Abstract
Aim
Eating disorders have a serious impact on quality of life, especially when combined with Type 1 diabetes. We investigated eating disorders in relation to factors early in life with some focus on Type 1 diabetes.
Methods
Out of 21,700 children born 1st of Oct 1997–1st of Oct 1999 17,055 (78.6%) were included in ABIS (All Babies in southeast Sweden) and 16,415 had adequate questionnaires. ICD-10 diagnosis from The National Patient Register was merged with the ABIS data.
Results
In total 247 individuals, 19 boys (7.7%) and 219 girls (92.3%) out of 16,415 (1.5%) developed eating disorders (EDs), 167 (1.0%) Type 1 diabetes of whom 7 (4.2%) also got eating disorders (ED) (OR 3.25 (1.47–7.28); p = 0.04), all of them years after diagnosis of Type 1 diabetes. EDs was associated with high parental education especially in fathers (OR 1.65 (1.09–2.50); p = 0.02) and to at birth anxiety, and depression among mothers. There was no association with the duration of breastfeeding.
Conclusions
Eating disorders are common in girls, with increased risk in high-educated but psychologically vulnerable families. Prevalence is increased in type 1 diabetes. Even modern diabetes treatment needs to be completed with psychological support.
Level of evidence
Level III: Evidence obtained from well-designed cohort or case–control analytic studies.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Eating disorders are characterized by a divergent relation to food and eating, or an excessive focus on body weight and weight control [1, 2]. In the general population, eating disorders are associated with extensive co-morbidity and more than 70% of those with eating disorders have an additional psychiatric diagnosis [2]. Most common are mood and anxiety disorders, personality disorders, neurodevelopment disorders, or disorders, including the use of alcohol or drugs [2].
There is a lack of knowledge from longitudinal prospective studies on how early factors in life influence the development of eating disorders in children, beside an increased risk for eating disorders in premature children and with older parents [3]. We, therefore, decided to use the prospective birth cohort ABIS (All Babies in Southeast Sweden) to analyze how psychosocial situation and early lifestyle may contribute to anorexia nervosa and bulimia during the following 20 years of life,
Eating disorders have a serious impact on quality of life for anybody but especially when combined with type 1 diabetes when it causes increased mortality [4]. Thus, one study showed 38% mortality in a group of patients with both type 1 diabetes and anorexia nervosa, which is five times higher mortality than with anorexia nervosa alone [4]. The increased mortality may be caused by weight loss in combination with omitted insulin doses, keto-acidosis, and hyperglycemia [5]. The increased prevalence of eating disorders in adolescents with type 1 diabetes has been estimated to be 6–8% (lifetime prevalence 10.3–14.0%) [6], even though the typical anorexia nervosa, according to some studies, may not be more common in patients with type 1 diabetes than in the general population. Eating disorders have usually been regarded as a consequence of having type 1 diabetes, decreasing quality of life [6]. With more restrictive dietary rules for patients with type 1 diabetes eating disorders were supposed to be a quite common consequence decades ago, but one would expect that this complication has become rare as modern treatment allows a less strict diet. However, the prevalence of eating disorders may still be high as intense insulin treatment is based on carbohydrate counting, in practice “diet”, and food habits are still an important part of type 1 diabetes treatment. Furthermore, there are studies suggesting that the association between eating disorders and autoimmune diseases may be complex, and that eating disorders actually may forego the diagnosis of autoimmune diseases, and in some way contribute to the development of, e.g., type 1 diabetes and not only be a consequence of dietary treatment [7]. Previous studies of eating disorders in type 1 diabetes are mainly based on cross-sectional associations. In this prospective study, we elucidate this question further by also investigating when eating disorders develop in patients with celiac disease, another autoimmune disease with dietary rules as an important part of treatment.
The aim of our study was, therefore, primarily to analyze how psychosocial factors in early life may contribute to eating disorders, especially anorexia nervosa, during the following 20 years of life, but secondary also to investigate the association between these disorders and type 1 diabetes or celiac disease.
Materials and methods
Our data derive from the longitudinal prospective population-based birth cohort study ABIS (All Babies in Southeast Sweden). All 21,700 mothers who gave birth to a child between 1st of October 1997 and the 1st of October 1999 were asked to participate in the ABIS study and 17 055 (78.6) did so, giving a study population which has been shown to be well-representative of the general Swedish population. ABIS was designed to identify environmental and genetic factors associated with development of immune-mediated, especially type 1 diabetes and other autoimmune diseases. Questionnaires were answered by parents at the birth of their child and then 1, 2.5–3, and 5 years later. At 8 and at 10–12 years, separate questionnaires were answered by both children and parents, and at 17–19 years by the teenagers. At every follow-up, several biological samples were collected. In total, 16,415 ABIS individuals could be included in this study with adequate questionnaires. National register data based on medical records and ICD-10 diagnosis from The Swedish National Board of Health and Welfare were merged with the ABIS data. The diagnoses of anorexia nervosa (F50.0, F50.8, F50.9), Bulimia (F50.2) type 1 diabetes (E10), celiac disease (K90), depression (F39.1) and anxiety (F42.1) were collected from the national register.
