Abstract
Background
In behavioural assessment, information can be gathered from internally referenced self-reports or from proxy informants.
Aims
This study aimed to fine-tune a brief but reliable method for evaluating the proxy accuracy in cases where responses obtained from adult and older adults’ patient cannot be considered reliable.
Methods
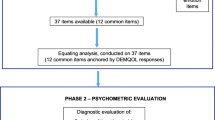
We generated a set of items reflecting both overt and covert behaviours related to the basic instrumental activities of daily living. The psychometric properties of the content, factorial, and criterium validity of these items were then checked. The Proxy Reliability Questionnaire—ProRe was created. We tested the frequency of “I don’t know” responses as a measure of proxy reliability in a sample of healthy older adults and their proxies, and in a second sample of proxy respondents who answered questions about their parents.
Results
As expected, response precision was lower for items characterizing covert behaviours; items about covert compared to overt behaviours generated more “I don’t know” answers. Proxies provided less “I don’t know” responses when evaluating the parent, they claimed they knew better. Moreover, we tried to validate our approach using response confidence. Encouragingly, these results also showed differences in the expected direction in confidence between overt and covert behaviours.
Conclusions
The present study encourages clinicians/researchers to how well the proxy the patient know each other, the tendency of proxies to exhibit, for example, response bias when responding to questions about patients’ covert behaviours, and more importantly, the reliability of informants in providing a clinical assessment of neurocognitive diseases associated with aging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Behaviours are an assembly of adaptive responses that a body equipped with a nervous system performs as a response to environmental stimuli which are also objectively observable [1]. This definition of behaviour emphasizes a person’s experience and socio-cultural context, suggesting that mental states, personality structure, physiology, neurology, genetic expression [2], and behavioural repertoires change.
Behavioural assessment is a powerful and well-established psychological paradigm [3] that can be divided into five types: (a) direct assessment, the study of behaviour as it changes during a given situation, also known as ‘Situational behavioural assessment’. However, it could not accurately capture an individual’s typical behaviour if the method is not standardized; (b) analog assessment, a type of behavioural assessment that studies behavioural change under simulated or made-up situations. It could be limited by the validity of the simulated situation, due to inconsistent data coming from different levels of the definition of the relevant behaviours; (c) idiographic assessment that describes the behavioural characteristics of the individual concerned. It could be affected by bias due to narrow definitions of behaviour that may lead to less consistency in observing behaviour; (d) contextual assessment in which the stimuli in the environment that cause the change in behaviour are in focus. The contextual dependence could influence the results, limiting the generalizability of the same evidence; finally, (e) indirect assessment in which the behaviour is not observed but inferred through retrospective analysis. Indirect assessment is the one that is most frequently adopted for its practicality and cost-effectiveness, at least in the initial stages of clinical evaluation. It is an excellent way to gain the understanding of individual characteristics but is susceptible to reporting bias, providing impressions and opinions and not hard evidence; indeed, the major challenge for this method is accuracy: it depends on grasping the significance of the context in which the behaviour was performed, the strength of episodic memory traces, and the respondents’ motivation and integrity in giving the response [4].
The role of external informants
During an assessment, if patients cannot provide accurate self-reports, it may be important/necessary to make recourse to external informants or proxies. Proxy reports can alternatively be used as a complementary evaluation to improve the accuracy of screening [5]. A proxy is an individual who provides reports on behalf of, or about, a patient, beneficiaries, or nursing home residents. In some cases, they substitute individuals who are unable to reliably self-report their outcomes, for reasons due to cognitive or linguistic impairment that constrains comprehension of items, self-awareness or self-expression, or symptom burden and clinical deterioration in terminal illness. Some aspects of patient health cannot be recorded using behavioural observation scales or performance-based measurement, but through self-report, such as for symptom experience, emotional well-being, and quality of life, in various stages of life. Representative and central examples of proxy reports have been designed specifically for infants and toddlers [6, 7] as well as for people with dementia [8], brain injuries [9], chronic mental illness [10, 11], severe physical illness [12], or those at risk of malingering [13]. In all these cases, patients may not be able to articulate accurately their experience (e.g. young children, people with severe mental illness) or they may be too sick to answer (e.g. end-stage disease), leading to invalid or missing data [14]. In turn, proxy reports could lead the clinician to collect reliable information and increases representativeness in studies [15]. Moreover, proxy ratings represent a way to examine the patient premorbid ability [16] and permit longer follow-up periods, as data collection is not dependent on patient’s capacity to answer [17].
Proxies are essential for minimizing selection bias and preserving external validity [18]. The clinician expects that a proxy’s report can truly integrate/substitute for the patient’s report. Generally, a proxy is a family member, caretaker, or the care staff member who is the closest to the person under evaluation or someone who has significant interactions with the patient. Proxy ratings improve response rates, leaving the costs of data collection practically unchanged [19]. Proxies can help in longitudinal studies where the patient’s condition gets worse over time [16], since data collection is no longer dependent on the patient’s capacity to respond [20]. Moreover, the schooling and the language proficiency of the patient do not seem to affect proxy reports [21].
Some issues may be encountered with proxy data collection. Generally speaking, a critical difficulty with the collection of proxy data is the low level of universality, which makes it more difficult to achieve standardization: different proxy questionnaires must be developed for the different stages of life [22, 23], and, to the best of our knowledge, no proxy questionnaire can be employed across diverse special populations or to assess different functions. However, despite such difficulties, proxy reports are useful for detecting and treating functional impairment and pain in a timely manner [24, 25], for assessing symptoms and the patient’s sense of self-worth, and several other aspects of the health-care situation which patients may not be able to accurately self-report themselves [26,27,28].
Observing overt and covert behaviours
A proxy’s ability to assess target behaviours may vary considerably. Overt behaviours [29] (e.g. public behaviours) are manifest and accessible to external observers, while covert behaviours may be less so. Overt behaviour is a type of external behaviour, which can be observed through physical actions (e.g. eating food, driving a car, falling) and can include verbal behaviours, and facial or bodily gestures. Unlike overt behaviour, covert behaviour is not detectable and consists essentially in mental processes. Covert behaviours include thinking, reasoning, retrieving memories, processing information for decision-making, and cognition [30]. Covert behaviours can be considered private behaviours that are unavailable to other persons [31, 32]. Private behaviours always have an audience of one (the subject), while public events have an audience greater than one [33]. Information on covert behaviours is usually collected from internally referenced self-reports since one of the most direct options for understanding psychological processes is to query the first-person perspective [34]. However, in some cases, such as when people are sick, impaired, unavailable, deceased or because another point of view is wanted, responses from a proxy become relevant [35]. In such case sometimes, the distinction between overt and covert behaviours may be blurred, with the proxy providing opinions that are not based accurate information [36] due to mental bias, a motivation to deceive, or to conform with perceived social desirability [37]. For example, especially in the context of behavioural assessment of child and older adults, proxies characterized by depressive or pessimistic may overestimate the patient conditions. Similarly, proxies with the role of caregivers may overstate the incapacities of the person he/she cares for because of the dependent patterns in their relationship [20]. Moreover, if proxy is a caregiver the Fabricated or Induced Illness by Carers may occur, previously known as the Munchausen Syndrome by Proxy, where caregivers intentionally deceive health practitioners about the person symptoms by subjecting him/her to unnecessary and often painful medical procedures [38]. Finally, socially desirable responding and a context dependent bias to respond in certain way, is due to perceived benefits or access to benefits.
The patient–proxy relationship
The nature of the patient–proxy relationship can influence proxy reports [39, 40]. The type of relationship is formal or informal (e.g. spouse, child, publicly or privately paid home-care professionals), although demographic characteristics of proxies (age, gender, education, and employment status) may play an important role on information reported [20].
For instance, the proxy’s knowledge of the patient can be measured by the amount of time they share with patients, the frequency and intensity of such contact, as well as the quality of their relationship and communication. Usually, the better the proxy’s knowledge and understanding of a patient, the more accurate their evaluation, because a more intimate the proxy/patient relationship, gives proxies more precise, repeated, episodic information regarding the patient’s disease experiences and suffering [41, 42]. It seems that the key issue to consider is the closeness to the patient and the frequency of the interaction with him/her [43]. According to this view, Cummins [44] found substantial differences between family carers and formal carers in a nursing home setting, concerning how often they visit the patient and the accuracy of evaluations.
On the other hand, there are some weaknesses that can affect the quality of information provided by proxy informants. In some cases, they tend to be inaccurate, to emphasize negative information [45], or to respond in what they perceive to be socially desirable with respect to perceived benefits or access to services. In other cases, proxy informants can perceive the patient to be vulnerable and hence in need of overprotection [46]. These psychological–emotional–perceptual mechanisms are relatively common among parents of children/adolescents with chronic conditions, reflecting a level of parental involvement that is excessive, taking into account the child’s actual abilities [47, 48]. Proxy respondents can both over- and underestimate morbidity and disability [40, 49,50,51,52,53,54]. If proxies are unable to accurately report a patient’s perspective, this can produce misleading information [55]. More specifically, considering clinician-reported outcomes, several studies have reported difficulties of formal caregiver in reporting information (e.g. response precision, different schema, [56]) related to less observable domains (e.g. emotional function) compared to more observable domains of health (e.g. physical function) [57, 58].
