Abstract
Background
Falls are a substantial health problem among older adults. An accessible and reliable tool for assessing individual fall risk is needed.
Aims
The predictive ability of a one-page self-rated fall risk assessment form (KaatumisSeula® [KS]) was evaluated among older women in its current form.
Methods
A subsample (n = 384) of community-living older women (aged 72–84 years) participating in the Kuopio Fall Prevention Study (KFPS) completed the KS form. Participants’ falls were prospectively registered for 12 months with SMS messages. Their group status and form-based fall risk category were compared to the verified fall events during the KFPS intervention. Negative binomial regression and multinomial regression analyses were used. Physical performance measurements (single leg stance, leg extension strength and grip strength) were used as covariates.
Results
During the follow-up, 43.8% of women fell at least once. Among the fallers, 76.8% had at least one self-determined injurious fall, and 26.2% had falls requiring medical attention. According to KS, 7.6% of the women had low fall risk, 75.0% moderate, 15.4% substantial, and only 2.1% high fall risk. Women in the “moderate fall risk” group had 1.47-fold (95% CI 0.74–2.91; nonsignificant), in “substantial fall risk” 4.00-fold (1.93–8.3; p < 0.001) and in “high fall risk” 3.00-fold (0.97–9.22; nonsignificant) higher risk of falls compared to the “low fall risk” group. Performance in physical tests did not account for future falls.
Conclusions
The KS form proved to be a feasible tool for self-administered fall risk assessment with moderate predictive ability.
Trial registration
ClinicalTrials.gov identifier: NCT02665169, date of first registration 27/01/2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Falls are a significant health issue causing fear of falls, fractures, and hospitalization. They are the second leading cause of unintentional injury deaths worldwide, especially among older adults [1]. In Finland, falls are the third most common cause of disability-adjusted life years [2]. In 2019, fall-related injuries caused over half of all accidental deaths in Finland. Around 90% of these persons were over 65 years old [3]. The number of fall-induced deaths has more than doubled in Finland during the past 40 years, mostly due to ageing of the population [4]. The proportion of older people is increasing rapidly, and it is predicted that in the near future the number of fall-induced deaths may increase 1.6-fold and 1.5-fold higher in Finnish men and women, respectively [5]. A recent global recommendation suggests that even among “healthier” older adults the fall risk should be reassessed annually [6]. Thus, a reliable tool for practical assessment of older persons’ fall risk is needed.
Numerous fall risk assessment tools, such as questionnaires and computer-based algorithms, are available. Some of these tools are designed to be used for hospitalized persons [7,8,9,10,11,12,13,14], whereas others [15,16,17,18] are intended for community-dwellers. However, most of these tools are not routinely used among community-living older people. Some tools are composed of more than 20 items [16, 19, 20], and although comprehensive, they are not quick to use. Moreover, many tools require data from clinical measurements of weight [21], grip strength [21, 22], walking [21, 22] and/or balance [21,22,23,24,25]. Furthermore, scoring from symptom scales such as MMSE or CES-D is often required [22, 26]. Some rapid tools for fall risk assessment and screening, such as FROP-Com [18], are available, but they rely on evaluation performed by health care professionals. Only a few tools consist of a simple self-rating for older adults [17, 27, 28].
In the present study, we assessed the predictive ability of a one-page self-rated fall risk assessment tool (KaatumisSeula® [KS]) among older women included in the Kuopio Fall Prevention Study (KFPS) during a 12-month follow-up. Results of physical performance measurements (single leg stance, leg extension strength, and grip strength) were used as covariates. The assessment was made according to existing KS risk categories with no intention to readjust the cut-off points or methodological aspects of the KS itself.
Methods
KaatumisSeula®
The UKK Institute for Health Promotion Research (Tampere, Finland) recently released the KaatumisSeula® (KS, meaning “falls screen” in English) self-evaluation tool for assessing the fall risk of older people and implementing preventive measures in the community [29, 30]. The one-page assessment form [31] is designed to be filled in either by the older persons themselves or together with (health care) professionals and used as a simple first line risk assessment for falls among general population even when older people together discuss the fall risk and how it could be managed. Moreover, the KS can also be used as an early-stage assessment in other situations where one’s fall risk is a concern. The KS also includes written material of falls prevention for the older adults.
