Abstract
Background
The Life-Space Assessment (LSA) can compliment traditional physical performance measures of mobility by accounting for the interaction between individuals and their environment. However, there are no studies that have generated percentile curves showing sex-stratified reference values in a large population-based sample of community-dwelling adults, making its interpretation difficult. Therefore, this study aimed to establish sex-stratified reference values for the LSA in middle-aged and older Canadians.
Methods
Baseline data for participants aged 45–84 years old from the Canadian Longitudinal Study on Aging (CLSA) were used (n = 22,154). Quantile regression was used to estimate specific percentiles, with age as the independent variable and LSA scores as the dependent variable. Models were run for the whole sample, then separately for males and females. The models were cross-validated to assess their reliability. CLSA inflation and analytic weights were applied.
Results
On average, the sample was 62.5 ± 10.0 y.o. (51.1% males), with a weighted mean LSA score of 89.2 ± 17.0. There was also a decrease in LSA scores with age, where scores were lower for older age groups compared to younger groups, and LSA scores were lower for females relative to males.
Discussion and conclusions
Reference data will aid in interpreting, comparing, and making inferences related to LSA scores obtained in clinical and research settings for Canadian adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A decline in mobility with age places a significant burden on older adults [1]. For example, impaired mobility is a predictor of falls, loss of independence, institutionalization, and death [2,3,4]. The literature consistently demonstrates that mobility is strongly associated with health and quality of life [5,6,7,8]. However, there is a mismatch between the level of functioning that individuals report as being capable of and the level of functioning that they achieve in their day-to-day life [9].
In 1998, Glass proposed a model to distinguish between three “tenses” of functioning: the hypothetical (i.e., what a person can do), experimental (i.e., what a person could do), and enacted (i.e., what a person does do) [9]. First, the hypothetical tense of functioning refers to the individual’s perceived ability, traditionally captured through self-report measures. Second, the experimental tense refers to the individual’s capability, which is often assessed by asking individuals to demonstrate their physical function in experimental or clinical settings (i.e., performance-based measures). Lastly, the enacted tense refers to the individual’s functional performance within the context of their home. Enacted functioning acknowledges situational and ecological factors that shape functioning in the real world. Although each tense represents different perspectives and may be more optimal in one situation over the other, relying solely on instruments which measure the hypothetical tense may lead to inaccurate estimates of disability rates, and underrepresentation of the importance of psychosocial factors in shaping functioning [9].
Mobility is often assessed in defined settings using physical performance measures, such as gait speed [10] and the Timed Up and Go test [11], capturing the experimental tense of functioning. Such physical performance measures focus on specific aspects of physical functioning (i.e., what individuals can do in experimental settings), but do not acknowledge the interaction between the person and environment (i.e., what individuals actually do in their daily life, including their homes) [12, 13].
Life-spaces refer to areas visited in everyday life (i.e., room, home, outdoors, neighborhood, service community, surrounding area, and world), and life-space mobility refers to an estimate of “the magnitude or extent of travel into the environment, regardless of how one gets there” [14]. In other words, life-space mobility captures an individual’s mobility within and outside their home. Notably, the construct of life-space mobility that has emerged in the literature [15] aligns well with Glass’s enacted tense of functioning.
The Life-Space Assessment (LSA) is the most widely used measure of life-space mobility [16, 17] and is gaining increasing attention in the literature for reflecting the mobility of individuals in their daily life, acting as an informative measure of aging-related changes and functional ability. Further, the LSA has been shown to predict important health outcomes, such as morbidity and healthcare utilization [18,19,20,21]. Given its advantages and its emerging use in research, reference data for the LSA is required to interpret, compare, and make inferences on scores obtained in clinical and research settings. To our knowledge, there are no studies that have generated percentile curves, using robust regression analyses, showing sex-stratified reference data for the LSA in a large population-based sample of community-dwelling Canadian adults, making its interpretation difficult. Therefore, the current study aimed to establish such sex-stratified reference values for the LSA using data from the Canadian Longitudinal Study on Aging (CLSA) for adults with no underlying mobility limitations [22, 23].
The CLSA offers a comprehensive population-based dataset from across Canada that is ideal for establishing sex-stratified reference values. We hypothesized that LSA scores will decrease with age. Further, LSA scores for females will be lower than LSA scores for males, given that among older adults, females with any disease experience lower physical functioning relative to males [24, 25], and the LSA has been shown to reflect this sex-based difference [26].
