Abstract
Purpose
ACTION Teens (NCT05013359) was conducted in 10 countries to identify perceptions, attitudes, behaviors, and barriers to effective obesity care among adolescents living with obesity (ALwO), caregivers of ALwO, and healthcare professionals (HCPs). Here, we report data from participants in Italy.
Methods
The ACTION Teens cross-sectional online survey was completed by 649 ALwO (aged 12– < 18 years), 455 caregivers, and 252 HCPs in Italy in 2021.
Results
Most ALwO thought their weight was above normal (69%), worried about weight affecting their future health (87%), and reported making a weight-loss attempt in the past year (60%); fewer caregivers responded similarly regarding their child (46%, 72%, and 33%, respectively). In addition, 49% of caregivers believed their child would lose excess weight with age. ALwO (38%) and caregivers (30%) most often selected wanting to be more fit/in better shape as a weight-loss motivator for ALwO; HCPs most often selected improved social life/popularity (73%). ALwO (25%) and caregivers (22%) most frequently selected lack of hunger control and not liking exercise, respectively, as weight-loss barriers, while HCPs most often agreed that unhealthy eating habits were a barrier (93%). ALwO most often obtained weight-management information from family/friends (25%) and search engines (24%); caregivers most often obtained information from doctors (29%).
Conclusion
In Italy, the impact of obesity on ALwO was underestimated by caregivers, and ALwO and HCPs had different perceptions of key weight-loss motivators and barriers. Additionally, the internet was a key information source for ALwO, which suggests new education/communication strategies are needed.
Level of evidence
IV; Evidence obtained from multiple time series with/without intervention, e.g. case studies.
Trial Registration: ClinicalTrials.gov, NCT05013359.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood obesity has a high prevalence in Italy (21% in boys and 14% in girls [aged 7–9 years]), as in most Southern European countries [1]. Excess adiposity in youth has several worrisome consequences, including the high persistence of obesity into adulthood (up to 80% of cases) and the association with increased morbidity and mortality in later life [2]. Youths with obesity can experience impaired health-related quality of life, discrimination, and stigma, which can lead to unhealthy eating behaviors, binge eating, and a reluctance to participate in physical activity, with the risk of worsening their obesity. Additionally, obesity-related stigma can increase vulnerability to depression, anxiety, low self-esteem, body image disturbance, and suicidal ideation [3].
As such, there is an urgent need for early diagnosis and treatment of obesity in children and adolescents, especially in light of evidence demonstrating that long-term outcomes (including cardiometabolic risk) are better for adolescents living with obesity (ALwO) when they receive early intervention [4, 5]. However, parents and caregivers frequently underestimate the overweight status of their children [6]. This may lead to a delayed obesity diagnosis, which may in turn delay the initiation of treatment of obesity and any complications that are already present.
Healthcare professionals (HCPs) play an important role in the assessment and treatment of obesity in children/adolescents [7], therefore their involvement is crucial in obesity care. Three factors should be considered for improving HCP activity in this field: (i) their level of familiarity with the guidelines for obesity diagnosis and management; (ii) the potential barriers to effective communication with ALwO and their caregivers; (iii) the potential areas of misalignment between ALwO and their caregivers regarding obesity care and management [8].
The ACTION Teens study was conducted in 10 countries (including Italy) to assess ALwO, caregivers’, and HCPs’ perceptions, attitudes, and behaviors relating to obesity, plus barriers impeding effective obesity management for ALwO [8]. Analysis of global data from ACTION Teens confirmed: the need to provide adequate information regarding obesity to ALwO, caregivers, and HCPs; the presence of communication barriers between ALwO, caregivers, and HCPs; and areas of misalignment between ALwO and caregivers regarding obesity care and management [8]. Here, we report the results from an analysis of ACTION Teens participants in Italy and discuss barriers preventing ALwO from receiving effective obesity care in Italy.
Methods
Study design and participants
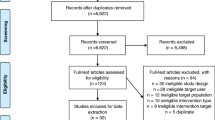
Methodology for the cross-sectional, survey-based ACTION Teens study (ClinicalTrials.gov; NCT05013359) has been reported previously [8].