The items of the KS tool are based on the relevant scientific literature on established factors affecting the fall risk in older adults and expert opinions working in the field of fall prevention. The form consists of six multiple-choice questions concerning age, fall history, balance and movement confidence, independence of daily living, chronic health conditions, and physical activity. Each question adds 0 to 2 or 4 points, and the total score ranges from 0 to 14 points. Based on the score, respondents are classified into four categories: (1) “Your fall risk is not elevated” (0 points), (2) “Your fall risk is elevated” (1–5 points), (3) “Your fall risk is clearly elevated. A professional assessment is recommended” (6–8 points), and (4) “Your fall risk is great. A professional assessment is required” (9–14 points) (Online Appendix 1). In this article, the categories were renamed as follows: (1) low fall risk (0 points); (2) moderate fall risk (1–5 points); (3) substantial fall risk (6–8 points); and (4) high fall risk (9–14 points). The form has also been released as an electronic version in Finnish [32]. Test–retest reliability of the KS has been tested among older people (n = 13) who participated in 1 week course of the Finnish Pensioners’ Federation. Test–retest reliability was very good for total score (kappa = 0.906) and good for fall risk classification (kappa = 0.755) [33].
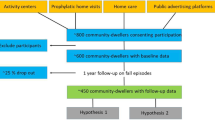
KFPS study and participants
The Kuopio Fall Prevention Study (KFPS) was a 2-year exercise randomized controlled trial (RCT) conducted in 2016–2019. It evaluated the effects of physical exercise, including gym training and Tai Chi, on the prevention of falls and promotion of well-being in older women [34]. The study cohort consisted of 914 women aged 72–84 years and living in the city of Kuopio in Finland. Participants were randomized to intervention (n = 457) and control groups (n = 457). The present KS assessment study consisted of subsample of 384 KFPS women.
During the study, the participants received biweekly Short Message Service (SMS) questions concerning falls (during the past 2 weeks) with a simple “yes/no” option to answer. Positive replies (yes) were verified for details by means of a phone interview. In addition, participants filled a self-administered diary with falls and leisure-time physical activity at 3-month intervals. National health care registers were cross-checked for fractures. Both study groups had physical performance measurements three times: at baseline and at the 12-month and 24-month follow-ups. The protocol of the KFPS study is available for further details [34].
Assessment of the KS fall risk assessment tool
The KS form was introduced to a subsample of 403 women during the 12-month study visit, which was set as the baseline of this study. Falls were followed up for the second year of the KFPS. Altogether, a subsample of 384 women from the KFPS (220 from the intervention group and 164 from the control group) both with successfully filled the KS forms and sufficient follow-up time after the 12-month study visit (mean follow-up 369 days, range 308–390 days) were included in the analysis. The participants did not get the results (i.e., estimated fall risk category) of their KS forms during the study. The clinical characteristics of the study participants are shown in Online Appendix 2.
Participants’ group status and fall risk category based on the KS were compared to all falls and injurious falls. Moreover, physical performance measurements (i.e., single-leg stance, maximal leg extension strength and maximal grip strength) [34] were made during the 12-month visit of the KFPS. The proportions of fallers were calculated for each KS score as follows: the number of women who had fallen during the follow-up was divided by the total number of women (both fallers and non-fallers) within each KS score. The original KS risk categories were used without readjusting the cut-off points. However, raw data features of falls per KS score is available for those interested (Online Appendix 3).
Statistical analysis
Negative binomial regression was used to examine how the KS fall risk category predicted falls during the 12-month follow-up period. Group status, follow-up time, single-leg stance time, leg extension strength and grip strength were used as covariates. The three physical performance measures served as independent predictors of the statistical model. The 95% confidence intervals of the regression coefficients are presented. Poisson log-linear regression was used to examine how well the KS risk points predicted the probability of future falls. Multinomial logistic regression was used in the sub-analysis to examine whether the intervention group status or fall risk category affected the incidence of falls leading to an injury. P values less than 0.05 were considered statistically significant. Statistical analyses were performed with SPSS version 27.
Results
The fall risk categories of the KFPS participants and falls during the follow-up
Among the 384 women, the KS indicated “low” fall risk for 29 (7.6%) women, “moderate” for 288 (75.0%), “substantial” for 59 (15.4%), and “high” only for 8 (2.1%). The highest KS score was 10 points in five women: none had the highest scores from 11 to 14 points (Fig. 1).
During the 12-month follow-up, 168 women out of 384 (43.8%) fell at least once, and the total number of falls was 309. Most fallers had only a few registered falls (on average 0.8 fall for each participant), but two women (0.5%) had up to 13 falls (Table 1). Of the women who had fallen, 126 (75%) had at least one self-determined fall injury and 44 cases (26.2% of fallers) required medical attention (Table 1).
