Abstract
Background
We consider the relationships between a clinical and radiological diagnosis of knee or hip OA and activities of daily-living (ADL) in older adults.
Methods
Data were available for 222 men and 221 women from the Hertfordshire Cohort Study (HCS) who also participated in the UK component of the European Project on Osteoarthritis (EPOSA). Participants completed the EuroQoL survey where they reported if they had difficulties with mobility, self-care, usual activities and movement around their house. Hip and knee radiographs were graded for overall Kellgren and Lawrence score (positive definition defined as a 2 or above). Clinical OA was defined using American College of Rheumatology criteria.
Results
In men, a clinical diagnosis of hip or knee OA were both associated with reported difficulties in mobility, ability to self-care and performing usual-activities (hip OA: OR 17.6, 95% CI 2.07, 149, p = 0.009; OR 12.5, 95% CI 2.51, 62.3, p = 0.002; OR 4.92, 95% CI 1.06, 22.8, p = 0.042 respectively. Knee OA: OR 8.18, 95% CI 3.32, 20.2, p < 0.001; OR 4.29, 95% CI 1.34, 13.7, p = 0.014; OR 5.32, 95% CI 2.26, 12.5, p < 0.001 respectively). Similar relationships were seen in women, where in addition, a radiological diagnosis of knee OA was associated with difficulties performing usual activities (OR 3.25, 95% CI 1.61, 6.54, p = 0.001). In general, men with OA reported stronger associations between moving around the house, specifically around the kitchen (clinical hip OA: OR 13.7, 95% CI 2.20, 85.6, p = 0.005; clinical knee OA OR 8.45, 95% CI 1.97, 36.2, p = 0.004) than women.
Discussion and conclusion
Clinical OA is strongly related to the ability to undertake ADL in older adults and should be considered in clinic consultations when seeing patients with OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increase in life expectancy and the subsequent ageing population has led to a higher prevalence of chronic, non-communicable diseases and in particular musculoskeletal (MSK) disorders. After cardiovascular diseases, malignant neoplasms and chronic respiratory diseases, MSK disorders are the fourth leading cause of morbidity in older people [1]. Osteoarthritis (OA) is the most common of the MSK disorders affecting older people [2]. It has been estimated that OA affects over 26 million people in the USA, and around 1.6–3.4 million in England and Wales [3, 4]. There is a significant economic burden associated with OA, largely secondary to the effects of disability associated with OA, comorbid diseases and cost of treatment [4].
In OA there is degeneration of the joints involving the articular cartilage and many of the surrounding tissues [5]. There is a breakdown of the equilibrium between breakdown and repair of joint tissue, leading to the loss of articular cartilage, remodelling of subchondral bone, osteophyte formation, ligament laxity, periarticular muscle weakening, and occasionally synovitis [6]. This can occur in any joint, but the joints more commonly afflicted by OA are the hands, feet, facet joints and large weight-bearing joints, such as the knees and hips [5]. Joint degeneration in OA results in pain, which in turn leads to stiffness and restricted movement.
Epidemiological studies of OA have principally defined OA using two methods: radiographic and clinical [7, 8]. A radiographic definition of OA captures the structural changes in the joints of interest. The majority of studies employ the radiographic technique first proposed by Kellgren and Lawrence [9], which characterises knee OA into five grades (0, normal to 4, severe) with a score of 2 or above representing OA. A radiological diagnosis of OA alone, however, may not accurately reflect the clinical burden of the disease as studies have shown that pain in OA is heightened by co-morbid illness, muscle-strength, mood, cognition and disability [10]. An alternative method of defining OA is to utilise clinical criteria. In the early 1990s, the American Rheumatism Association (ACR) developed a definition of OA that takes into account medical history, laboratory test results and physical examinations.
OA can contribute to inactivity with ageing, secondary to pain and reduced function, thus ultimately impairing quality of life. It is well established that OA pain, swelling or stiffness can make it difficult for individuals to perform simple activities of daily living (ADL) such as opening boxes of food, tucking in bedsheets, writing, using a computer mouse, driving a car, walking, climbing stairs and lifting objects [11] but to our knowledge the impact the condition has on everyday function has been little studied in individuals who are not awaiting joint replacement surgery.