Close family members or proxy professionals tend to be capable proxies, although proxy reports may be influenced by caregiving burden, especially for those who provide care to older adults or to people with chronic diseases/health condition. Proxy ratings of disability increased with caregiving hours and higher perceived burden, and proxies reporting more burden tended to report more patient impairment [20, 59]. Evidence showed that caregiver burden may result in misleading representation of the older person’s functional status, specifically in regard to instrumental activities of daily living (IADL) items [60].
The reliability of proxy reports
Given everything said so far, it is important to assess the reliability of proxy reports, provided that such evaluations are affordable in terms of human resources and time constraints. Moreover, ensuring the reliability of proxy reports avoids the recommendation that they be used only as supplements, rather than replacements, for self-reports [26]. Proxy reliability is usually measured in terms of response precision and response bias [61]. Response precision refers to the degree to which the proxy’s response agrees with the patient’s response. Response bias is systematic over- or underreporting by the rater in comparison with the patient’s report. Both response precision and bias depend on the nature of the construct being assessed, the characteristics of the patient and the proxy, as well as on the characteristics of the items assessed [13, 62, 63]. Generally, the proxy completes an adapted version of the set of questions patients have addressed and the proxy is asked to answer from the patient’s point of view. Although studies have used a wide range of data collection methods and instruments, most have focused on patients’ health outcomes and quality of life [64].
Yet, it is less clear how socio-demographic characteristics such as the concordance/discordance between proxy–patient gender, age, and education might influence proxy accuracy. Results from the literature are not completely convergent: in some cases, concordance between patient and proxy ratings appears to depend on those factors [65, 66]; in other cases, no significant results have been identified for proxy characteristics [50, 53, 67,68,69,70,71].
Furthermore, such psychological theories predict the precision. It is well known that people adapt to their conditions, and consequently they perceive them differently [72]. This happens also for the conditions of others. One implication of this theory is that the chronicity of a condition will decrease ratings of that condition, especially in ageing. Research on the attitudes and beliefs showed a discrepancy between self- and external ratings because people are inherently biased in their self-ratings, and also towards others [56]. Also, attitudes, beliefs, and stereotypes towards the patient’s health condition or aging itself affect the role of the proxy because self-schemas (e.g. complex implicit internal theories about which aspects of one’s life and of others are stable, and which are subject to change) reorganize memories of events and experiences in order to accommodate beliefs [73]. In such cases, proxy tend to downplay experiences, disinclining to attribute negative symptoms to the patient when there are pertinent implications for himself. For instance, caregivers may consider themselves as a good caretaker, and this belief may be threatened by the patient’s health condition. On the other hand, a caregiver who believes that being a caregiver compromises his/her life and involves failures in various areas of its existence because of the sacrifices he or she makes as a caregiver, might evaluate the patient symptoms as more serious than they really are, supporting this self-concept [56].
Moreover, an understudied aspect of proxy questionnaires that could increase the inaccuracy of responses is the construction of items for proxy rating. It is broadly agreed that an item represents a stimulus and prescribes a response, but it is also important to understand how proxies respond to items [74]. In some cases, notwithstanding conceptual consistency among items—that is, items stem from a certain theory of measurement and their characteristics complement that theoretical framework—it can be hard for a proxy to know how to respond, when items are not about overtly manifested behaviours but rather about the patient’s covert perspective as manifested in thinking, or retrieved memories, or behaviours that the patient mainly performs alone. For instance, this is the case with some questions used in informant interviews to assess dementia outcomes in older people (e.g. “Does the patient have more trouble remembering things that have happened recently than she used to?”). In fact, research on inter-rater reliability has shown that proxy responses were generally more precise and less systematically biased when evaluating more objective domains—such as reporting patients’ symptoms and specific events [54, 75, 76]. Finally, items employed in self-reported measures are often used unchanged in proxy ratings, without taking the responder’s point of view into consideration.
For one, the motivation of a proxy respondent may differ from that of a target respondent, leading to differences in effort, and potential errors in responses provided by the proxy respondent [77]. Proxy respondents may also base their answer on their own behaviours and attitudes and guess instead of using a recall strategy [77, 78]. Respondents’ perspectives also vary depending on whether they are providing a self versus proxy response, and this can influence response quality and error rates. Proxy responses are not based on self-knowledge or first-hand knowledge of events, but rather on the perception of events that happened to someone else, which may be less accurate, detailed, or salient [79, 80].
Finally, another psychological construct that can be considered when proxy responses are analysed is their level of confidence. This concept has recently been deemed important because of its predictive validity for responses [81]. There are two methodologies that measure confidence: a self-report measure, and a measure described as “online.” The online measure is a post-task question, which asks the respondent to rate how confident they are that their answer was correct [82]. The measurement of online confidence developed from early research on decision-making, which employed the use of accuracy ratings in relation to items on cognitive tests [82]. These measures have been described as “online” because they relate to a just completed task and involve a metacognitive judgment of accuracy. Cognitive, personal, and motivational factors influence the level of confidence such as gender with mixed findings [83], personality factors [84] as well as openness and conscientiousness, trait factors as optimism [85], and finally self-concept and self-efficacy as a cognitive representation of one’s own abilities and expectations about successful task completion, respectively [84].
The present study
What if a direct comparison between proxy and patient responses is not possible? As stated by Elliot and colleagues [54], we should treat proxy responses to subjective ratings cautiously. Our study was developed to provide clinically useful answer to this question. We were also motivated by the need to bring more attention to the important topic of proxy reliability, a topic that has been a bit neglected by recent literature yet remains essential and compelling from a clinical point of view.
The Introduction highlights some sources of variation that must be considered in the evaluation of proxy responses. If it is not possible to compare the responses of the proxy with those of the patient or this is not feasible, for example because the latter is affected by a neurocognitive disease or brain injury, it might be useful to find strategies to evaluate proxy reliability per se, with no need for a direct comparison with the patient’s responses.
The smartest strategy would be to evaluate the proxy’s level of knowledge of the patient (e.g. time living together, frequency of contact, etc.). However, as reported in the Introduction, several types of behaviour are hard to evaluate because, for example, they relate to internal states, and proxies’ tendency to respond inaccurately to this kind of question (i.e. to exhibit response bias) cannot be excluded.
We decided to focus on an older adults’ population, considering evidence from the literature that reports from older individuals and their proxies are not highly related on domains such as quality of life and psychological wellbeing [20, 82] but show relatively good agreement with respect to the patient’s functional status, instrumental activities of daily living, and cognitive status [20, 62, 86, 87].
The general aim of the study was to fine-tune a reliable method for evaluating the accuracy of proxy responses when the patient’s answers cannot be considered fully reliable. As mentioned above, this is the situation that most often leads a clinician to turn to a proxy. Ahasic and colleagues [88] previously explored the reliability of assessments made by carefully chosen proxies, by evaluating agreement between patient and proxy responses when assessing activities of daily living (ADLs). Their research suggests that carefully chosen proxies tend to provide reliable information on patients’ functional status and recommend systematic screening to determine the reliability of proxy responses.
The basic idea here is straightforward since it consists in exploiting the difference in proxy responses to question probing the frequency of the patient’s overt versus covert behaviours. The rationale is that reliable and consistent proxies will show signs of being in trouble or uncomfortable when answering questions about covert behaviours. As showed by Evans and colleagues [89], the uncertainty to respond differs according to the nature of the question being asked, generating a feeling of inadequacy in the proxy. Operationally, this difficulty should be manifested as more frequently replying “I don’t know” to for covert than overt questions. To demonstrate the validity of this effect, our study had the following specific aims:
-
1.
To develop and then test the psychometric properties of a set of new items, examining their content validity. For this purpose, we first collected an initial sample of 12 items, reflecting covert and overt behaviours inspired by both indoor and outdoor activities of basic/instrumental daily living. We then asked five experts to provide a qualitative assessment of how well these items elicited information on overt or covert behaviours. Next, we performed exploratory and confirmatory factor analyses (EFA and CFA, respectively) to test the factorial validity of the questionnaire. The final set included 10 items (Study I);
-
2.
To demonstrate the criterium validity of the questionnaire, we employed a sample of healthy older adults and their proxies in a first sub-study, to ascertain a) how response precision, namely the degree to which the proxy’s response agreed with the patient’s response, was lower in the case of items characterizing covert as compared to overt behaviours, b) that the items about covert behaviours generated more “I don’t know” answers than those that represented overt behaviours, and that the level of the proxy’s knowledge of the patient (operationalized here as being or not being a cohabitant) affected the number of “I don’t know” responses. Finally, c) we conducted a replication study (second sub-study) to compare the previous results regarding “I don’t know” answers generated by covert behaviours, using a sample of students who answered questions about their parents. In this case, the level of knowledge students had of their parents was measured by directly asking students to identify the parent they felt they knew best (Study II).