Briefly, KJT Group Inc. (Rochester, NY, USA) collected survey responses from ALwO, caregivers, and HCPs in 10 countries (Australia, Colombia, Italy, Mexico, Saudi Arabia, South Korea, Spain, Taiwan, Turkey, and the United Kingdom) in 2021 [8]. Participants (plus parents/legal guardians of ALwO) gave informed consent to participate in the study, which was conducted in compliance with the Declaration of Helsinki, EphMRA Code of Conduct [9], and relevant regulations/laws governing data management.
In Italy, the Ethics Committee for Clinical Trials at Integrated University Hospital Verona (Verona, Italy) approved the study on August 9, 2021, and survey responses were collected from August 26 to December 13, 2021. Eligible ALwO lived in Italy, had a body mass index (BMI; calculated using self-reported weight, height, age, and sex) ≥ 95th percentile for their age and sex according to World Health Organization BMI charts [10], and were aged 12– < 18 years. Eligible caregivers resided with an ALwO in Italy ≥ 50% of the time, participated in their ALwO’s healthcare-related decisions, and were aged ≥ 25 years. HCPs had ≥ 2 years’ clinical practice experience, were practicing in Italy, spent most of their time (≥ 50%) in direct patient care, and typically saw/treated ≥ 10 ALwO per month. ALwO were excluded if they indicated that they were “extremely muscular” or had a major injury/illness that caused a significant weight change in the previous 6 months; caregivers were excluded if they responded similarly regarding their ALwO.
Surveys
An external steering committee co-developed and approved separate surveys (with overlapping themes) for each respondent group [8].
Survey questions used single-/multiple-item selection, numeric entry fields, or Likert scales. As previously described [8], primary outcome measures included: attitudes and beliefs about obesity and its impact; weight-loss attempts, motivators, and barriers, and how successful weight loss is defined; history/frequency of weight-related conversations, who initiates weight conversations during HCP appointments, and who is responsible for initiating the conversation; interactions between HCPs and ALwO/caregivers, reasons why obesity is not discussed, and frequency of diagnosing obesity and scheduling weight-related follow-up appointments; and sources used to learn about healthy lifestyles/obesity and weight loss/management.
Recruitment and data collection
For Italy, the aim was to collect surveys from 650 ALwO, 650 caregivers, and 250 HCPs. This sample size was chosen to balance recruitment feasibility with statistical power.
Potential participants were identified from online databases/panels and invited to participate via email, where possible; additionally, some potential candidates (identified from databases) were contacted and screened via telephone, with eligible candidates invited to participate via email.
Caregivers were recruited from a general population sample, then asked to consent to their ALwO participating. After maximizing recruitment of “matched caregiver and ALwO pairs,” the sample size was increased by recruiting additional ALwO and caregivers. The general population sample was stratified to reflect local demographic targets gathered from government data (age, sex, region, education, and income).
Each invitation email included a unique link that was only accessible to the recipient (plus the recipient’s ALwO, if the recipient was a caregiver), which prevented unauthorized access to screening questions [8]. As ALwO and caregivers could access screening questions using the same link, response rates could not be determined for these groups.
To reduce bias, ALwO/caregiver invitation emails and screening questions were designed to conceal the topic of the study until eligibility had been confirmed. Eligible respondents could access the survey, which was provided in Italian. All respondents completed the survey online.
Decipher Survey Software (Forsta) was used to program surveys. Programming ensured that no data were missing (all questions were compulsory) and prevented “multiple participation” from respondents (surveys could not be completed more than once).
Statistical analysis
De-identified data from all respondents with completed surveys (i.e., the full analysis set) were analyzed by KJT Group using Excel (Microsoft 365), SPSS (IBM, version 23.0), and Stata (StataCorp LLC, version IC 14.2). Data weighting was used to limit selection bias and increase the generalizability of results; weights were applied to caregiver data to reflect representative demographic targets for Italy (i.e., age, sex, region, education, and household income). All data were summarized descriptively. For continuous variables, outliers (i.e., data points two standard deviations from the mean) were removed from analyses of relevant variables; where applicable, this reduced the sample size for relevant variables.
Results
Participant characteristics
In Italy, 649 ALwO, 455 caregivers, and 252 HCPs were surveyed (Table 1). The response rate among HCPs was 41%; response rates for ALwO and caregivers could not be determined due to the recruitment methods utilized.