The EuroQol survey is a standardized instrument for measuring generic health status developed in 1990 by the EuroQol group which is a multidisciplinary team of researchers from five European countries; The Netherlands, UK, Sweden, Finland, and Norway [12]. Their aim was to develop an instrument which is not specific to disease but standardized and can be used as a complement for existing health-related quality of life (HRQoL) measures. In the current study, we use components of the Euroqol survey to consider the relationships between a clinical or radiological diagnoses of lower limb OA and ADL in older men and women.
Methods
The study participants were 222 men and 221 women from the Hertfordshire Cohort Study (HCS) who also participated in the UK component of the European Project on Osteoarthritis (EPOSA). The Hertfordshire Cohort Study (HCS) is a population-based UK cohort of older adults. Study design and recruitment have been described in detail previously [13]. In brief, we traced men and women born between 1931 and 1939 in Hertfordshire and who still lived there in 1998–2003. A nurse-administered questionnaire, which included details of socioeconomic status and dietary calcium intake, was conducted at this time. In a follow-up study in 2011–2012, 443 participants consented to a home visit by a trained research nurse. At this visit a nurse-administered questionnaire was again administered which included details of smoking status, alcohol consumption and physical activity (average minutes per day spent walking, cycling, gardening, playing sport and doing housework in the last 2 weeks). Height was measured to the nearest 0.1 cm and weight to the nearest 0.1 kg on a SECA floor scale (Chasmors Ltd, London, UK). Body mass index (BMI) was calculated as weight divided by height2 (kg/m2). Participants also answered questions taken from the EuroQol study where they were asked: “Do you have problems with mobility?”; “Do you have problems with self-care?”; “Do you have problems undertaking your usual activities?” [12]. Participants were then asked more detailed questions on mobility where they were asked: “Do you have problems moving around inside and outside your house?”; “Do you have problems moving around your bathroom?”; “Do you have problems moving around your kitchen?”; “Do you have problems moving around your toilet?”; “Do you have problems accessing public facilities such as grocery shops, bus stops or banks?”. Radiographs were taken of the hip and knees under standardised conditions at a local hospital after the home visit. Clinical OA was defined based on algorithms developed by the American College of Rheumatology [14].
A clinical diagnosis of hip OA was made if pain, as assessed by WOMAC, was present in addition to all of the following: (1) pain associated with hip internal rotation in at least one side; (2) morning stiffness lasting < 60 min evaluated by the WOMAC stiffness subscale (score from ‘mild’ to ‘extreme’); and (3) age of over 50 years [15]. Pain was assessed using the Western Ontario and McMaster Universities OA Index (WOMAC) pain subscale score. The WOMAC is a 24-item questionnaire with three subscales measuring pain (five items), stiffness (two items), and physical function (17 items) [16].
To diagnose clinical knee OA the patient had to experience knee pain and any three of the following: (1) bony tenderness in at least one side on examination; (2) crepitus on active motion in at least one side on examination; (3) less than 30 min of morning stiffness, evaluated by the WOMAC stiffness subscale; (4) no palpable warmth of synovium in both knees on examination; (5) age over 50 years; or (6) bony enlargement in at least one side on examination.
Radiographs were graded according to Kellgren and Lawrence (KL). KL classifies OA into five grades (0, normal to 4, severe). The KL grading system is briefly described as follows: grade 0—no radiographic features of OA are present; grade 1—unlikely narrowing of the joint space and possible osteophytes on the radiograph; grade 2—small osteophytes and possible narrowing of the joint space; grade 3—multiple, moderately sized osteophytes, definite joint space narrowing, some sclerotic areas and possible deformation of bone ends; and grade 4—multiple large osteophytes, severe joint space narrowing, marked sclerosis and definite bony end deformity [9]. In our study, a positive definition of OA reflected a KL score of 2 or above. The radiographs were all graded by two experienced rheumatologists with good inter-observer agreement.
