric [10,11,12, 19].
Rooks, Laurent et al. (Rooks 2017a) included young healthy participants [8]; the same group later evaluated individuals with older age [7, 10, 18] (Rooks 2017b, Rooks 2020a, Rooks 2020b) or obesity (Rooks 2020b) [18] in three different studies. Polkey et al. assessed the effect of bimagrumab in chronic obstructive pulmonary disease [11], while Heymsfield et al. included patients with obesity or diabetes mellitus [19]. The most recent study evaluated older patients who had undergone internal fixation or hemiarthroplasty for a proximal femoral fracture [12].
The doses of bimagrumab were different between studies. A single dose of 30 mg/kg bimagrumab was used in two studies [8, 18]. Additionally, in one of these studies, a single dose of 3 mg/kg was used (in the older subgroup of patients [10]). Two studies used two doses of 30 mg/kg bimagrumab (at baseline and 8 weeks) [7, 11]. The rest of the studies administered bimagrumab at 4 weeks – 700 mg [10], 10 mg/kg (with a maximum dose of 1200 mg) [19] and 70 mg, 210 mg or 700 mg [12].
Body composition
4 studies analyzed the effect of bimagrumab on thigh muscle volume (TMV) [7, 8, 10, 11]. Overall, there was a significant increase in TMV levels with bimagrumab treatment (Mean Difference (MD) 5.29%, 95% Confidence Interval (CI) 4.08% to 6.50%, P < 0.001; heterogeneity χ2 = 6.41, I2 = 38%, P = 0.17) (Fig. 2, 1.1.1). The effect of bimagrumab on fat-free body mass (LBM) was assessed in 5 studies [8, 10, 12, 18, 19]. As shown in Fig. 2, 1.1.2, bimagrumab treatment significantly increased fat-free body mass (MD 1.90 kg, 95% CI 1.57 kg to 2.23 kg, P < 0.001; heterogeneity χ2 = 8.60, I2 = 30%, P = 0.20). As compared with placebo, bimagrumab was also effective in reducing fat body mass (MD − 4.55 kg, 95% CI − 5.08 kg to − 4.01 kg, P < 0.001; heterogeneity χ2 = 27.44, I2 = 89%, P < 0.001) (Fig. 2, 1.1.3). [8, 10, 12, 18, 19] Although not included in the meta-analysis because of unit incompatibility of the results, Rooks, Laurent et al. [8] also identified an increase in fat-free body mass and a reduction in fat body mass with bimagrumab treatment (Supplementary Table 3).
Physical performance
Voluntary knee extension strength was assessed in 2 studies [8, 10], and no change in muscle strength was detected in the bimagrumab-treated groups. The effect of treatment on hand grip strength was mixed. Although a minimally, but significant, increase was noted by Rooks et al. [8] at different time points during the study period, no changes were seen in the other two other studies [10, 19]. Similarly, there was no significant difference between bimagrumab and placebo on gait speed [7, 8, 10, 12] or the six-minute walk distance [8, 10], although a sub-analysis of one of the studies suggested that participants with slower walking speed (< 0.8 m/s) or lower 6-min walking distance (< 300 m) at baseline who received bimagrumab consistently increased their gait speed (0.15 m/s) or walking distance (118 m) more than those on placebo [7].
Sensitivity analysis and evaluation of publication bias
The leave-one-out type of analysis was used to assess the influence of each individual study on the overall pooled effect estimate, but also on the heterogeneity of these results. Using this approach, we noticed that most of the heterogeneity observed for the Fat Body Mass analysis was due to the study by Heymsfield et al., suggesting an increased effect of bimagrumab in reducing fat mass in obese and diabetic patients (although this is the study that used the highest doses of bimagrumab, it didn’t influence the heterogeneity in the Lean Body Mass analysis).
With the limitation of a low number of studies included, the funnel plot (Fig. 3) shows a rather symmetrical plot for each of the three outcomes, which makes reporting bias improbable using the type of assessment.
