Abstract
Oral bisphosphonates are a key intervention in the treatment of osteoporosis and in reducing the risk of fragility fractures. Their use is supported by over 3 decades of evidence; however, patient adherence to oral bisphosphonates remains poor in part due to complex dosing instructions and adverse events, including upper gastrointestinal symptoms. This problem has led to the development of novel oral bisphosphonate formulations. Buffered, effervescent alendronate is dissolved in water and so seeks to reduce upper gastro-intestinal adverse events, and gastro-resistant risedronate aims to reduce the complexity of dosing procedure (e.g. fasting prior to consumption) whilst still maintaining the efficacy of fracture risk reduction. Clinical trials and real-world data have been employed to demonstrate some benefits in terms of reduced upper gastro-intestinal adverse events, adherence, persistence and health economic outcomes. This report describes the result of an ESCEO (European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis) expert working group, which explores where oral bisphosphonates sit in current clinical practice guidelines, review their risk–benefit profile and the consequences of poor adherence before exploring novel oral bisphosphonate formulations and their potential clinical and health economic impact. Further research is required but there are signs that these novel, oral bisphosphonate formulations may lead to improved tolerance of oral bisphosphonates and thus, improved adherence and fracture outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a highly prevalent condition affecting older men and women and predisposing to fragility fractures [1, 2]. Oral bisphosphonates have a rich heritage of use in the treatment of osteoporosis but adherence is affected, in large part, by adverse effects [3]. For this reason, new formulations of oral bisphosphonates including gastro-resistant risedronate and buffered alendronate have been produced to improve patient acceptability and an overview of these is potentially beneficial.
Bisphosphonates are pyrophosphate analogues containing a P–C–P bond. The degree of bisphosphonate potency depends on the side-chain length [4] and they have substantial affinity for hydroxyapatite leading to inhibition osteoclast recruitment, osteoclast activity with a subsequent reduction in bone resorption [5].
In this report we describe where oral bisphosphonates sit in current clinical practice guidelines, review their risk–benefit profile and the consequences of poor adherence before exploring the novel oral bisphosphonate formulations and their potential clinical and health economic impact.
Current clinical practice guidelines
Clinical practice guidelines are defined as “a statement developed systematically to help practitioners and patients make decisions about appropriate medical services” [6] and include recommendations for particular treatments based on review of the available literature at the time [7].
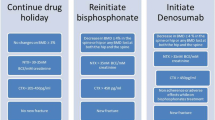
Using the above definition there are a number of clinical practice guidelines relevant to the use of oral bisphosphonates in the treatment of osteoporosis [8] which highlight three main situations when these therapies can be gainfully employed: a first-line therapy in confirmed osteoporosis, a subsequent treatment after bone-forming therapy, and a subsequent treatment after denosumab.
In the first of these use cases, European guidelines for postmenopausal osteoporosis advocate for treatment of high risk patients defined according to the country-specific 10-year fracture risk as calculated by the Fracture Risk Assessment Tool (FRAX®) (modulated by dual-energy X-ray absorptiometry (DXA), trabecular bone score, glucocorticoid therapy, falls history type 2 diabetes and hip axis length as available) or having sustained a fragility fracture of the spine or hip [5].
The exact usage of ‘high risk’ FRAX® thresholds varies across guidelines with the American Association of Clinical Endocrinology/American College of Endocrinology 2020 guidelines for postmenopausal osteoporosis recommending a threshold of 10 years major osteoporotic fracture risk of ≥ 20% or hip fracture risk of ≥ 3% [9].
Those patients at ‘very high risk’, defined as either above the upper assessment threshold on FRAX ® assessment [10, 11], or those with low bone mineral density (BMD) with advanced age, frailty, glucocorticoids, very low T scores or increased falls risk [9] are considered for bone-forming therapies first-line if these are available [9, 10].
In the second use case, anti-resorptive therapies, including oral bisphosphonates are used to ‘lock-in’ the benefits accrued from bone-forming therapies [12] and in the third case, they are used similarly to reduce the immediate, rebound fracture risk which occurs after discontinuing denosumab [5, 13].
In the majority of the cases above, an oral bisphosphonate should be used as first-line, with intravenous preparations and denosumab as alternatives if oral bisphosphonates are contraindicated or not tolerated [5, 9]. Treatment with oral bisphosphonates should be reviewed every 3–5 years [5] with the AACE/ACE recommending additional years (up to 5 years) of treatment to be considered if the fracture risk remains high at assessment [9].
Oral bisphosphonates form a cornerstone of osteoporosis therapy and their benefits are established; however, their risks need to be addressed, particularly when consenting patients for therapy.
Risk–benefit
Oral bisphosphonates have been available for the treatment of osteoporosis since the release of etidronate in the early 1990s [14, 15], alendronate in the mid-1990s [16, 17] and risedronate in the late-1990s [18,19,20] with risk reduction for radiographic vertebral fractures of 40–50% at 3–5 years compared to placebo and non-vertebral fracture risk reduction of 20–30%.
Oral bisphosphonates can be associated with mild, common adverse effects, including upper gastro-intestinal irritation which will be addressed later as they are relevant to the novel bisphosphate formulations; however, there are important, rare adverse events which require particular attention as they often arise in consultations when consenting a patient in clinic. These include osteonecrosis of the jaw, atypical femoral fractures and cardiovascular effects.
