Abstract
Objective
This study aims to analyse the impact of the pandemic on the amount of use and new medication dispensation for chronic diseases in the Italian population aged 65 years and older (almost 14 million inhabitants).
Methods
The “Pharmaceutical Prescriptions database”, which gathers data on medications, reimbursed by the National Health Service and dispensed by community pharmacies, was employed. Data were analysed as amount of use (defined daily dose—DDD per 1000 inhabitants); variation in DDD between 2020 and 2019 was calculated for the 30 categories with major consumption in 2020. Trends in prevalence and incidence of dispensations between 2020 and 2019 were calculated for four categories: antidiabetics, antihypertensives, antidepressants and drugs for respiratory diseases.
Results
All medications showed a negative variation in DDD/1000 inhabitants between 2020 and 2019 except for anticoagulants (+ 5%). The percentage variation ranged from − 27.7% for antibiotics to − 6.4% for antipsychotics in 85 + year-old persons, but increased for most classes in the youngest (65–69 years). On the other hand, a decrease of the dispensation incidence of antidiabetics, antihypertensives, antidepressants and drugs for pulmonary disease was high, especially in the two extreme age groups, the youngest and the oldest one.
Conclusions and relevance
Great variation in medication use between 2020 and 2019 was observed probably reflecting the low rate of infectious diseases due to the widespread use of protective devices and self-isolation, reduced healthcare access because of the lockdowns and the fear of going to hospital, and the reduction of screening and diagnostics due to health-care system overload.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In March 2020, the World Health Organization declared a pandemic after the coronavirus disease 2019 (COVID-19), a novel infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), spread worldwide in a few months [1]. Due to its high direct mortality and impact on hospitalization, COVID-19 has put pressure on the health-care systems. Primary care was drastically impacted by the pandemic, resulting in challenges in the treatment of chronic diseases which require routine care [2]. First, national lockdowns, social distancing restrictions and different organizational rules for the admission to medical ambulatories were likely to affect health-care access [3]. Second, to prevent infection, people may have decided to postpone visits with their general practitioner, both for monitoring existing health conditions and for the onset of new signs and symptoms [4]. This resulted in an increase of missed and untimely diagnoses as shown in previous studies. The incidence of hospital admissions for acute coronary syndrome decreased as well as the provision of mammograms [5,6,7,8].
Italy was one of the first Western countries greatly affected by the pandemic, particularly the Northern regions. The older population was affected in terms of hospitalizations and mortality, accounting for 20% of the total number of subjects infected with SARS-CoV-2, but representing more than 90% of deaths [9]. Further, older persons are the part of the population mostly affected by multiple non-communicable diseases [10] which require chronic pharmacological prescriptions.
Different policies have been adopted in Italy to balance the need of reducing the infections and guaranteeing the therapeutic continuity for other diseases, such as the introduction of the electronic prescription, but there was a gap in knowledge regarding medications’ accessibility by patients, especially during the first year of the pandemic. From a National Health Service (NHS) perspective, it is of utmost importance to measure the effects of the pandemic on accessibility to medications to estimate the future consequences in terms of mortality and morbidity and to improve health-care accessibility during this and future pandemics.
This study aims at analysing the impact of the pandemic on the use of medicines in Italy in older persons comparing medication use in the outpatient setting in 2020 to that registered in 2019.
Methods
Data analysis
This is a quasi-experimental study based on aggregated administrative data. For the present analysis, we extracted records from the Pharmaceutical Prescriptions database (also known as the Italian Health Insurance Card database) that includes patient-level data on medicines prescribed and dispensed by community pharmacies reimbursed by Italian NHS in the Italian population aged 65 and older (almost 14 million inhabitants) [11]. Information on each drug package, identified via package unique identifier codes and the 5th level Anatomical Therapeutic Chemical (ATC) classification, was tracked at the individual level. The medicines were grouped into therapeutic classes according to the main indication, and the first 30 categories which had shown major consumption in 2020 were analysed [12].
Drug consumption was measured as the number of defined daily dose (DDD), which is the assumed average maintenance dose per day for a drug used for its main indication in adults [13]. It represents a standard in performing valid and reliable cross-national or longitudinal studies on drug consumption. The indicator calculated as “number of DDD per 1,000 inhabitants” was used and it was calculated by dividing the total number of DDDs prescribed and dispensed during 2019 and 2020 by the total number of inhabitants in the Italian population in the specific age group and sex. The result was then divided by 365 and reported per 1000 inhabitants.
