Abstract
Background
Screening for dementia in relevant healthcare settings may help in identifying low cognitive functioning for comprehensive cognitive assessments and subsequent dementia treatment after diagnosis.
Aims
This study sought to estimate the prevalence of no reported dementia-related diagnosis in a nationally-representative sample of older Americans with a cognitive impairment consistent with dementia (CICD) by healthcare utilization.
Methods
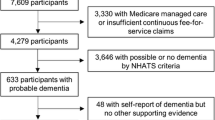
The unweighted analytical sample included 1514 Americans aged ≥ 65 years that were identified as having a CICD without history of stroke, cancers, neurological conditions, or brain damage who participated in at least one-wave of the 2010–2016 waves of the Health and Retirement Study. An adapted Telephone Interview of Cognitive Status assessed cognitive functioning. Those with scores ≤ 6 had a CICD. Dementia-related diagnosis was self-reported. Respondents indicated if they visited a physician, received home healthcare, or experienced an overnight nursing home stay in the previous two years.
Results
The prevalence of no reported dementia-related diagnosis in persons with a CICD who visited a physician was 89.9% (95% confidence interval (CI): 85.4%-93.1%). Likewise, the prevalence of no reported diagnosis in those with a CICD who received home healthcare was 84.3% (CI: 75.1–90.5%). For persons with a CICD that had an overnight nursing home stay, the prevalence of no reported dementia-related diagnosis was 83.0% (CI: 69.1–91.4%).
Discussion
Although the prevalence of no reported dementia-related diagnosis in individuals with a CICD differed across healthcare settings, the prevalence was generally high nonetheless.
Conclusions
We recommend increased awareness and efforts be given to dementia screenings in various clinical settings.
Similar content being viewed by others
References
Arvanitakis Z, Bennett DA (2019) What is dementia? JAMA 322:1728. https://doi.org/10.1001/jama.2019.11653
Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed 26 July 2021
Koedam EL, Pijnenburg YA, Deeg DJ et al (2008) Early-onset dementia is associated with higher mortality. Dement Geriatr Cogn Disord 26:147–152. https://doi.org/10.1159/000149585
Matthews KA, Xu W, Gaglioti AH et al (2019) Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged ≥65 years. Alzheimers Dement 15:17–24. https://doi.org/10.1016/j.jalz.2018.06.3063
Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM (2013) Monetary costs of dementia in the United States. N Engl J Med 368:1326–1334. https://doi.org/10.1056/NEJMsa1204629
Healthy Brain Initiative. https://www.cdc.gov/aging/pdf/2018-2023-Road-Map-508.pdf. Accessed 26 July 2021
Arvanitakis Z, Shah RC, Bennett DA (2019) Diagnosis and management of dementia: review. JAMA 322:1589–1599. https://doi.org/10.1001/jama.2019.4782
Foster NL, Bondi MW, Das R et al (2019) Quality improvement in neurology: Mild cognitive impairment quality measurement set. Neurology 93:705–713. https://doi.org/10.1212/WNL.0000000000008259
Centers for Medicare & Medicaid Services. Cognitive Assessment & Care Plan Services. https://www.cms.gov/cognitive. Accessed 26 July 2021
US Preventive Services Task Force, Owens DK, Davidson KW et al (2020) Screening for Cognitive Impairment in Older Adults: US Preventive Services Task Force Recommendation Statement. JAMA 323:757–763. https://doi.org/10.1001/jama.2020.0435
McGrath R, Robinson-Lane SG, Clark BC, Suhr JA, Giordani BJ, Vincent BM (2021) Self-reported dementia-related diagnosis underestimates the prevalence of older americans living with possible dementia. J Alzheimers Dis 82:373–380. https://doi.org/10.3233/JAD-201212
HRS Data Book. https://hrs.isr.umich.edu/about/data-book?_ga=2.177450149.1489958521.1509473800-353572931.1501594459. Accessed 26 July 2021
Health and Retirement Study. Sample Sizes and Response Rates. https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf. Accessed 26 July 2021
Lin PJ, Emerson J, Faul JD et al (2020) Racial and ethnic differences in knowledge about one’s dementia status. J Am Geriatr Soc 68:1763–1770. https://doi.org/10.1111/jgs.16442
Gaugler JE, Jutkowitz E, Peterson CM, Zmora R (2018) Caregivers dying before care recipients with dementia. Alzheimers Dement (NY) 4:688–693
Harris ML, Titler MG, Hoffman GJ (2021) Associations between alzheimer’s disease and related dementias and depressive symptoms of partner caregivers. J Appl Gerontol 40:772–780. https://doi.org/10.1177/0733464820952252
Plassman BL, Newman TT, Welsh KA, Helms M, Breitner JC (1994) Properties of the Telephone Interview for Cognitive Status Application in epidemiological and longitudinal studies. Cognit Behav Neurol 7:235–241
Crimmins EM, Kim JK, Langa KM, Weir DR (2011) Assessment of cognition using surveys and neuropsychological assessment: the Health and Retirement Study and the Aging, Demographics, and Memory Study. J Gerontol B Psychol Sci Soc Sci 66(Suppl 1):i162–i171
Langa KM, Larson EB, Crimmins EM et al (2017) A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med 177:51–58. https://doi.org/10.1001/jamainternmed.2016.6807
HRS/AHEAD Documentation Report. Documentation of Cognitive Functioning Measures in the Health and Retirement Study. https://hrs.isr.umich.edu/sites/default/files/biblio/dr-006.pdf. Accesed 26 July 2021
