Abstract
Background
Sedentary behavior, or time spent sitting, may increase risk for dynapenic abdominal obesity (DAO), but there are currently no studies on this topic.
Aims
Therefore, we investigated the association between sedentary behaviour and DAO in a nationally representative sample of older adults from six low- and middle-income countries.
Methods
Cross-sectional data from the Study on Global AGEing and Adult Health were analysed. Dynapenia was defined as handgrip strength < 26 kg for men and < 16 kg for women. Abdominal obesity was defined as waist circumference of > 88 cm (> 80 cm for Asian countries) for women and > 102 cm (> 90 cm) for men. DAO was defined as having both dynapenia and abdominal obesity. Self-reported sedentary behavior was categorized as ≥ 8 h/day (high sedentary behaviour) or < 8 h/day. Multivariable multinomial logistic regression was conducted.
Results
Data on 20,198 adults aged ≥ 60 years were analyzed [mean (SD) age 69.3 (13.1) years; 54.1% females]. In the overall sample, ≥ 8 h of sedentary behavior per day (vs. <8 h) was significantly associated with 1.52 (95%CI = 1.11–2.07) times higher odds for DAO (vs. no dynapenia and no abdominal obesity), and this was particularly pronounced among males (OR = 2.27; 95%CI = 1.42–3.62). Highly sedentary behavior was not significantly associated with dynapenia alone or abdominal obesity alone.
Discussion
High sedentary behaviour may increase risk for DAO among older adults.
Conclusions
Interventions to reduce sedentary behaviour may also lead to reduction of DAO and its adverse health outcomes, especially among males, pending future longitudinal research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dynapenic abdominal obesity (DAO) is defined as the co-existence of abdominal obesity and low muscle strength [1], and its prevalence has been reported to be high in the general population, particularly among older adults [2]. DAO is an emerging important risk concept as recent studies have shown that this condition is associated with a high risk for a myriad of adverse health outcomes including falls [3, 4], cognitive impairment [5], worsening disability, and premature mortality [6]. Given this, it is particularly important to identify risk factors of DAO among the older population to inform targeted interventions in the prevention of DAO and its adverse health outcomes.
While the specific risk factors for DAO are largely unknown, one potentially important risk factor may be sedentary behavior. Sedentary behavior refers to any waking behavior with an energy expenditure ≤ 1.5 metabolic equivalent task units (METs), while in a reclining, sitting, or lying posture [7]. Sedentary behavior could potentially increase risk for DAO as excessive sedentary time has been associated with higher risk for its individual components (i.e., central obesity and weak muscle strength) [8,9,10]. Specifically, reduction in energy expenditure due to excessive sedentary behavior can lead to central obesity, while sedentary behavior can potentially cause low muscle strength via absence of muscle contractile activity, and other physiological consequences on muscle metabolism [11].
While no literature exists on the relationship between sedentary behavior and DAO, a small number of studies exist on the association between sedentary behavior and sarcopenic obesity. Sarcopenic obesity is defined as low skeletal muscle mass coupled with high levels of adiposity [12], and is a similar but distinctly different concept from DAO, as low skeletal muscle mass does not always correspond with muscle strength [13]. Specifically, one cross-sectional study which included 1286 British men, aged 70 to 92 years, found that sedentary time was associated with an increased risk of sarcopenic obesity independent of levels of moderate-to-vigorous physical activity [14]. In another cross-sectional study including black South African women between the ages of 60–85 years (n = 122) from a low-income community, it was observed that those with sarcopenic obesity presented with a descriptive profile of higher sedentary time than women without sarcopenic obesity [15]. Of note, this latter study used body mass index (BMI) to define obesity and not indicators of central obesity. Research suggests that BMI does not differentiate between lean body mass and fat mass; therefore, when using BMI as a measure, inaccurate assessment of adiposity is possible [16]. Moreover, existing evidence suggests that central obesity and abdominal deposition of fat are more strongly associated with a plethora of chronic diseases compared to BMI [17].
