Abstract
Background
Active mobility index (AMI) is a questionnaire to assess going-out behavior with physical and social activity. The association between AMI scores and objectively measured physical activity (PA) in older adults is unknown.
Methods
Community-dwelling older adults aged ≥ 70 years participated in an examination and wore a triaxial accelerometer for seven or more days. The accelerometer measured the time of moderate-to-vigorous intensity PA (MVPA) and light intensity PA (LPA), and step counts. The AMI assessed life space (distance from the respondent’s home: < 1, 1–10, or > 10 km) and related activities during the previous month. The AMI total, physical, and social scores were calculated.
Results
The analyzed data were 2499 participants (mean age: 75.5 ± 4.0 years; 54.4% female). Comparing PA among quartile groups of each AMI score, higher AMI total and physical score groups were associated with higher MVPA, LPA, and step counts (all P < 0.01). The Q4 group of AMI social scores showed significantly higher LPA and step counts than the Q1 and Q2 groups (P < 0.01). The logistic regression model showed higher score groups of AMI total and physical scores associated with increased adjusted odds ratio (aOR) of meeting recommended PA, ≥ 150 min/week of MVPA.
Conclusions
Older adults with higher AMI total and physical scores, engaged in more PA. Future studies can use the present findings when estimating PA in older adults from AMI scores and examining the association between AMI scores and health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Life space is regarded as an important factor in older adult’s health [1]. Extensive research has reported that life space predicts health outcomes, including cognitive decline, falls, mortality, and quality of life [1]. To assess life space and related activities simultaneously, a previous study developed an active mobility index (AMI) which includes a questionnaire to evaluate life space with physical activity (PA) and social activity [2]. In a longitudinal study, higher AMI total and physical scores were associated with a reduced risk of disability onset [2].
The linkage between life space and health in order adults has been partly explained by PA. Maintenance of PA contributes to the prevention of chronic diseases or functional decline [3,4,5] and a larger life space is associated with greater engagement in PA [6, 7]. A longitudinal study using an accelerometer found that lower step counts and less time spent in moderate activity at baseline were prospectively associated with a reduced life-space mobility score over 2 years [7]. A cross-sectional study showed that older adults who moved beyond the neighborhood more frequently were inclined to engage in longer moderate-and low-intensity PA [6]. However, the association between AMI and the amount of PA is unknown. To examine the mechanism of the link between AMI and health, knowledge of whether AMI scores are associated with PA is required. The present study aimed to examine the association between AMI scores and objectively measured PA in community-dwelling older adults.
Methods
Participants
This cross-sectional observational study used data from the National Center for Geriatrics and Gerontology-Study of Geriatric Syndromes (NCGG-SGS). This community-based cohort study aimed to establish a screening program for geriatric syndromes and to validate evidence-based interventions for their prevention [8]. The eligibility criterion for participation in this study was age ≥ 70 years.
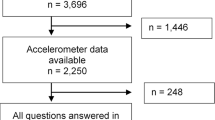
Of the 5257 participants at baseline examination, 5178 agreed to an additional survey and were provided with an accelerometer to measure daily PA. The exclusion criteria in this study were as follows: invalid accelerometer data (n = 2260; 1034 participants did not have the data within 30 days after examination, 1208 participants did not wear the accelerometers for 10 h per day for at least 7 days, and 18 participants experienced technical errors with the data reader); the need for support or care certified by LTCI before the examination (n = 2); having a self-reported basic activities of daily living (BADL) disability (n = 4); having a medical history including stroke, dementia, Parkinson’s disease, or depression (n = 302); having a cognitive impairment (mini-mental state examination [MMSE] score < 21 [9] [n = 50]); or having missing data (n = 61). Finally, a total of 2499 participants were included in the analysis. All participants provided written informed consent before participation. This study was conducted in accordance with the guidelines proposed in the Declaration of Helsinki, and the study protocol was reviewed and approved by the research ethics committee of the National Center for Geriatrics and Gerontology.
Measurement
Physical activity
PA was assessed using a triaxial accelerometer (GT40-020; Kao Corporation, Tokyo, Japan). The display of the accelerometer was set as blinded, and participants were instructed to wear it on either the left or right side of the waist for a month, except during water-based activities, such as bathing or swimming. To collect accelerometer data, the FeliCa RC-S380 data reader (SONY, Tokyo, Japan) was set in nine regional cooperative pharmacies. Participants were instructed to visit these pharmacies and use the data reader within 30 days of the examination. Inclusion criteria for accelerometer data were those who had more than 7 days of data within 30 days after the examination with ≥ 10 h of recording [10] excluding non-wearing time designated as ≥ 35 min of non-recorded time.