HRS Documentation Report. Updates to HRS Sample Weights. https://hrs.isr.umich.edu/sites/default/files/biblio/dr-013.pdf. Accessed 26 July 2021
Ashman JJ, Rui P, Okeyode T (2019) Characteristics of office-based physician visits, 2016. NCHS Data Brief 331:1–8
Sazlina SG (2015) Health screening for older people-what are the current recommendations? Malays Fam Physician 10:2–10
Gaugler JE, Yu F, Davila HW, Shippee T (2014) Alzheimer’s disease and nursing homes. Health Aff (Millwood) 33:650–657. https://doi.org/10.1377/hlthaff.2013.1268
Brooks LG, Loewenstein DA (2010) Assessing the progression of mild cognitive impairment to Alzheimer’s disease: current trends and future directions. Alzheimers Res Ther 2:28
Mlinac ME, Feng MC (2016) Assessment of activities of daily living, self-care, and independence. Arch Clin Neuropsychol 31:506–516. https://doi.org/10.1093/arclin/acw049
Moore KL, Boscardin WJ, Steinman MA, Schwartz JB (2014) Patterns of chronic co-morbid medical conditions in older residents of US nursing homes: differences between the sexes and across the agespan. J Nutr Health Aging 18:429–436
Savva GM, Arthur A (2015) Who has undiagnosed dementia? A cross-sectional analysis of participants of the Aging. Demogr Mem Study Age Ageing 44:642–647. https://doi.org/10.1093/ageing/afv020
Nogueras DJ, Postma J, Van Son C (2016) Why didn’t I know? Perspectives from adult children of elderly parents with dementia. J Am Assoc Nurse Pract 28:668–674. https://doi.org/10.1002/2327-6924.12382
Astell AJ, Bouranis N, Hoey J et al (2019) Technology and Dementia: The Future is Now. Dement Geriatr Cogn Disord 47:131–139. https://doi.org/10.1159/000497800
Barnes DE, Beiser AS, Lee A et al (2014) Development and validation of a brief dementia screening indicator for primary care. Alzheimers Dement 10:656–665.e1. https://doi.org/10.1016/j.jalz.2013.11.006
Aiello EN, Gramegna C, Esposito A et al (2021) The Montreal Cognitive Assessment (MoCA): updated norms and psychometric insights into adaptive testing from healthy individuals in Northern Italy. Aging Clin Exp Res. https://doi.org/10.1007/s40520-021-01943-7
McGrath RP, Clark BC, Erlandson KM et al (2019) Impairments in individual autonomous living tasks and time to self-care disability in middle-aged and older adults. J Am Med Dir Assoc 20:730–735.e3. https://doi.org/10.1016/j.jamda.2018.10.014
Müller-Spahn F (2003) Behavioral disturbances in dementia. Dialogues Clin Neurosci 5:49–59 https://doi.org/10.31887/DCNS.2003.5.1/fmuellerspahn
McGrath R, Vincent BM, Hackney KJ et al (2020) Weakness and cognitive impairment are independently and jointly associated with functional decline in aging Americans. Aging Clin Exp Res 32:1723–1730. https://doi.org/10.1007/s40520-019-01351-y
Parker K, Rhee Y, Tomkinson GR et al (2021) Handgrip weakness and asymmetry independently predict the development of new activity limitations: results from analyses of longitudinal data from the US health and retirement study. J Am Med Dir Assoc 22:821–826. https://doi.org/10.1016/j.jamda.2020.11.006
McGrath R, Cawthon PM, Cesari M et al (2020) Handgrip strength asymmetry and weakness are associated with lower cognitive function: a panel study. J Am Geriatr Soc 68:2051–2058. https://doi.org/10.1111/jgs.16556
Shaughnessy KA, Hackney KJ, Clark BC et al (2020) A narrative review of handgrip strength and cognitive functioning: bringing a new characteristic to muscle memory. J Alzheimers Dis 73:1265–1278. https://doi.org/10.3233/JAD-190856
Klawitter L, Mahoney SJ, Dahl L et al (2020) Evaluating additional aspects of muscle function with a digital handgrip dynamometer and accelerometer for cognitive functioning in older adults: a pilot study. J Alzheimers Dis Rep 4:495–499
Zuliani G, Polastri M, Romagnoli T et al (2021) Clinical and demographic parameters predict the progression from mild cognitive impairment to dementia in elderly patients. Aging Clin Exp Res 33:1895–1902. https://doi.org/10.1007/s40520-020-01697-8
Liu T, Li N, Hou Z et al (2021) Nutrition and exercise interventions could ameliorate age-related cognitive decline: a meta-analysis of randomized controlled trials. Aging Clin Exp Res 33:1799–1809. https://doi.org/10.1007/s40520-020-01730-w
Meng Q, Yin H, Wang S et al (2021) The effect of combined cognitive intervention and physical exercise on cognitive function in older adults with mild cognitive impairment: a meta-analysis of randomized controlled trials. Aging Clin Exp Res. https://doi.org/10.1007/s40520-021-01877-0
Wallace RB, Herzog AR (1995) Overview of the health measures in the Health and Retirement Study. Journal of Human Resources 30:S84–S107
Funding
None to report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None to report.
Informed consent
Written informed consent was provided by participants before entering the HRS.
Research having human and animal participants
HRS protocols were approved by the University’s Behavioral Sciences Committee Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parker, K., Vincent, B., Rhee, Y. et al. The estimated prevalence of no reported dementia-related diagnosis in older Americans living with possible dementia by healthcare utilization. Aging Clin Exp Res 34, 359–365 (2022). https://doi.org/10.1007/s40520-021-01980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01980-2