At this point, we asked how the questionnaire could best serve clinicians noting the need for a method that could identify reliable proxies even when direct comparison with patients’ responses could not be made due to the latter’s incapacity. To do this, we decided to validate the effectiveness of our reasoning using online response confidence levels. So, we administered the 10 items questionnaire to a sample of healthy older adults and their proxies, asking the proxy to also report its confidence in the responses (Study III). We expected that reliable proxies would exhibit differences in confidence for overt versus covert behaviours.
Study I–content and factorial validity
Content analysis
The first aim of Study I was to assess the content validity of a set of items designed to probe another person’s overt and covert behaviours. To meet the need for a reliable and valid instrument for assessing both indoor and outdoor covert and overt behaviours, two Authors (AL, AB) developed a pool of 20 test items, in order to start from a streamlined and easy to use tool. After conducting an extensive review of the literature on overt and covert behaviours, identifying the constructs in the theoretical context of interest, they selected those that best represented the constructs and met the guidelines of Clark and Watson [90, 91] for item-writing leading to 12 items. The items addressed common problems encountered when shopping, going for a walk, driving, preparing meals, taking medications, and handling money [92, 93], items compatible with the IADLs, complex activities related to the ability to live independently in the community. Including the basic ADLs, skills required to manage one’s basic physical needs, could have meant intercepting people in a more advanced clinical condition. The 12 original items together with the response modality are shown in Table 1.
Method
A panel of five expert raters, psychologists and psychotherapists expert in psychology of ageing (2 females, age M ± SD: 40.80 ± 7.46, education M ± SD: 21.20 ± 0.40), were asked to judge the 12 items as representative of overt or covert daily living behaviours. Expert evaluation of the concordance was performed through Fleiss’ kappa index [94].
Results
Fleiss’ kappa returned a high coefficient of concordance well above chance. As reported in Table 1, raters achieved perfect agreement. They identified six items covering overt behaviours and six involving overt behaviours.
Exploratory factors analysis
The second aim of Study I was to examine the psychometric properties of the pool of 12 items by testing its dimensionality through an EFA.
Method
Participants
One hundred and sixty-two young adults (93 females, between 19 and 35 years of age; age M ± SD: 23.77 ± 3.08, education M ± SD: 16.52 ± 1.33) took part in the study. All the participants were enrolled from January to February 2021. They were university students who responded to an advertisement and participated without compensation. All participants were blind to the hypothesis of the study and provided informed consent. Participation was anonymous and voluntary. The inclusion criterium for young adults was academic performance considered as a measure of cognitive efficacy [95,96,97,98]. Participants had high/adequate academic achievement measured as the number of exams per years (inclusion cut-off: five or more exams; maximum number of exams per year: seven). The choice to enrol young adults was due to the notion of an early onset of cognitive decline [99], lowering the age of possible proxies. The local Ethical Committee of the Institution approved the study protocol (ET-21-01). Following Hair and colleagues [100], an acceptable sample size for EFA, as well as for CFA, would include observations equal to 5 times the number of observed variables (i.e. items), while a more acceptable ratio would be 10 times the number of observed variables. In the present study, there were 162 observations for 12 observed variables.
Materials and procedure
The 12 items, based on a 5-point Likert-type scale, that provides respondents with a manageable range of options to choose from never (1) to always (5), were shown to the participants, together with a short general anamnesis requiring demographic information. The entire procedure was explained to the participants beforehand. Participants were assessed individually in a well-lit and quiet room without disturbances. Data were collected in a single session. The whole assessment lasted no more than 20 min.
Statistical analysis
The data were analysed using the R software packages psych [101], MVN [102], and lavaan [103]. The assumptions of normality, linearity, homogeneity, and homoscedasticity were checked to identify any violations. Measures of reliability and validity were obtained by measuring internal consistency (Cronbach’s α) and performing EFA according to Arifin’s guidelines [104].
Results
Data were not normally distributed at the multivariate level. The subsequent principal axis factoring (PAF) extraction method was applied to deal with this non-normality. To check the suitability of the data for analysis, we applied the Kaiser–Meyer–Olkin (KMO) Measure of Sampling Adequacy (MSA) and found KMO was equal to 0.80, that is, meritorious [105]. Bartlett’s test of sphericity confirmed significant correlations between the items (χ2 = 668.641; p < 0.001). Cronbach’s alpha was used to examine the internal consistency of items. Any value above 0.7 is usually considered to indicate acceptable reliability for any given scale [106]. Here, the Cronbach’s alpha of the 12 items composing the scale was 0.82. A parallel analysis, performed to determine the number of relevant factors, suggested two factors.
We next ran EFA. As stated above, the data were not normally distributed. For this reason, we chose PAF as the extraction method, because it does not assume normality of data [107] and used the recommended rotation method, Oblimin [108]. The quality of items was then assessed; those that did not load adequately were not well-correlated with their factors. The starting point was to extract the number of factors equal to those suggested by the scree-plot (i.e. two). Two items did not load adequately, that is, above 0.30 [100]. To develop a slender tool, we chose the best five descriptors for each component with adequate communalities, factor loadings, and low item complexity [109,110,111,112] according to Table 2, excluding two items with factor loadings below 0.5 (factor loadings “Practically Significant”, [100]). These items were (Q8) Getting into the bathtub or shower when no one is home, and (Q9) Driving a vehicle after drinking.
The final set comprised 10 items. The two factors were: Covert Behaviours, (Factor 1), and Overt Behaviours (Factor 2). Next, we checked the internal consistency reliability of the factors extracted in the EFA with Cronbach’s alpha. We ascertained the reliability of each factor separately by including the selected items per factor. The Cronbach alphas (0.78 for each factor) indicated adequate internal consistency reliability [113, pp. 95–96]. The total scale reliability was 0.82, which is considered good. The two factors seemed to share a remarkable amount of variance (r = 0.487), as was expected for two facets of the same construct, that is, common daily activities.
Confirmatory factor analysis
Two hundred and forty-four participants were employed to validate the previous analysis by performing a CFA.
Method
Participants
Overall, 244 young adults, 104 females, between 19 and 35 years of age (age M ± SD: 22.41 ± 2.73), took part in the study, enrolled in the same way as for Study II. The mean level of education for the overall sample was 15.72 years (SD = 0.96 years). The inclusion criterium was the same of EFA.
Materials and procedure
Setting and materials were the same as in EFA.
Statistical analysis
CFA was performed using maximum likelihood (ML) estimation to test the construct validity of the identified EFA structure and the fit of the set of items. The adequacy of fit was assessed using the relative Chi-square (χ2/df ≤ 2, [114]), comparative fit index (CFI) ≥ 0.95, Tucker–Lewis Index (TLI) ≥ 0.95, root-mean-square error of approximation (RMSEA) ≤ 0.06, and standardized root mean square residual (SRMR) ≤ 0.08 [115].
Results
CFA was used to test the construct validity of the identified two-domain factor structure of the set of items (see Fig. 1). As the standard Chi-square test may not be a reliable indicator to model adequacy [116], the relative Chi-square fit index (χ2/df) was also considered (values less than two have been suggested to represent “good” data-model fit, [117]). The relative Chi-square fit index for this model satisfied the recommended cut-off values (χ2/df = 1.8). Accepted values were also found for four other “goodness-of-fit” indices (χ2 = 60.32; p ≤ 0.001; CFI = 0.96; TLI = 0.96; RMSEA = 0.06; SRMR = 0.04), suggesting a good fit between the hypothesized model and the observed data [115, 116]. The correlations between factors were also confirmed by CFA. Recurring to the modification indices, the residual co-variances of Q5 and Q12, and Q6 and Q10 were unconstrained to obtain a model with better fit.
Discussion
A new questionnaire was developed, including items that describe overt and covert behaviours in activities of daily living. A panel of five experts was employed to assess content validity. Applying EFA to 12 items yielded a two-factor model with 10 items reflecting overt and covert behaviours with good internal consistency. This model was confirmed by CFA, and construct validity was also supported by the correlations between the two factors. The two factors were called overt and covert behaviour, each consisting of five items. The 10 items were used to produce a questionnaire we named the Proxy Reliability Questionnaire (ProRe). This is a classic questionnaire including questions relating to the frequency of behaviours (overt and covert) in a person of whom s/he had direct and in-depth knowledge (like an older adults’ parent or spouse).
Study II–criterium validity
To pursue the aims of this study, the Proxy Reliability Questionnaire (ProRe) was administered to a sample of healthy older adults and their proxies. Two versions of the questionnaire were employed. The difference between the two versions was that the proxy could provide the answer “I don’t know” in addition to the other answers related to frequency (never, rarely, occasionally, quite often, almost always). It was expected that proxy “I don’t know” answers would appear significantly more often in response to questions regarding covert behaviours.