The control group consists of 16,168 participants in the study without any of the four F50.0, F50.8, F50.9 and F50.2 diagnoses.
The following variables were used derived from the questionnaires at birth: age of mothers at birth, educational level, family composition, and number of siblings. From the questionnaire answered at 1 year of age we included duration of breastfeeding, which might influence both contacts between mother and child, and influence the gut microbiome, and from the questionnaire at 2.5–3 years, we included early symptoms of dysbiosis (stomach ache or vomiting). Household income of the family is based on information from year 2000, in terms of the family income available after taxation, collected from Statistics Sweden and divided into the quintiles low, quite low, middle, quite high, and high. Further description of variables from the questionnaires is given in Appendix.
Statistics
Statistical analyses were made in IBM SPSS Statistics 28.0. Chi-squared test was used to compare the variables for the cases and controls. Multiple multivariate binary regressions were performed to assess the relationship and risks (OR, 95% CI) between the dependent variable, eating disorder compared to the control group. Variables for multivariate binary regression analyses were selected based on significant values in univariate analyses using Chi-squared and correlations tests. A p value less than 0.05 was statistically significant.
Results
In total 247 individuals, 19 boys (7.7%) and 219 girls (92.3%) out of 16,415 (1.5%) developed eating disorders (probands), 167 (1.0%) developed type 1 diabetes of whom 7 (4.2%) also eating disorders (OR 3.25 (1.47–7.28); p = 0.04) and 228 (1.4%) developed celiac disease of whom 6 (2.6%) also eating disorders. Parental educational level was significantly higher in probands, especially so in the fathers (Table 1). Mothers of probands reported already at birth of the probands health problems such as anxiety, and depression but also type 2 diabetes more frequently than the control group. There was no association with the duration of breastfeeding, but early symptoms of vomiting were more frequent among the probands. There was no association between development of eating disorders and BMI of their parents at repeated follow-ups (1, 2.5–3, 5 and 8 years of age).
Comorbidities of probands are shown in Table 2. Compared to the controls, the probands had more often also been diagnosed with anxiety (17.2% versus 2.7%) (p < 0.001), depression ((10.1% versus 2.4%) (p < 0.001), and type 1 diabetes (2.9% versus 0.99%) (p = 0.004).
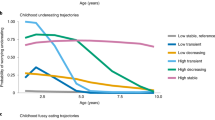
Age at diagnosis of type 1 diabetes, anorexia nervosa, bulimia, and celiac disease is shown in Fig. 1. A majority (62.5%) of individuals with both depression and eating disorders got their two diagnoses the same year and half of the cases with anxiety (51.2%) and eating disorders. However, all type 1 diabetes individuals got their diagnosis of anorexia nervosa or bulimia years after they had got the type 1 diabetes diagnosis. Similarly, in individuals with both celiac disease and eating disorder; all the patients got the celiac disease diagnosis years before the eating disorder.
Multiple logistic regression of factors associated with eating disorder diagnoses is shown in Table 3. Thus, it is evident that high paternal education as well as factors such as depression and anxiety in the children with ED remain significantly related to the risk of developing eating disorders.
Discussion
In the general population, eating disorders are rather common, mainly in girls. We find early life risk factors in addition to earlier results [3]. Already at birth of the child, mothers of children who later develop eating disorders (the probands) more often had reported anxiety and/or depression, which may indicate a more psychologically vulnerable family. One can speculate that the increased risk of eating disorders in children of parents with high education, in agreement with earlier findings of connection between anorexia and higher socioeconomic status [8], is related to higher expectations which may become an extra burden for the child. That vomiting was reported more often already at 3 years of age in the probands may suggest a disposition to gastrointestinal problems.
Comorbidity with anxiety and depression underlines that eating disorders are part of broader psychological problems, and even the most modern treatment of Type 1 diabetes needs to be completed with psychological support not least in high-educated families with history of earlier psychological problems.
Still with modern quite successful diabetes treatment, eating disorders are more common in individuals with type 1 diabetes, and somewhat more common also in patients with celiac disease. It has been suggested that there is a non-genetic association between eating disorders and autoimmune diseases, especially type 1 diabetes, with increased prevalence of eating disorders already before diagnosis of type 1 diabetes [7], but in our study, there is no such indication. All individuals with eating disorders got their diagnosis years after their diagnosis of type 1 diabetes resp celiac disease, suggesting that the eating disorders in young individuals are a consequence of having type 1 diabetes and/or celiac disease. In type 1 diabetes, it is well-known that the patients, usually teenagers or young adults sometimes deliberately omit insulin to lose weight, or restrict their eating, or alternate between vomiting and binge eating. That eating disorders also are quite common in individuals some years after the diagnosis of celiac disease suggests that the dietary rules may contribute to eating disorders, even if it may be so that people who get their celiac disease diagnosed in adulthood may have had problems with food intake and eating disorders before their celiac disease was discovered [9]. Connections between anorexia nervosa and autoimmune/inflammatory disorders, e.g., inflammatory bowel disease may be explained by similar mechanisms [10].