Given this background, the aim of the present study was to investigate the association between sedentary behavior and DAO in a sample of 20,198 adults aged ≥ 60 years from six low- and middle-income countries (LMICs). DAO may be particularly problematic in LMICs as the speed of ageing is surpassing that of high-income countries in this setting [18], while obesity and dynapenia are likely to be increasing due to changes in lifestyles (e.g., change in dietary habits, greater sedentary behavior).
Methods
The survey
We analyzed data from the Study on Global Ageing and Adult Health (SAGE), which is a publicly available dataset. The principal aim of the survey was to collect information on adult health and wellbeing (mainly older adults) to address the gap in scientific knowledge and reliable data on health and ageing in LMICs. This survey was undertaken in China, Ghana, India, Mexico, Russia, and South Africa between 2007 and 2010. These countries represent diverse geographical locations as well as economic development, and demographic and health transition. Of note, two of the most populous countries in the world (i.e., China and India) were included in the survey. Based on the World Bank classification at the time of the survey, Ghana and India were a low-income country and a lower middle-income country, respectively, while Mexico, Russia, and South Africa were all upper middle-income countries. China was a lower middle-income country when the survey began but became an upper middle-income country in 2010. Details of the survey methodology are provided elsewhere [19]. Briefly, to obtain nationally representative samples, a multistage clustered sampling design method was utilized. With the exception of Mexico, which used a similar but slightly different sampling method, households were classified into two mutually exclusive groups: (a) everyone aged ≥ 50 years were selected from households named “50 + households”, and were invited to complete the individual interview; and (b) a single individual aged 18–49 years was selected from the “18–49 household” for the individual interview. Thus, the sample consisted of adults aged ≥ 18 years including an oversampling of people aged ≥ 50 years. In order to obtain the final sampling units, household enumerations were conducted. Trained interviewers performed face-to-face interviews using a standard questionnaire. Standard translation procedures were undertaken to ensure comparability of the questionnaire between countries. Computer-assisted personal interviews (CAPI) were utilized in half of the interviews in China, while the other half was completed using paper and pencil. Mexico only utilized CAPI, while the other four countries only used paper and pencil format. On average, the duration of the interview was 2.5 h. The survey response rates were: China 93%; Ghana 81%; India 68%; Mexico 53%; Russia 83%; and South Africa 75%. In Mexico, response rates were lowest, possibly due to the short time available for field visits, which did not allow for enough re-visits if the participant was not at home. Sampling weights were created to adjust for the population structure based on information from the United Nations Statistical Division. Ethical approval was obtained from the WHO Ethical Review Committee as well as local ethics research review boards. Written informed consent was obtained from all participants.
Sedentary behavior
To assess sedentary behavior, participants were asked to state how much time they spent usually (expressed in minutes per day) sitting or reclining in total including at work, getting to and from places, at home, or with friends (sitting with friends, sitting at a desk, travelling in bus, car, train, reading, watching television or playing cards). Time spent sleeping was excluded. This single question is derived from the Global Physical Activity Questionnaire (GPAQ) [20]. The variable on sedentary behavior was used as continuous variable, and also as a dichotomous variable (< 8 or ≥ 8 h per day (i.e., highly sedentary)) in the analysis. The eight hours cut-off was selected as previous research showed that being sedentary for ≥ 8 h/day is associated with a higher risk for premature mortality [21].