-
(A)
The occurrence of “I don’t know” answers for overt and covert behaviours
Method
Participants
First, a power analysis was carried out with G*Power 3.1 [118] to estimate the sample size (p level = 0.05; a cautious low effect size = 0.10); and power = 0.80). Results indicated that a sample size of about 90 participants was adequate to warrant an 80% chance of correctly rejecting the null hypothesis. The final sample included ninety-two healthy older adults’ persons (mean age ± sd 71.25 ± 6.66; mean level of education in years ± sd 10.22 ± 4.16), each coupled with a proxy informant. The older adults and proxy informant (mean age ± sd 46.64 ± 17.20; mean level of education in years ± sd 14.03 ± 4.12) were all first-degree relatives (e.g. spouse or son/daughter) who did or did not live together. They were volunteers recruited by word of mouth enrolled in the study from April to May 2021. All participants were blind to the hypothesis of the study and provided informed consent. People with a history of suspected uncompensated systemic/traumatic/psychiatric disease or with a severe vision/hearing loss that could have affected cognition were excluded from the final sample according to the results of a preliminary general anamnesis carried out by three supervised trainees in psychogeriatric assessment. Moreover, global cognitive function was assessed through the General Practitioner Assessment of Cognition test (GPCOG, [119, 120]). The inclusion cut-off was a GPCOG score above 7 (healthy patients mean ± sd 7.89 ± 0.31; proxy informant mean ± sd 8.94 ± 0.22), which had been shown to be the optimal cut-off for discriminating healthy participants from participants with probable cognitive impairment in an Italian sample of older adults [120]. Finally, the Activities of Daily Living and Instrumental Activities of Daily Living (ADL, [121]; IADL [122],) were administered to control for any possible occurrence of functional decline usually associated with dementia (inclusion cut-off higher than 4 for ADL: healthy patients mean ± sd 5.86 ± 0.36; proxy informant mean ± sd 5.90 ± 0.29; higher than 4 for males and 6 for females for IADL: healthy patients mean ± sd 6.97 ± 1.20; proxy informant mean ± sd 7.13 ± 1.10). No one was excluded from the sample.
Materials and procedure
Two versions of the ProRe questionnaire were created (see Supplementary materials), one for the healthy patient who answered for himself, and one for the proxy who provided responses about the patient’s behaviours. The items were administered in the form of questions (e.g. patient version: How often does it happen that you…?; Proxy version: Did Mr/Mrs …?) on a 5-point Likert-like scale from never (1) to almost always (5). Moreover, proxy informants were given the option to respond “I don’t know” in cases where they had no clear memory of item content or were not completely confident in their answer. All the participants completed the questionnaires in Italian through an online survey platform (Google Forms) under the direct control of the research assistants. The Ethical Committee of the Institution approved the general study protocol (n. ET-21-01), and the whole study was performed following the Helsinki Declaration and its later amendments.
Statistical analysis
-
a)
To compute the measure of agreement (beyond chance) between the patient and the proxy, we computed weighted K statistics. This is the standard statistical approach to evaluate response precision between patients and external raters [62], an indicator of inter-rater reliability. The k interpretations by Landis and Koch [123] could be applied to guide interpretation of patient/proxy agreement as poor (< 0.20), fair (0.21–0.4), moderate (0.41–0.60), or substantial (0.61–0.80). Moreover, another way to compute the response precision was used. We evaluated the amount and direction of response discrepancy between the patient and the proxy respondent with the discrepancy score (proxy score–patient score). The main idea of this study was to verify the concordance between patient and proxy, comparing two classes of behaviours. The deviations in scores are interpreted purely as discrepancies, so this score can become a useful marker of the gap between the patient and the proxy point of views [56].
-
b)
Then, a mixed factor ANOVA was performed with behaviour (two levels: overt and covert), as repeated measure, the status of cohabitants (two levels: cohabitants, not cohabitants) as between factor, and the number of “I don’t know” answers as the dependent variable, using gender and age of participants as covariates.
Results
First, we evaluated the discrepancy between proxy and patients’ evaluations. Table 3 presents this data reporting the values of weighted K statistics—the discrepancy score—and the number of “I don’t know” answers. As can be seen from the table, overt behaviours are more easily assessed than covert ones. Accordingly, the gap between the proxy and the patient evaluation shows greater discrepancy for covert compared to overt behaviours. The number of “I don’t know” answers is significantly higher for covert behaviours.
Secondly, we checked whether covert behaviours generated more “I don’t know” answers than those that represented overt behaviours. The results of the mixed factor ANOVA, calculated only on proxy responses, showed the significant main effect of classes of behaviour F(1, 85) = 7.52, p < 0.01; \({\upeta }_{p}^{2}\)= 0.10 (overt: 0.09 ± 0.05; covert: 0.45 ± 0.1), and level of knowledge F(1, 85) = 4.25, p = 0.04; \({\upeta }_{p}^{2}\)= 0.05 (cohabitants: 0.10 ± 0.10; not cohabitants: 0.42 ± 0.10). Moreover, classes of behaviour x level of knowledge, F(1, 85) = 6.91, p = 0.01; \({\upeta }_{p}^{2}\)= 0.07, was also significant. From the inspection of the graph (see Fig. 2), it emerged that the number of “I don’t know” answers was higher for not cohabitants and for covert behaviour. The effects of covariates were not significant.
-
(B)
The occurrence of “I don’t know” answers for overt and covert behaviours: A replication
Method
Participants
The present section of the study was aimed to replicate and extend the previous results regarding the “I don’t know” answers. Firstly, a power analysis was carried out using G*Power 3.1 [118] to estimate the suitable sample size, using the following parameters: p level of 0.05, medium effect size (0.25), and power of 0.80. Results indicated that a sample size of 52 participants was adequate to warrant an 80 per cent chance of correctly rejecting the null hypothesis.
So, to accomplish the third aim of the study (i.e. (c)), a convenience sample of 81 healthy students (40 females), between 18 and 29 years of age (age M ± SD: 20.03 ± 2.47), took part in the study. The mean level of education for the overall sample was 14.38 years (SD = 1.88). All the participants were enrolled from June to July 2021. They were university students who responded to an advertisement and performed the experiment without compensation. All participants were blind to the hypothesis of the study and provided informed consent. Participation was anonymous and voluntary. The inclusion criteria for all participants were: (a) completing the entire survey; (b) cohabiting with the targets of the assessment (i.e. parents); (c) both parents were still in full-time employment; (d) both parents enjoyed good cognitive health. Academic performance was an adequate measure of cognitive efficacy [96, 97, 124, 125]. Young participants had high/adequate academic achievement measured as the number of exams per years (inclusion cut-off five or more exams, maximum number of exams per year: seven). No one was excluded from the sample. Participants freely specified which parent they thought they knew better, their mother or their father, but were nonetheless requested to rate both.
Materials and procedure
Participants completed the proxy version of ProRe questionnaire focusing consecutively on behaviours of their parents. Half the sample was asked to first choose and rate the parent who they thought they knew best, and then the parent who they thought they knew less well, vice versa for the other half. Procedures were the same as in the previous sections of the study.
Statistical analysis
Preliminary counterbalancing was used to control for any order effects in the choice of the parents (better known, less known) on the outcome variable being measured, namely the number of “I don’t know” responses. For the purposes of the study, a within-subjects ANOVA was performed with classes of behaviour (two levels: overt and covert) and the level of knowledge of the parents (two levels: best known, less known) as repeated measures, and the number of “I don’t know” answers as the dependent variable, using gender and age of participants as covariates.
Results
The main effect of classes of behaviour F(1, 75) = 11.13, p = 0.01; \({\upeta }_{p}^{2}\)= 0.12 (overt: 0.19 ± 0.05; covert: 0.40 ± 0.06), and level of knowledge of the parents F(1, 75) = 16.53, p < 0.001; \({\upeta }_{p}^{2}\)= 0.16 (best known: 0.08 ± 0.02; less known: 0.52 ± 0.10) proved to be significant. Moreover, classes of behaviour x level of knowledge, F(1, 75) = 4.50, p = 0.03; \({\upeta }_{p}^{2}\)= 0.05, was also significant. From the inspection of the graph (see Fig. 3), it emerged that the number of “I don’t know” answers was higher for the less known parents and for covert behaviour. The effects of covariate were not significant.
Discussion
In order to verify the criterium validity of the Proxy Reliability Questionnaire (ProRe), we employed two different samples: the first was composed of a group of healthy seniors each with his/her proxy (cohabitants or not cohabitants), while the second comprised students who lived with their parents.