Although 42% of HCPs self-reported receiving advanced training in obesity/weight management after medical school, just 17% had > 1 day of advanced training with certification/evaluation. Most HCPs were aware of clinical guidelines for treating obesity in ALwO (64%), and 86% of HCPs in this subset found the guidelines somewhat/very effective.
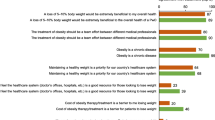
Impact of obesity
The vast majority of HCPs agreed that obesity is a chronic disease (79%). Additionally, most respondents recognized that obesity has a strong impact on a person’s overall health and well-being and thought obesity was at least as impactful as cancer, heart disease, diabetes, and depression (Fig. 1).
Perceived impact of obesity on overall health and well-being. Participants rated how much of an impact they thought different conditions have on a person’s overall health and well-being (1: no impact; 2: slight impact; 3: moderate impact; 4: strong impact; 5: very strong impact) (ALwO/caregiver Q510; HCP Q305). Panel a shows the proportion of participants who indicated obesity has a strong/very strong impact. Panel b shows data comparing each participant’s response about how impactful they believe obesity is in relation to the impact of other health conditions: “Obesity is more impactful” indicates a higher response for obesity than for another health condition; “Obesity is as impactful” indicates an equal response. ALwO adolescents living with obesity, HCP healthcare professional, ADHD attention deficit hyperactivity disorder. Figure adapted from Halford et al. [8]
Some ALwO and caregivers believed that a person with excess weight would find it harder to make friends (38% and 38%, respectively), do well at school (17% and 19%), and get a job (34% and 36%), relative to a person without excess weight.
Many ALwO reported that their weight often/always makes them unhappy (43%) and their body often/always makes them feel insecure (45%), although fewer caregivers reported that their child had these negative feelings (24% and 30%, respectively).
Perceptions of weight/health
Only 46% of caregivers thought their ALwO’s weight was above normal, compared with 69% of ALwO. While 22% of ALwO felt they had fair/poor health, over half (52%) were at least somewhat worried about their weight, and the majority (87%) worried about weight affecting their future health, although the proportions of caregivers responding similarly for their ALwO were lower (3%, 34%, and 72%, respectively) (Fig. 2). Additionally, compared with HCPs, caregivers less frequently reported that their child had diagnosed comorbidities (78% of HCPs’ ALwO patients, on average, vs 33% of caregivers’ ALwO).
ALwO’s weight and health: perceptions and level of worry. Proportion of participants who selected each prespecified answer (ALwO Q106, Q101, Q108, and Q512; caregiver Q106, Q101, Q112, and Q515). Percentages may not sum to 100% due to rounding. ALwO adolescents living with obesity. Figure adapted from Halford et al. [8]
Weight-loss attitudes
Most HCPs (88%) agreed that 5–10% weight loss would be extremely beneficial for an ALwO’s overall health.
Few HCPs (11%) agreed that their ALwO patients are entirely responsible for weight loss. By comparison, a greater proportion of ALwO (69%) and caregivers (50%) agreed that they/their child were entirely responsible.
Many ALwO (71%) and caregivers (59%) agreed that they/their child could lose weight if they really set their mind to it. However, almost half (49%) of caregivers agreed that their ALwO will naturally “slim down” as they grow older/taller, although few HCPs (17%) agreed.
For ALwO and caregivers, successful weight loss was most frequently defined as the ALwO feeling better about themselves (37% and 35%, respectively); for HCPs it was defined as improved self-esteem (58%).
Weight-loss motivators/barriers
The most frequently reported weight-loss motivator among ALwO and caregivers was the ALwO wanting to be more fit/in better shape; by contrast, HCPs thought that the top motivators were ALwO wanting to have improved social life/popularity and confidence/self-esteem, and to look like their peers (Fig. 3). Overall, only 16% of ALwO indicated they had no desire to lose weight, whereas 29% of caregivers thought their child felt this way.