Method
Study design
A cross-sectional secondary analysis of the CLSA baseline Comprehensive Cohort dataset (collected 2012–2015) was conducted.
Sample
The CLSA is a Canada-wide, 20 year longitudinal study of around 50,000 community-dwelling adults aged 45–85 years at baseline [22, 23]. All 50,000 participants were asked to provide a core set of information regarding multiple measures (e.g., lifestyle/behaviour, social, physical/clinical, psychological, economic, and health status measures). Additionally, 30,000 of the 50,000 participants were asked to supplement this core set with in-depth information (i.e., via interviews, physical examinations, and biospecimen collection), forming the CLSA Comprehensive Cohort. The CLSA Comprehensive Cohort was used for this study.
The CLSA’s eligibility criteria excluded individuals who were: residents in the three territories and some remote regions, living on federal First Nations reserves and other First Nations settlements in the provinces, full-time members of the Canadian Armed Forces, unable to respond in English or French, temporary visa holders or have transitional health coverage, and living in long-term care institutions. Further, individuals with cognitive impairments or participants judged by the CLSA interviewers as unable to understand the purpose of the study and/or provide reliable data were excluded.
The current study employed a subset of the CLSA Comprehensive Baseline Dataset to include all eligible participants ages 45–84 years. Participants with incomplete data on the LSA were excluded. Further, participants who: (i) had any injury over the last 12 months that limited normal activities, (ii) underwent surgery over the last three months, (iii) had chemotherapy in the last four weeks, and (iv) were currently receiving dialysis treatment were also excluded (participants with missing or incomplete values for these criteria were not excluded to avoid making assumptions about their health state). Lastly, individuals who reported one or more limitations in activities of daily living (ADL)/ instrumental activities of daily living (IADL) were considered to have ADL disability and were excluded (participants with missing or inconclusive values were excluded to ensure that the included sample did not have any functional limitations). This exclusion criterion is necessary to ensure that the reference sample generated was representative of healthy aging and minimize the influence of underlying mobility limitations or serious chronic diseases.
Outcome measure
The LSA was completed using an in-home face-to-face interview and asks participants about the life-spaces they visited (i.e., 1 = rooms in the house outside of the bedroom, 2 = yard or immediate outdoor area, 3 = their neighbourhood, 4 = neighbourhoods outside their own, and 5 = outside of their city or town) [17]. Specifically, the LSA asks if an individual went to a certain life-space in the past 4 weeks (“Yes” or “No” for each level), with a “No” option scoring a 0, a level 1 life-space scoring 1 point for "Yes,” incrementally increasing until the 5th life-space level which is given a score of 5 points for “Yes” [17]. Participants are then asked about the frequency of their movement within each life-space (i.e., 1 = < 1/week, 2 = 1–3 times/week, 3 = 4–6 times/week, and 4 = daily), and if assistance was required (i.e., 1 = personal assistance, 1.5 = assistive devices, 2 = no assistance) [17]. The method of scoring which accounts for all of this information is called the composite score (LS-C) and is calculated by multiplying the values across each level, and then the 5 level scores are added together. This scoring produces a value that can range from 0 to 120, with a change of 5 or more points considered clinically meaningful [17, 27]. The LSA scores presented in this paper are the calculated composite scores (i.e., LS-C scores).
Ethical considerations
This study received approval from the Hamilton Integrated Research Ethics Board (HiREB application #8131).
Analysis
Descriptive summary statistics are presented as means and standard deviations (SD) for continuous variables. Counts and percentages are presented for categorical data. As the data did not meet the assumptions of a linear regression, quantile regression was used to estimate specific percentiles (i.e., 5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles), with age measured continuously as the independent variable and LSA scores as the dependent variable [28, 29]. Quantile regression was also used as it allows for the exploration of the relationship between variables at different percentiles. Cross-validation was used to compare between linear, quadratic, and cubic polynomials for age. To cross-validate the models, from each year of age and sex strata, 70% of the included sample was randomly selected by the software as the “training” sample, while the remaining 30% was selected as the “testing” sample. The model fitted in the training sample was applied to the “testing” sample. The observed versus expected count of participants with measurements within each percentile range were determined. This process was repeated one hundred times using a seed of 1234. The cross-validation suggested that the quadratic model was satisfactory, compared to the linear or cubic models, as assessed by the proportion of the population covered by each percentile range (e.g., whether the 5th percentile covered 5% of the population) (Supplementary File 1: Table 2). Models were run for the sample, and then separately for males and females. Mean percentile values of the resulting model are presented by sex and age group (45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, and 80–84 years).