Prevalence and incidence of use were assessed for four commonly prescribed medications classes, i.e. antidiabetics, antihypertensives, antidepressants and drugs for chronic pulmonary disease. The prevalence of use was calculated by dividing the number of individuals receiving at least one medication in 2019 and 2020 by the total number of Italian individuals in that same age group as reported by the Italian National Institute of Statistics in January 2019 and 2020. The incidence of use was estimated dividing the number of subjects that received the first dispensation (new users) of a medication belonging to a specific therapeutic category by the subjects at risk. The new users were defined as patients who did not receive a medical dispensation in the previous 6 months. The results of prevalence and incidence were reported per 1000 inhabitants. To estimate the impact of COVID-19 on medication use, the variation between 2020 and 2019 was calculated.
Ethical considerations
Ethical review and approval were not required for this study in accordance with the local legislation and institutional requirements.
Results
In the whole population analysed, almost all medication categories showed a negative variation in DDD/1000 inhabitants between 2020 and 2019; the biggest differences were reported for the following: antibiotics (− 22.9%) without differences by sex; drugs for the genital system/sexual hormones (− 17.6%) with a greater reduction in women than in men; dermatological and non-steroidal anti-inflammatory drugs (− 13%) without differences by sex. Anticoagulants were the only class showing an increase in dispensation between 2020 and 2019 (+ 5.0%), similarly in men and women (Table 1).
Table 2 describes the DDD/1000 inhabitants and the percentage variation between 2020 and 2019 for the 30 most used categories according to age groups. The age group with the widest negative difference between 2020 and 2019 was the one including persons 85-year-old and older ranging from − 27.7% for antibiotics to − 6.4% for antipsychotics; notably, this was the only age group with a negative variation of anticoagulants too (− 7.4%). The group of people aged 80–84 years was also characterized by a negative variation in dispensation of almost all drug categories, despite to a lesser extent than the oldest ones, except for anticoagulants (+ 2.3%) and antipsychotics (+ 0.7%). On the contrary, in the youngest age group, i.e. 65–69 years, the percentage variation in medication use was positive for most classes, ranging from + 0.1% for antipsychotics to + 15.8% for anticoagulants.
Few medications showed a negative variation across all age groups, namely, non-steroidal anti-inflammatory drugs (from − 25.3% in 85 + to − 5.8% in 65–69 years), antibiotics (from − 27.7% in 85 + to − 19.7% in in 75–79 years), dermatologic drugs (from − 25.2% in 85 + to − 5.7% in 65–69 years), and drugs for the genital system/sexual hormones (from − 26.0% in 85 + to − 13.6% in 65–69 years).
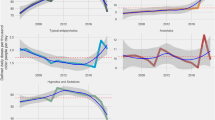
Figures 1, 2, 3, and 4 show the difference in DDD/1000 inhabitants, prevalence, and incidence between 2020 and 2019 of antidiabetics, antihypertensives, drugs for chronic pulmonary disease and antidepressants, according to age groups and sex. Incidence variations between 2020 and 2019 were very high in both men and women in all the four categories: for antidiabetics incidence ranged from − 35% in men to − 30% in women; for antihypertensives from − 47% in men to − 42% in women, for antidepressants from − 18.9% in women to − 14.6% in men, and for respiratory drugs from − 38% in women to − 35% in men (Figs. 1a, 2a, 3a, 4a). When we analysed incidence variation across age groups, we found that the highest negative trend was in the youngest persons (65–69 years) for antidiabetics (− 57%) and for antidepressants (− 35%) and in the oldest ones (85 + years) for respiratory drugs and for antihypertensives (− 43, − 75%, respectively).
Discussion
In our analysis, we found that almost all medications had a negative percentage variation in DDD/1000 inhabitants between 2020 and 2019 except for anticoagulants. However, variation varied widely according to age and was highest in 85 + year-old persons. On the contrary, in the youngest age group (65–69 years), the percentage variation in medication consumption was positive for most drug classes, reaching + 15.8% for anticoagulants. Notably, when we calculated the incidence of dispensation of four common drug classes, i.e. antidiabetics, antihypertensives, antidepressants and drugs for chronic pulmonary disease, and its difference between 2020 and 2019, we found huge negative variations (− 32.8,− 44,− 17 and− 36.9%, respectively).