ALwO weight-loss motivators. Proportion of participants who selected each prespecified answer when asked why they/their child has wanted to lose weight (ALwO/caregiver Q208) or what most motivates adolescents to lose weight (HCP Q205). ALwO adolescents living with obesity, HCP healthcare professional. Figure adapted from Halford et al. [8]
The weight-loss barriers most frequently reported by ALwO were not being able to control hunger, lack of motivation, and enjoyment of unhealthy food. According to caregivers, not liking exercise, enjoying unhealthy food, and not being able to control their hunger were the most common weight-loss barriers for their ALwO (Fig. 4). Most HCPs agreed that unhealthy eating habits (93%), lack of exercise (90%), and a preference for unhealthy food (88%) were weight-loss barriers.
ALwO weight-loss barriers according to ALwO and caregivers (a) and HCPs (b). Proportion of participants who: selected each prespecified answer when asked what is keeping them/their child from losing weight (panel a: ALwO/caregiver Q210); and indicated they “strongly agree” or “somewhat agree” that each prespecified answer is a barrier to weight loss for their ALwO patients (panel b: HCP Q206). ALwO adolescents living with obesity, HCP healthcare professional. Figure adapted from Halford et al. [8]
Weight-loss attempts
HCPs thought only 41% of their ALwO patients had made a serious weight-loss attempt within the past year, with just 29% of these patients successful. A higher proportion of ALwO than caregivers reported a recent weight-loss attempt by the ALwO and that the ALwO was likely to attempt to lose weight within 6 months (Fig. 5).
ALwO weight-loss attempts. Proportion of participants who selected each prespecified answer (panel a: ALwO Q108a and caregiver Q110a; panel b: ALwO Q109 and caregiver Q111). In panel b, the “very likely” category includes the answers “very likely” and “extremely likely”, and the “not very likely” category includes the answers “not very likely” and “not likely at all.” Percentages may not sum to 100% due to rounding. ALwO adolescents living with obesity. Figure adapted from Halford et al. [8]
Weight-management methods
HCPs believed the most effective weight-management methods were becoming more physically active (86%), improving eating habits (79%), and reducing screen time (69%); these were also the methods that HCPs who discussed weight with ALwO most often recommended (58%, 57%, and 46% of HCPs, respectively).
The weight-management methods most frequently used by ALwO in the previous year were improving eating habits (37%) and being more physically active (30%); caregivers also reported these were their ALwO’s most commonly used methods (43% and 33%, respectively). Only 15% of ALwO said they had started a formal exercise program and only 13% had tried a specific diet/diet program; 6% had used over-the-counter weight-loss medication, 4% had taken prescription weight-loss medication, and 2% had tried weight-loss surgery.
Weight discussions
Although most ALwO felt they could talk honestly with their mother/father about their weight (62%), only 38% could with an HCP. Figure 6 shows barriers preventing weight discussions with HCPs.
ALwO and caregivers’ self-reported barriers to discussing weight with HCPs (a), HCPs’ self-reported barriers to discussing weight with ALwO (b), and HCPs’ perception of the barriers preventing ALwO from discussing weight with HCPs (c). Proportion of participants who selected each prespecified answer when asked: what prevents them from discussing their/their child’s weight with their/their child’s HCP (panel a: ALwO/caregiver Q425); why they might not discuss weight with ALwO patients (panel b: HCP Q413); and why their ALwO patients might not initiate conversations about their weight (panel c: HCP Q412). ALwO adolescents living with obesity, HCP healthcare professional. Figure adapted from Halford et al. [8]
HCPs generally reported feeling very/somewhat comfortable discussing weight with ALwO (93%). The factors that most frequently influenced whether HCPs initiate weight discussions were the patient’s mental/emotional state (62%), risk of developing new/additional obesity-related comorbidities (58%), BMI-for-age-and-sex (58%), and unhealthy lifestyle (58%).
Most ALwO (61%) and caregivers (73%) reported discussing their/their child’s weight with an HCP in the previous year; similarly, HCPs reported discussing weight with 72% of ALwO patients. Over half of ALwO (56%) and caregivers (55%) who had discussed weight with an HCP in the previous year reported that they started conversations about weight during HCP appointments, although HCPs felt they initiated discussions 55% of the time, on average. Equal proportions of ALwO thought that the responsibility for initiating weight discussions was with the HCP (44%) or themselves (44%); most HCPs (51%) thought this varied depending on the patient, although 23% felt HCPs should be responsible.