To generalize the results to the Canadian population and account for the complex survey design of the CLSA, sampling weights were incorporated into the analyses. As recommended and provided by the CLSA [22, 23], inflation weights were applied to the descriptive summary statistics (i.e., means and standard deviations), while analytic weights were applied to the quantile regression analyses. The appropriateness of the sampling weights was then assessed after removal of participants as per the exclusion criteria. Significance levels for all statistical tests were set at the 0.05 level, and statistical analyses were conducted using STATA version 16.0 or R version 4.1.1. for Macintosh software.
Results
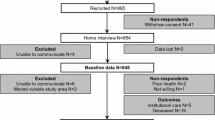
As per the eligibility criteria, participants were excluded if they had incomplete data on the required questions of the LSA, which comprised 0.2% (n = 53) of the whole sample. Furthermore, participants with any injury over the last 12 months that limited normal activities (n = 4,362), underwent surgery over the last three months (n = 1,243), had chemotherapy in the last 4 weeks (n = 95), were currently receiving dialysis treatment (n = 14), and reported having ADL/IADL limitations (n = 2,931) or had an inconclusive ADL/IADL classification due to missing values (n = 108) were excluded.
Table 1 outlines the unweighted characteristics of the whole sample (n = 22,154), for males (n = 11,330) and females (n = 10,824). Around 50% of the participants were males (51.1%) and the mean age of the sample was 62.5 years (SD = 10.0). Majority of the sample had a post-secondary degree/diploma (78.1%), had at least one chronic condition (90.5%), and lived in an urban environment (90.5%).
Table 2 outlines the weighted LSA scores for the whole sample, as well as for males and females separately, after the incorporation of the sampling weights. The weighted LSA scores ranged from 0 to 120 for both males and females, with a mean LSA score of 89.2 (SD = 17.0) for the whole sample, 91.0 (SD = 16.6) for males, and 87.4 (SD = 17.3) for females, suggesting that, on average, the sample was able to move independently outside their neighborhood (i.e., LSA score > 60) [30]. Weighted mean LSA scores were typically lower for females compared to males. There was also a decrease in LSA scores with age, where scores were lower for older age groups compared to younger groups.
Table 3 presents a summary of results of the quantile regression, outlining the percentile mean values for the weighted sex-stratified reference values for the LSA scores (i.e., 5th to 95th percentiles) by age group (see Supplementary File 1: Table 1 for the reference values of the whole sample, and Supplementary File 2 for quantile regression raw percentile scores). The cross-validation suggested that the quadratic model was satisfactory, compared to the linear or cubic models, as assessed by the proportion of the population covered by each percentile range (e.g., whether the 5th percentile covered 5% of the population) (Supplementary File 1: Table 2). Choice of the quadratic model was also supported by the visual inspection of the data. LSA scores were lower for the higher age groups and lower for females relative to males. These age-specific percentile trends are further illustrated in Figs. 1 and 2 (see Supplementary File 1: Fig. 1 for age-specific percentile trends of the whole sample). The greatest decline in LSA scores generally occurred in the sixties, with an earlier decline occurring in the early fifties for those in the bottom percentiles (i.e., 5th and 10th). In addition to identifying trends, these graphs can be used to compare an individual’s score relative to others of the same age and sex.
Discussion
To our knowledge, this is the first study to use a population-based dataset and robust regression-based analyses to establish sex-stratified reference values for the LSA and present corresponding percentile graphs in community-dwelling Canadian adults aged 45–84 years. Overall, LSA scores were lower for older individuals and for females. By generating reference values using quantile regression, the current study provided an opportunity to investigate the effect of age on LSA scores at the different percentiles of the population, as stratified by sex. Although the greatest decline in LSA scores occurred around 60 years of age, earlier declines (i.e., in the early fifties) were observed in the lower percentiles (i.e., 5th and 10th), suggesting that those individuals could be more at risk of experiencing earlier functional limitations.