The accelerometer estimated the intensity of PA using 11 levels, on a scale of 0.5 (minimal intensity) to 9 (maximal intensity), and recorded the duration in 4-s epoch lengths similar to the Kenz Lifecoder (Suzuken Corporation, Limited: Aichi, Japan) [11]. One to three levels corresponds to ≥ 1.6 to < 3.0 METs, light intensity PA (LPA) (1.6–3 METs), and four or higher levels corresponds to ≥ 3.0 or more METs, moderate-to-vigorous intensity PA (MVPA). The accelerometer also measured step counts. As a secondary outcome, those who met the recommended PA guideline (≥ 150 min/week of MVPA) were identified by referring to the World Health Organization 2020 guidelines on PA [12].
Active mobility index
The AMI assess the participant’s life space with PA and social activity. The detailed protocol has been described in a previous study [2]. The AMI assess three levels of life space in recent a month: < 1, 1–10, and > 10 km from the participant’s residence. In each area, participants were asked how often they visited the location per week (< once/1–3/4–6 days/every day); the purpose [mainly for physical activity (such as walking and exercise)/mainly for daily chores and appointments (shopping or meeting people)/and both equally]; transportation (walking/bicycle/bus, train/car, or other); extent of interaction with others [how many people (0/1–2/3–4/≥ 5)]; and extent of physical activity [how much (almost none/very little/some, or a lot)].
The life-space scores were computed for each level by multiplying the life-space level and frequency. AMI physical/social scores were computed by multiplying the life-space score and physical/social scores. Physical scores were the sum of the purpose, transportation, and extent of physical activity. Social scores were the sum of the purpose, transportation, and extent of interaction with others. The allocation of points can be found in the original literature on AMI [2]. The AMI physical and social scores ranged from 0 to 144, with higher scores indicating greater mobility with activities. Either the physical or social scores were high, or both scores were equal in response to the purpose and transportation question. The range of the AMI total score was the sum of the AMI physical and social scores from 0 to 216. The original literature provides the scoring sample in the Appendix [2].
Confounding factors
Data on sociodemographic characteristics (age, sex, and years of education) and medical information were collected through face-to-face interview. As the medical data, body mass index (BMI), cognitive function, depressive symptoms, fall history in a year (yes/no), whether having pain in any body part (yes/no) were assessed. Cognitive function was assessed using the MMSE [13]. Depressive symptoms were assessed using the 15-item geriatric depression scale (GDS), consisting of 15 yes/no questions and a score ranging from 0 to 15 [14]. In addition, gait speed (m/s) at a comfortable pace was measured using a stopwatch with a sensor by walking a 6.4 m path on a flat and straight surface. A 2.4 m walking path to measure walking speed was set using two markers, and 2 m sections before the start marker and beyond the end marker were set to ensure a consistent walking pace while on the timed path.
Statistical analysis
The differences in participant’s characteristics between meeting or not meeting PA guidelines were analyzed using an independent t-test for continuous variables and the χ2-test for discrete variables. MVPA, LPA, and step counts among the quartile groups of AMI total, physical, and social scores were compared using one-way ANOVA and Tukey’s post hoc test. Linear associations between AMI scores and PA were examined using multiple linear regression analysis in the crude model and fully adjusted model for all covariates. Associations between the quartiles of AMI total, physical, and social scores and meeting PA guidelines were examined using binomial logistic regression models. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) of quartile score groups referred to the Q1 group for meeting PA guidelines were calculated in the crude model and fully adjusted model for all covariates. To assess the discriminative ability of AMI scores to meet PA guidelines, a receiver operating characteristic (ROC) curve was used, and the area under the curve (AUC) was calculated. The optimal cut-off values of AMI scores for meeting PA guidelines were determined using the maximal Youden’s index. All analyses were performed using SPSS version 25 (IBM, New York City, NY, USA). The level of statistical significance was set at P < 0.05.
Results
The characteristics of the 2499 participants (75.5 ± 4.0 years old, 54.4% female, and 12.0 ± 2.6 years of education) are presented in Table 1. The mean AMI total, physical, and social scores were 73.2 ± 29.9, 32.5 ± 17.9, and 40.7 ± 19.0, respectively. Participants had 22.0 ± 6.6 days of the valid accelerometer data, and the mean PA outputs were 25.0 ± 17.6 min/day of MVPA, 43.8 ± 17.8 min/day of LPA, and 5516 ± 2768 step counts. Among all participants, 1188 (47.5%) met the PA guidelines (MVPA ≥ 150 min/week). The meeting PA guideline group showed significantly higher AMI scores (all P < 0.001). The difference in the AMI physical scores between the two groups was larger than the difference in AMI social score.