Only 36% of ALwO and 11% of caregivers reported that they/their child had received an obesity diagnosis, despite HCPs reporting they inform 86% of their ALwO patients/caregivers about the obesity diagnosis, on average.
Receptiveness to HCP interactions
Among ALwO (n = 543) and caregivers (n = 367) who reported no conversations about their/their child’s weight with HCPs in the previous year or reported that the HCP was not typically the initiator of weight conversations, most would like the HCP to initiate weight discussions during appointments (ALwO: 80%; caregivers: 86%). Similarly, among ALwO (n = 106) and caregivers (n = 88) who said the HCP usually started conversations about weight in the previous year, most liked that the HCP had raised the topic (ALwO: 80%; caregivers: 90%).
Among ALwO (n = 399) and caregivers (n = 330) who discussed the ALwO’s weight with an HCP in the previous year, most trusted the HCP’s weight-management advice (79% and 69%, respectively), agreed the HCP listened carefully when the ALwO talked about weight (78% and 67%), felt comfortable discussing weight with the HCP (72% and 67%), and agreed the HCP understood the difficulties of weight loss (74% and 61%). After their most recent weight conversations with HCPs, ALwO and caregivers had more positive than negative feelings overall, most often feeling motivated, supported, and hopeful (Fig. 7).
ALwO and caregivers’ feelings after their latest discussion with an HCP about weight. Proportion of participants who selected each prespecified answer (ALwO/caregiver Q410), among the subgroups of ALwO and caregivers who had discussed their/their child’s weight with an HCP in the prior year (per ALwO/caregiver Q201). The proportion of participants who selected at least one positive feeling (i.e., motivated, supported, hopeful, relieved, and/or surprised) is shown in the net positive category; the proportion of participants who selected at least one negative feeling (i.e., ashamed, confused, blamed, depressed, discouraged, and/or offended) is shown in the net negative category. ALwO adolescents living with obesity, HCP healthcare professional. Figure adapted from Halford et al. [8]
Information sources
The most important and frequently used sources of information about weight management for ALwO were family and friends (most important for 15%; used by 25%) and search engines (most important for 15%; used by 24%); caregivers’ top response was doctors (most important for 26%; used by 29%). HCPs’ most commonly used information sources were medical education programs (63%) and journal articles (58%).
Discussion
This analysis of ACTION Teens Italy data provides important insights into the barriers to effective obesity care for adolescents in Italy.
Although most ALwO surveyed in Italy were aware of the negative impact of obesity on health/well-being and correctly perceived their weight was above normal, one-third of ALwO and over half of caregivers were not aware that their/their child’s weight was above normal. This is not surprising, as previous research suggests most parents of children with obesity underestimate their child’s weight status [6]. This may be due to caregivers having an inaccurate personal reference of “weight normality” for their children [11, 12], which could lead to children acquiring the same inaccurate perception. Nevertheless, underestimation of weight status may explain why many ALwO and caregivers had not discussed the ALwO’s weight with an HCP. Additionally, caregivers’ common belief that ALwO will naturally slim down as they grow older/taller [13] may further contribute to reducing caregivers’ motivation to discuss their child’s weight with an HCP. Taken together, these findings suggest a need to provide information to caregivers about the natural course of obesity and its health implications [8].
The results of this analysis also indicate that ALwO in Italy are aware of the direct role they play in obesity management: most believed weight loss was entirely their responsibility. However, the discouraging results commonly reported following lifestyle intervention for obesity management [14] point to a need to implement techniques that engage and motivate ALwO to start and maintain a treatment program. It is therefore notable that ALwO and HCPs appeared to have differing perceptions of weight-loss motivators and barriers. For ALwO, the leading motivator was to be more fit/in better shape, whereas HCPs believed it was improving their social life. Additionally, ALwO identified their inability to control hunger as the leading barrier, but this was not among the top three barriers identified by HCPs (unhealthy eating habits, lack of exercise, and preference for unhealthy food). Of note, disrupted hunger/satiety regulation is a potent driver of body weight gain, and drugs restoring functionality of these disrupted pathways are effective in promoting weight loss [15, 16]. Therefore, increasing the ability to control hunger is likely an important treatment target. However, ALwO and HCPs’ differing perceptions of weight-loss motivators/barriers might affect weight-management strategies and reduce the chance of success. Although HCPs believed that lifestyle changes were most effective for weight management, only one in seven ALwO had tried a specific diet/diet program or started a formal exercise program, and very few had tried weight-loss medication/surgery. These findings underscore the need for further training on obesity for HCPs (as reported in recent guidelines [17]), in order to increase awareness of the biological basis of obesity [17] and the benefits of multidisciplinary treatment approaches [17, 18]. This is especially important given that only one-sixth of the HCPs surveyed had received > 1 day of advanced training in obesity with certification/evaluation.