Osteonecrosis of the jaw is a rare condition defined by the presence of exposed, necrotic bone lesions which are present beyond 8 weeks and do not respond to appropriate therapy [21]. It occurs mainly in the mandible but the maxilla can also be affected and may occur in response to potent anti-resorptive therapy with the diagnosis excluded by the use of previous radiotherapy to the affected area. It is associated with poor oral hygiene, smoking, diabetes, concomitant glucocorticoid or chemotherapy, and invasive dental procedures (including dental extractions or implants) but even so, it has a small incidence rate of 1–90/100,000 patient-years [22, 23].
Atypical femoral fractures occur in the subtrochanteric and diaphyseal region of the femur and are associated with bisphosphonate usage [24]. The absolute risk of occurrence is low with incidence rates of 1.8/100,000 patient-years after 2 years of therapy, though the risk does rise with increasing length of treatment leading to 113/100,000 patient-years at 8–9.9 years of exposure to bisphosphonates [22, 24,25,26]. The risk of atypical fractures is outweighed by the benefit of anti-resorptive therapy as a study of 1.8 million patients demonstrated that, over a 5-year period, 162 fragility fractures of the spine, hip and forearm are saved for each atypical femoral fracture sustained [26].
The cardiovascular effects of bisphosphonates are debated, with data from animal studies (using higher dosages than used in human studies) suggesting potential cardiovascular protective effects due to reduced atherosclerosis in response to bisphosphonate therapy [27,28,29,30]. This is supported by a limited signal from a trial of risedronate which showed a protective effect of 2.5 mg dose for cardiovascular mortality (RR 0.69, 95% CI 0.49–0.99) and stroke mortality (RR 0.36, 95% CI 0.17–0.78), though this effect is caveated by the fact that there was no significant effect at the 5 mg dose or on the incidence of coronary artery disease [31]. Indeed, meta-analyses have shown no significant associations (either protective or adverse) between bisphosphonates and cardiovascular death, adverse cardiovascular outcomes, myocardial infarction or stroke [32] and this is echoed by long term, prospective database studies [33].
Consequences of poor adherence
The adherence to a medication is defined as the process by which patients take a medication. This can be divided into three phases; initiation, implementation and persistence [34, 35] and can be measured, for example, by the medication possession ratio (MPR, the number of days covered by treatment in a given period of time divided by the total number of days in that period) [36]. Forms of ‘non-adherence’ can, therefore, include non-initiation of treatment, errors in dosing (including missed doses or taking the medication incorrectly) and discontinuing the treatment [34, 35].
In terms of initiation, a study of over 75,000 patients found that between 20 and 30% did not initiate a prescribed medication [37]. This is particularly concerning given the established osteoporosis ‘Treatment Gap’ [38] with a Belgian study demonstrating that of over 23,000 patients sustaining a hip fracture, only 6% were commenced on anti-osteoporosis treatment within 1 year [39].
When considering the implementation phase, it is important to note that the majority of established bisphosphonates are ‘immediate-release’ formulations which have approximately 1% bioavailability as their absorption is limited by chelation with aluminium, magnesium and calcium cations [40]. For this reason, these immediate-release preparations require complex dosing instructions including taking them on a fasted stomach (to avoid chelation by foods containing the above cations), with water and up to 2 h of fasting after consumption (thus delaying breakfast), with strict instructions to remain upright (and not lie down) after consumption [41] and to be taken separately from other medications. These complexities affect adherence with an estimated 50% of patients not following the above recommendations [42].
A survey of 36 women aged ≥ 55 years taking immediate-release bisphosphonates found that 56.5% were non-adherence with dosing instructions, and further, that 40.5% were non-adherent with instructions related to improving absorption (e.g. fasting prior to dosing) and 34.7% were non-adherent with instructions related to adverse effects (e.g. remaining upright following dosing) [42].
Discontinuation of medication is common with rates up to 40% by 12 months for all medications [43] and as high as 85% by 3 years with anti-osteoporosis medications [39]. A systematic review of 89 real-world studies revealed a 12 months persistence range of 17.7—74.8% for oral bisphosphonates with a mean MPR of 28.2—84.5% over the same time period [44]. The determinants identified from this study included geographic residence, marital status, tobacco use, educational status, income, hospitalisation, medication type and dosing frequency [44]. A further systematic review of 10 studies specifically investigating adherence and persistence to bisphosphonate therapy in postmenopausal women and found a mean MPR range of 54–71% at 1 year and persistence ranged from 28 to 74% [45]. Though these ranges are large, the authors did note that adherence and persistence were higher in formulations which required less frequent dosing and fracture rates were significantly lower in women with higher adherence (particularly a MPR > 80%) [45]. This finding is supported by data from national claims database which found that the MPR of bisphosphates rose with increasing interval between prescribed doses (from daily to 3 monthly), though some of the included medications were intravenously delivered [46].
This poor adherence leads to suboptimal efficacy in terms of fracture risk reduction [47,48,49] and an increased financial burden to the health system [50, 51]. Healthcare professionals play a vital role in ensuring that correct dosing instructions are provided and, wherever possible, adhered to. Indeed, adherence can be monitored using bone turnover markers [52].
The determinants of poor adherence are manifold, and social (e.g. low health literacy), economic (e.g. lack of healthcare insurance), healthcare system (e.g. healthcare provider communication skills), condition-specific (e.g. the lack of symptoms of osteoporosis), therapy-specific (e.g. the lack of immediate, tangible medication benefit) and patient-related factors (e.g. visual impairment) all play a role [53].
Data from the ‘Screening in the community to reduce fractures in older women’ (SCOOP) trial showed that the FRAX® input characteristics which were significantly associated with improved adherence over 5 years of follow-up included younger age (OR 0.96, p = 0.01), parental fractured hip (OR 1.67, p < 0.01) and having a dual-energy X-ray absorptiometry (DXA) scan (OR 1.89, p < 0.01) [54]. Importantly, those in a higher FRAX® risk category were also significantly more adherent to anti-osteoporosis medications (OR 2.80, p = 0.02) [54].