Discussion
Sarcopenia, defined by the presence of low muscle strength, muscle quantity or quality and low physical performance leading to increased risk of adverse events such as falls, fractures and physical disability, has a varying prevalence ranging between 2.5% to 35% depending on the study population with higher rates in elderly populations and depending on the method of investigation and diagnostic criteria utilized [1, 20,21,22]. Although there are considerable variations in the diagnostic criteria in different guidelines, current methods for the evaluation of sarcopenia include bio-impedance analysis, dual-energy X-ray absorptiometry, handgrip strength, walking speed and imaging modalities such as computed tomography or magnetic resonance imaging [23]. Whilst resistance and strength training comprise the backbone of non-pharmacological treatment modalities, there is currently no pharmacotherapeutic approach approved by the United States Food and Drug Administration (FDA) for use in the management of sarcopenia. In this meta-analysis, we aimed to investigate the efficacy of bimagrumab in the management of sarcopenia in terms of alterations in muscle mass and muscle strength. We have shown that bimagrumab therapy leads to statistically significant improvements in fat-free body mass and TMV and a decline in body fat mass, however, no clinically relevant improvement has been recorded in muscle strength assessed via gait speed, six-minute walking distance or hand-grip strength. Such lack of correlation between fat-free body mass or TMV and muscle strength may be attributable to various factors including lack of neural adaptation including recruitment of motor units and de-activation of antagonist muscles, lack of resistance training and relatively short duration of follow-up in clinical trials for such a functional outcome to develop. There is a clear need for future large-scale clinical and pre-clinical studies investigating whether such discordance is related to those confounding factors.
Anabolic agents, frequently utilized in the management of sarcopenia, often yield augmented body mass in affected individuals by promoting muscle protein synthesis. However, their efficacy in enhancing muscle function remains variable and multifactorial. Several factors may contribute to this discordance. Firstly, anabolic agents may selectively target specific muscle fiber types, potentially neglecting those crucial for functional improvements. Secondly, age-related alterations in muscle composition, such as increased intramuscular fat and fibrosis, may impede the translation of increased mass into enhanced function [24]. Additionally, concomitant physical rehabilitation modalities are also effective to gain sufficient amount of strength beyond sole medical treatment [25]. Moreover, individual variability in treatment response, influenced by genetic, hormonal, and behavioral factors, can further confound the relationship between increased mass and improved function [26]. Lastly, inadequate dosages or durations of treatment, treatment compliance, may limit the therapeutic potential of anabolic agents in sarcopenic patients [27]. Understanding these intricacies is paramount in optimizing treatment strategies for sarcopenia, emphasizing the need for comprehensive approaches targeting both mass and function.
Even though the exact underlying physiological mechanisms of sarcopenia are largely unknown, the activin/myostatin pathway appears to have a central role in the regulation of muscular growth and atrophy. The activin receptor pathway has a critical role in hyperplasia, hypertrophy and atrophy of skeletal muscle cells and is under the influence of various signals including therapeutic interventions. The binding of various ligands to activin type II receptors leading to heterodimerization with activin type I receptors activates the signalling pathway in which mitogen-activated protein kinases (MAPK) activation, suppression of mothers against decapentaplegic (Smad) and forkhead box transcription factors (FoxO) activation and phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) pathway inhibition occur [28]. The result is the inhibition of skeletal muscle cell proliferation and hypertrophy via the inhibition of genes involved in myogenesis and induction of apoptosis causing muscular atrophy [28]. Three major mechanisms have been proposed and investigated in pre-clinical and clinical studies including the use of anti-ligand, primarily against myostatin such as domagrozumab [29,30,31], the use of soluble activin type IIB receptor blockers, namely ACE-031 [32], and use of receptor antagonists such as bimagrumab (Fig. 4).
Another important therapeutic aspect of bimagrumab is patients with peripheral insulin resistance and obesity. A phase II RCT involving 75 participants with type II diabetes mellitus (HbA1c between 6.5–10%) and body-mass index of 28 to 40 kg/m2 has demonstrated statistically significant beneficial effects on fat-free body mass (+ 3.6% vs. − 0.8%, p-value < 0.001), total body fat mass (− 20.5% vs. − 0.5%, p-value < 0.001), HbA1c (− 0.76 vs. 0.04, p-value = 0.005) and total body weight (− 6.5% vs. − 0.8%, p-value < 0.001) over forty-eight week clinical trial period [19]. Similar patterns of improvement in fat-free body mass and total body fat mass have been demonstrated in another clinical trial involving sixteen participants with a mean body-mass index of 29.3 kg/m2 and insulin resistance after receiving a single dose of bimagrumab therapy [33]. Also, another study evaluating the efficiency and safety of bimagrumab therapy on elderly participants with obesity has illustrated effectiveness and safety on 24 participants [18]. Even though the initial clinical results of bimagrumab therapy in the management of obesity appear promising, current literature is primarily limited due to the inclusion of a low number of participants and there is a clear need for future large-scale clinical trials. Moreover, two clinical trials are being conducted to further evaluate such potential clinical use (NCT05933499, NCT05616013).