Predictive value of the KS
Negative binomial regression showed that the group status (intervention/control) of the KFPS was not significantly associated with the KS predictions when analyzing all falls (Table 2). Altogether, a higher KS score predicted a higher incidence of falls. Initially, we studied how the continuous KS score would explain number of falls in log-linear Poisson regression adjusted with intervention indicator and found out that each one-point increment in KS score would yield exp(B) to be 1.25 (95% CI 1.17–1.34, p < 0.001). As a categorical predictor, women in the “moderate fall risk” group had a 1.47-fold (95% CI 0.74–2.91, p = 0.27) higher risk for falls during the next 12 months compared to women with “low fall risk”. Correspondingly, women in the “substantial fall risk” category had a 4.00-fold (95% CI 1.93–8.30, p < 0.001), and in the “high fall risk” group a 3.00-fold (95% CI 0.97–9.22, p = 0.056) higher risk for falls during the next 12 months compared to the “low fall risk” group. Overall, using analysis of deviance test (Chi-squared = 27.2773, df = 1, p < 0.001) the KS classification variable was found to be a crucial predictor in the model which also had the intervention variable as a predictor. The inclusion of single-leg stance time, leg extension and grip strength as covariates did not change the results of the negative binomial regression. None of the three physical performance variables were significantly associated with overall fall incidence and thus they were omitted from the final model (Table 2). Three women had a substantially higher number of falls (eight or more) in comparison to the others. Analyses were also made without these outliers, which did not affect the results and therefore they were included in the final model.
In the sub-analysis concerning the injuries, belonging to the higher fall risk group increased the risk of a fall-related injury. Women with “substantial fall risk” and “high fall risk” had 5.93-fold (95% CI 2.03–17.3, p = 0.001) and 8.71-fold (95% CI 1.34–56.8, p = 0.024) higher risks for injurious falls than women in the “low fall risk”, respectively. Neither the intervention group status nor physical performance was significant in this sub-analysis (Table 3).
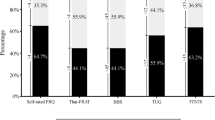
The proportion of fallers increased with a higher KS score (Fig. 2). However, this association was non-linear, as the highest proportion was seen with a score of six, which is a middle-range score in the form. According to the fall history, the women with a score of six (n = 26) had also reported more falls prior to the KS fall assessment compared to all other scores (Chi-square test, p < 0.001) which appears to be in line with the highest incidence of falls during the follow-up. The definition of the cut-off scores for the KS fall risk groups among the KFPS population would not be apparent, as the increase in the proportion of both fallers and falls was non-linear in the highest scores above six (Online Appendix 3).
Discussion
This prospective 12-month study among community-living older women examined not only the ability of a Finnish self-rated fall risk assessment tool KaatumisSeula® (KS) to predict falls but also the utility of additional physical performance measurements in parallel with the KS score. The KS was shown to be a feasible tool for fall risk prediction, whereas the physical performance measurements provided no added value.
Although the risk was elevated with more than 90% of the participants, around half of them did not fall during the follow-up. As age is a major risk factor for falls, all 75-year-old persons are assigned at least one point in the KS. Therefore, most of the participants were categorized in the “moderate fall risk” group (1–5 points). As previous falls are a risk factor for future falls, a person with one fall in the past 12 months receives two points, and a person with ≥ 2 falls four points in the KS. Of those women who fell, three out of four hurt themselves to some degree, and approximately every fourth faller required medical attention. In the sub-analysis, the KS was able to predict injurious falls in the “substantial” (almost six times higher risk for injurious fall) and “high” fall risk (almost ninefold higher risk) groups compared to the “low fall risk” group.
In terms of overall fall risk, the KS was able to predict falls in the “substantial fall risk” (fourfold higher risk for falls) and in the “high fall risk” (threefold higher risk, non-significant) groups compared to the “low fall risk” group. However, based on the proportions of fallers, the women with lower scores appeared to have a relatively higher risk for future falls than those with the highest scores. One explanation could be that older women with more risk factors for falls may self-adjust their daily actions in risk-reducing manners. The small number of women (n = 8) in the “high fall risk” group also makes the analyses in this category uncertain. Nevertheless, six points in the KS is the cut-off recommending “professional assessment”, which appears to be in line with the results. The KS could not significantly predict fall risk in the “moderate fall risk” group. However, it is worth noting that even with the lowest KS scores of 0–2, almost 30% of the women fell during the follow-up, with a KS score of 3 over 40% of the women fell, and with 5 points more than half of the women fell. According to Poisson regression, fall risk increased almost 23% per each increased KS point.