Dynapenia, abdominal obesity, and dynapenic abdominal obesity
Handgrip strength was measured with a Smedley Hand Dynamometer (Scandidact Aps, Denmark). The definition of dynapenia was < 26 kg for men and < 16 kg for women [22], using the mean value of the two handgrip measurements of the dominant hand. Waist circumference was measured at the midpoint between the lower margin of the least palpable rib and the top of the iliac crest while keeping the measuring tape parallel to the floor. Abdominal obesity was defined as a waist circumference of > 88 cm for women and > 102 cm for men for non-Asian countries (i.e., Ghana, Mexico, Russia, South Africa) [23]. For Asian countries (i.e., China, India), abdominal obesity referred to a waist circumference of > 80 cm for women and > 90 cm for men [24]. Participants were classified into four groups according to dynapenia and abdominal obesity status: (a) No dynapenia and no abdominal obesity; (b) dynapenia alone; (c) abdominal obesity alone; and (d) dynapenia and abdominal obesity (i.e., DAO).
Control variables
The selection of the control variables was based on past literature [25, 26] and included age, sex, highest level of education achieved (≤ primary, secondary, tertiary), country-wise wealth quintiles based on income, marital status (currently married/cohabiting or else), setting (urban or rural), smoking (never, current, past), alcohol consumption, fruit/vegetable consumption, physical activity, number of chronic physical conditions, and disability. Consumers of at least four (females) or five drinks (males) of any alcoholic beverage per day on one day or more in the past week were considered ‘heavy’ drinkers. Those who had ever consumed alcohol but were not heavy drinkers were considered ‘non-heavy’ drinkers [27]. Participants were asked the two following questions: “How many servings of fruit do you eat on a typical day?” and “How many servings of vegetables do you eat on a typical day?”Those who consumed ≥ 2 servings of fruits and ≥ 3 servings of vegetables were considered to have adequate fruit/vegetable consumption [28]. Levels of physical activity were assessed with the Global Physical Activity Questionnaire and were categorized as low, moderate, and high based on conventional cut-offs [20]. Information on 11 chronic physical diseases (angina, arthritis, asthma, chronic back pain, chronic lung disease, diabetes, edentulism, hearing problem, hypertension, stroke, visual impairment) were collected. The details on the diagnosis of these conditions are shown in Table S1 (Appendix). The number of chronic conditions were summed per participant and categorized as 0, 1, and ≥ 2. Standard basic ADL questions were used to assess the level of disability [29,30,31]. The six questions on ADL had the introductory phrase “overall in the last 30 days, how much difficulty did you have” followed by: in washing your whole body?; in getting dressed?; with moving around inside your home?; with eating (including cutting up your food)?; with getting up from lying down?; with getting to and using the toilet? Answer options included none, mild, moderate, severe, extreme/cannot do. Disability was a dichotomous variable where those who answered severe or extreme/cannot do to any of the six questions were considered to have ADL disability [32].
Statistical analysis
The statistical analysis was performed with Stata 14.1 (Stata Corp LP, College station, Texas). Multivariable multinomial logistic regression analysis was conducted to assess the association between sedentary behavior (exposure) and the four-category variable on dynapenia, abdominal obesity, or both (outcome), with no dynapenia and no abdominal obesity being the base category for the outcome. Sedentary behavior was used in the analysis as a dichotomous variable (i.e., < 8 and ≥ 8 h/day) or as a continuous variable (hours/day). Analyses using the overall sample and sex-stratified samples were conducted. The models were adjusted for age, sex, education, wealth, marital status, setting, smoking, alcohol consumption, fruit/vegetable consumption, physical activity, number of chronic physical conditions, disability, and country, except for the sex-wise analysis which was not adjusted for sex. Adjustment for country was done by including dummy variables for each country in the model as in previous SAGE publications [27, 33]. The sample weighting and the complex study design were taken into account in all analyses. Results from the regression analyses are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The level of statistical significance was set at two-sided P < 0.05.