Stata version 14 was used for all analyses. Study participants’ characteristics were summarised using means and standard deviations (SD) or medians and interquartile ranges (IQR) for continuous variables, and numbers and percentages for binary and categorical variables. Logistic regression was used to model the association between self-reported OA, clinical OA and radiographic OA with the components of the EuroQol survey and questions on mobility. These analyses were completed with and without adjustment for age, BMI, social class, activity, alcohol intake, baseline dietary calcium and smoking status and years since menopause and HRT use in women. These confounders were selected as they have been shown to be associated with the ability to undertake ADL and OA in previous studies. A study by Pollard and colleagues on a cohort of 763 people who had been diagnosed with OA in Somerset and Avon, UK showed that impact of OA on ADL appears to vary with respect to social deprivation [17]. A recent study by Magnusson and colleagues showed alcohol was associated with inflammatory hand OA whereas smoking appeared to be protective [18]. Farr et al. have demonstrated using accelerometry that the majority of patients with knee OA do not meet the recommended levels of physical activity [19] which results in weight gain and obesity, progression of OA and impairment of function [20]. Finally, significantly higher concentrations of calcium have been found in the meniscus of individuals with knee OA undergoing total knee replacement surgery [21].
Results
The mean [standard deviation (SD)] age of study participants was 75.5 (2.5) and 75.8 (2.6) years in men and women, respectively. The mean body mass index (BMI) was 27.9 kg/m2 (SD 3.9) in men and 28.4 kg/m2 (SD 5.1) in women. Men had a lower median activity time than women in the last 2 weeks [176 min/day (IQR 105–270) and 200 min/day (IQR 135–283) respectively], although this did not reach statistical significance (p = 0.089). A higher proportion of men were current smokers [5% (n = 11) vs 2.7% (n = 6) of women] (Table 1).
Seven (3.2%) men and 13 (6.0%) women had a clinical diagnosis of hip OA. Radiographic hip OA was more common, affecting 46.3% (n = 93) of men and 40.6% (n = 78) of women. Knee OA was overall more common than hip OA in both sexes with the radiographic diagnosis again being more prevalent [50.2% (n = 101) of men and 58.7% (n = 118) of women], compared with the clinical diagnosis [12% (n = 26) of men and 19% (n = 41) of women] (Table 1).
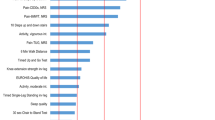
In men, a clinical diagnosis of hip or of knee OA were both associated with reported difficulties in mobility, ability to self-care and performing usual activities (hip OA: OR 17.6, 95% CI 2.07, 149, p = 0.009; OR 12.5, 95% CI 2.51, 62.3, p = 0.002; OR 4.92, 95% CI 1.06, 22.8, p = 0.042, respectively. Knee OA: OR 8.18, 95% CI 3.32, 20.2, p < 0.001; OR 4.29, 95% CI 1.34, 13.7, p = 0.014; OR 5.32, 95% CI 2.26, 12.5, p < 0.001 respectively). With the exception of the association between clinical knee OA and self-care these findings remained robust following adjustment for confounders (Table 2). Very similar relationships were seen in women, where clinical OA at hip and knee were both associated with reported difficulties in mobility, ability to self-care and performing usual activities (Hip OA: OR 5.49, 95% CI 1.63, 18.5, p = 0.006; OR 8.81, 95% CI 2.67, 29.0, p < 0.001 and OR 15.9, 95% CI 3.40, 74.0, p < 0.001 respectively; Knee OA: OR 7.51, 95% CI 3.56, 15.9, p < 0.001; OR 9.52, 95% CI 3.87, 23.4, p < 0.001 and OR 9.20, 95% CI 4.31, 19.7, p < 0.001, respectively). The association between clinical knee OA and difficulties with mobility, self-care and performing usual activates remained robust following adjustment for confounders but for clinical hip OA only the association with problems performing usual activities remained significant following adjustment for confounders (OR 19.6, 95% CI 1.18, 326, p < 0.038). Additionally, in women a radiological diagnosis of knee OA was associated with similar, though less marked, reported difficulties in mobility, self-care and performing usual activities (OR 2.56, 95% CI 1.36, 4.85, p = 0.004; OR 2.81, 95% CI 1.00, 7.90, p = 0.050 and OR 3.25, 95% CI 1.61, 6.54, p = 0.001 respectively). Aside from the association with self-care these associations remained robust following adjustment for confounders (Table 3).