It is often unclear if items in proxy reports refer to objective or subjective events. If survey questions are about objective public circumstances or events, a proxy is more likely to be accurate. When the questions are about events or circumstances that are more subjective or private, involving thinking or reasoning processes, there is an increased risk of receiving inaccurate answers [126]. Indeed, many response biases lead respondents to give answers even when it would be correct/appropriate to refuse to answer at all [127]. Moreover, comparing responses of patients and their proxies, the latter were more accurate in predicting patients’ overt behaviours and had difficulty estimating covert behaviours. This result is consistent with the notion that overt behaviours are more easily assessed than covert ones, because they rely on frequent observation of activities of daily living. It is consistent that being faced with covert behaviour in a condition of lower knowledge increase the likelihood of answers “I don’t know”. As reported in the Introduction, this evidence should make the clinician aware that proxies find some questions hard to respond to [74], but it is unlikely that they will reveal this fact spontaneously. Overall, the findings of the present study suggested that (a) the degree to which the proxy’s response agrees with the patient’s response is lower in the case of items characterizing covert compared to overt behaviours (Section A of the study); (b) the items concerning covert behaviours generated significantly more “I don’t know” answers than those that represented overt behaviours (Sections A and B of the study) and finally (c) comparing different levels of patient/proxy exposure (cohabiting or not, Section A of the study; asking the proxy to judge the best known parent, section B of the study) revealed that “I don’t know” answers were significantly more frequent for covert behaviours and, in turn, for less known parents.
Proxy respondents facing questions regarding covert behaviours might base their answer on their own behaviours and attitudes or appeal to their own beliefs instead of recurring to a recall strategy [78, 126]. Also, ageism could influence the answers [128]: stereotypes associated with aging may influence treatment decisions. Moreover, people have low levels of health literacy regarding ageing [129] that can lead to exaggerated negative responses associated with covert behaviour. Researchers and clinicians could reframe attitudes toward aging, through the mitigation of prejudices and increasing knowledge, allaying the impact of this response bias. In these conditions, the respondent is not answering based on first-hand knowledge of actual events, but rather on their perception of events, which may be less accurate, detailed, or salient [79, 80]. Furthermore, it is known that agreement between proxy and self-responses can vary based on the relationship between the proxy and the individual they are reporting on or on behalf of [130,131,132].
Higher non-response rates for some items by a proxy may indicate either that a proxy respondent does not have sufficient knowledge or that they are not comfortable providing responses to such questions [133]. In the present study, (a) cohabitating (vs. not cohabitating) with the patient, and (b) identifying a cohabitating parent as better known, were associated with reduced “I don’t know” responses. This evidence revealed that proxy respondents’ answers should be considered as accurate as, or more accurate than, responses that would have been given by subjects themselves [134]. The present–concurrent–criterion validity study suggested that a questionnaire that includes questions about both overt and covert behaviours that (those that not directly observable or which refer to mental states) can detect reliable respondents. Such respondents will provide more “I don’t know” answers or rate their confidence lower on covert than on overt questions. As a limitation of this study, it should be noted that the relationship between an older adult and his/her proxy is likely to be much more complex, due to numerous and intricate changes in the older adult's functioning, than student–parent one, and this could affect the answers.
Study III–confidence as a measure of the reliability of proxy respondents
Study III aimed to overcome a limitation that emerged from the previous two studies, regarding participants’ tendency to provide what they perceived to be desirable responses. This could be considered a sort of social-desirability bias, namely the tendency of survey respondents to answer questions in a manner that will be viewed favourably, instead of admitting that they cannot provide a response. We know that there are four cognitive recall states (available, accessible, generatable, ignorant) that characterized the response bases framework [135]. The ignorant state refers to one in which the requested information is not known, and there is no basis to approximate this information. On the one hand, respondents might avoid explicit “I don’t know” answers, providing substantive answers under a broad range of conditions, that is, both in cases where they have precise answers and are making wild guesses (error of commission). On the other hand, the presence of “I don’t know” answers might encourage less motivated respondents to select them as an “easy out” (error of omission). These possible respondent tendencies must be taken seriously when using proxy responses on behalf of a patient. To remedy this problem, we introduced the use of online confidence evaluation of each response. Moreover, studies have shown that confidence better predicts response accuracy when it is measured after a decision related response [136,137,138,139].
Usually, the “I don’t know” responses were not very abundant, indicating that many respondents tried to respond to each question even when it was inappropriate, indicating they suffered from some kind of survey/response bias. The most common online measures come in the form of a numerical confidence rating yoked to individual items in an ability task. Following each item, the respondent is asked to give a confidence rating in response to the question “How confident are you your answer is correct?”.
Method
Participants
For this study, a power analysis was carried out with G*Power 3.1 [118] to estimate the sample size (p level = 0.05; a cautious low effect size = 0.10); and power = 0.80). Results indicated that a sample size of about 90 participants was adequate to warrant an 80% chance of correctly rejecting the null hypothesis. The sample consisted of 90 healthy older adults (mean age ± sd 78.60 ± 6.30; mean level of education in years ± sd 7.76 ± 4.79), each coupled with a proxy informant (mean age ± sd 52.60 ± 8.70; mean level of education in years ± sd 12.23 ± 3.70). Older adults and proxy informant were first-degree relatives (e.g. spouse or child), cohabitants or not and were enrolled in the study from September to November 2022. The inclusion/exclusion criteria were the same as for Study II (GPCOG, healthy patients mean ± sd 8.04 ± 0.66; proxy informant mean ± sd 8.35 ± 0.20; ADL, healthy patients mean ± sd 5.83 ± 0.31; proxy informant mean ± sd 5.87 ± 0.25; IADL: healthy patients mean ± sd 6.98 ± 1.04; proxy informant mean ± sd 7.05 ± 0.96). No one was excluded from the sample.
Materials and procedure
The two versions of the ProRe questionnaire were administered, one for the healthy patient who answered for himself, and one for the proxy who provided responses about the patient’s behaviours with the addition of “I don’t know” answers and online confidence ratings (How confident are you your answer is correct?) along a 5-point Likert-like scale from very unsure (1) to very sure (5).
Statistical analysis
First of all, in order to verify the concordance between patient and proxy, the discrepancy score was calculated on overt and covert behaviours. Then, a mixed factor ANOVA was performed with classes of behaviour (two levels: overt and covert) as repeated measures, level of knowledge (two levels: cohabitants, not cohabitants) as between factors, and discrepancy as the dependent variable, using gender and age of participants as covariates. Moreover, a mixed factor ANOVA was performed with classes of behaviour (two levels: overt and covert) as repeated measures, level of knowledge (two levels: cohabitants, not cohabitants) as between factors, and confidence as the dependent variable, using gender and age of participants as covariates.
Results
We checked whether covert behaviours generated more discrepancy between healthy patients and their proxies than those that represented overt behaviours. The results of the mixed factor ANOVA showed a significant main effect of classes of behaviour F(1, 84) = 8.23, p < 0.01; \({\upeta }_{p}^{2}\)= 0.10 (overt: 0.27 ± 0.05; covert: 0.59 ± 0.05), and level of knowledge F(1, 84) = 21.15, p < 0.001; \({\upeta }_{p}^{2}\)= 0.20 (cohabitants: 0.24 ± 0.07; not cohabitants: 0.62 ± 0.04). The first-order interaction effect was not significant. The effects of covariates were not significant.
Moreover, we investigated differences in confidence between overt and covert behaviours. The results of the mixed factor ANOVA showed the marginal significant main effect of classes of behaviour F(1, 84) = 4.04, p = 0.04; \({\upeta }_{p}^{2}\)= 0.05 (overt: 4.37 ± 0.06; covert: 4.17 ± 0.08), and level of knowledge F(1, 84) = 12.00, p < 0.001; \({\upeta }_{p}^{2}\)= 0.13 (cohabitants: 4.05 ± 0.06; not cohabitants: 0.49 ± 0.09). The first-order interaction effect was not significant. The effects of covariates were not significant.
Discussion
Generally, people feel obliged to provide answers and comply with requests made by researchers [140]. It may also happen that a person gives an answer even when his/her confidence in that answer is low. To overcome this distortive effect, we introduced online confidence ratings, to investigate if a difference in confidence between overt and covert behaviours was present.
The starting point of the present study was to replicate the results obtained in the previous study concerning the accuracy with which a proxy responds to answers regarding overt and covert behaviours. Using the discrepancy score (proxy score–patient score), it emerged that covert behaviours were more difficult to identify than overt behaviours and a higher level of knowledge of the patient, as well as living together, generated a lower level of discrepancy.
The use of the online confidence ratings made it possible to solve the problems described above with the “I don’t know” answer option. The online confidence ratings can be considered marginally significant indicators of proxy accuracy but still promising. The slight difference between overt and covert behaviours represented an important starting point for continuing to use confidence ratings as a measure of proxy reliability.
Probably, as a limitation of this study, the item wording should be improved in order to tap into information reflecting proxy confidence in evaluating patient behaviours. Moreover, the proxy’s level of knowledge of the patient was found significant even when the confidence rating measure was taken into account.
General conclusion
In some clinical situations, patient-reported data are either unavailable or missing. Employing proxy respondents such as family members is a commonly suggested strategy to address this issue [141, 142].