Results
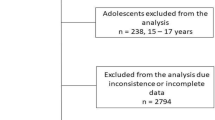
A total of 20,198 adults aged ≥ 60 years were included in the analysis. The sample size of each country was: China n = 7474; Ghana n = 2616; India n = 3621; Mexico n = 1879; Russia n = 2465; South Africa n = 2143. The prevalence of high sedentary behavior (i.e., ≥ 8 h/day) was 13.7%, while the prevalence of dynapenia alone, abdominal obesity alone, and DAO were 25.9%, 27.0%, and 15.1%, respectively. The sample characteristics are provided in Table 1. The mean (SD) age was 69.3 (13.1) years and 54.1% were females. The prevalence of highly sedentary behavior by dynapenia/abdominal obesity status is shown in Fig. 1. Overall, the prevalence of highly sedentary behavior was particularly high among people with DAO (16.7%), but different patterns were observed between men and women. Specifically, DAO alone was associated with a particularly high prevalence of highly sedentary behavior among men but among women, this prevalence was high not only for DAO but also dynapenia alone. Multivariable multinomial logistic regression showed that in the overall sample, ≥ 8 h of sedentary behavior per day (vs. <8 h) was significantly associated with 1.52 (95%CI = 1.11–2.07) times higher odds for DAO (vs. no dynapenia and no abdominal obesity), and this was particularly pronounced among males (OR = 2.27; 95%CI = 1.42–3.62) (Table 2). Eight hours or more of sedentary behavior was not significantly associated with dynapenia alone or abdominal obesity in the overall sample and in the sex-stratified samples, while this was not significantly associated with DAO among females. When the continuous sedentary behavior variable was used (i.e., hours/day), a one-hour increase in sedentary behavior was associated with a significant 1.08 (95%CI = 1.03–1.13) times higher odds for DAO (vs. no dynapenia and no abdominal obesity) in the overall sample, and this was again more pronounced among males (OR = 1.13; 95%CI = 1.06–1.20) (Table 3). In the overall sample and the sample restricted to males, a one-hour increase in sedentary behavior was also associated with a significant 1.06–1.07 times higher odds for dynapenia alone. Sedentary behavior was not significantly associated with abdominal obesity alone (in the overall sample and sex-stratified samples), while increasing sedentary behavior was not significantly associated with dynapenia alone and DAO either among females.
Discussion
Main findings
In our nationally representative study including more than 20,000 adults aged ≥ 60 years from six LMICs, we found that the prevalence of highly sedentary behavior (i.e., ≥ 8 h/day) (13.7%) and DAO (15.1%) were high. Furthermore, multivariable multinomial logistic regression showed that in the overall sample, excessive sedentary behavior was significantly associated with 1.52 (95%CI = 1.11–2.07) times higher odds for DAO (vs. no dynapenia and no abdominal obesity), and this was particularly pronounced among males (OR = 2.27; 95%CI = 1.42–3.62). When the sedentary behavior variable was used as a continuous variable (hours/day), increasing hours spent in sedentary behavior was significantly associated with increased odds for DAO in the overall sample and males, but not females. To the best of the authors’ knowledge, this is the first study to investigate the association between sedentary behavior and DAO.
Interpretation of the findings
Our novel finding that sedentary behavior is associated with an increase in odds for DAO is indeed an important finding as DAO has been shown to be related with multiple detrimental health outcomes, including, for example, cognitive impairment, falls, disability, and premature mortality [3, 5, 6].
There are several plausible mechanisms that likely explain why sedentary behavior is associated with higher odds for DAO. First, sedentary behavior is characterized by a low energy expenditure, and when intake exceeds energy expenditure, fat accumulation occurs [34], especially in the abdominal region in the case of older adults [35]. Second, sedentary behavior could potentially reduce muscular strength through lack of muscle contractile activity, and other physiological consequences on muscle metabolism (e.g. reduces muscle glucose) [11]. This is particularly problematic in older adults as there is a natural loss of muscle strength with ageing [36]. Interestingly, in the present study, highly sedentary behavior was only associated with DAO and not dynapenia alone nor abdominal obesity alone. This finding suggests that when one exhibits excessive sedentary behavior, these two conditions likely develop simultaneously and not alone. For example, obesity can increase risk for weak muscle strength as fatty infiltration of muscle can cause low muscle strength, while abdominal obesity can potentially decrease muscle strength via endocrine and inflammatory mechanisms [37].