The trends in reference values from the current study are comparable to those obtained from Australia (n = 3032) using data from the South Australian Health Omnibus Survey. Australian reference values show that LSA scores were lower for older age groups, and that females have lower LSA scores than males [26]. More specifically, after 55 years, LSA scores in Australia were lower in females relative to males [26]. Similarly, in the current study, LSA scores were lower with increasing age in Canada, and were lower for females relative to males. Also, the greatest decreases in LSA scores by age occurred in the late fifties, with females showing larger decreases than males. Previous research provides an explanation for these sex-based differences: it has demonstrated that, among older adults, females with any disease/condition experience lower physical functioning relative to males [24, 25], and the LSA has been shown to reflect this sex-based difference [26].
In the literature, LSA scores < 60 typically indicate “restricted” life-space mobility (i.e., that individuals are confined to their neighborhood) [30]. On the other hand, LSA scores > 60 have been associated with an individual’s ability to get out of their neighborhood independently (i.e., “un-restricted life-space”) [30]. It is important to note that various factors can contribute to having a restricted life-space mobility besides physical function (e.g., reduced social participation). Our results show that the age at which individuals’ LSA scores drop below 60 varies by sex. For the whole sample, restricted LSA scores are observed after 65 years in the 5th percentile, and after 75 years at the 10th percentile. For males, restricted LSA scores are observed after 70 years for the 5th percentile and after 80 years for the 10th percentile. For females, restricted LSA scores are observed earlier than men, with the 5th percentile showing restricted LSA scores after 60 years and the 10th percentile after 70 years. Scores at other percentiles were not less than 60 points within this sample, suggesting that individuals at lower percentiles are most at risk for having restricted life-space mobility. This is critical as restricted LSA scores have been associated with negative health outcomes, such as a greater risk (4.4 times) of admissions to a nursing home after six years, relative to those with unrestricted life-space mobility [31], and individuals performing at these lower percentiles should be addressed to mitigate the effect of negative health outcomes. The LSA can track declines in individuals’ community mobility, often preceding IADL/ADL limitations [31], and can provide an opportunity for early multidisciplinary intervention, specifically for those performing at lower percentiles of the population.
Restrictions in LSA scores can result from a variety of different factors. For example, Peel et al. [16] demonstrated that ADL, IADL, and the Short Physical Performance Battery (SPPB) only explained 45.5% of LSA score variability, suggesting that elements of social participation could also be reflected within this variability in scores. Furthermore, Kuspinar et al. [12] suggested that driving, social support, and walking speed were most associated with LSA scores in the CLSA. Together, these studies show that the LSA could be capturing aspects of daily mobility that are not reflected in traditional physical performance measures. The variables mentioned (e.g., physical function, driving, and social support) tend to decrease with age and could be contributing to the overall LSA trends observed in this study (e.g., restrictions were observed around the age at which people tend to retire and stop commuting). Moreover, environmental barriers play a critical role in influencing life-space mobility: individuals experiencing high curbs or a lack of sidewalks have higher odds of restricted life-space mobility [15]. This further highlights the utility of the LSA in assessing a wholistic view of mobility, providing an opportunity for the exploration of the different factors that influence mobility from the home to the outside world.
The three tenses of functioning (i.e., the hypothetical, experimental, and enacted), defined by Glass, represent different yet complimentary perspectives on functioning [9]. Assessing one tense over another is likely to have different applications; however, relying solely on measuring the hypothetical tense may lead to an inaccurate estimation of disability rates and mobility in everyday life [9]. It is, therefore, important to consider the use of the LSA to compliment the use of other mobility measures [9]. Furthermore, since the LSA predicts morbidity, mortality, and healthcare utilization [18,19,20,21], declines in life-space mobility could indicate an early decline in functioning, providing an opportunity to intervene early during a period when interventions are more likely to result in improvement [16]. Having population-specific, sex-stratified reference values of the LSA then becomes essential to clinicians and researchers in Canada when assessing patients’ performance relative to the general population and, if needed, determining appropriate courses of action/treatment.
A strength of this study is the use of robust, regression-based methods and the use of a large population-based dataset and sampling weights. However, given that the data collection sites of the CLSA are located in urban regions and given the CLSA’s exclusion criteria, results of this study may not apply to those living in remote regions and the three territories, federal First Nations reserves and other First Nations settlements in the provinces. The sample may also not be representative of those who are not English- or French-speaking. Further, the percentile scores are limited to providing information about LSA score distribution and do not provide information about which scores are indicative of risk. Lastly, the data was collected between 2012 and 2015, prior to the COVID-19 pandemic, and may not reflect any changes in life-space mobility that were a consequence of it. Future research could determine LSA scores that are indicative of risk of negative health outcomes, as well as investigate the effect of the COVID-19 pandemic on LSA scores.