The present study aims to encourage clinicians and researchers to further research the importance of the relationship between the person under evaluation and the proxy respondent, as well as on the content of items and the type of information these items aim to detect. Coming from the same family (cohabiting or not) with a patient who faces with some kind of barriers to providing their own answers to health professionals does not guarantee accurate reports on that person's characteristics, habits, behaviours, goals, preferences. The core aim of this study was to analyse two classes of patient behaviours that are commonly evaluated—overt and covert behaviours—and a source of variation in the evaluation of proxy responses, namely the patient–proxy relationship, which may affect the reliability of the proxy. In our view, the systematic comparison of evaluations of a small number of situations regarding overt and covert patient behaviours could allow the clinician to evaluate the reliability of the proxy. This vision is in line with the European Medicines Agency (EMA) which underlines that proxy reports should “include only events or behaviours that can be observed” [143, pp. 11–12]. Moreover, only confidence ratings may help to address a possible response bias generated by “I don’t know” answers.
We believe that reflecting on the issue of the reliability of proxy informant and the construction of items for proxy rating is of paramount importance given the goal of obtaining accurate assessments of the patient [144]. This work might represent a starting point and a valuable source of knowledge for those researchers want to contribute further to the topic, and it has limitations. We used convenience sampling to recruit participants, which may limit the generalizability of the findings to other populations. Additionally, the study did not measure divergent or convergent validity, which may limit the accuracy of the results. It is also important to note that the study did not account for the potential influence of caregiver burden or other individual characteristics that were not assessed or controlled for.
More research is clearly necessary to improve the ProRe questionnaire and the online confidence ratings. Future directions should be devoted to (a) the possibility of jointly use the answer “I don’t know” and the online confidence rating for the purpose of identifying the reliability of the proxy answers in a two-step model, and (b) the appropriateness and relevance to clinical practice of the present research [145]. External validity is another critical focus when applying study results to specific practices and population contexts [146], in order to make study outcomes directly relevant and informative to clinical practice. The next step could be the creation of a structured clinical interview including probing questions designed to reveal if responses are based on observed data, stereotypes, prejudices, or beliefs, allowing the clinician to promptly decide whether the answers provided are reliable or if, instead, they should obtain a second opinion from another relative or to start a more expensive session of direct observation by a trained caregiver in order to ensure they can compile a rigorous and reliable sketch of the patient's clinical condition.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to policy of the funder but are available from the corresponding author on reasonable request.
References
Neveanu PP (1978) DicĠionar de psihologie, Bucureúti, Albatros, 123. DicĠionar de psihologie, Bucureúti, Humanitas, 155
Popescu G (2014) Human behavior, from psychology to a transdisciplinary insight. Procedia Soc 128:442–446
Goldstein G, Hersen M (2000) Handbook of psychological assessment. Elsevier
Seng E, Kerns RD, Heapy A (2014) Psychological and behavioral assessment. Practical management of pain. Mosby, USA, pp 243–256
Li M, Harris I, Lu ZK (2015) Differences in proxy-reported and patient-reported outcomes: assessing health and functional status among medicare beneficiaries. BMC Med Res Methodol 15:1–10
Sudan D, Horslen S, Botha J et al (2004) Quality of life after pediatric intestinal transplantation: the perception of pediatric recipients and their parents. Am J Transplant 4:407–413
Elad D, Barak S, Eisenstein E et al (2013) Discrepancies between mothers and clinicians in assessing functional capabilities and performance of children with cerebral palsy. Res Dev Disabil 34:3746–3753
Porzsolt F, Kojer M, Schmidl M et al (2006) New instrument to describe indicators of well-being in old old patients with severe dementia: vienna list. Optimizing health: improving the value of healthcare delivery. Springer, Boston, MA, pp 56–65
Kuipers P, Kendall M, Fleming J et al (2004) Comparison of the sydney psychosocial reintegration scale (SPRS) with the community integration questionnaire (CIQ): psychometric properties. Brain Inj 18:161–177
Becchi A, Rucci P, Placentino A et al (2004) Quality of life in patients with schizophrenia—comparison of self-report and proxy assessments. Soc Psychiatry Psychiatr Epidemiol 39:397–401
Giovannetti ER, Reider L, Wolff JL et al (2013) Do older patients and their family caregivers agree about the quality of chronic illness care? IJQHC 25:515–524
Gnanadesigan N, Salib D, Roth CP et al (2004) The quality of care provided to vulnerable older community-based patients with urinary incontinence. JAMDA 5:141–146
Lynn Snow A, Cook KF, Lin PS et al (2005) Proxies and other external raters: methodological considerations. Health Serv Res 40:1676–1693
Schwartz CE, Ayandeh A, Rodgers JD et al (2015) A new perspective on proxy report: Investigating implicit processes of understanding through patient–proxy congruence. Qual Life Res 24:2637–2649
Rydén L, Sigström R, Nilsson J et al (2019) Agreement between self-reports, proxy-reports and the National Patient Register regarding diagnoses of cardiovascular disorders and diabetes mellitus in a population-based sample of 80-year-olds. Age Ageing 48:513–518
McDowell I (2006) Measuring health: a guide to rating scales and questionnaires. Oxford University Press, USA
Jorm AF, Mackinnon AJ, Henderson AS et al (1995) The psychogeriatric assessment scales: a multidimensional alternative to categorical diagnoses of dementia and depression in the elderly. Psychol Med 25:447–460
Gruber-Baldini AL, Shardell M, Lloyd KD et al (2012) Use of proxies and informants. The epidemiology of aging. Springer, Dordrecht, pp 81–90
Cobb C (2018) Answering for someone else: proxy reports in survey research. The Palgrave Handbook of Survey Research. Palgrave Macmillan, Cham, pp 87–93
Neumann PJ, Araki SS, Gutterman EM (2000) The use of proxy respondents in studies of older adults: lessons, challenges, and opportunities. JAGS 48:1646–1654
Jorm AF (2004) The informant questionnaire on cognitive decline in the elderly (IQCODE): a review. Int Psychogeriatr 16:275–293
Arts J, Gubbels JS, Verhoeff AP et al (2022) A systematic review of proxy-report questionnaires assessing physical activity, sedentary behavior and/or sleep in young children (aged 0–5 years). IJBNPA 19:1–39
Schützwohl M, Voß E, Salize HJ et al (2018) Self-and proxy-rated needs in adults with mild to moderate intellectual disabilities: perspective matters. JARID 31:285–295
Alvarez-Nebreda ML, Heng M, Rosner B et al (2019) Reliability of proxy-reported patient-reported outcomes measurement information system physical function and pain interference responses for elderly patients with musculoskeletal injury. JAAOS 27:e156–e165
Ersek M, Polissar N, Neradilek MB (2011) Development of a composite pain measure for persons with advanced dementia: Exploratory analyses in self-reporting nursing home residents. J Pain Symptom Manag 41:566–579
Bradford A, Brenes GA, Robinson RA et al (2013) Concordance of self-and proxy-rated worry and anxiety symptoms in older adults with dementia. J Anxiety Disord 27:125–130
Krug R, Karus D, Selwyn PA et al (2010) Late-stage HIV/AIDS patients’ and their familial caregivers’ agreement on the palliative care outcome scale. J Pain Symptom Manag 39:23–32
Kua ZJ, Pachana NA, Byrne GJ et al (2018) How well do caregivers detect depression and anxiety in patients with Parkinson disease? J Geriatr Psych Neur 31:227–236
Skinner BF (1953) Science and human behavior. The Free Press, New York
Baer DM, Wolf MM, Risley TR (1968) Some current dimensions of applied behavior analysis. JABA 1:91
Baum WM (2011) Behaviorism, private events, and the molar view of behavior. Behav Anal 34:185–200
Ortu D (2012) Neuroscientific measures of covert behavior. Behav Anal 35:75–87
Moore M (1995) Creating public value: strategic management in the public sector. Harvard University, Boston
Tang YY, Tang R (2020) The neuroscience of meditation: understanding individual differences. Academic Press, Cambridge
Bauer DJ, Howard AL, Baldasaro RE et al (2013) A trifactor model for integrating ratings across multiple informants. Psychol Methods 18:475
Nelson LM, Longstreth WT Jr, Checkoutay H et al (1994) Completeness and accuracy of interview data from proxy respondents: demographic, medical, and life-style factors. Epidemiology 5:204–217
Oczkowski C, O’Donnell M (2010) Reliability of proxy respondents for patients with stroke: a systematic review. J Stroke Cerebrovasc Dis 19:410–416
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington, DC
Sandgren AK, Mullens AB, Erickson C et al (2004) Confidant and breast cancer patient reports of quality of life. Qual Life Res 13:155–160
Shaw C, McColl E, Bond S (2000) Functional abilities and continence: the use of proxy respondents in research involving older people. Qual Life Res 9:1117–1126
The Medical Research Council Cognitive Function and Ageing Study (2000) Survey into health problems of elderly people: a comparison of self-report with proxy information. Int J Epidemiol 29:684–697
Tang ST (2006) Predictors of the extent of agreement for quality of life assessments between terminally ill cancer patients and their primary family caregivers in Taiwan. Qual Life Res 15:391–404
Marosszeky N, Sansoni E (2008) The use of proxy/informant reports for people with dementia, National Health Outcomes Conference. Australian Health Outcomes Collaboration, Wollongong, Australia, 13.