Adjustment with physical performance did not affect the results. This was expected, because questions on balance, safety in movement and physical activity are already included in the KS, and good performance in these areas correlates with sufficient physical capability (e.g., good lower limb strength). On the other hand, physically inactive older people may be less likely to fall because of spending less time on their feet. Previous results of the KFPS showed that more active older women may have an increased risk for falls and fractures [35]. Other studies have also suggested that physically more active older people may have more fall events [36]. Physical activity may even increase the risk for upper limb fractures [37, 38]. However, multi-component exercise RCTs have indicated long-term reductions in injurious falls, falls requiring medical attention, and fractures among older Finnish women [39,40,41].
The other simple self-rated fall risk evaluation tool for older adults have had similar results as the KS. For example, a short postal screening tool to prevent falls injury (PreFIT) had only modest predictive ability of any falls (AUC 0.66), recurrent falls (AUC 0.70) as well as fractures (AUC 0.60) in a large UK study among community dwelling older adults [28]. Moreover, a 13-item self-fillable Fall Risk Questionnaire (FRQ) performed well (kappa = 0.875, p < 0.001) when comparing to clinical evaluation, although some items of the tool had only moderate correlation with the clinical exam in a small study [27]. Also, an Activities-specific balance confidence scale (ABC) could predict future falls well (p = 0.003 in linear regression) during a 6-month follow-up among a small cohort of community dwelling older adults. However, it could correctly classify the fall status only in around 78% of the participants [17]. Similar findings were also stated in a recent meta-analysis observing that a single tool is not able to detect older people’s falls with sufficient accuracy, whereas the use of two or more assessment tools in combination may enhance the predictability of falls [14]. Thus, in future studies, the outcomes of the self-administered KS could be verified further with clinically measured tests for falls screening, such as Timed Up & Go test and Berg Balance scale [14]. However, as discussed above, physical performance assessments alongside the KS would not necessarily improve fall prediction. Also, a more throughout evaluation of the KS would require having more participants with the highest fall risk.
The strength of this study is its relatively large sample size and the intensive follow-up protocol utilizing biweekly SMS questions and the verification of falls with phone interviews. Since several participants with notable fall history sustained multiple falls also during the follow-up, a simple “yes/no” interpretation was an easy and adequate way to report fall events.
The participants of the KFPS study are known to be physically and mentally healthier than the non-participating and non-invited women within the region [35]. This participation bias, along with the lack of men, limits the generalizability of the results at the population level. Furthermore, as the participants were community-living older women, the results cannot be extrapolated to people living in residential care or nursing homes. Also, during the KFPS intervention the participants were not in their habitual routine which may influence the results. Only 17.5% of the women had substantial or high fall risk according to the KS in the present study, and none of the participants had the highest scores from 11 to 14 points. This underrepresentation of the “most frail” women with the highest scores was expected due to demographic bias among this study based on voluntary participation. Thus, whether the incidence of falls is truly greatest in the high fall risk group remains to be studied with other cohorts.
The original KS risk categories were used in this study without any intention to modify the methodological aspects of the KS. A left-skewed distribution of the KS scores was evident and even if the risk factors of falls are well-established, apparently the cutoff points are subject to change. However, the redefinition of the KS categories would not be appropriate by utilizing the KFPS population alone, as the cut-off values of the KS would presumably be different in other populations.
The present study provided relevant information on issues that may need revision in the further versions of the KS fall risk assessment tool, and further research on this topic is still needed. However, it seems that the KS has future development potential for a simple, self-administered screening tool evaluating the risk of falls among the general population of older people. The World Falls Guidelines Task Force recently recommended that “opportunistic case finding for falls risk is recommended for community-dwelling older adults” [6] and KS may become an effective tool to answer this need.
Conclusions
The KS tool showed moderate reliability in predicting falls among this cohort of older women. However, the optimal number and location of cutoff points needs further research and validation.
Availability of data and materials
The raw data of the current study includes personal information and therefore it is not available as such. However, the data can be de-identified and made available on reasonable request from the corresponding author. The code used may also be made available upon request.