Another important finding from the present study was that the relationship between sedentary behavior and DAO was only significant in men. While the reason for this sex difference is unclear, it could be related to difference in body fat distribution. Indeed, males are known to accumulate more fat in the abdominal cavity than females, and this fat accumulation starts at a younger age [38]. In addition, age-related loss of muscle strength has been reported to be more pronounced in males than females and also commences at a younger age in males [39]. Previous studies have shown that abdominal obesity can lead to a reduction in hormonal and neural trophic aspects in the muscles, via chronic inflammation and reduction in tolerance to glucose [40]. Thus, it could be that males are more likely to accumulate abdominal fat due to sedentary behavior than females, and that this can lead to more pronounced muscle weakness than in females.
Implication of the study findings
Findings from the present study suggest that interventions to reduce sedentary behavior among older adults may aid in the prevention of DAO and its associated adverse health outcomes, particularly in males. One such approach may be to utilize self-regulatory strategies (e.g., setting goals, problem-solving and planning, providing normative feedback), as such strategies have been shown to lead to declines in sedentary behavior among older adults [41]. Moreover, interventions to displace sedentary behavior with physical activity and strength training may be particularly effective as physical activity and strength training have been found to reduce central adiposity and slow down the natural decline of age-related muscle atrophy and strength [42,43,44,45,46].
Strengths and limitations
The analysis of large representative samples of older adults from six LMICs and the novel investigation of the sedentary behavior-DAO association are clear strengths of the present work. However, findings must be interpreted in light of the study’s limitations. First, the study was cross-sectional in nature, and therefore, the direction of the association cannot be determined. For example, it is also possible that people with DAO prefer to be sedentary due to factors such as fear of falling. Second, the variable on sedentary behavior was based on self-report, and thus, recall bias is possible. Future studies should consider using objective measures of sedentary behavior. Third, we only had limited information regarding dietary factors (i.e., fruit and vegetable consumption), and thus, we were unable to assess the influence of other dietary factors in the association between sedentary behavior and DAO, such as total caloric intake. Fourth, given that institutionalized people were not included in the survey, our study results cannot be generalized to this population that could have higher prevalence of sedentary behavior and DAO. Finally, the survey was undertaken between 2007 and 2010. The social and economic conditions of the six nations investigated have changed since this time, and thus, it is not known whether the same associations would be observed if the study was repeated currently. However, considering that the underlying mechanism of the association between sedentary behaviour and DAO is likely to be predominantly physiological, it could be speculated that the association has not changed drastically in recent years.
Conclusion
In the present study including large representative samples of older adults from six LMICs, it was found that sedentary behavior is associated with increased odds for DAO. Interventions to reduce sedentary behavior among older adults may have the additional benefit of preventing DAO and its adverse health outcomes. However, future longitudinal or interventional studies are needed to make concrete recommendations.
Data availability
No datasets were generated or analysed during the current study.