In general, men reported stronger associations between OA and moving around the house than women. In men there was a significant association with problems moving around inside and outside the house and a clinical diagnosis of OA at the hip or the knee (OR 14.4, 95% CI 2.98, 69.3, p = 0.001 and OR 7.85, 95% CI 2.90, 21.3, p < 0.001, respectively) and this remained robust following adjustment for confounders. Very similar associations with clinical hip and knee OA were seen when men were asked if they had difficulties mobilising around the kitchen specifically (OR 13.7, 95% CI 2.20, 85.6, p = 0.005 and OR 8.45, 95% CI 1.97, 36.2, p = 0.004, respectively) and these findings again remained significant following adjustment for confounders. Furthermore, clinical hip and knee OA in men were positively associated with problems accessing public facilities (OR 10.4, 95% CI 2.20, 49.5, p = 0.003 and OR 3.78, 95% CI 1.46, 9.80, p = 0.006, respectively) but only clinical hip OA remained significant following adjustment for confounders (OR 108, 95% CI 7.69, 1529, p = 0.001). Interestingly, following adjustment for confounders, knee OA was not associated with problems moving around the bathroom or toilet in men but significant associations were seen with both clinical hip OA and radiographic hip OA (bathroom: clinical hip OA—OR 290, 95% CI 11.1, 7559, p = 0.001 and radiographic hip OA—OR 7.71, 95% CI 1.28, 46.4, p = 0.026; toilet: clinical hip OA—OR 93.1, 95% CI 5.44, 1593, p = 0.002 and radiographic hip OA—OR 5.84, 95% CI 1.00, 34.1, p = 0.050) (Table 4).
Overall, the associations between OA and difficulties with reported mobility were weaker in women. In contrast to men there was no association between either hip or knee OA and difficulties accessing public facilities and moving around the bathroom following adjustment for confounders. Knee, but not hip, OA in women was associated with general problems moving inside and outside the house following adjustment for confounders (clinical knee OA: OR 13.5, 95% CI 4.09, 44.7, p < 0.001; radiographic knee OA: OR 12.4, 95% CI 2.41, 64.0, p = 0.003) and problems moving around the kitchen after adjustment for confounders (clinical knee OA: OR 5.38, 95% CI 1.17, 24.7, p < 0.030). Similarly to men, clinical hip OA was associated with problems moving around the toilet (OR 12.1, 95% CI 3.34, 43.6, p < 0.001) and this association also remained significant post adjustment for confounders (Table 5).
Discussion
In the current study, we have shown that a diagnosis of lower limb OA is strongly related to the ability to undertake ADL in older adults. We have demonstrated that in both men and women a clinical diagnosis of hip or of knee OA and a radiological diagnosis of knee OA in women is associated with difficulties in mobility, ability to self-care and performing usual activities. Our data, therefore. suggests that using a clinical criteria to diagnose OA, especially in men, is more sensitive at identifying individuals who are at risk of functional impairment then employing a radiographic diagnosis alone. This is consistent with previous studies that have shown radiographic knee OA correlates poorly with the physical symptoms of OA [22]. Indeed, a previous study utilising participants from the HCS demonstrated that a substantial proportion of men and women who were diagnosed with radiographic OA did not have self-reported or diagnosis of clinical OA (57.7%) [7]. Our study therefore lends further credence to the argument that in the clinical setting where the focus of intervention is on the improvement of symptoms, the use of a clinical definition of knee OA, which includes pain, may be more useful than relying on a radiographic diagnosis alone to identify individuals at risk of functional impairment and target resources accordingly. Indeed, the International Rheumatologic Board (IRB) recently proposed guidelines for the diagnosis of OA in primary care which are based on the ACR criteria for clinical OA [23].
Our data are consistent with previous studies that have shown that OA leads to impairments in quality of life and ADL and as a consequence, results in dependency, institutionalisation and increased health-care costs [24, 25]. The majority of these studies have been qualitative in nature but a recent study by Stamm and colleagues explored the limitations in the ADLs in older adults in a population-based survey of 3097 subjects aged ≥ 65 years in Austria. They demonstrated that OA was associated with a with a 68% higher chance of impairment of intense ADLs such as lifting and carrying a shopping bag of over 5 kg of weight, bending and kneeling down, walking 500 m without the use of aids, climbing stairs without the use of aids and heavy housework [25].