Interventions which have strong evidence to support their usage in improving medication adherence (in osteoporosis and other conditions) include patient counselling, patient education in combination with counselling, adherence monitoring combined with counselling, reminders to take medication and dose simplification including flexibility of dosing regimens [53]. From a fairly broad literature, this represents a small proportion of possible interventions with the majority showing little or no improvement [53], but it does appear that multicomponent interventions which incorporate patient education have the most marked beneficial effects [55].
The key steps to improving adherence include understanding the problem at hand (initiation, implementation or persistence), accurately measuring adherence and robustly identifying the reasons for non-adherence so that they can be addressed [53]. In addition, there have been therapeutic developments with novel oral bisphosphonates, which aim to reduce the therapy-specific factors impairing adherence.
Novel formulations
Novel formulations which overcome the complexities of drug delivery have been developed including buffered alendronate and gastro-resistant risedronate.
Buffered alendronate
Upper gastro-intestinal adverse effects are a substantial adverse effect when using bisphosphonates for the treatment of osteoporosis [56]. Indeed, in an acidic environment (with a pH < 3) alendronate is in a free acidic form which is far more irritant to the gastro-oesophageal mucosa than the sodium salt (alendronate sodium) form [57].
A possible solution for the problem is novel, effervescent alendronate which aims to improve tolerability by dissolving the active alendronate in a buffered solution with pH 4.8–5.4 (taken in at least 120 ml of water) [58] to reduce gastro-oesophageal irritation.
A prospective, observational, post-authorisation study in Italy and Spain examined the performance of a form of buffered alendronate (Binosto®) focusing on key outcomes of adverse events, medication errors, persistence and compliance, in a group of post-menopausal females (intention to treat n = 1084, safety cohort n = 1028, completed n = 873) over a 12-month period [59].
The mean age of participants was 67 years and just over a third (36%) had sustained a fracture previously. History of Gastrointestinal symptoms were observed in 31% (n = 319) participants and, of these, 85% (n = 271) were upper gastrointestinal. The cumulative incidence of all upper gastro-intestinal adverse events was 12.7%, with 9.6% specifically related to the effervescent, buffered alendronate (8% mild, 1.5% moderate, 0.2% severe but none of these adverse events were graded as serious) [59].
In terms of the specific symptoms or pathologies associated with these adverse effects the incidence rate was highest for nausea (IR = 2.1, 95% CI 1.4–3.2) followed by abdominal pain (IR = 1.2, 95% CI 0.6–2.1) and gastritis (IR = 0.8, 95% CI 0.4–1.6) with no reported gastric stenosis, ulceration, perforation or haemorrhage [59].
Medication errors were recorded in 30% of participants (n = 307) including not waiting a sufficient time before consuming the first meal (10%), using a liquid other than water to dissolve the effervescent alendronate (9%) and an insufficient volume of water (< 30 ml) drunk following the consumption of the medication (7.6%) [59].
Approximately 80% of participants continued the effervescent alendronate through the duration of follow-up with the most common cause of discontinuation labelled as “patient decision” in 42.6% (n = 89) of those who discontinued [59]. Persistence rates were therefore higher than that reported in bisphosphonates in a similar study in which 71.3% participants were taking a bisphosphonate at 6 months of follow-up.
The percentage of upper gastro-intestinal adverse events related to the effervescent alendronate (9.6%) was lower than those reported in studies of alendronate in populations of post-menopausal women which include 30% in the Fracture Intervention Trial [60] and above 20% in the Fosamax International Trial Study [61] and other early studies of alendronate [62, 63].
Real-world data on effervescent alendronate comes from a clinical database study by Giusti and colleagues, which recruited postmenopausal women with osteoporosis (T ≤ − 2.5 or T ≤ 2.0 with a vertebral fracture) comparing effervescent alendronate (n = 144) to conventional alendronate (n = 216) [64]. Persistence was measured and was found to be significantly higher in the effervescent group at 6 months (91 vs 75%, p < 0.01) and 12 months (81 vs 69%, p = 0.009). Discontinuation due to upper gastro-intestinal adverse events was significantly lower in the effervescent group (4 vs 11%, p = 0.027) as was discontinuation due to patient decision (6 vs 13%, p = 0.016). The findings of this study are from a single area in North–West Italy and did not include adherence data; however, they suggest that the real-world experience of effervescent alendronate may be favourable for upper gastro-intestinal adverse events and persistence rates.
One of the current issues regarding the widespread usage of effervescent alendronate is that it is currently available in a relatively small number of countries, though work is ongoing to broaden the geographic scope of supply.
Gastro-resistant risedronate
Gastro-resistant risedronate is coated with a gastro-resistant, ethylenediaminetetraacetic acid (EDTA) coating which acts as a food stabiliser and calcium chelator and means that it bypasses the oesophagus and stomach [41] prior to tablet disintegration more distally in the gastro-intestinal tract [65]. This eliminates the need for pre-consumption fasting and therefore allows more ‘user-friendly’ instructions for drug consumption and provides potentially better drug absorption regardless of prior food intake (or fasting status) [41, 66].