The impact of COVID-19 pandemic on the worldwide population has been dramatic, especially in the older age strata. According to the Italian National Health Institute, 75.000 individuals died because of COVID-19 during 2020, 10% of all deaths in Italy [14]. Beyond mortality, it is already clear that the effects of the pandemic in older persons will include symptoms of long-term COVID in those who survived the infection [15] and possibly consequences of social isolation and change in care provision.
One implication of the pandemic which has been poorly analysed is the observed trend in medication consumption between 2020, when the pandemic initiated, and the previous years. Reasons for a change in the amount, prevalence and incidence of medication use may have several explanations; first, the decrease in doses used in 2020 in the very old persons may reflect the high mortality in this stratum of the population. The mean age of persons who died in Italy due to COVID-19 was 80 years (median is 82); among all deaths only 1.2% of persons were 50-year-old or younger [14]. Further, the mean number of comorbidities in those who died was 3.7, and 67.7% were affected by at least three co-existent diseases [16]. Considering that polypharmacy increases with increasing age and with the number of co-occurring diseases, it is obvious that the most negative variation amount of drug use is found in persons aged 80 + years. On the other hand, the maintenance and, for some drug classes, the increase in prevalence of dispensation in the younger adults during 2020 show the ability of the national and regional health systems to providing care supplies to patients already treated for chronic diseases even during the worst months of the pandemic. The only positive variation in DDD/1000 inhabitants concerns the class of anticoagulants. This data is not surprising considering that both low-weight heparins and oral direct anticoagulants were widely prescribed to treat COVID-19 intrinsic risk of coagulopathy and its consequences, such as deep venous thrombosis, even at home [17].
Second, underdispensation of some specific medications such as antibiotics and anti-inflammatories may reflect a lower rate of infectious diseases due to the widespread use of protective devices and self-isolation during lockdown periods as well as better appropriateness of antibiotic prescription for upper respiratory infections. Studies have reported a reduction in commonly prescribed antibiotics in several countries. A decrease in antibiotic consumption was observed in the European Union/European Economic Area-wide between 2019 and 2020 and it is the largest in European Surveillance of Antimicrobial Consumption Network’s two-decade long antimicrobial consumption surveillance history [18]. Overall, antibiotic consumption decreased by 18.3% between 2019 and 2020 and the largest decrease in terms of DDD/1,000 inhabitants between 2019 and 2020 was observed for penicillins [18]. Similar changes in community antibiotic consumption have been described at the national levels: in the adult population of primary care in Asturias in the period from March to December 2020, the consumption of antibiotics decreased by 28.6% compared to the same period in 2019 [19]. Similar data were found in primary care in Andalusia with the sharpest decline occurring in the second quarter of 2020, when the lockdown was more extensive [20]. In the USA, significant reductions in mean monthly fills of the four most prescribed outpatient agents (i.e. amoxicillin, azithromycin, amoxicillin–clavulanate, doxycycline) were found in April and persisted throughout 2020, compared to estimations based on pre-pandemic trends [21]. Considering trend in other medication use, in a very large study evaluating psychotropic drugs in comparison with statins in the 13 weeks before and after the first-known COVID-19-related death in California, in contrast to continued prescriptions, new fills for psychotropic medications were substantially lower than what would have been expected based on 2019 rates. Patients were especially less likely to fill new prescriptions for benzodiazepines, hypnotics, and statins and those aged ≥ 65 years demonstrated decreased fills for most medication classes [22].
Finally, when we evaluated the incidence of dispensation of some common medication classes and its difference between 2020 and 2019, we found negative variations in all age groups, but especially in the young-old (65–69 years) and the very old (85 + years). Different reasons may have led to a reduction in the incidence of dispensation according to age; on one hand, the lockdown, the lack of social support and the fear of going to hospitals may explain the phenomenon in persons aged 85 years or older; on the other hand, the reduction of screening and diagnostics due to the health-care system overload have probably led to a reduction of first diagnoses in the young-old. Indeed, the COVID‐19 pandemic has affected all areas of the health-care system, not just infectious disease, and critical care [23]. The first wave of COVID‐19 was associated with decreases and delays in acute care presentations for cardiovascular diseases such as myocardial infarction in the USA and Europe [24]. Primary cancer screenings (e.g. low‐dose chest CT, colonoscopies) could not be performed without significant risk leading to delays in diagnosis. Given health professionals’ reassignment, and reduced operating room capacity, it is likely that chemotherapy, radiation therapy and surgical excision of tumours were delayed [25]. Further, the COVID-19 pandemic prevented some individuals from keeping regular medical appointments even in countries with a low infection risk; in Taiwan the visits of the elderly (≥ 80 years) were the most frequent before the COVID-19 pandemic but were reduced by 44% [26].