Conclusions
In conclusion, this study determined sex-stratified reference values for the LSA in community-dwelling middle-aged and older Canadians aged 45–84 years. The results suggest that LSA scores are lower for females and decline with age, with earlier declines observed among those scoring in the lowest percentiles. Consideration of life-space mobility is important for a comprehensive assessment of mobility and these population-based reference values will aid clinicians and researchers in interpreting LSA scores of individuals in Canada.
Data availability
All relevant data are presented in the manuscript and supplementary materials.
References
Bizier C, Fawcett G, Gilbert S (2016) Mobility disabilities among Canadians aged 15 years and older, 2012. Statistics Canada= Statistique Canada
Hirvensalo M, Rantanen T, Heikkinen E (2000) Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc 48:493–498. https://doi.org/10.1111/j.1532-5415.2000.tb04994.x
Rubenstein LZ, Powers CM, MacLean CH (2001) Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders. Ann Intern Med 135:686–693. https://doi.org/10.7326/0003-4819-135-8_part_2-200110161-00007
von Bonsdorff M, Rantanen T, Laukkanen P et al (2006) Mobility limitations and cognitive deficits as predictors of institutionalization among community-dwelling older people. Gerontology 52:359–365. https://doi.org/10.1159/000094985
Groessl EJ, Kaplan RM, Rejeski WJ et al (2007) Health-related quality of life in older adults at risk for disability. Am J Prev Med 33:214–218. https://doi.org/10.1016/j.amepre.2007.04.031
Shafrin J, Sullivan J, Goldman DP et al (2017) The association between observed mobility and quality of life in the near elderly. PLoS ONE 12:e0182920. https://doi.org/10.1371/journal.pone.0182920
Netuveli G, Wiggins RD, Hildon Z et al (2006) Quality of life at older ages: evidence from the English longitudinal study of aging (wave 1). J Epidemiol Community Health 60:357–363. https://doi.org/10.1136/jech.2005.040071
Yeom HA, Fleury J, Keller C (2008) Risk factors for mobility limitation in community-dwelling older adults: a social ecological perspective. Geriatr Nurs 29:133–140. https://doi.org/10.1016/j.gerinurse.2007.07.002
Glass TA (1998) Conjugating the “tenses” of function: discordance among hypothetical, experimental, and enacted function in older adults. Gerontologist 38:101–112. https://doi.org/10.1093/geront/38.1.101
Peel NM, Kuys SS, Klein K (2013) Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci 68:39–46. https://doi.org/10.1093/gerona/gls174
Bohannon RW (2006) Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther 29:64–68. https://doi.org/10.1519/00139143-200608000-00004
Kuspinar A, Verschoor CP, Beauchamp MK et al (2020) Modifiable factors related to life-space mobility in community-dwelling older adults: results from the Canadian Longitudinal Study on Aging. BMC Geriatr 20:35. https://doi.org/10.1186/s12877-020-1431-5
Taylor JK, Buchan IE, van der Veer SN (2019) Assessing life-space mobility for a more holistic view on wellbeing in geriatric research and clinical practice. Aging Clin Exp Res 31:439–445. https://doi.org/10.1007/s40520-018-0999-5
Stalvey BT, Owsley C, Sloane ME et al (1999) The life space questionnaire: a measure of the extent of mobility of older adults. J Appl Gerontol 18:460–478. https://doi.org/10.1177/073346489901800404
Johnson J, Rodriguez MA, Al SS (2020) Life-space mobility in the elderly: current perspectives. Clin Interv Aging 15:1665–1674. https://doi.org/10.2147/CIA.S196944
Peel C, Sawyer Baker P, Roth DL et al (2005) Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther 85:1008–1119
Baker PS, Bodner EV, Allman RM (2003) Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc 51:1610–1614. https://doi.org/10.1046/j.1532-5415.2003.51512.x
Iyer AS, Wells JM, Bhatt SP et al (2018) Life-Space mobility and clinical outcomes in COPD. Int J Chron Obstruct Pulmon Dis 13:2731–2738. https://doi.org/10.2147/COPD.S170887
Kennedy RE, Williams CP, Sawyer P et al (2019) Life-space predicts health care utilization in community-dwelling older adults. J Aging Health 31:280–292. https://doi.org/10.1177/0898264317730487