We have observed in the current study that problems with mobilising around specific rooms in the house and accessing public facilities varied according to site and sex. The ability of men to mobilise around the kitchen and to access public facilities was impeded by both hip and knee OA with stronger associations seen when a clinical definition of OA is utilised. In contrast to men, there was no significant association between lower limb OA and difficulties accessing public facilities or mobilising around the bathroom in women following adjustment for confounders. In both sexes, however, hip OA was associated with difficulties mobilising around the toilet. These results suggest that the specific movements required for mobilising around a toilet, which is usually in a confined space, and the action of getting on and off a toilet are more impeded by hip OA than knee OA. Conversely, mobilising around traditionally larger rooms, such as the kitchen, appears to be more impeded by knee OA. These results are particularly pertinent when considering the benefit of potentially tailoring occupational therapy (OT) services to different groups of patients and that we should ask about ADL in the clinic setting. Indeed, there is strong evidence to suggest that to successfully design healthcare programs for the treatment of OA it is essential to consider what patients need and prefer, and how they value various aspects of a health intervention [26].
Our study is limited in that the results may not be entirely representative of the wider UK population since all recruited participants were born in the county of Hertfordshire and at age 75 were still living there (as had been the case in previous studies). We have demonstrated that this cohort are a good representation of the general population with regard to body build and lifestyle factors, such as smoking and alcohol intake, therefore suggesting that selection bias was minimal [27]. Furthermore, all comparisons undertaken were internal. There is a possibility that there may have been some inconsistencies in the interpretation of radiographs. To minimise this risk, however, two experienced rheumatologists were used to grade the radiographs, with high inter-observer concordance. We have also previously shown that for both clinical and radiographic assessment of OA used within this current study good levels of agreement exists between- and within-observer variation. Briefly, repeatability for all observations was graded either good or excellent by multiple observers [28]. Additionally, only a small number of participants (7 men and 13 women) fit the diagnostic criteria for clinical hip OA which may limit our power to detect statistically significant relationships. Finally, the study population did not specifically exclude individuals who were awaiting a joint replacement operation and therefore some of these individuals may have been included in the analysis. There is evidence to suggest, however, that although functional improvements following knee arthroplasty are excellent regardless of age, knee arthroplasty contributes little to the quality of life in older patients (octogenarians) [29].
Conclusions
Our study shows that a diagnosis of OA is strongly related to the ability to undertake ADL in older adults. Limitations in ADLs and mobility vary according to site and sex and these differences should be considered in the clinical setting. These data support the requirement for functional assessment and corresponding interventions to prevent worsening functional decline in individuals with OA and the consequent health and social problems which would arise at great expense to the individual and society.
References
Prince MJ, Wu F, Guo Y et al (2015) The burden of disease in older people and implications for health policy and practice. Lancet 385:549–562. https://doi.org/10.1016/s0140-6736(14)61347-7
Felson DT, Naimark A, Anderson J et al (1987) The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 30:914–918
Lawrence RC, Felson DT, Helmick CG et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58:26–35. https://doi.org/10.1002/art.23176
Lord J, Victor C, Littlejohns P et al (1999) Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee. Health Technol Assess 3:1–55
Litwic A, Edwards MH, Dennison EM et al (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105:185–199. https://doi.org/10.1093/bmb/lds038
Hutton CW (1989) Osteoarthritis: the cause not result of joint failure? Ann Rheum Dis 48:958–961
Parsons C, Clynes M, Syddall H et al (2015) How well do radiographic, clinical and self-reported diagnoses of knee osteoarthritis agree? Findings from the Hertfordshire cohort study. SpringerPlus 4:177. https://doi.org/10.1186/s40064-015-0949-z