The differences in PA among the quartile groups of AMI total, physical, and social scores are shown in Fig. 1. In AMI total and physical scores, higher score groups indicated longer time of MVPA and LPA and more step counts than the lower score groups. In the AMI social score, only the Q4 group showed a significantly longer time of LPA and more step counts than the Q1 and Q2 groups. The multiple linear regression models of AMI scores and PA are summarized in Table 2. AMI total and physical scores were associated with MVPA, LPA, and step counts [standardized partial regression coefficient (β) for MVPA, LPA, and step counts of AMI total score were 0.21, 0.16, and 0.24, respectively; all P < 0.001; AMI physical scores were 0.34, 0.18, and 0.36, respectively; all P < 0.001]. AMI social score was associated with LPA (β = 0.08, P < 0.001) and step counts (β = 0.04, P < 0.036).
The ORs of AMI scores for meeting PA guidelines in the logistic regression model are summarized in Table 3. Higher score quartile groups of AMI total and physical scores showed a clear association with increased OR of meeting PA guidelines [aOR (95% CI): AMI total score Q2: 1.67 (1.32–2.11); Q3: 1.93 (1.52–2.45); Q4: 2.98 (2.33–3.81); AMI physical score Q2: 2.22 (1.75–2.81); Q3: 2.78 (2.19–3.54); Q4: 5.29 (4.11–6.80)]. The AMI social score was not significantly associated with meeting PA guidelines.
The AMI physical score had the highest predictive ability for identifying meeting PA guidelines among the AMI scores (AUC 0.68, 95% CI 0.66–0.70). The cut-off value of the AMI physical score was 35, with 52.9% sensitivity and 72.9% specificity. The AUC of AMI total score was 0.63 (95% CI 0.61–0.65, cut-off 66, sensitivity 67.8%, specificity 50.8%), and that of AMI social score was 0.53 (95% CI 0.51–0.55, cut-off 40, sensitivity 52.2%, specificity 53.3%).
Discussion
The present study examined the association between AMI scores and objectively measured PA among community-dwelling older adults. Higher AMI total and physical scores were associated with longer time of MVPA, LPA, and more step counts, and with increased OR for meeting PA guidelines. The AMI social score showed a weak association with LPA. The AMI physical score had the highest predictive ability among the AMI scores to identify those who met the PA guidelines.
Our findings showed that higher AMI total and physical scores were associated with higher PA. This was consistent with previous studies that showed that a larger life space was associated with a more objectively measured PA [6, 7]. AMI total and physical scores considered the extent of PA, which probably led to the association between MVPA and meeting PA guidelines. Although the AUC value was not high for AMI physical scores to discriminate meeting PA guidelines, older adults with higher AMI physical scores are likely to meet the recommended PA guidelines. Therefore, future study is required to refer these findings when examining the association between AMI physical score and health outcomes.
On the other hand, the higher AMI social score group engaged in longer periods of LPA, and the AMI social score had a weak association with MVPA and step counts. Other studies support the finding of an association between AMI social score and LPA. Social isolation was related to reduced LPA in older adults [15], and social connectedness moderated the negative association between loneliness and self-reported PA [16]. Therefore, older adults with higher AMI social scores might engage in more LPA. Systematic reviews have reported that engaging in LPA has health benefits, including cardiometabolic health and mental health [17,18,19], and in a cohort study, older adults with higher AMI social scores were associated with reduced OR of depressive symptoms and physical frailty [2]. Thus, the AMI social score may be associated with health outcomes not only through social activity but also through LPA.
The strength of the present study is that it examined the associations between AMI and PA using large cohort data, and the findings from this study add to the evidence concerning the association between life space and PA [6, 7]. Our study had some limitations. First, it had a cross-sectional design and could not examine the causal relationships between AMI and PA. Future studies with longitudinal designs are needed to examine causal relationships. Second, there was selection bias because the participants were not randomly selected. They were relatively healthy and able to access examination places from their homes, which might distort the association between AMI and PA among community-dwelling older adults. Third, because participants wore the accelerometer on the waist and could not wear it during water-based activities such as swimming, there was a possibility that we could not assess PA by upper limbs or water-based activity.
Conclusions
Higher AMI scores were associated with a higher PA. In particular, older adults with higher AMI total and physical scores engaged in longer MVPA, LPA, and more step counts. Future studies can refer to the present findings when estimating PA in older adults from AMI scores and examining the association between AMI scores and health outcomes.