Gastro-resistant risedronate taken before (n = 308) and after (n = 307) breakfast was compared to immediate-release risedronate (n = 307) and was found to perform similarly in all three groups with regard to efficacy (percentage change in lumbar spine BMD) and safety outcomes and approximately 80% of participants completed the initial 12 months of a non-inferiority study [67]. When this study was extended to 2 years comparable increases in BMD were observed across all three groups but significantly greater CTX decreases were observed in the gastro-resistant treatment cohort [66]. There were no significant differences in incident vertebral fractures (gastro-resistant risedronate before breakfast = 6, gastro-resistant risedronate after breakfast = 2 and immediate-release risedronate = 2). Medication completion rates were similar (gastro-resistant risedronate before breakfast 76.2%, gastro-resistant risedronate after breakfast 77.2% and immediate-release risedronate 80.8%) but rates of upper abdominal pain adverse events were higher in the gastro-resistant risedronate before breakfast group (gastro-resistant risedronate before breakfast 7.5%, gastro-resistant risedronate after breakfast 2.9% and immediate-release risedronate 2.3%).
Beyond randomized controlled trials, real-world studies have provided insights regarding safety and efficacy. A study of women in the IBM MarketScan Commercial and Medicine Supplemental databases (spanning 10 years from 2009 to 2019) used a retrospective, observational design to compare gastro-resistant risedronate to all other oral bisphosphonates [36]. Patients were matched for ages, year of index bisphosphonate administration, insurance plan type, region, comorbidity index, fracture and use of drugs affecting BMD.
Drug adherence was measured with persistence defined as the time from initiation to the end of treatment, discontinuation was defined as a treatment gap of ≥ 90 consecutive days and adherence was measured according to the MPR.
Over more than 50 months of observation, 16,737 women took gastro-resistant risedronate and 1,348,153 took other oral bisphosphonates (66.3% alendronate, 20.2% ibandronate, 13.5% immediate-release risedronate) leading to matched groups containing 2726 patients with a median age of 60.0 years and 1.7% were diagnosed with a fracture during the baseline study period.
The prescription of gastro-resistant risedronate led to a 17% reduction in overall risk of fracture (incidence rates per 1000 patient-years 34.65 on gastro-resistant risedronate vs 42.13 on other oral bisphosphonates, p < 0.05) and a 29% reduction in the risk of spinal fracture (incidence rates per 1000 patient-years 10.84 on gastro-resistant risedronate vs 15.13 on other oral bisphosphonates, p < 0.05). This benefit in fracture rate was seen numerically over time, though was only significant at 36 months (7.08% on gastro-resistant risedronate vs 8.67% on other oral bisphosphonates, p < 0.05).
When compared to the most common oral bisphosphonate (alendronate), those initiated on gastro-resistant risedronate had a 19% lower risk of any fracture and a 31% lower risk of spinal fracture.
Persistence on treatment was generally poor with the majority of patients discontinuing their index treatment within 2 years of initiation (80.5% discontinuation rate of gastro-resistant risedronate, 74.4% discontinuation rate of other bisphosphonates over 2 years) though persistence was lower for gastro-resistant risedronate particularly due to high rates of discontinuation within the first months of commencing therapy. These results are within the spectrum of mean persistence for bisphosphonates recorded from prospective and retrospective observational studies with 2 years mean persistence rates of 12.9–60.6% and mean compliance of 34.5–47.9% over the same time period [44].
In a further US claims database analysis comparing gastro-resistant risedronate with immediate-release risedronate and alendronate, the gastro-resistant preparation was associated with a lower rate of fracture in women with osteoporosis [68]. This was observed in subgroup analyses for those aged ≥ 65 years (incidence risk ratio (IRR) 0.63 (95% CI 0.46–0.86) for any fracture, IRR 0.41 (95% CI 0.18–0.93) for pelvic fracture), those aged ≥ 70 years (IRR 0.63 (95% CI 0.50–0.96) for any fracture, IRR 0.24 (95% CI 0.08–0.68) for pelvic fracture) and in a ‘high-risk’ population with older age, comorbidity and using medications which increase fracture risk (IRR 0.36 (95% CI 0.16–0.82) for pelvic fracture). In this study, the discontinuation rate for bisphosphonates was 40% within 1 year. Although limited by a young population (due to the nature of the database) and the use of a coded diagnoses, this study suggests potential benefits, in terms of fracture protection, of gastro-resistant risedronate compared to commonly used immediate-release preparations.
Economic benefits of new formulations
Both buffered, effervescent alendronate and gastro-resistant risedronate have the potential to improve adherence which can lead to reduced fractures and improved health outcomes and reduced costs associated with fractures. However, these novel preparations are more expensive than the standard formulations which will increase costs, and increased adherence will also lead to an increase in drug costs.
The economic value of a drug is typically assessed using a cost-effectiveness analysis which aims to answer the question “Is the intervention worth the price?”. The result of a cost-effectiveness analysis is expressed using the incremental cost effectiveness ratio (ICER), a measure of the difference between an intervention and comparator calculated as the total cost divided by the difference between the intervention and comparator in terms of Quality Adjusted Life Years (QALY, equivalent to 1 year lived in perfect health). The ICER is measured against a threshold for cost–effectiveness, which can be estimated as a multiple of GDP per capita.
When considering the wider utility of these novel formations of bisphosphonates health economic analyses should be conducted in line with the ESCEO-IOF recommendations [69] to ensure that decision-makers and policy-makers are adequately informed of the economic impact of introducing these novel formulations so that the most cost-effective interventions can be identified and healthcare resources allotted accordingly.
The cost-effectiveness of effervescent alendronate was assessed using a Markov microsimulation model adjusted to the Italian healthcare system (using fracture data from 2017 discharge summaries) and incorporating the costs and consequences of fracture events over a lifetime of women up to the age of 100 years (or death) [70]. Effervescent alendronate was compared to alendronate, denosumab, zoledronate and no treatment. Participants were aged 60–80 years and had T-scores ≤ − 3.0 or an existing vertebral fracture. Persistence data provided 12 months of follow-up with the model extended to 3 years to better reflect clinical practice [70].