References
De Oliveira Máximo R, de Oliveira DC, Ramírez PC et al (2021) Dynapenia, abdominal obesity or both: which accelerates the gait speed decline most? Age Ageing 50:1616–1625
de Araújo FC, da Silva KS, Ohara DG et al (2022) Prevalence of and risk factors for dynapenic abdominal obesity in community-dwelling older adults: a cross-sectional study. Cien Saude Colet 27:761–769
Lv D, Shen S, Chen X (2022) Association between dynapenic abdominal obesity and fall risk in older adults. Clin Interv Aging 17:439
Kushkestani M, Parvani M, Ghafari M, Avazpoor Z (2022) The role of exercise and physical activity on aging-related diseases and geriatric syndromes. Sport TK-Revista Euroam Ciencias Del Deport 11:6
Oba K, Tamura Y, Ishikawa J et al (2022) Dynapenic abdominal obesity is associated with mild cognitive impairment in patients with cardiometabolic disease: a cross-sectional study. BMC Geriatr 22:1–9
Rossi AP, Fantin F, Caliari C et al (2016) Dynapenic abdominal obesity as predictor of mortality and disability worsening in older adults: a 10-year prospective study. Clin Nutr 35:199–204
Tremblay MS, Aubert S, Barnes JD et al (2017) Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int J Behav Nutr Phys Act 14:1–17
Tigbe WW, Granat MH, Sattar N, Lean MEJ (2017) Time spent in sedentary posture is associated with waist circumference and cardiovascular risk. Int J Obes 41:689–696
Lee S-Y, Son D-H, Lee Y-J (2020) Relationship between sedentary time and handgrip strength in healthy Korean women: Korea National Health and Nutrition Examination Survey 2014–2016. Korean J Fam Med 41:422
López Sánchez GF, Vigueras Hernández MR, Lucas Casas P et al (2022) Impact of physical activity, BMI and sociodemographic and lifestyle factors on the risk of diabetes in 9511 Ghanaian adults. Sport TK Rev Euroam ciencias del Deport 11:15
Keevil VL, Wijndaele K, Luben R et al (2015) Television viewing, walking speed, and grip strength in a prospective cohort study. Med Sci Sports Exerc 47:735
Atkins JL (2019) Effects of sarcopenic obesity on cardiovascular disease and all-cause mortality. Nutrition and skeletal muscle. Elsevier, pp 93–103
Chen L, Nelson DR, Zhao Y et al (2013) Relationship between muscle mass and muscle strength, and the impact of comorbidities: a population-based, cross-sectional study of older adults in the United States. BMC Geriatr 13:1–8
Aggio DA, Sartini C, Papacosta O et al (2016) Cross-sectional associations of objectively measured physical activity and sedentary time with Sarcopenia and sarcopenic obesity in older men. Prev Med (Baltim) 91:264–272
Mendham AE, Goedecke JH, Micklesfield LK et al (2021) Understanding factors associated with sarcopenic obesity in older African women from a low-income setting: a cross-sectional analysis. BMC Geriatr 21:1–15
Després J-P (2012) Body fat distribution and risk of cardiovascular disease: an update. Circulation 126:1301–1313
Jayedi A, Soltani S, Zargar MS et al (2020) Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ 370:m3324
Goodman-Palmer D, Ferriolli E, Gordon AL et al (2023) Health and wellbeing of older people in LMICs: a call for research-informed decision making. Lancet Glob Heal 11:e191–e192
Kowal P, Chatterji S, Naidoo N et al (2012) Data resource profile: the World Health Organization Study on global AGEing and adult health (SAGE). Int J Epidemiol 41:1639–1649
Armstrong T, Bull F (2006) Development of the world health organization global physical activity questionnaire (GPAQ). J Public Health (Bangkok) 14:66–70
Ekelund U, Steene-Johannessen J, Brown WJ et al (2016) Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388:1302–1310
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558
World Health Organization (2011) Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008
Romano E, Ma R, Vancampfort D et al (2021) Multimorbidity and obesity in older adults from six low-and middle-income countries. Prev Med (Baltim) 106816
Jacob L, Gyasi RM, Oh H et al (2023) Leisure-time physical activity and sarcopenia among older adults from low‐and middle‐income countries. J Cachexia Sarcopenia Muscle 14(2):1130–1138
Laverty AA, Palladino R, Lee JT, Millett C (2015) Associations between active travel and weight, blood pressure and diabetes in six middle income countries: a cross-sectional study in older adults. Int J Behav Nutr Phys Act 12:1–11