Lo AX, Brown CJ, Sawyer P et al (2014) Life-space mobility declines associated with incident falls and fractures. J Am Geriatr Soc 62:919–923. https://doi.org/10.1111/jgs.12787
Mackey DC, Lui LY, Cawthon PM et al (2016) Life-space mobility and mortality in older women: prospective results from the study of osteoporotic fractures. J Am Geriatr Soc 64:2226–2234. https://doi.org/10.1111/jgs.14474
Raina PS, Wolfson C, Kirkland SA et al (2009) The Canadian longitudinal study on aging (CLSA). Can J Aging 28:221–229. https://doi.org/10.1017/S0714980809990055
Raina P, Wolfson C, Kirkland S et al (2019) Cohort profile: The Canadian Longitudinal Study on Aging (CLSA). Int J Epidemiol 48:1752–1753i. https://doi.org/10.1093/ije/dyz173
Macklai NS, Spagnoli J, Junod J et al (2013) Prospective association of the SHARE-operationalized frailty phenotype with adverse health outcomes: evidence from 60+ community-dwelling Europeans living in 11 countries. BMC Geriatr 13:3. https://doi.org/10.1186/1471-2318-13-3
Stenholm S, Westerlund H, Head J et al (2015) Comorbidity and functional trajectories from midlife to old age: the Health and Retirement Study. J Gerontol A Biol Sci Med Sci 70:332–338. https://doi.org/10.1093/gerona/glu113
Phillips J, Dal Grande E, Ritchie C et al (2015) A population-based cross-sectional study that defined normative population data for the life-space mobility assessment-composite score. J Pain Symptom Manage 49:885–893. https://doi.org/10.1016/j.jpainsymman.2014.09.010
Kennedy RE, Almutairi M, Williams CP et al (2019) Determination of the minimal important change in the life-space assessment. J Am Geriatr Soc 67:565–569. https://doi.org/10.1111/jgs.15707
Balion C (2019) Rethinking reference intervals for older adults: data from the Canadian Longitudinal Study on Aging (CLSA). Paper presented at the Annual Conference of the Canadian Society Of Clinical Chemists, Saint John, NB, Canada
Jung Y, Hu J (2015) A K-fold averaging cross-validation procedure. J Nonparametr Stat 27:167–179. https://doi.org/10.1080/10485252.2015.1010532
Sawyer P, Allman RM (2019) Resilience in mobility in the context of chronic disease and aging. New frontiers in resilient aging. Cambridge University Press, pp 310–339
Sheppard KD, Sawyer P, Ritchie CS et al (2013) Life-space mobility predicts nursing home admission over 6 years. J Aging Health 25:907–920. https://doi.org/10.1177/0898264313497507
Acknowledgements
This research was made possible using the data/biospecimens collected by the Canadian Longitudinal Study on Aging (CLSA). This research has been conducted using the CLSA dataset Baseline Comprehensive Version 5.0, under Application Number 190239. The CLSA is led by Drs. Parminder Raina, Christina Wolfson and Susan Kirkland. PR holds the Raymond and Margaret Labarge Chair in Optimal Aging and Knowledge Application for Optimal Aging and a Tier 1 Canada Research Chair in Geroscience. MB holds a tier 2 Canada Research Chair in Mobility, Aging, and Chronic Disease.
Funding
Funding for the Canadian Longitudinal Study on Aging (CLSA) is provided by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference: LSA 94473 and the Canada Foundation for Innovation, as well as the provinces of Newfoundland, Nova Scotia, Quebec, Ontario, Manitoba, Alberta, and British Columbia. This research was supported by a Labarge Mobility scholarship from the Labarge Centre for Mobility in Aging within the McMaster Institute for Research on Aging (MIRA) at McMaster University.
Author information
Authors and Affiliations
Contributions
Conceptualization: AK. Methodology: SM, AM, AK, MB, JR, PR. Analysis: SM, AM, HYS, AK. Writing, original draft preparation: SM. Writing, review, and editing: SM, AM, AK, MB, JR, PR. Supervision: AK. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
None reported.
Informed Consent
As per the CLSA protocol.
Human and animal rights
As per the CLSA protocol.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Malouka, S., Mayhew, A.J., So, H.Y. et al. Sex-stratified reference values for the life-space assessment in the Canadian longitudinal study on aging. Aging Clin Exp Res 35, 1073–1080 (2023). https://doi.org/10.1007/s40520-023-02382-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02382-2