References
World Health Organization (WHO): Falls. https://www.who.int/news-room/fact-sheets/detail/falls. Accessed 29 May 2021
Institute for Health Metrics and Evaluation. Health data on Finland. [Internet: http://www.healthdata.org/finland]. Accessed 8 Apr 2021
Official Statistics of Finland (OSF): Causes of death [e-publication]. ISSN = 1799-5078. 2019, 5. Growth in number of accidental deaths halted in 2019. Helsinki: Statistics Finland. Accessed 16 Feb 2021
Official Statistics of Finland (OSF): Causes of death [e-publication]. ISSN = 1799-5078. 2017. Helsinki: Statistics Finland. Accessed 16 Feb 2021
Kannus P, Niemi S, Sievänen H et al (2018) Declining incidence in fall-induced deaths of older adults: Finnish statistics during 1971–2015. Aging Clin Exp Res 30:1111–1115
Montero-Odasso M, Van der Velde N, Martin FC et al (2022) World guidelines for falls prevention and management for older adults: a global initiative. Age Aging 51:1–36
Hou W, Kang C, Ho M et al (2017) Evaluation of an inpatient fall risk screening tool to identify the most critical fall risk factors in inpatients. J Clin Nurs 26:698–706
Hnizdo S, Archuleta RA, Taylor B et al (2013) Validity and reliability of the modified John Hopkins Fall Risk Assessment Tool for elderly patients in home health care. Geriatr Nurs 34:423–427
Patterson BW, Repplinger MD, Pulia MS et al (2018) Using the Hendrich II Inpatient fall risk screen to predict outpatient falls after emergency department visits. JAGS 66:760–765
Stapleton C, Hough P, Oldmeadow L et al (2009) Four-item fall risk screening tool for subacute and residential aged care: the first step in fall prevention. Australas J Ageing 28:139–143
Sardo PMG, Simões CSO, Alvarelhão JJM et al (2016) Fall risk assessment: retrospective analysis of Morse Fall Scale scores in Portuguese hospitalized adult patients. Appl Nurs Res 31:34–40
Solie C, Swanson M, Harland K et al (2020) Two-item fall screening tool identifies older adults at increased risk of falling after emergency department visit. West J Emerg Med 21:1275–1282
Yazdani C, Hall S (2017) Evaluation of the “medication fall risk score.” Am J Health Syst Pharm 74:e32–e39
Park S (2017) Tools for assessing fall risk in the elderly: a systematic review and meta-analysis. Aging Clin Exp Res 30:1–16
Rasche P, Nitsch V, Rentemeister L et al (2019) The Aachen falls prevention scale: multi-study evaluation and comparison. JMIR Aging 2:e12114
Demura S, Yamada T, Uchiyama M et al (2010) Selection of useful items for fall risk screening for community dwelling Japanese elderly from the perspective of fall experience, physical function, and age level differences. Arch Gerontol Geriatr 53:123–130
Cleary K, Skornyakov E (2017) Predicting falls in community dwelling older adults using the activities-specific Balance Confidence Scale. Arch Gerontol Geriatr 72:142–145
Russell MA, Hill KD, Blackberry I et al (2008) The reliability and predictive accuracy of the falls risk for older people in the community assessment (FROP-Com) tool. Age Ageing 37:634–639
Fielding SJ, McKay M, Hyrkas K (2013) Testing the reliability of the fall risk screening tool in an elderly ambulatory population. J Nurs Manag 21:1008–1015
Obrist S, Rogan S, Hilfiker R (2016) Development and evaluation of an online fall-risk questionnaire for nonfrail Community-Dwelling elderly persons: a pilot study. Curr Gerontol Geriatr Res 2016:1520932–1521016
Crow RS, Lohman MC, Pidgeon D et al (2018) Frailty versus stopping elderly accidents, deaths and injuries initiative fall risk score: ability to predict future falls. J Am Geriatr Soc 66:577–583
Tromp AM, Pluijm SMF, Smit JH et al (2001) Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 54:837–844
Pape H, Schemmann U, Foerster J et al (2015) The ‘Aachen Falls Prevention Scale’—development of a tool for self-assessment of elderly patients at risk for ground level falls. Patient Saf Surg 9:7
Elliott SJ, Ivanescu A, Leland NE et al (2012) Feasibility of interdisciplinary community-based fall risk screening. Am J Occup Ther 66:161–168
Bongue B, Dupré C, Beauchet O et al (2011) A screening tool with five risk factors was developed for fall-risk prediction in community-dwelling elderly. J Clin Epidemiol 64:1152–1160
Palumbo P, Klenk J, Cattelani L et al (2016) Predictive performance of a fall risk assessment tool for Community-Dwelling Older People (FRAT-up) in 4 European Cohorts. JAMDA 17:1106–1113
Bruce J, Hossain A, Ji C et al (2023) Falls and fracture risk screening in primary care: update and validation of a postal screening tool for community dwelling older adults recruited to UK Prevention of Falls Injury Trial (PreFIT). BMC Geriatr 23:42
Rubenstein LZ, Vivrette R, Harker JO et al (2011) Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. J Saf Res 42:493–499
Karinkanta S, Kulmala T, Kannus P et al (2017) KaatumisSeula®: Implementation of evidence-based fall prevention for communities. Innov Aging 1:522–523
KaatumisSeula®: Implementation of Evidence-Based Fall Prevention for Communities. UKK Institute. [Internet: https://ukkinstituutti.fi/en/research-development/promoting-safety-in-physical-activity/kaatumisseula-implementation-of-evidence-based-fall-prevention-for-communities/. Accessed 2 Feb 2021.