Where misalignment was identified among ALwO, caregivers, and HCPs in Italy, lack of communication may have been a contributing factor, as many ALwO indicated they could not discuss their weight honestly with their mother/father and most could not do so with their HCP. Despite this, most ALwO would like HCPs to initiate weight discussions during appointments. Interestingly, HCPs indicated that the most important factor they consider when deciding whether to initiate weight discussions with ALwO/their caregivers is the adolescent’s mental/emotional state. Although HCPs’ attention to the psychological well-being of ALwO is important, it warrants further investigation; there is a need to determine the appropriate criteria for HCPs to consider when deciding when they should initiate weight discussions and inform ALwO/caregivers about the obesity diagnosis.
As expected, weight discussions with HCPs induced a mixture of positive and negative feelings in ALwO and caregivers, although many reported that they felt motivated, supported, and hopeful after discussing weight with the HCP. The first ALwO–HCP weight discussion may therefore play a crucial role in prompting ALwO to initiate and maintain a treatment program. This finding should encourage HCPs in Italy to be more actively involved in their patients’ weight management. Nevertheless, HCPs should not overlook the impact of negative feelings, as they could potentially discourage ALwO from discussing weight with HCPs in future. It is therefore crucial for HCPs to acquire the skills needed to motivate ALwO and have discussions about weight management in a caring, supportive, and non-judgmental way [19].
This analysis also provided further evidence that search engines are frequently used by ALwO to obtain health information [20, 21]. Unfortunately, most of the information available online is not scientifically certified and can be misleading [21]. As such, scientific societies and healthcare authorities should ensure adequate information, communicated in a simple and captivating way, is available on web channels used by adolescents.
Based on our findings, we propose several strategies to overcome difficulties in obesity management in adolescence: (i) increase awareness of the biological basis of obesity among ALwO, caregivers, and HCPs, as well as the general public and the Italian government, as there is a need for obesity to be recognized as a chronic, relapsing, and progressive disease that deserves appropriate management; (ii) increase the level of training provided to HCPs on the clinical management of obesity in children and adolescents based on the latest treatment guidelines, emphasizing the need to diagnose obesity early and initiate appropriate therapy using effective evidence-based treatments; (iii) modify the commonly held but inaccurate belief that obesity treatment is completely the responsibility of the ALwO, for example, by increasing awareness among HCPs that weight conversations with ALwO and caregivers should be initiated early and sensitively.
Strengths and limitations
Strengths of this analysis include the use of data from ALwO, caregivers, and HCPs involved in obesity management/treatment to gain a multistakeholder perspective on adolescent obesity, and the stratified sampling method that was used to recruit ALwO and caregivers who were representative of their counterparts in the wider Italian population.
Limitations of the ACTION Teens study include the cross-sectional design and use of self-reported weight and height to calculate BMI [8]. Additionally, the HCP response rate may have reduced the representativeness of the HCPs surveyed in Italy, although the response rate in Italy was higher than in the ACTION Teens global analysis [8].
Conclusion
In conclusion, we identified several potential barriers to effective obesity care for adolescents in Italy. First, the caregivers surveyed appeared to underestimate the weight of their ALwO and assumed their ALwO would naturally slim down with age, while ALwO assumed excessive personal responsibility for weight loss. This highlights a need to provide more information about obesity and its management to ALwO and caregivers. Second, the HCPs surveyed were not aligned with ALwO regarding the top weight-loss motivators and barriers, and many ALwO experienced negative feelings after discussing weight with an HCP. This suggests a need to improve the quality of communication between ALwO and HCPs, for example, by offering advanced training on obesity management to HCPs. Third, the internet appears to be a key information source for ALwO, which underscores the need for new education/communication strategies.