Strengths and limitations
This study has several limitations. Data on reimbursed medications exclude unfilled prescriptions and non-reimbursed medications. This might have led to an underestimation of the prevalence and incidence of use and the amount of consumption, although it is important to highlight that in Italy medicines proven to be effective for the treatment of acute or chronic diseases are covered by NHS and private purchase represents less than 30% of the outpatient consumption. It is worth noting that oncological drugs in Italy are mostly dispensed in the inpatient setting; therefore, data presented in this study related to medicines dispensed by community pharmacies could not provide a full picture for this category. Differences in the use of anti-osteoporotic drugs observed can be explained by a change in the prescription regulation, occurring at the end of 2019 [27]. Since the data referred to prescribed and dispensed medicines, it is not possible to evaluate medication adherence and the actual intake of the medications by patients, information particularly relevant in the management of chronic diseases [28]. Moreover, the analysis did not consider medication use during potential hospitalization periods of patients, for instance for the treatment of COVID-19. Finally, the annual analysis included individuals that had died within the year; however, since the analysed data referred to the entire Italian population aged 65 years and older, it is unlikely that the difference in medications use between 2020 and 2019 might have been influenced by the mortality rate. While it is true that the pandemic onset was the major acute event characterizing the period 2019–2020, there may be unmeasured events that may explain medication utilization patterns over time. Despite these limitations, our study provides important insights into the impact of the pandemic on medication utilization in older people in Italy.
Conclusions
Variation in drug dispensation between 2020 and 2019 is a consequence of the COVID-19 pandemic: first, underprescription of some specific drug categories such as antibiotics and anti-inflammatory drugs may reflect a lower rate of infectious diseases due to the widespread use of protective devices and self-isolation; second, the lockdown, the fear of going to hospital and the reduction of screening and diagnostics due to health-care system overload may have led to a dramatic reduction of first drug prescriptions. The consequences of underdiagnosis and underprescription should be a priority of future studies.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available because of data sharing legal restrictions, the dataset including individual records cannot be made publicly available. However, aggregated data will be shared on reasonable request to the corresponding author.
References
https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (last access March 11st, 2022)
Ismail H, Marshall VD, Patel M et al (2021) The impact of the COVID-19 pandemic on medical conditions and medication adherence in people with chronic diseases. J Am Pharm Assoc. https://doi.org/10.1016/j.japh.2021.11.013
Palmer K, Monaco A, Kivipelto M et al (2020) The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res 32:1189–1194. https://doi.org/10.1007/s40520-020-01601-4
Gillam MH, Roughead E, Tavella R et al (2022) Impact of COVID-19 restrictions on pathology service utilisation. Intern Med J 52:42–48. https://doi.org/10.1111/imj.15501
De Filippo O, D’Ascenzo F, Angelini F et al (2020) Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 383:88–89. https://doi.org/10.1056/NEJMc2009166
Song H, Bergman A, Chen AT et al (2021) Disruptions in preventive care: mammograms during the COVID-19 pandemic. Health Serv Res 56:95–101. https://doi.org/10.1111/1475-6773.13596
Diegoli H, Magalhaes PSC, Martins SCO et al (2020) Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-1 era. Stroke 51:2315–2321. https://doi.org/10.1161/STROKEAHA.120.030481
Solomon MD, McNulty EJ, Rana JS et al (2020) The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 383:691–693. https://doi.org/10.1056/NEJMc2015630
ISTAT Impatto dell’epidemia COVID-19 sulla mortalità totale della popolazione residente. Anno 2020 e gennaio-aprile 2021. Available from: https://www.iss.it/documents/20126/0/Report_ISS_Istat_2021_10_giugno+%281%29.pdf/3df35cd3-edd5-56e1-5867-d274f5032fb5?t=1623336923282
Calderón-Larrañaga A, Vetrano DL, Onder G et al (2017) Assessing and measuring chronic multimorbidity in the older population: a proposal for its operationalization. J Gerontol A Biol Sci Med Sci 72:1417–1423. https://doi.org/10.1093/gerona/glw233
The Medicines utilisation monitoring centre. national report on medicines use in older adults in Italy. Year 2019. Rome: Italian Medicines Agency, 2021. Rome: Italian Medicines Agency, 2021. Available from: https://www.aifa.gov.it/documents/20142/1577699/OsMed_Farmaci_anziani_13.10.2021.pdf
The Medicines utilisation monitoring centre. national report on medicines use in Italy. Year 2020. Rome: Italian Medicines Agency, 2021. Available from: https://www.aifa.gov.it/en/-/rapporto-nazionale-osmed-2020-sull-uso-dei-farmaci-in-italia
WHO collaborating centre for drug statistics methodology, guidelines for ATC classification and DDD assignment 2020. Oslo, Norway, 2019.