Data availability
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
References
Johnson J, Rodriguez MA, Al SS (2020) Life-space mobility in the elderly: current perspectives. Clin Interv Aging 15:1665–1674. https://doi.org/10.2147/CIA.S196944
Doi T, Tsutsumimoto K, Nakakubo S et al (2021) Associations between active mobility index and disability. J Am Med Dir Assoc. https://doi.org/10.1016/j.jamda.2021.08.036
Dunlop DD, Song J, Semanik PA et al (2014) Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: prospective cohort study. BMJ 348:g2472. https://doi.org/10.1136/bmj.g2472
Fielding RA, Guralnik JM, King AC et al (2017) Dose of physical activity, physical functioning and disability risk in mobility-limited older adults: results from the LIFE study randomized trial. PLoS One 12:e0182155. https://doi.org/10.1371/journal.pone.0182155
Shah RC, Buchman AS, Leurgans S et al (2012) Association of total daily physical activity with disability in community-dwelling older persons: a prospective cohort study. BMC Geriatr 12:63. https://doi.org/10.1186/1471-2318-12-63
Portegijs E, Tsai LT, Rantanen T et al (2015) Moving through life-space areas and objectively measured physical activity of older people. PLoS One 10:e0135308. https://doi.org/10.1371/journal.pone.0135308
Tsai LT, Rantakokko M, Rantanen T et al (2016) Objectively measured physical activity and changes in life-space mobility among older people. J Gerontol A Biol Sci Med Sci 71:1466–1471. https://doi.org/10.1093/gerona/glw042
Shimada H, Makizako H, Doi T et al (2016) Cognitive impairment and disability in older Japanese adults. PLoS One 11:e0158720. https://doi.org/10.1371/journal.pone.0158720
Perneczky R, Wagenpfeil S, Komossa K et al (2006) Mapping scores onto stages: mini-mental state examination and clinical dementia rating. Am J Geriatr Psychiatry 14:139–144. https://doi.org/10.1097/01.JGP.0000192478.82189.a8
Gorman E, Hanson HM, Yang PH et al (2014) Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. Eur Rev Aging Phys Act 11:35–49. https://doi.org/10.1007/s11556-013-0132-x
Kumahara H, Schutz Y, Ayabe M et al (2004) The use of uniaxial accelerometry for the assessment of physical-activity-related energy expenditure: a validation study against whole-body indirect calorimetry. Br J Nutr 91:235–243. https://doi.org/10.1079/BJN20031033
Bull FC, Al-Ansari SS, Biddle S et al (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54:1451–1462. https://doi.org/10.1136/bjsports-2020-102955
Folstein MF, Robins LN, Helzer JE (1983) The mini-mental state examination. Arch Gen Psychiatry 40:812
Yesavage JA (1988) Geriatric depression scale. Psychopharmacol Bull 24:709–711
Schrempft S, Jackowska M, Hamer M et al (2019) Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health 19:74. https://doi.org/10.1186/s12889-019-6424-y
Gyasi RM, Phillips DR, Asante F et al (2021) Physical activity and predictors of loneliness in community-dwelling older adults: the role of social connectedness. Geriatr Nurs 42:592–598. https://doi.org/10.1016/j.gerinurse.2020.11.004
Fuzeki E, Engeroff T, Banzer W (2017) Health benefits of light-intensity physical activity: a systematic review of accelerometer data of the National Health and Nutrition Examination Survey (NHANES). Sports Med 47:1769–1793. https://doi.org/10.1007/s40279-017-0724-0
Felez-Nobrega M, Bort-Roig J, Ma R et al (2021) Light-intensity physical activity and mental ill health: a systematic review of observational studies in the general population. Int J Behav Nutr Phys Act 18:123. https://doi.org/10.1186/s12966-021-01196-7
Amagasa S, Machida M, Fukushima N et al (2018) Is objectively measured light-intensity physical activity associated with health outcomes after adjustment for moderate-to-vigorous physical activity in adults? A systematic review. Int J Behav Nutr Phys Act 15:65. https://doi.org/10.1186/s12966-018-0695-z
Acknowledgements
We would like to thank the Midori Ward office for help with subject recruitment.
Funding
This work was financially supported by Strategic Basic Research Programs Redesigning Communities for Aged Society (RISTEX) of the Japan Science and Technology Agency (JST), Health and Labor Sciences Research Grants, joint research with Kao Corporation, and the funds of Obu City local government. The authors also received financial support through JSPS KAKENHI Grant Number JP22K11846. The funders played no role in the design, conduct, and reporting of this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: SK. Formal analysis: SK. Funding acquisition: HS and SK. Investigation: TD, KT, and SN. Project administration and supervision: HS. Writing—original draft: SK. Writing—review and editing: TD, KT, SN, YK, KN, and HS.
Corresponding author
Ethics declarations
Conflict of interest
SK, TD, KT, SN, YK, KN, and HS declare that they have no conflicts of interest.
Ethical approval
Ethical approval for the study was obtained in all countries according to the local regulations.
Statement of human and animal rights
Not applicable.
Informed consent
Participants were invited to take part in the study and were free to decline participation. Consent was obtained with assurance of data confidentiality. Participants who did not give their consent were excluded from the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kurita, S., Doi, T., Tsutsumimoto, K. et al. Associations between Active Mobility Index and objectively measured physical activity among older adults. Aging Clin Exp Res 35, 147–153 (2023). https://doi.org/10.1007/s40520-022-02256-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02256-z