What is already known on this subject?
-
The prevalence of obesity among children and adolescents is high in Italy; there is an urgent need for early diagnosis and treatment.
-
An international study conducted in 10 countries demonstrated there is misalignment among ALwO, their caregivers, and the HCPs who treat them regarding obesity care and management.
What this study adds?
-
This is the first comprehensive description of the perceptions, attitudes, and behaviors of ALwO, caregivers, and HCPs in Italy.
-
This analysis is also the first to explore how ALwO, caregivers, and HCPs in Italy communicate regarding obesity; the results suggest a need for new strategies to improve the quality of communication.
-
Finally, this analysis demonstrates there is a need to disseminate information about obesity to ALwO, caregivers, and HCPs in Italy; we recommend utilizing web-based communication channels for adolescents and offering additional training programs to HCPs.
Data availability
Data will be shared with bona fide researchers submitting a research proposal approved by the independent review board. Individual participant data will be shared in data sets in a de-identified and anonymized format. Data will be made available after research completion. Information about data access request proposals can be found at novonordisk-trials.com.
References
Spinelli A, Buoncristiano M, Nardone P et al (2021) Thinness, overweight, and obesity in 6- to 9-year-old children from 36 countries: the World Health Organization European Childhood Obesity Surveillance Initiative—COSI 2015–2017. Obes Rev 22:e13214. https://doi.org/10.1111/obr.13214
Nicolucci A, Maffeis C (2022) The adolescent with obesity: what perspectives for treatment? Ital J Pediatr 48:9. https://doi.org/10.1186/s13052-022-01205-w
Pont SJ, Puhl R, Cook SR, Slusser W, Section on Obesity, The Obesity Society (2017) Stigma experienced by children and adolescents with obesity. Pediatrics 140:e20173034. https://doi.org/10.1542/peds.2017-3034
Correa-Burrows P, Rogan J, Blanco E et al (2021) Resolving early obesity leads to a cardiometabolic profile within normal ranges at 23 years old in a two-decade prospective follow-up study. Sci Rep 11:18927. https://doi.org/10.1038/s41598-021-97683-9
Marcus C, Danielsson P, Hagman E (2022) Pediatric obesity—long-term consequences and effect of weight loss. J Intern Med 292:870–891. https://doi.org/10.1111/joim.13547
Ramos Salas X, Buoncristiano M, Williams J et al (2021) Parental perceptions of children’s weight status in 22 countries: the WHO European Childhood Obesity Surveillance Initiative: COSI 2015/2017. Obes Facts 14:658–674. https://doi.org/10.1159/000517586
Belay B, Frintner MP, Liebhart JL et al (2019) US pediatrician practices and attitudes concerning childhood obesity: 2006 and 2017. J Pediatr 211:78–84.e72. https://doi.org/10.1016/j.jpeds.2019.04.030
Halford JCG, Bereket A, Bin-Abbas B et al (2022) Misalignment among adolescents living with obesity, caregivers, and healthcare professionals: ACTION Teens global survey study. Pediatr Obes 17:e12957. https://doi.org/10.1111/ijpo.12957
EphMRA (2023) EphMRA Code of Conduct/AER. https://www.ephmra.org/code-conduct-aer. Accessed 8 Feb 2024
World Health Organization (2007) Growth reference data: BMI-for-age (5–19 years). https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age. Accessed 8 Feb 2024
Binkin N, Spinelli A, Baglio G, Lamberti A (2013) What is common becomes normal: the effect of obesity prevalence on maternal perception. Nutr Metab Cardiovasc Dis 23:410–416. https://doi.org/10.1016/j.numecd.2011.09.006
Hansen AR, Duncan DT, Tarasenko YN, Yan F, Zhang J (2014) Generational shift in parental perceptions of overweight among school-aged children. Pediatrics 134:481–488. https://doi.org/10.1542/peds.2014-0012
Wu Y, Ma X, Fraser WD et al (2021) Caregivers’ perceptions, challenges and service needs related to tackling childhood overweight and obesity: a qualitative study in three districts of Shanghai, China. BMC Public Health 21:768. https://doi.org/10.1186/s12889-021-10744-6
Al-Khudairy L, Loveman E, Colquitt JL et al (2017) Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev 6:CD012691. https://doi.org/10.1002/14651858.Cd012691