Tosato M, Carfì A, Martis I, Pais C, Ciciarello F, Rota E, Tritto M, Salerno A, Zazzara MB, Martone AM, Paglionico A, Petricca L, Brandi V, Capalbo G, Picca A, Calvani R, Marzetti E, Landi F (2021) Gemelli Against COVID-19. Post-Acute Care Team. Prevalence and Predictors of Persistence of COVID-19 Symptoms in Older Adults: A Single-Center Study. J Am Med Dir Assoc https://doi.org/10.1016/j.jamda.2021.07.003
Palmieri L, Vanacore N, Donfrancesco C, Lo Noce C, Canevelli M, Punzo O, Raparelli V, Pezzotti P, Riccardo F, Bella A, Fabiani M, D'Ancona FP, Vaianella L, Tiple D, Colaizzo E, Palmer K, Rezza G, Piccioli A, Brusaferro S, Onder G (2020) Italian National Institute of Health COVID-19 Mortality Group. Clinical Characteristics of Hospitalized Individuals Dying With COVID-19 by Age Group in Italy. J Gerontol A Biol Sci Med Sci 75:1796–1800. https://doi.org/10.1093/gerona/glaa146
Hanff TC, Mohareb AM, Giri J et al (2020) Thrombosis in COVID-19. Am J Hematol 95:1578–1589. https://doi.org/10.1002/ajh.25982
Högberg LD, Vlahović-Palčevski V, Pereira C, Weist K, Monnet DL; ESAC-Net study group; ESAC-Net study group participants. (2021) Decrease in community antibiotic consumption during the COVID-19 pandemic, EU/EEA, 2020. Euro Surveill https://doi.org/10.2807/1560-7917.ES.2021.26.46.2101020.
Nicieza García ML, Pérez Solís P, Gómez de Oña C et al (2021) Antibiotic consumption in primary care in the adult population of Asturias during 2014–2020 period. Aten Primaria 54:102261. https://doi.org/10.1016/j.aprim.2021.102261
Peñalva G, Benavente RS, Pérez-Moreno MA et al (2021) Effect of the coronavirus disease 2019 pandemic on antibiotic use in primary care. Clin Microbiol Infect 27:1058–1060. https://doi.org/10.1016/j.cmi.2021.01.021
Buehrle DJ, Wagener MM, Nguyen MH et al (2021) Trends in outpatient antibiotic prescriptions in the united states during the COVID-19 pandemic in 2020. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2021.26114
Hirschtritt ME, Slama N, Sterling SA et al (2021) Psychotropic medication prescribing during the COVID-19 pandemic. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000027664
Chang AY, Cullen MR, Harrington RA et al (2021) The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med 289:450–462. https://doi.org/10.1111/joim.13184
Bhatt AS, Moscone A (2020) McElrath EE et al Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic: a multicenter tertiary care experience. J Am College Cardiol 76:280–288. https://doi.org/10.1016/j.jacc.2020.05.038
Willan J, King AJ, Hayes S et al (2020) Care of haematology patients in a COVID-19 epidemic. Br J Haematol 189:241–243. https://doi.org/10.1111/bjh.16620
Jeng Y, Chen FH, Jen GH, Chen HC, Yen AM, Chen CD, Kuo HW, Wang ST, Hsu CY (2021) Impact of COVID-19 pandemic on accessibility of Taiwanese medical care. Am J Manag Care 27:e330–e335. https://doi.org/10.37765/ajmc.2021.88698
https://www.aifa.gov.it/documents/20142/1030827/Nota%2096.pdf
Doggrell SA (2010) Adherence to medicines in the older-aged with chronic conditions. Drugs Aging 27:239–254
Acknowledgements