Cummins RA (2002) Proxy responding for subjective well-being: a review. Int Rew Rea Ment Retard 25:183–207
Novella JL, Boyer F, Jochum C et al (2006) Health status in patients with Alzheimer’s disease: an investigation of inter-rater agreement. Qual Life Res 15:811–819
Duncan FA, Caughy OM (2009) Parenting style and the vulnerable child syndrome. J Child Adolesc 22:228–234
Ozhek SR (2008) Overprotection and adolescents with physical disabilities. Speech Educ Rehabilit 9:100–106
Thomasgard M, Shonkoff JP, Metz WP et al (1995) Parent–child relationship disorders. Part II: The vulnerable child syndrome and its relation to parental overprotection. JDBP 16:251–256
Magaziner J, Simonsick EM, Kashner TM et al (1988) Patient-proxy response comparability on measures of patient health and functional status. J Clin Epidemiol 41:1065–1074
Sneeuw KC, Aaronson NK, Sprangers MA et al (1997) Value of caregiver ratings in evaluating the quality of life of patients with cancer. J Clin Oncol 15:1206–1217
Todorov A, Kirchner C (2000) Bias in proxies’ reports of disability: data from the national health interview survey on disability. Am J Public Health 90:1248
Tang ST, McCorkle R (2002) Use of family proxies in quality of life research for cancer patients at the end of life: a literature review. Cancer Invest 20:1086–1104
Pickard SA, Johnson JA, Feeny DH et al (2004) Agreement between patient and proxy assessments of health-related quality of life after stroke using the EQ-5D and Health Utilities Index. Stroke 35:607–612
Elliott MN, Beckett MK, Chong K et al (2008) How do proxy responses and proxy-assisted responses differ from what Medicare beneficiaries might have reported about their health care? Health Ser Res 43:833–848
Roydhouse JK, Wilson IB (2017) Systematic review of caregiver responses for patient health-related quality of life in adult cancer care. Qual Life Res 26:1925–1954
Snow AL, Kunik ME, Molinari VA et al (2005) Accuracy of self-reported depression in persons with dementia. JAGS 53:389–396
von Essen L (2004) Proxy ratings of patient quality of life–factors related to patient-proxy agreement. Acta Oncol 43:229–234
Roydhouse JK, Cohen ML, Eshoj HR, Corsini N, Yucel E, Rutherford C, ISOQOL Proxy Task Force and the ISOQOL Board of Directors (2021) The use of proxies and proxy-reported measures: a report of the international society for quality of life research (ISOQOL) proxy task force. Qual Life Res 1–11.
Zinkevich A, Lubasch JS, Uthoff SAK et al (2021) Caregiver burden and proxy-reported outcomes of people without natural speech: a cross-sectional survey study. BMJ Open 11:e048789
Long K, Sudha S, Mutran EJ (1998) Elder-proxy agreement concerning the functional status and medical history of the older person: the impact of caregiver burden and depressive symptomatology. JAGS 46:1103–1111
Magaziner J (1992) The use of proxy respondents in health studies of the aged. In: Wallace RB, Woolson RF (eds) The epidemiologic study of the elderly. Oxford University Press, New York, pp 120–129
Magaziner J, Bassett SS, Hebel JR et al (1996) Use of proxies to measure health and functional status in epidemiologic studies of community-dwelling women aged 65 years and older. AJE 143:283–292
Nekolaichuk CL, Bruera E, Spachynski K et al (1999) A comparison of patient and proxy symptom assessments in advanced cancer patients. Palliat Med 13:311–323
Graham C (2016) Incidence and impact of proxy response in measuring patient experience: secondary analysis of a large postal survey using propensity score matching. IJQHC 28:246–252
Sneeuw KC, Aaronson NK, Sprangers MA et al (1998) Comparison of patient and proxy EORTC QLQ-C30 ratings in assessing the quality of life of cancer patients. J Clin Epidemiol 51:617–631
Sneeuw KCA, Aaronson NK, Spranger MAG et al (1999) Evaluating the quality of life of cancer patients: assessments by patients, significant others, physicians and nurses. BJC 81:87–94
Wennman-Larsen A, Tishelman C, Wengstrom Y et al (2007) Factors influencing agreement in symptom ratings by lung cancer patients and their significant others. J Pain Symptom Manag 33:146–155
Sneeuw KC, Aaronson NK, Osoba D et al (1997) The use of significant others as proxy raters of the quality of life of patients with brain cancer. Med Care 35:490–506
Tang ST (2006) Concordance of quality-of-life assessments between terminally ill cancer patients and their primary family caregivers in Taiwan. Cancer Nurs 29:49–57
Pickard AS, Lin HW, Knight SJ et al (2009) Proxy assessment of health-related quality of life in African American and white respondents with prostate cancer: perspective matters. Med Care 47:176
Rabin EG, Heldt E, Hirakata VN et al (2009) Depression and perceptions of quality of life of breast cancer survivors and their male partners. Oncol Nursing Forum 36:E153–E158
Daltroy LH, Larson MG, Eaton HM et al (1999) Discrepancies between self-reported and observed physical function in the elderly: the influence of response shift and other factors. Soc Sci Med 48:1549–1561
Markus H, Zajonc RB (1985) The cognitive perspective in social psychology. In: Lindzey G, Aronson E (eds) The handbook of social psychology, 3rd edn. Random House, New York, pp 137–230
Osterlind SJ (1989) Definition, purpose, and characteristics of items. Constructing test items. Springer, Dordrecht, pp 17–61
Rothman ML, Hedrick SC, Bulcroft KA et al (1991) The validity of proxy-generated scores as measures of patient health status. Med Care 29:115–124
Sneeuw KCA, Aaronson NK, Haan RJ et al (1997) Assessing quality of life after stroke: the value and limitations of proxy ratings. Stroke 28:1541–1549
Blair J, Menon G, Bickart B (1991) Measurement effects in self vs. proxy responses to survey questions: An information processing perspective. In: Groves R (ed) Measurement errgrs in surveys. John Wiley and Sons, New York, pp 145–166
Bickart BA, Blair J, Menon G et al (1990) Cognitive aspects of proxy reporting of behvior. Adv Consum Res 17:198–206
Krosnick JA, Presser S, Fealing KH, et al. (2015) The future of survey research: Challenges and opportunities. The National Science Foundation Advisory Committee for the Social, Behavioral and Economic Sciences Subcommittee on Advancing SBE Survey Research, pp 1–15.
Mathiowetz NA, Groves RM (1985) The effects of respondent rules on health survey reports. Am J Public Health 75:639–644
Burns KM, Burns NR, Ward L (2016) Confidence—more a personality or ability trait? It depends on how it is measured: a comparison of young and older adults. Front Psychol 7:518
Stankov L, Morony S, Lee YP (2013) Confidence: the best non-cognitive predictor of academic achievement? Educ Psychol 34:9–28
Jonsson AC, Allwood CM (2003) Stability and variability in the realism of confidence judgments over time, content domain, and gender. Pers Individ Differ 34:559–574
Händel M, de Bruin AB, Dresel M (2020) Individual differences in local and global metacognitive judgments. Metacogn Learn 15:51–75
de Bruin ABH, Kok EM, Lobbestael J et al (2017) The impact of an online tool for monitoring and regulating learning at university: overconfidence, learning strategy, and personality. Metacogn Learn 12:21–43
Williams LS, Bakas T, Brizendine E et al (2006) How valid are family proxy assessments of stroke patients’ health-related quality of life? Stroke 37:2081–2085
Elliott PC, Smith G, Ernest CS et al (2009) Everyday cognitive functioning in cardiac patients: relationships between self-report, report of a significant other and cognitive test performance. Aging Neuropsychol Cogn 17:71–88
Ahasic AM, Van Ness PE, Murphy TE et al (2015) Functional status after critical illness: agreement between patient and proxy assessments. Age Ageing 44:506–510
Medical Research Council Cognitive Function and Ageing Studyb (2000) Survey into health problems of elderly people: a comparison of self-report with proxy information. Int J Epidemiol 26:684–686
Bosco A (2003) Come si costruisce un questionario. Carocci ed.