KaatumisSeula tools to prevent falls-web page. UKK Institute. https://ukkinstituutti.fi/en/products-services/kaatumisseula-tools-to-prevent-falls/. Accessed 21 Mar 2022.
Electronic form of the KaatumisSeula in Finnish. UKK Institute. https://ukkinstituutti.fi/liikkumisen-turvallisuus/kaatumisten-ehkaisy-ammattilaisille/materiaalia/kaatumisseula/. Accessed 21 Mar 2022
Karinkanta S, Edgren J, Uusi-Rasi K, Tokola K, Becker P, Nikander R, Sievänen H (2019) Conference abstract: is it repeatable, can it predict? Validation of self-rated fall risk screening tool among community-dwelling older adults. IAGG-ER Congress, Gothenburg
Vilpunaho T, Kröger H, Honkanen R et al (2019) Randomised controlled trial (RCT) study design for a large-scale municipal fall prevention exercise programme in community-living older women: study protocol for the Kuopio Fall Prevention Study (KFPS). BMJ Open 9:e028716
Vilpunaho T, Sund R, Koivumaa-Honkanen H et al (2021) Urban RCT participants were healthier than non-participants or rural women. J Clin Epidemiol 140:44–55
Soares WJS, Lopes AD, Nogueira E et al (2018) Physical activity level and risk of falling in community-dwelling older adults: systematic review and meta-analysis. J Aging Phys Act 27:1–43
Uusi-Rasi K, Karinkanta S, Kannus P et al (2020) Does long-term recreational gymnastics prevent injurious falls in older women? A prospective 20-year follow-up. BMC Geriatr 20:37
Rikkonen T, Salovaara K, Sirola J et al (2010) Physical activity slows femoral bone loss but promotes wrist fractures in postmenopausal women: a 15-year follow-up of the OSTPRE study. JBMR 25:2332–2340
Karinkanta S, Kannus P, Uusi-Rasi K et al (2015) Combined resistance and balance-jumping exercise reduces older women’s injurious falls and fractures: 5-year follow-up study. Age Ageing 44:784–789
Uusi-Rasi K, Patil R, Karinkanta S et al (2015) Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Intern Med 175:703–711
Uusi-Rasi K, Patil R, Karinkanta S et al (2017) A 2-year follow-up after a 2-year RCT with vitamin D and exercise: effects on falls, injurious falls and physical functioning among older women. J Gerontol Ser A Biol Sci Med Sci 72:1239–1245
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital. This work was supported by the Academy of Finland, the Ministry of Education and Culture, the Finnish Cultural Foundation’s North Savo Regional Fund, and the Uulo Arhio Foundation. The funding bodies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
TV: formal analysis, funding acquisition, visualization, writing—original draft. SK: conceptualization, methodology, writing—review and editing. HS: conceptualization, methodology, writing—review and editing. JK: formal analysis, writing—review and editing. HK: conceptualization, methodology, funding acquisition, writing—review and editing. TR: conceptualization, formal analysis, funding acquisition, investigation, methodology, writing—original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant financial or non-financial interest to disclose.
Research involving Human Participants & Informed consent
The study involved human participants and has been reviewed and approved by the Research Ethics Committee of the Hospital District of North Savo. All regulations and measures of ethics and confidentiality are handled in accordance with the Declaration of Helsinki. Written informed consent was received from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vilpunaho, T., Karinkanta, S., Sievänen, H. et al. Predictive ability of a self-rated fall risk assessment tool in community-dwelling older women. Aging Clin Exp Res 35, 1205–1212 (2023). https://doi.org/10.1007/s40520-023-02423-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02423-w