The major limitations of this meta-analysis study include the heterogeneity of included studies in terms of the methods and criteria utilized for the diagnosis and staging of sarcopenia, the underlying aetiology of sarcopenia, the duration and dosage of bimagrumab therapy, and the basic demographic characteristics of the study populations including age and sex. Such variations limit the generalizability of the results of our meta-analysis. Nevertheless, our meta-analysis study is investigating the efficacy and adverse effect profile of bimagrumab therapy in the management of sarcopenia, which is a growing medical concern, especially in the elderly. However, there is a clear need for future large-scale standardized clinical studies investigating the efficacy and adverse effect profile of bimagrumab therapy in the treatment of sarcopenia.
Conclusion
This meta-analysis study aimed to investigate the effects of bimagrumab, a monoclonal antibody, on muscle mass and strength in adult patients with sarcopenia. The standard treatments for improving skeletal muscle mass and strength in older patients, such as dietary protein intake and resistance exercise training, can be challenging to maintain, so there is growing interest in developing pharmacological treatments that can counter muscle atrophy and enhance functional recovery. Bimagrumab therapy has a positive effect on body composition but does not appear to improve physical performance in the evaluated patient population, although it may be beneficial for those with slower baseline walking speed or distance, according to subgroup analyses. It is safe for individuals with elderly age, obesity and type 2 diabetes mellitus in several studies, making it a suitable candidate for future therapy options.
Data availability
No datasets were generated or analysed during the current study.
References:
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Yuan S, Larsson SC (2023) Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism 144:155533
Papadopoulou SK (2020) Sarcopenia: A Contemporary Health Problem among Older Adult Populations. Nutrients. https://doi.org/10.3390/nu12051293
Ishida J, Saitoh M, Ebner N et al (2020) Growth hormone secretagogues: history, mechanism of action, and clinical development. JCMS rapid commun. https://doi.org/10.1002/rco2.9
Saitoh M, Ishida J, Ebner N et al (2017) Myostatin inhibitors as pharmacological treatment for muscle wasting and muscular dystrophy. JCSM Clinic Rep. https://doi.org/10.17987/jcsm-cr.v2i1.37
Lach-Trifilieff E, Minetti GC, Sheppard K et al (2014) An antibody blocking activin type II receptors induces strong skeletal muscle hypertrophy and protects from atrophy. Mol Cell Biol 34:606–618
Rooks D, Praestgaard J, Hariry S et al (2017) Treatment of sarcopenia with bimagrumab: results from a phase II, randomized, controlled proof concept study. J Am Geriatr Soc 65:1988–1995
Rooks DS, Laurent D, Praestgaard J et al (2017) Effect of bimagrumab on thigh muscle volume and composition in men with casting-induced atrophy. J Cachexia Sarcopenia Muscle 8:727–734
Hanna MG, Badrising UA, Benveniste O et al (2019) Safety and efficacy of intravenous bimagrumab in inclusion body myositis (RESILIENT): a randomised, double-blind, placebo-controlled phase 2b trial. Lancet Neurol 18:834–844
Rooks D, Swan T, Goswami B et al (2020) Bimagrumab vs optimized standard of care for treatment of sarcopenia in community-dwelling older adults: a randomized clinical trial. JAMA Netw Open 3:e2020836
Polkey MI, Praestgaard J, Berwick A et al (2019) Activin type II receptor blockade for treatment of muscle depletion in chronic obstructive pulmonary disease. A randomized Trial. Am J Respir Crit Care Med 199:313–320. https://doi.org/10.1164/rccm.201802-0286OC
Hofbauer LC, Witvrouw R, Varga Z et al (2021) Bimagrumab to improve recovery after hip fracture in older adults: a multicentre, double-blind, randomised, parallel-group, placebo-controlled, phase 2a/b trial. Lancet Healthy Longev 2:e263–e274
Schuelke M, Wagner KR, Stolz LE et al (2004) Myostatin mutation associated with gross muscle hypertrophy in a child. N Engl J Med 350:2682–2688
Kambadur R, Sharma M, Smith TP et al (1997) Mutations in myostatin (GDF8) in double-muscled belgian blue and piedmontese cattle. Genome Res 7:910–916
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1-34
Dobrescu AI, Nussbaumer-Streit B, Klerings I et al (2021) Restricting evidence syntheses of interventions to english-language publications is a viable methodological shortcut for most medical topics: a systematic review. J Clin Epidemiol 137:209–217