Parsons C, Fuggle NR, Edwards MH et al (2017) Concordance between clinical and radiographic evaluations of knee osteoarthritis. Aging Clin Exp Res. https://doi.org/10.1007/s40520-017-0847-z
Kellgren JH, Lawrence JS (1957) Radiological assessment of rheumatoid arthritis. Ann Rheum Dis 16:485–493
Issa SN, Sharma L (2006) Epidemiology of osteoarthritis: an update. Curr Rheumatol reports 8:7–15
Marshall M, Watt FE, Vincent TL et al (2018) Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nat Rev Rheumatol. https://doi.org/10.1038/s41584-018-0095-4
The EuroQol Group (1990) EuroQol–a new facility for the measurement of health-related quality of life. Health policy 16:199–208
Syddall HE, Aihie Sayer A, Dennison EM et al (2005) Cohort profile: the Hertfordshire cohort study. Int J Epidemiol 34:1234–1242. https://doi.org/10.1093/ije/dyi127
Altman RD (1991) Classification of disease: osteoarthritis. Semin Arthritis Rheum 20:40–47
van der Pas S, Castell MV, Cooper C et al (2013) European project on osteoarthritis: design of a six-cohort study on the personal and societal burden of osteoarthritis in an older European population. BMC Musculoskelet Disord 14:138. https://doi.org/10.1186/1471-2474-14-138
Bellamy N (2002) WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol 29:2473–2476
Pollard B, Dixon D, Johnston M (2014) Does the impact of osteoarthritis vary by age, gender and social deprivation? A community study using the international classification of functioning, disability and health. Disabil Rehabil 36:1445–1451. https://doi.org/10.3109/09638288.2013.847123
Magnusson K, Mathiessen A, Hammer HB et al (2017) Smoking and alcohol use are associated with structural and inflammatory hand osteoarthritis features. Scand J Rheumatol 46:388–395. https://doi.org/10.1080/03009742.2016.1257736
Farr JN, Going SB, Lohman TG et al (2008) Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Rheum 59:1229–1236. https://doi.org/10.1002/art.24007
Yazigi F, Espanha M, Marques A et al (2018) Predictors of walking capacity in obese adults with knee osteoarthritis. Acta Reumatol Port 43:256–263
Kosik-Bogacka DI, Lanocha-Arendarczyk N, Kot K et al (2018) Calcium, magnesium, zinc and lead concentrations in the structures forming knee joint in patients with osteoarthritis. J Trace Elem Med Biol 50:409–414. https://doi.org/10.1016/j.jtemb.2018.08.007
Hannan MT, Felson DT, Pincus T (2000) Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol 27:1513–1517
Martel-Pelletier J, Maheu E, Pelletier JP et al (2019) A new decision tree for diagnosis of osteoarthritis in primary care: international consensus of experts. Aging Clin Exp Res 31:19–30. https://doi.org/10.1007/s40520-018-1077-8
Woolf AD, Erwin J, March L (2012) The need to address the burden of musculoskeletal conditions. Best Pract Res Clin Rheumatol 26:183–224. https://doi.org/10.1016/j.berh.2012.03.005
Stamm TA, Pieber K, Crevenna R et al (2016) Impairment in the activities of daily living in older adults with and without osteoporosis, osteoarthritis and chronic back pain: a secondary analysis of population-based health survey data. BMC Musculoskelet Disord 17:139. https://doi.org/10.1186/s12891-016-0994-y
Hiligsmann M, Pinto D, Dennison E et al (2019) Patients’ preferences for osteoarthritis treatment: the value of stated-preference studies. Aging Clin Exp Res 31:1–3. https://doi.org/10.1007/s40520-018-1098-3
Egger P, Duggleby S, Hobbs R et al (1996) Cigarette smoking and bone mineral density in the elderly. J Epidemiol Commun Health 50:47–50
Cushnaghan J, Cooper C, Dieppe P et al (1990) Clinical assessment of osteoarthritis of the knee. Ann Rheum Dis 49:768–770
Yun ST, Kim BK, Ahn BM et al (2018) Difference in the degree of improvement in patient-reported outcomes after total knee arthroplasty between octogenarians and sexagenarians: a propensity score matching analysis. Aging Clin Exp Res 30:1379–1384. https://doi.org/10.1007/s40520-018-0913-1
Funding
This study was funded by the Porticus foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Michael Clynes has received support for attending conferences from UCB, Pfizer and Eli Lily. Author Elaine Dennison has received fees from Pfizer and UCB. Author Professor Cyrus Cooper has received lecture fees and honoraria from Amgen, Danone, Eli Lilly, GSK, Medtronic, Merck, Nestlé, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB outside of the submitted work.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The UK component of EPOSA had ethical approval from the Hertfordshire Research Ethics Committee, reference number 10/h0311/59.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Clynes, M.A., Jameson, K.A., Edwards, M.H. et al. Impact of osteoarthritis on activities of daily living: does joint site matter?. Aging Clin Exp Res 31, 1049–1056 (2019). https://doi.org/10.1007/s40520-019-01163-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01163-0