The economic analysis demonstrated that effervescent alendronate was cost-effective compared to all comparators for postmenopausal women ≥ 60 years in Italy. In subgroup analyses, effervescent alendronate was dominant (indicating more QALYs for lower total costs) for cost-effectiveness over denosumab at 1 and 3 years for both low BMD and vertebral fracture groups, over alendronate at 1 and 3 years for the low BMD group ≥ 65 years and the fracture group ≥ 75 years and cost-saving compared to no treatment at 1 and 3 years for the low BMD group ≥ 65 years and the fracture group ≥ 75 years. Effervescent alendronate was dominant over zoledronate at 3 years but not at 1 year as it was assumed that persistence for zoledronate over 1 year would be 100% [70]. However, even at 1 year the ICER was below € 20,000 (€ 2019) per QALY. The persistence data for this Italian model was taken from the 12-month study by Giusti and colleagues [64] and extrapolated to 3 years which could be a limitation, however, the model conservatively assumed similar rates of adverse effects from effervescent alendronate compared to conventional alendronate.
Similar Markov model, microsimulation methods were used for a study of the cost-effectiveness of gastro-resistant risedronate in a French population of postmenopausal women aged 60–80 years with BMD T-scores ≤ − 2.5 with or without vertebral fractures [47]. In this case, efficacy data were taken from a previous meta-analysis and persistence data drawn from an Australian longitudinal study (as no French data for persistence on gastro-resistant risedronate were available).
This found that gastro-resistance risedronate was cost-effective compared with alendronate, generic risedronate and no treatment, in a French population of postmenopausal women [47]. Cost-effectiveness improved with increasing age and with increasing risk of fracture at baseline.
In subgroup analyses, gastro-resistant risedronate was dominant over immediate-release risedronate and alendronate in those ≥ 75 years and cost saving compared to no treatment in those ≥ 70 years [47].
The cost-effectiveness of gastro-resistant risedronate is supported by the findings of a US, healthcare resource utilization study of claims data which demonstrated a significantly lower number of hospital in-patient stays for patients on gastro-resistant risedronate compared to other oral bisphosphonates (IRR 0.86, 95% CI 0.76–0.97) and subsequently lower costs for in-patient healthcare utilization ($993 per patient per year lower, p < 0.05) [36]. However, there was no significant difference for emergency department, out-patient or ambulatory costs and pharmacy costs were higher for gastro-resistant risedronate compared to other oral bisphosphonates ($680 per patient per year higher). Indeed costs, in particular out-of-pocket costs, were considered to be a likely cause for patient discontinuation of gastro-resistant risedronate, as the mean cost of a 28–30-day supply was $ 42.39 for gastro-resistant risedronate compared to $10.72 for other bisphosphonates [36].
These economic analyses highlight the potential health economic benefits of novel bisphosphonate formulations; however, further work in other populations would assist in supporting these findings.
Conclusions
Oral bisphosphonates play a key role in the treatment of osteoporosis and the amelioration of fracture risk. They are, however, hampered by adverse events, particularly affecting the upper gastro-intestinal tract, which reduce patient adherence and persistence. Effervescent alendronate and gastro-resistant risedronate seek to improve adherence by simplifying the complex dosing rigmarole and reducing upper gastro-intestinal adverse events. Data from trials and real-world data are encouraging with regard to the benefits of these medications both clinically and from a health economic perspective. Further research across diverse populations and focusing on fracture outcomes will strengthen the body of evidence around these formulations.
Change history
31 December 2022
In the published article, the author would like to update the following lines History of Gastrointestinal symptoms were observed in 31% (n=319) participants and, of these, 85% (n =271) were upper gastrointestinal
03 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40520-022-02319-1
References
Kaufman JM (2021) Management of osteoporosis in older men. Aging Clin Exp Res 33:1439–1452. https://doi.org/10.1007/s40520-021-01845-8
Barnsley J, Buckland G, Chan PE et al (2021) Pathophysiology and treatment of osteoporosis: challenges for clinical practice in older people. Aging Clin Exp Res 33:759–773. https://doi.org/10.1007/s40520-021-01817-y
Blanch J, González E, Valdés C et al (2016) Medical professionals’ perceptions regarding therapeutic adherence in patients with osteoporosis. Rev Osteoporos Metab Miner 8:15–23. https://doi.org/10.4321/S1889-836X2016000100003
Rizzoli R (2011) Bisphosphonates for post-menopausal osteoporosis: are they all the same? QJM 104:281–300. https://doi.org/10.1093/qjmed/hcq259
Kanis JA, Cooper C, Rizzoli R et al (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44. https://doi.org/10.1007/s00198-018-4704-5
Institute of Medicine Committee to Advise the Public Health Service on Clinical Practice G (1990) In: Field MJ and Lohr KN (eds) Clinical Practice Guidelines: Directions for a New Program. Washington (DC): National Academies Press (US) Copyright © National Academy of Sciences