Koyanagi A, Lara E, Stubbs B et al (2018) Chronic physical conditions, multimorbidity, and mild cognitive impairment in low-and middle‐income countries. J Am Geriatr Soc 66:721–727
Smith L, López Sánchez GF, Veronese N et al (2022) Fruit and vegetable intake and non-communicable diseases among adults aged ≥ 50 years in low-and middle-income countries. J Nutr Health Aging 1–7
Backholer K, Wong E, Freak-Poli R et al (2012) Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta‐analysis. Obes Rev 13:456–468
Al Snih S, Graham JE, Kuo Y-F et al (2010) Obesity and disability: relation among older adults living in Latin America and the Caribbean. Am J Epidemiol 171:1282–1288
Katz S, Ford AB, Moskowitz RW et al (1963) Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Koyanagi A, Moneta MV, Garin N et al (2015) The association between obesity and severe disability among adults aged 50 or over in nine high-income, middle-income and low-income countries: a cross-sectional study. BMJ Open 5:e007313
Koyanagi A, Oh H, Vancampfort D et al (2019) Perceived stress and mild cognitive impairment among 32,715 community-dwelling older adults across six low-and middle-income countries. Gerontology 65:155–163
Hill JO, Wyatt HR, Peters JC (2012) Energy balance and obesity. Circulation 126:126–132
Camell CD, Günther P, Lee A et al (2019) Aging induces an Nlrp3 inflammasome-dependent expansion of adipose B cells that impairs metabolic homeostasis. Cell Metab 30:1024–1039
Sternäng O, Reynolds CA, Finkel D et al (2015) Factors associated with grip strength decline in older adults. Age Ageing 44:269–274
Singla P, Bardoloi A, Parkash AA (2010) Metabolic effects of obesity: a review. World J Diabetes 1:76
Nauli AM, Matin S (2019) Why do men accumulate abdominal visceral fat? Front Physiol 1486
Vianna LC, Oliveira RB, Araújo CGS (2007) Age-related decline in handgrip strength differs according to gender. J Strength Cond Res 21:1310–1314
Ellulu MS, Patimah I, Khaza’ai H et al (2017) Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci 13:851–863
White I, Smith L, Aggio D et al (2017) On your feet to earn your seat: pilot RCT of a theory-based sedentary behaviour reduction intervention for older adults. Pilot Feasibility Stud 3:1–14
Harvard Health Publishing (2016) Preserve your muscle mass. https://www.health.harvard.edu/staying-healthy/preserve-your-muscle-mass. Accessed 8 Dec 2023
Strasser B, Schobersberger W (2011) Evidence for resistance training as a treatment therapy in obesity. J Obes 2011:482564
Dodds R, Kuh D, Aihie Sayer A, Cooper R (2013) Physical activity levels across adult life and grip strength in early old age: updating findings from a British birth cohort. Age Ageing 42:794–798
Rodríguez Cabeo D, Inglés López M (2020) The relationship between body image and muscle strength in Spanish children and adolescents. Atena J Public Heal 2:4
Sánchez García C, Zauder R, López Sánchez GF (2019) Analysis of body composition and physical fitness of futsal players at school age according to their level of physical activity, diet and body image. Atena J Sport Sci 1:4
Acknowledgements
This paper uses data from WHO’s Study on Global Ageing and Adult Health (SAGE). SAGE is supported by the U.S. National Institute on Aging through Interagency Agreements OGHA 04034785, YA1323–08-CN-0020, Y1-AG-1005–01 and through research grants R01-AG034479 and R21-AG034263.
Funding
Dr. Guillermo F. López Sánchez is funded by the European Union – Next Generation EU.
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
All authors have made substantial, direct and intellectual contribution to the work, and approved it for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests. Prof. Nicola Veronese is Editor in Chief of Aging Clinical and Experimental Research.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smith, L., López Sánchez, G.F., Rahmati, M. et al. Association between sedentary behavior and dynapenic abdominal obesity among older adults from low- and middle-income countries. Aging Clin Exp Res 36, 109 (2024). https://doi.org/10.1007/s40520-024-02763-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40520-024-02763-1