We would like to acknowledge IWGMUE, formed as follows: Italian Medicines Agency (Agenzia Italiana del Farmaco “AIFA”): Nicola Magrini, AC, Ivano Comessatti, Aurora Di Filippo, Andrea Fabrizi, Marco Fontanella, Filomena Fortinguerra, Ramon Frulio, Francesca Gallinella, Maria Alessandra Guerrizio, Mariarosaria Italiano, Marco Marinelli, Roberto Marini, Federica Milozzi, Serena Perna, AP, Linda Pierattini, Emanuela Pieroni, Giuliano Pistolesi, Filippo Pomponi, Matteo Sacconi, Daniela Settesoldi, Maurizio Trapanese, Giuseppe Traversa, FT, Saverio Antonio Vasta, and SZ. Istituto Superiore di Sanità (ISS): Silvio Brusaferro, RDC, II, GO, and Paola Ruggeri. Ministero della Salute: Claudia Biffoli, Rosaria Boldrini, and Chiara Brutti. Ministero dell’Economia e delle Finanze: Luciana Patrizi, Antonietta Cavallo, Sara Guerrini, and Marco Martino. Istituto di Ricerche Farmacologiche Mario Negri IRCCS: Alessandro Nobili, Luca Pasina, Carlotta Franchi, Mauro Tettamanti, and Alessio Novella. Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico di Milano: Pier Mannuccio Mannucci. Università di Bologna: Elisabetta Poluzzi. Università di Brescia: AM. Società Italiana di Medicina Interna (SIMI): Antonello Pietrangelo and Maria Lorenza Muiesan. Società Italiana di Medicina Generale e delle Cure Primarie (SIMG): Claudio Cricelli, Pierangelo Lora Aprile, Gerardo Medea, Ignazio Grattagliano, Raffaella Michieli, Damiano Parretti, Francesco Lapi, and Ettore Marconi.
Nicola Magrini, Ivano Comessatti, Aurora Di Filippo, Andrea Fabrizi, Marco Fontanella, Filomena Fortinguerra, Ramon Frulio, Francesca Gallinella, Maria Alessandra Guerrizio, Mariarosaria Italiano, Marco Marinelli, Roberto Marini, Federica Milozzi, Serena Perna, Linda Pierattini, Emanuela Pieroni, Giuliano Pistolesi, Filippo Pomponi, Matteo Sacconi, Daniela Settesoldi, Maurizio Trapanese, Giuseppe Traversa, Saverio Antonio Vasta, Silvio Brusaferro, Paola Ruggeri, Claudia Biffoli, Rosaria Boldrini, Chiara Brutti, Luciana Patrizi, Antonietta Cavallo, Sara Guerrini, Marco Martino, Alessandro Nobili, Luca Pasina, Carlotta Franchi, Mauro Tettamanti, Alessio Novella, Antonello Pietrangelo, Maria Lorenza Muiesan, Claudio Cricelli, Pierangelo Lora Aprile, Gerardo Medea, Ignazio Grattagliano, Raffaella Michieli, Damiano Parretti, Francesco Lapi, Ettore Marconi.
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
Drs Cangini and Trotta had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Drs Marengoni, Cangini, Zito, Onder, Trotta. Acquisition, analysis, or interpretation of data: Drs Cangini, Trotta, Zito, Pierantozzi. Drafting of the manuscript: Drs Marengoni, Cangini. Critical revision of the manuscript for important intellectual content: Drs Marengoni, Onder, Trotta, Cangini, Ippoliti, Zito, Pierantozzi, Da Cas.
Corresponding author
Ethics declarations
Conflict of interest
No disclosures were reported.
Statement of human and animal rights
Thia article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of formal consent is not required.
Disclaimer
The views expressed in this article are the personal views of the authors and may not be understood or quoted as being made on behalf of or reflecting the position of the respective authors’ organizations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marengoni, A., Cangini, A., Pierantozzi, A. et al. Impact of COVID-19 pandemic on medication use in the older Italian population. Aging Clin Exp Res 35, 443–453 (2023). https://doi.org/10.1007/s40520-022-02303-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02303-9