Institute of Medicine Committee on Standards for Developing Trustworthy Clinical Practice G (2011) In: Graham R, Mancher M, Miller Wolman D, et al. (eds) Clinical Practice Guidelines We Can Trust. Washington (DC): National Academies Press (US) Copyright 2011 by the National Academy of Sciences. All rights reserved
De Vincentis A, Behr AU, Bellelli G et al (2021) Orthogeriatric co-management for the care of older subjects with hip fracture: recommendations from an Italian intersociety consensus. Aging Clin Exp Res 33:2405–2443. https://doi.org/10.1007/s40520-021-01898-9
Camacho PM, Petak SM, Binkley N et al (2020) American association of clinical endocrinologists/American college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis- 2020 update executive summary. Endocr Pract 26:564–570. https://doi.org/10.4158/gl-2020-0524
Kanis JA, Harvey NC, McCloskey E et al (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31:1–12. https://doi.org/10.1007/s00198-019-05176-3
Curtis EM, Reginster JY, Al-Daghri N et al (2022) Management of patients at very high risk of osteoporotic fractures through sequential treatments. Aging Clin Exp Res 34:695–714. https://doi.org/10.1007/s40520-022-02100-4
Saag KG, Petersen J, Brandi ML et al (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377:1417–1427. https://doi.org/10.1056/NEJMoa1708322
Kondo H, Okimoto N, Yoshioka T et al (2020) Zoledronic acid sequential therapy could avoid disadvantages due to the discontinuation of less than 3-year denosumab treatment. J Bone Miner Metab 38:894–902. https://doi.org/10.1007/s00774-020-01126-w
Storm T, Thamsborg G, Steiniche T et al (1990) Effect of intermittent cyclical etidronate therapy on bone mass and fracture rate in women with postmenopausal osteoporosis. N Engl J Med 322:1265–1271. https://doi.org/10.1056/nejm199005033221803
Watts NB, Harris ST, Genant HK et al (1990) Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med 323:73–79. https://doi.org/10.1056/nejm199007123230201
Black DM, Cummings SR, Karpf DB et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541. https://doi.org/10.1016/s0140-6736(96)07088-2
Cummings SR, Black DM, Thompson DE et al (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 280:2077–2082. https://doi.org/10.1001/jama.280.24.2077
Harris ST, Watts NB, Genant HK et al (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA 282:1344–1352. https://doi.org/10.1001/jama.282.14.1344
Reginster J, Minne HW, Sorensen OH et al (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91. https://doi.org/10.1007/s001980050010
McClung MR, Geusens P, Miller PD et al (2001) Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 344:333–340. https://doi.org/10.1056/nejm200102013440503
Anastasilakis AD, Pepe J, Napoli N et al (2022) Osteonecrosis of the jaw and antiresorptive agents in benign and malignant diseases: a critical review organized by the ECTS. J Clin Endocrinol Metab 107:1441–1460. https://doi.org/10.1210/clinem/dgab888
Adler RA, El-Hajj Fuleihan G, Bauer DC et al (2016) Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the American society for bone and mineral research. J Bone Miner Res 31:16–35. https://doi.org/10.1002/jbmr.2708
Khan A, Morrison A, Cheung A et al (2016) Osteonecrosis of the jaw (ONJ): diagnosis and management in 2015. Osteoporos Int 27:853–859. https://doi.org/10.1007/s00198-015-3335-3
Rizzoli R, Akesson K, Bouxsein M et al (2011) Subtrochanteric fractures after long-term treatment with bisphosphonates: a European society on clinical and economic aspects of osteoporosis and osteoarthritis, and international osteoporosis foundation working group report. Osteoporos Int 22:373–390. https://doi.org/10.1007/s00198-010-1453-5
Shane E, Burr D, Abrahamsen B et al (2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29:1–23. https://doi.org/10.1002/jbmr.1998
Dell RM, Adams AL, Greene DF et al (2012) Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 27:2544–2550. https://doi.org/10.1002/jbmr.1719
McFarlane SI, Muniyappa R, Shin JJ et al (2004) Osteoporosis and cardiovascular disease: brittle bones and boned arteries, is there a link? Endocrine 23:1–10. https://doi.org/10.1385/ENDO:23:1:01
Bevilacqua M, Dominguez LJ, Rosini S et al (2005) Bisphosphonates and atherosclerosis: why? Lupus 14:773–779. https://doi.org/10.1191/0961203305lu2219oa
Wagner WD, Clarkson TB, Foster J (1977) Contrasting effects of ethane-1-hydroxy-1,1-diphosphonate (EHDP) on the regression of two types of dietary-induced atherosclerosis. Atherosclerosis 27:419–435. https://doi.org/10.1016/0021-9150(77)90161-7
Kramsch DM, Aspen AJ, Rozler LJ (1981) Atherosclerosis: prevention by agents not affecting abnormal levels of blood lipids. Science (New York, NY) 213:1511–1512. https://doi.org/10.1126/science.6792706
Steinbuch M, D’Agostino RB, Mandel JS et al (2002) Assessment of mortality in patients enrolled in a risedronate clinical trial program: a retrospective cohort study. Regul Toxicol Pharmacol 35:320–326. https://doi.org/10.1006/rtph.2002.1550
Kim DH, Rogers JR, Fulchino LA et al (2015) Bisphosphonates and risk of cardiovascular events: a meta-analysis. PLoS ONE 10:e0122646. https://doi.org/10.1371/journal.pone.0122646
Bunch TJ, Anderson JL, May HT et al (2009) Relation of bisphosphonate therapies and risk of developing atrial fibrillation. Am J Cardiol 103:824–828. https://doi.org/10.1016/j.amjcard.2008.11.037