Kelly AS (2023) Current and future pharmacotherapies for obesity in children and adolescents. Nat Rev Endocrinol 19:534–541. https://doi.org/10.1038/s41574-023-00858-9
Alcantara IC, Tapia APM, Aponte Y, Krashes MJ (2022) Acts of appetite: neural circuits governing the appetitive, consummatory, and terminating phases of feeding. Nat Metab 4:836–847. https://doi.org/10.1038/s42255-022-00611-y
Hampl SE, Hassink SG, Skinner AC et al (2023) Executive summary: clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 151:e2022060641. https://doi.org/10.1542/peds.2022-060641
Maffeis C, Olivieri F, Valerio G et al (2023) The treatment of obesity in children and adolescents: consensus position statement of the Italian society of pediatric endocrinology and diabetology, Italian Society of Pediatrics and Italian Society of Pediatric Surgery. Ital J Pediatr 49:69. https://doi.org/10.1186/s13052-023-01458-z
Ananthakumar T, Jones NR, Hinton L, Aveyard P (2020) Clinical encounters about obesity: systematic review of patients’ perspectives. Clin Obes 10:e12347. https://doi.org/10.1111/cob.12347
Freeman JL, Caldwell PHY, Bennett PA, Scott KM (2018) How adolescents search for and appraise online health information: a systematic review. J Pediatr 195:244–255.e1. https://doi.org/10.1016/j.jpeds.2017.11.031
Armstrong M, Halim NK, Raeside R et al (2021) How helpful and what is the quality of digital sources of healthy lifestyle information used by Australian adolescents? A mixed methods study. Int J Environ Res Public Health 18:12844. https://doi.org/10.3390/ijerph182312844
Acknowledgements
We gratefully acknowledge the study participants and personnel involved. We thank Andrea Stoltz, Nick Henderson, Peg Jaynes, Rebecca Hahn, and Lynn Clement of KJT Group for data collection and analysis. Medical writing support was provided by Lauren McNally, MSci, of Apollo, OPEN Health Communications, and funded by Novo Nordisk A/G, in accordance with Good Publication Practice (GPP) guidelines (www.ismpp.org/gpp-2022).
Funding
Novo Nordisk A/G funded the ACTION Teens study and the provision of medical writing assistance for this article. Novo Nordisk A/G also paid the article processing charge for this article.
Author information
Authors and Affiliations
Contributions
Claudio Maffeis is a member of the ACTION Teens Steering Committee and thus contributed to the study design. All authors contributed to data interpretation, participated in drafting and revising this article, and approved the final article.
Corresponding author
Ethics declarations
Ethics approval
ACTION Teens was conducted in compliance with the Declaration of Helsinki. In Italy, approval was granted by the Ethics Committee for Clinical Trials at Integrated University Hospital Verona (Verona, Italy) on August 9, 2021 (Protocol number: 46600).
Informed consent
Respondents (plus parents/legal guardians of ALwO) gave informed consent to participate.
Competing interests
Claudio Maffeis received consultancy fees from Novo Nordisk for his role as a member of the ACTION Teens Steering Committee during the conduct of the study; he also reports honoraria (for lectures) from Aboca, Eli Lilly, Novo Nordisk, Roche, and Sanofi, and participation in advisory boards for Abbott, Eli Lilly, Medtronic, and Sanofi outside the submitted work. Luca Busetto reports honoraria (for lectures) from PronoKal and Rhythm Pharmaceuticals, and participation in advisory boards for Bruno Farmaceutici, Eli Lilly, Novo Nordisk, and Pfizer outside the submitted work. Malgorzata Wasniewska is a consultant for Merck, Novo Nordisk, Pfizer, and Sandoz. Daniele Di Pauli and Andrea Lenzi have no relevant financial/non-financial interests to disclose. Carla Maccora is a permanent employee of Novo Nordisk.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maffeis, C., Busetto, L., Wasniewska, M. et al. Perceptions, attitudes, and behaviors among adolescents living with obesity, caregivers, and healthcare professionals in Italy: the ACTION Teens study. Eat Weight Disord 29, 35 (2024). https://doi.org/10.1007/s40519-024-01663-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40519-024-01663-7