Higgins JPT TJ. Handbook for Systematic Reviews of Interventions. https://handbook-5-1.cochrane.org/chapter_7/7_7_3_2_obtaining_standard_deviations_from_standard_errors_and.htm. Accessed 16 July 2024
Rooks D, Petricoul O, Praestgaard J et al (2020) Safety and pharmacokinetics of bimagrumab in healthy older and obese adults with body composition changes in the older cohort. J Cachexia Sarcopenia Muscle 11:1525–1534
Heymsfield SB, Coleman LA, Miller R et al (2021) Effect of bimagrumab vs placebo on body fat mass among adults with type 2 diabetes and obesity: a phase 2 randomized clinical trial. JAMA Netw Open 4:e2033457
Brown JC, Harhay MO, Harhay MN (2016) Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J Cachexia sarcopenia Muscle 7:290–298
Kim H, Hirano H, Edahiro A et al (2016) Sarcopenia: prevalence and associated factors based on different suggested definitions in community-dwelling older adults. Geriatr Gerontol Int 16:110–122
Patel HP, Syddall HE, Jameson K et al (2013) Prevalence of sarcopenia in community-dwelling older people in the UK using the European working group on sarcopenia in older people (EWGSOP) definition: findings from the hertfordshire cohort study (HCS). Age Ageing 42:378–384
Dhillon RJ, Hasni S (2017) Pathogenesis and management of sarcopenia. Clin Geriatr Med 33:17–26
Distefano G, Goodpaster BH (2018) Effects of exercise and aging on skeletal Muscle. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a029785
Tezze C, Sandri M, Tessari P (2023) Anabolic resistance in the pathogenesis of sarcopenia in the elderly: role of nutrition and exercise in young and old people. Nutrients. https://doi.org/10.3390/nu15184073
Liu J, Zhu Y, Tan JK et al (2023) Factors associated with sarcopenia among elderly individuals residing in community and nursing home settings: a systematic review with a meta-analysis. Nutrients. https://doi.org/10.3390/nu15204335
Ooi H, Welch C (2024) Obstacles to the early diagnosis and management of sarcopenia: current perspectives. Clin Interv Aging 19:323–332
Lodberg A (2021) Principles of the activin receptor signaling pathway and its inhibition. Cytokine Growth Fact Rev 60:1–17
Latres E, Pangilinan J, Miloscio L et al (2015) Myostatin blockade with a fully human monoclonal antibody induces muscle hypertrophy and reverses muscle atrophy in young and aged mice. Skelet Muscle 5:34
Becker C, Lord SR, Studenski SA et al (2015) Myostatin antibody (LY2495655) in older weak fallers: a proof-of-concept, randomised, phase 2 trial. Lancet Diabet Endocrinol 3:948–957
Bhattacharya I, Pawlak S, Marraffino S et al (2018) Safety, tolerability, pharmacokinetics, and pharmacodynamics of domagrozumab (PF-06252616), an antimyostatin monoclonal antibody. Healthy Subj Clin Pharmacol Drug Dev 7:484–497
Attie KM, Borgstein NG, Yang Y et al (2013) A single ascending-dose study of muscle regulator ACE-031 in healthy volunteers. Muscle Nerve 47:416–423
Garito T, Roubenoff R, Hompesch M et al (2018) Bimagrumab improves body composition and insulin sensitivity in insulin-resistant individuals. Diab Obes Metab 20:94–102
Acknowledgement
Figure 3 is crafted in biorender.com.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was not funded by any grant.
Author information
Authors and Affiliations
Contributions
Contributed substantially to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work: Mehmet Kanbay, Sidar Copur, Nuri Baris Hasbal, Mustafa Guldan, Dimitrie Siriopol. Drafted the work or revised it critically for important intellectual content: Mehmet Kanbay, Dimitrie Siriopol, Kam Kalantar-Zadeh, Tania Garfias-Veitl, Stephan von Haehling
Corresponding author
Ethics declarations
Conflict of Interest
Dr Kalantar has received honoraria from Fresenius, DaVita, CSL, GSK. Dr. S.v.H. has been a paid consultant for and/or received honoraria payments from Amomed, AstraZeneca, Bayer, Boehringer Ingelheim, BRAHMS, Edwards Lifesciences, MSD, Novartis, Pfizer, Pharmacosmos, Respicardia, Roche, Servier, Sorin, and Vifor. S.v.H. reports research support from Amgen, AstraZeneca, Boehringer Ingelheim, Pharmacosmos, IMI, and the German Center for Cardiovascular Research (DZHK). Other Authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kanbay, M., Siriopol, D., Copur, S. et al. Effect of Bimagrumab on body composition: a systematic review and meta-analysis. Aging Clin Exp Res 36, 185 (2024). https://doi.org/10.1007/s40520-024-02825-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02825-4