De Geest S, Zullig LL, Dunbar-Jacob J et al (2018) ESPACOMP medication adherence reporting guideline (EMERGE). Ann Intern Med 169:30–35. https://doi.org/10.7326/m18-0543
Vrijens B, De Geest S, Hughes DA et al (2012) A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73:691–705. https://doi.org/10.1111/j.1365-2125.2012.04167.x
Thomasius F, Palacios S, Alam A et al (2022) Fracture rates and economic outcomes in patients with osteoporosis prescribed risedronate gastro-resistant versus other oral bisphosphonates: a claims data analysis. Osteoporos Int 33:217–228. https://doi.org/10.1007/s00198-021-06108-w
Fischer MA, Stedman MR, Lii J et al (2010) Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med 25:284–290. https://doi.org/10.1007/s11606-010-1253-9
Harvey NC, McCloskey EV, Mitchell PJ et al (2017) Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int 28:1507–1529. https://doi.org/10.1007/s00198-016-3894-y
Rabenda V, Vanoverloop J, Fabri V et al (2008) Low incidence of anti-osteoporosis treatment after hip fracture. J Bone Jt Surg Am 90:2142–2148. https://doi.org/10.2106/jbjs.G.00864
Lin JH (1996) Bisphosphonates: a review of their pharmacokinetic properties. Bone 18:75–85. https://doi.org/10.1016/8756-3282(95)00445-9
Pazianas M, Abrahamsen B, Ferrari S et al (2013) Eliminating the need for fasting with oral administration of bisphosphonates. Ther Clin Risk Manag 9:395–402. https://doi.org/10.2147/tcrm.S52291
Vytrisalova M, Touskova T, Ladova K et al (2015) Adherence to oral bisphosphonates: 30 more minutes in dosing instructions matter. Climacteric 18:608–616. https://doi.org/10.3109/13697137.2014.995164
Blaschke TF, Osterberg L, Vrijens B et al (2012) Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol 52:275–301. https://doi.org/10.1146/annurev-pharmtox-011711-113247
Fatoye F, Smith P, Gebrye T et al (2019) Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open 9:e027049. https://doi.org/10.1136/bmjopen-2018-027049
Fardellone P, Lello S, Cano A et al (2019) Real-world adherence and persistence with bisphosphonate therapy in postmenopausal women: a systematic review. Clin Ther 41:1576–1588. https://doi.org/10.1016/j.clinthera.2019.05.001
Lee H, Lee S, Kim D et al (2021) Effect of dosing interval on compliance of osteoporosis patients on bisphosphonate therapy: observational study using nationwide insurance claims data. J Clin Med. https://doi.org/10.3390/jcm10194350
Hiligsmann M, Reginster JY (2019) Cost-effectiveness of gastro-resistant risedronate tablets for the treatment of postmenopausal women with osteoporosis in France. Osteoporos Int 30:649–658. https://doi.org/10.1007/s00198-018-04821-7
Adachi J, Lynch N, Middelhoven H et al (2007) The association between compliance and persistence with bisphosphonate therapy and fracture risk: a review. BMC Musculoskelet Disord 8:97. https://doi.org/10.1186/1471-2474-8-97
Siris ES, Fan CS, Yang X et al (2016) Association between gastrointestinal events and compliance with osteoporosis therapy. Bone Rep 4:5–10. https://doi.org/10.1016/j.bonr.2015.10.006
Weycker D, Li X, Barron R et al (2016) Hospitalizations for osteoporosis-related fractures: Economic costs and clinical outcomes. Bone Rep 5:186–191. https://doi.org/10.1016/j.bonr.2016.07.005
Cutler RL, Fernandez-Llimos F, Frommer M et al (2018) Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open 8:e016982. https://doi.org/10.1136/bmjopen-2017-016982
Lorentzon M, Branco J, Brandi ML et al (2019) Algorithm for the use of biochemical markers of bone turnover in the diagnosis, assessment and follow-up of treatment for osteoporosis. Adv Ther 36:2811–2824. https://doi.org/10.1007/s12325-019-01063-9
Hiligsmann M, Cornelissen D, Vrijens B et al (2019) Determinants, consequences and potential solutions to poor adherence to anti-osteoporosis treatment: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Osteoporosis Foundation (IOF). Osteoporos Int 30:2155–2165. https://doi.org/10.1007/s00198-019-05104-5
Parsons CM, Harvey N, Shepstone L et al (2020) Systematic screening using FRAX(®) leads to increased use of, and adherence to, anti-osteoporosis medications: an analysis of the UK SCOOP trial. Osteoporos Int 31:67–75. https://doi.org/10.1007/s00198-019-05142-z
Cornelissen D, de Kunder S, Si L et al (2020) Interventions to improve adherence to anti-osteoporosis medications: an updated systematic review. Osteoporos Int 31:1645–1669. https://doi.org/10.1007/s00198-020-05378-0
Invernizzi M, Cisari C, Carda S (2015) The potential impact of new effervescent alendronate formulation on compliance and persistence in osteoporosis treatment. Aging Clin Exp Res 27:107–113. https://doi.org/10.1007/s40520-014-0256-5
Peter CP, Handt LK, Smith SM (1998) Esophageal irritation due to alendronate sodium tablets: possible mechanisms. Dig Dis Sci 43:1998–2002. https://doi.org/10.1023/a:1018894827961
EMC (2022) Binosto 70 mg effervescent tablets: patient information leaflet (PIL), https://www.medicines.org.uk/emc/product/7113/pil#gref. Accessed 31 July 2022
Minisola S, Vargas AP, Letizia Mauro G et al (2021) A prospective open-label observational study of a buffered soluble 70 mg alendronate effervescent tablet on upper gastrointestinal safety and medication errors: the GastroPASS study. JBMR Plus 5:e10510. https://doi.org/10.1002/jbm4.10510
Bauer DC, Black D, Ensrud K et al (2000) Upper gastrointestinal tract safety profile of alendronate: the fracture intervention trial. Arch Intern Med 160:517–525. https://doi.org/10.1001/archinte.160.4.517