Clark LA, Watson D (2019) Constructing validity: new developments in creating objective measuring instruments. Psychol Assess 31:1412
Gallo JJ, Paveza GJ (2006) Activities of daily living and instrumental activities of daily living assessment. In: Gallo JJ, Bogner HR, Fulmer T, Paveza GJ (eds) Handbook of geriatric assessment, 4th edn. Jones and Bartlett Publishers, MA, pp 193–240
Lopez A, Caffò AO, Tinella L et al (2023) The four factors of mind wandering questionnaire: content, construct, and clinical validity. Assessment. https://doi.org/10.1177/10731911211058688
Fleiss JL, Levin B, Paik MC (1981) The measurement of interrater agreement. Stat Methods Rates Proportions 2:22–23
Fenollar P, Román S, Cuestas PJ (2007) University students’ academic performance: an integrative conceptual framework and empirical analysis. Br J Educ 77:873–891
Mangels JA, Butterfield B, Lamb J et al (2006) Why do beliefs about intelligence influence learning success? A social cognitive neuroscience model. Soc Cogn Affect 1:75–86
Richardson K, Norgate SH (2015) Does IQ really predict job performance? Appl Dev Sci 19:153–169
Lopez A, Caffò AO, Bosco A (2020) Memory for familiar locations: The impact of age, education and cognitive efficiency on two neuropsychological allocentric tasks. Assessment 27:1588–1603
Nilsson LG, Sternang O, Ronnlund M et al (2009) Challenging the notion of an early-onset of cognitive decline. Neurobiol Aging 30:521–524
Hair JF, Black WC, Babin BJ et al (2010) Multivariate data analysis: Global perspective, 7th edn. Pearson Education, London
Revelle WR (2017) psych: Procedures for personality and psychological research. R package version 1.4.8. Northwestern University, Evanston, Illinois, 2014. URL http://CRAN.R-project.org/package=psych. Accessed 20 Apr 2021
Korkmaz S, Göksülük D, Gokmen Z (2014) MVN: An R package for assessing multivariate normality. R J. https://doi.org/10.32614/RJ-2014-031
Rosseel Y (2011) Lavaan: Latent Variable Analysis. R package version 0.3–3.
Arifin WC (2017) Exploratory factor analysis and Cronbach’s alpha Questionnaire Validation Workshop. USM Health 12 Assessment 00(0) Campus, University Sains Malaysia. wnarifin.github.io, wnarifin@usm.my .
Kaiser HF, Rice J (1974) Little jiffy, mark IV. Educ Psychol Meas 34:111–117
KlineP A (1999) Handbook of psychological testing, 2nd edn. Routledge, Milton Park
Brown TA (2015) Confirmatory factor analysis for applied research. Guilford Press
Fabrigar LR, Wegener DT (2011) Exploratory factor analysis. Oxford University Press
Bergkvist L, Rossiter JR (2007) The predictive validity of multiple-item versus single-item measures of the same constructs. J Mark Res 44:175–184
Drolet AL, Morrison DG (2001) Do we really need multiple-item measures in service research? J Serv Res 3:196–204
Hardesty DM, Bearden WO (2004) The use of expert judges in scale development: Implications for improving face validity of measures of unobservable constructs. J Bus Res 57:98–107
Wanous JP, Reichers AE, Hudy MJ (1997) Overall job satisfaction: how good are single-item measures? J Appl Psychol 82:247–252
Devellis R (2012) Scale development theory and applications. SAGE, Thousand Oaks
Schreiber JB, Nora A, Stage FK et al (2006) Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res 99:323–338
McNeish D, Wolf MG (2021) Dynamic fit index cutoffs for confirmatory factor analysis models. Psychol Methods 28:61–88
Hu LT, Bentler MP (1998) Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods 3:424–453
Ullman JB (2001) Structural equation modeling. In: Tabachnick BG, Fidell LS (eds) Using multivariate statistics, 4th edn. Allyn & Bacon, Boston, pp 653–771
Faul F, Erdfelder E, Buchner A et al (2009) Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Brodaty H, Pond D, Kemp NM et al (2002) The GPCOG: a new screening test for dementia designed for general practice. JAGS 50:530–534
Pirani A, Brodaty H, Martini E et al (2010) The validation of the Italian version of the GPCOG (GPCOG-It): a contribution to cross-national implementation of a screening test for dementia in general practice. Int Psychogeriatr 22:82–90
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. JAGS. https://doi.org/10.1111/j.1532-5415.1983.tb03391.x
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Fenollar P, Román S, Cuestas PJ (2007) University students’ academic performance: an integrative conceptual framework and empirical analysis. Br J Educ Psychol 77:873–891
Lopez A, Caffò AO, Spano G et al (2019) The effect of aging on memory for recent and remote egocentric and allocentric information. Exp Aging Res 45:57–73
Ortman JM, Bates N, Brown A, Sawyer RC (2017) Optimizing self and proxy response to survey questions on sexual orientation and gender identity. In: Presentation at the Annual Meeting of the Population Association of America, Chicago, IL.
Schuman H, Presser S (1981) Questions and answers in attitude surveys (New 1996 copyright by Sage Publications, Thousand Oaks, CA. ed.).
Chopik WJ, Giasson HL (2017) Age differences in explicit and implicit age attitudes across the life span. Gerontologist 57:S169–S177
Geboers B, Uiters E, Reijneveld SA et al (2018) Health literacy among older adults is associated with their 10-years’ cognitive functioning and decline-the Doetinchem Cohort Study. BMC Geriatr 18:1–7
Blair A, Kross B, Stewart PA et al (1995) Comparability of information on pesticide use obtained from farmers and their proxy respondents. J Agric Saf Health 1:165–176
Gilpin EA, Pierce JP, Cavin SW et al (1994) Estimates of population smoking prevalence: self-vs proxy reports of smoking status. Am J Public Health 84:1576–1579
Kojetin B, Jerstad S (1997) The quality of proxy reports on the Consumer Expenditure Survey. In Society for Consumer Psychology Conference, St. Petersburg, Florida.
Joloza T, Evans J, O’Brien R, Potter-Collins A (2010) Measuring sexual identity: an evaluation report. Office of National Statistics, UK
Hendershot GE (2004) The effects of survey nonresponse and proxy response on measures of employment for persons with disabilities. DSQ. https://doi.org/10.18061/dsq.v24i2.481
Kerwin PBDHCJP (1998) “Don’t know” responses in surveys: is what I know what you want to know and do I want you to know it? Memory 6:407–426
Pereira M, Faivre N, IturrateI WM et al (2020) Disentangling the origins of confidence in speeded perceptual judgments through multimodal imaging. PNAS 117:8382–8390
Siedlecka M, Skóra Z, Paulewicz B et al (2019) Responses improve the accuracy of confidence judgements in memory tasks. JEP 45:712–723
Wokke ME, Achoui D, Cleeremans A (2019) Action information contributes to metacognitive decision-making. Sci Rep 10:3632
Siedlecka M, Koculak M, Paulewicz B (2021) Confidence in action: differences between perceived accuracy of decision and motor response. PBR 28:1698–1706
Freedman JL, Fraser SC (1966) Compliance without pressure: the foot-in-the-door technique. J Pers Soc Psychol 4:195
Fairclough DL (2005) Practical considerations in outcomes assessment for clinical trials. Outcomes assessment in cancer: measures, methods, and applications. Cambridge University Press, Cambridge, UK, pp 346–361
Simes RJ, Greatorex V, Gebski VJ (1998) Practical approaches to minimize problems with missing quality of life data. Stat Med 17:725–737
European Medicines Agency (2016) Appendix 2 to the guideline on the evaluation of anticancer medicinal products in man: The use of patient-reported outcome (PRO) measures in oncology studies. London, UK: European Medicines Agency.
Sommers-Flanagan J, Zeleke WA, Hood ME (2015) The clinical interview. In: Cautin R, Lilienfeld S (eds) The encyclopedia of clinical psychology. John Wiley & Sons, Inc, Hoboken, pp 1–9
Methodology Committee of the Patient-Centered Outcomes Research Institute (2012) Methodological standards and patient-centeredness in comparative effectiveness research: the PCORI perspective. JAMA 307:1636–1640
Burchett H, Umoquit M, Dobrow M (2011) How do we know when research from one setting can be useful in another? A review of external validity, applicability and transferability frameworks. J Heal Serv Res Policy 16:238–244
Acknowledgements
Thanks to study participants and students in the Department of Educational Sciences, Psychology and Communication of the University of Bari.
Funding
Open access funding provided by Università degli Studi di Bari Aldo Moro within the CRUI-CARE Agreement. The first author is supported by the project “A-WAND! Strengthening the skills of self-monitoring and preventing the risk of accidents in and outdoors in a population of elderly people in the south of Italy”. Action Founded by Research for Innovation (REFIN)-POR Puglia FESR FSE 2014–2020–Asse X–Azione 10.4. (Grant Code 8C40CDAA), and by the project AMA–Apulia Mindful Aging. Action Founded by AReSS Puglia.
Author information
Authors and Affiliations
Contributions
Conceptualization, AL and AB; methodology, AL and AB; software, AL; validation, AL, AB; formal analysis, AL; investigation, AL, AB, AOC and LT; resources AB and AL; data curation, AL; writing—original draft preparation, AL; writing—review and editing, AL, AB, AOC, LT; visualization, AL; supervision, AB; project administration, AB and AL; funding acquisition, AB and AL
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The study was compliant with the declaration of Helsinki. This study was approved by the Institutional Review Board of Department of Educational Sciences, Psychology, Communication, University of Bari n. ET-21-01.
Informed consent
Informed consent and participant responses to the questionnaires were obtained simultaneously from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lopez, A., Tinella, L., Caffò, A. et al. Measuring the reliability of proxy respondents in behavioural assessments: an open question. Aging Clin Exp Res 35, 2173–2190 (2023). https://doi.org/10.1007/s40520-023-02501-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02501-z