Pols HA, Felsenberg D, Hanley DA et al (1999) Multinational, placebo-controlled, randomized trial of the effects of alendronate on bone density and fracture risk in postmenopausal women with low bone mass: results of the FOSIT study. Fosamax International Trial Study Group. Osteoporos Int 9:461–468. https://doi.org/10.1007/pl00004171
Rosen CJ, Hochberg MC, Bonnick SL et al (2005) Treatment with once-weekly alendronate 70 mg compared with once-weekly risedronate 35 mg in women with postmenopausal osteoporosis: a randomized double-blind study. J Bone Miner Res 20:141–151. https://doi.org/10.1359/jbmr.040920
Schnitzer T, Bone HG, Crepaldi G et al (2000) Therapeutic equivalence of alendronate 70 mg once-weekly and alendronate 10 mg daily in the treatment of osteoporosis. Alendronate Once-Weekly Study Group. Aging (Milano) 12:1–12
Giusti A, Bianchi G, Barone A et al (2021) A novel effervescent formulation of oral weekly alendronate (70 mg) improves persistence compared to alendronate tablets in post-menopausal women with osteoporosis. Aging Clin Exp Res 33:2529–2537. https://doi.org/10.1007/s40520-020-01777-9
Kleinermans D, Joyson A, Wray H (2022) An open-label randomized study of the relative absorption of gastro-resistant risedronate taken fasted or with food versus immediate-release risedronate. Pharmacol Res Perspect 10:e00957. https://doi.org/10.1002/prp2.957
McClung MR, Balske A, Burgio DE et al (2013) Treatment of postmenopausal osteoporosis with delayed-release risedronate 35 mg weekly for 2 years. Osteoporos Int 24:301–310. https://doi.org/10.1007/s00198-012-2175-7
McClung MR, Miller PD, Brown JP et al (2012) Efficacy and safety of a novel delayed-release risedronate 35 mg once-a-week tablet. Osteoporos Int 23:267–276. https://doi.org/10.1007/s00198-011-1791-y
Casado E, Palacios S, Thomasius F et al (2022) Not all oral bisphosphonates are equal: risedronate gastro-resistant is more effective than oral alendronate at reducing fractures and lowering healthcare cost. J Bone Miner Res 37:186–187
Hiligsmann M, Reginster JY, Tosteson ANA et al (2019) Recommendations for the conduct of economic evaluations in osteoporosis: outcomes of an experts’ consensus meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the US branch of the International Osteoporosis Foundation. Osteoporos Int 30:45–57. https://doi.org/10.1007/s00198-018-4744-x
Hiligsmann M, Maggi S, Veronese N et al (2021) Cost-effectiveness of buffered soluble alendronate 70 mg effervescent tablet for the treatment of postmenopausal women with osteoporosis in Italy. Osteoporos Int 32:595–606. https://doi.org/10.1007/s00198-020-05802-5
Funding
The ESCEO Working Group was funded by the ESCEO. The ESCEO receives unrestricted educational grants to support its educational and scientific activities from non-governmental organizations, not-for-profit organizations, non-commercial or corporate partners.
Author information
Authors and Affiliations
Contributions
All authors contributed to the review conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
NRF, NA-D, OBo, JB, ECav, MdW, PH, NCH, JMK, AK, RM, SMi, SP, JAK, RR, CC have no conflicts of interest to declare. OBr reports consulting or lecture fees for Amgen, Aptissen, Biophytis, IBSA, MEDA, Mylan, Novartis, Sanofi, TRB Chemedica, UCB, Viatris outside this manuscript. ECas reports Advisory Board participation and lecture fees for Theramex. BC reports Advisory Board participation and lecture fees for Theramex and Advisory Board participation for Expanscience. AG reports consulting and lecture fees from Abiogen Pharma, Theramex, and Bruno. MH has received research grants through institution from Radius Health, Amgen and ViiV Healthcare, lecture fees from Teva and Mylan Pharmaceuticals and consulting fees from UCB. SMa has received grants from Sanofi, MSD, GSK, Pfizer and Viatris outside of the submitted work. RPR has received fees for lectures or scientific advisory boards from Abiogen, Danone, Echolight, European Milk Forum, ObsEva, Pfizer Consumer Health and Theramex. FT reports Advisory Board participation and lecture fees for Theramex. NV reports personal fees from IBSA, Mylan, Viatris, Fidia, MSD outside of the submitted work. JYR reports consulting fees or paid advisory boards for IBSA-Genevrier, Mylan, Radius Health, Pierre Fabre, Faes Pharma, Rejuvenate Biomed, Samumed, Teva, Theramex, Pfizer, Mithra Pharmaceutical; lecture fees when speaking at the invitation of sponsor for IBSA-Genevrier, Mylan, CNIEL, Dairy Research Council (DRC), Nutricia, Danone, Agnovos and grant support (through institution) from IBSA-Genevrier, Mylan, CNIEL, Radius Health, TRB.
Informed consent
For this retrospective review, formal consent is not required.
Content to participants
The choice of topics, participants, content and agenda of the Working Groups as well as the writing, editing, submission and reviewing of the manuscript are the sole responsibility of the ESCEO, without any influence from third parties.
Human/animal rights
This article is a retrospective review. To the authors’ knowledge, the reviewed studies were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fuggle, N., Al-Daghri, N., Bock, O. et al. Novel formulations of oral bisphosphonates in the treatment of osteoporosis. Aging Clin Exp Res 34, 2625–2634 (2022). https://doi.org/10.1007/s40520-022-02272-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02272-z