Strength and limitations
This study has several strengths with the prospective follow-up from birth of a large general population and can therefore give reliable information on the importance of early factors in life for the development of eating disorders. However, there are limitations with regard to development of eating disorders in type 1 diabetes, as the numbers inevitably are small with only 7 cases with that combination in a population of 17,000 individuals. However, as all cases got their eating disorder several years after their diagnosis of type 1 diabetes, that picture seems rather robust. Another limitation could be use of only the birth questionnaire concerning demographic variables, which might have changed during the follow-ups. However, the focus of our study was to study the importance of factors early in life.
Conclusions
Factors early in life may contribute to development of eating disorders many years later. Anorexia nervosa and Bulimia are especially common in individuals with type 1 diabetes, with onset several years after type 1 diabetes is diagnosed, suggesting that type 1 diabetes and its treatment causes this dangerous combination. Celiac disease shows a similar relationship. Even modern diabetes treatment needs to be completed with psychological support, not least in high-educated families with history of earlier psychological problems.
What is already known on this subject?
Associations to socioeconomic status and development of eating disorders are shown earlier, but there is lack of knowledge about the importance of factors early in life from prospective studies with long-term follow-up. That type 1 diabetes is associated with development of eating disorders is known.
What this study adds?
Already at birth of the child mothers of children who later develop eating disorders more often had reported anxiety and/or depression, and there is an increased risk of eating disorders in children of parents with high education. Still with modern treatment of type 1 diabetes prevention of eating disorders needs early psychological support, especially in families with high educated parents with previous psychological symptoms.
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EDs:
-
Eating Disorders
- T1D:
-
Type 1 diabetes
- HbA1c:
-
Haemoglobin A1c
- OR:
-
Odds Ratio
- ABIS:
-
All Babies in Southeast Sweden
References
Young V, Eiser C, Johnson B, Brierley S, Epton T, Elliott J et al (2013) Eating problems in adolescents with type 1 diabetes: a systematic review with meta-analysis. Diabet Med 30:189–198
Treasure J, Duarte TA, Schmidt U (2020) Eating disorders. Lancet 395(10227):899–911
Larsen JT, Bulik CM, Thornton LM, Koch SV, Petersen L (2021) Prenatal and perinatal factors and risk of eating disorders. Psychol Med 51(5):870–880. https://doi.org/10.1017/S00332917190039
Nielsen S, Emborg C, Molbak AG (2002) Mortality in concurrent type 1 diabetes and anorexia nervosa. Diabetes Care 25:309–212
Bermudez O. Diabetes and eating disorders. Audio Dig Fam Pract. 2013; 62. www.audiodigest.org/adfwebcasts/pdfs/fp6102.pdf.
Winston AP (2020) Eating disorders and diabetes. Curr Diab Rep 20(8):32. https://doi.org/10.1007/s11892-020-01320-0
Raevuori A, Haukka J, Vaarala O, Suvisaari JM, Gissler M, Grainger M et al (2014) The increased risk for autoimmune diseases in patients with eating disorders. PLoS ONE 9(8):e104845. https://doi.org/10.1371/journal.pone.0104845)
Koch SV, Larsen JT, Plessen KJ, Thornton LM, Bulik CM, Petersen LV (2022) Associations between parental socioeconomic-, family-, and sibling status and risk of eating disorders in offspring in a Danish national female cohort. Int J Eat Disord 55(8):1130–1142. https://doi.org/10.1002/eat.23771
Mårild K, Størdal K, Bulik CM, Rewers M, Ekbom A, Liu E et al (2017) Celiac disease and anorexia nervosa: a nationwide study. Pediatrics 139(5):e20164367. https://doi.org/10.1542/peds.2016-4367
Zerwas S, Larsen JT, Petersen L, Thornton LM, Quaranta M, Koch SV et al (2017) Eating disorders, autoimmune, and autoinflammatory disease. Pediatrics 140(6):e20162089. https://doi.org/10.1542/peds.2016-2089
Acknowledgements
We are grateful to all ABIS individuals and their parents who answered the questionnaires.
Funding
Open access funding provided by Linköping University. ABIS was supported by Barndiabetesfonden (the Swedish Child Diabetes Foundation); Swedish Council for Working Life and Social Research, Grant/Award Numbers: FAS2004-1775, FAS2004–1775; Swedish Research Council, Grant/Award Numbers: K2005-72X-11242-11A and K2008-69X-20826-01-4, K2008-69X-20826-01-4; Östgöta Brandstodsbolag; Medical Research Council of Southeast Sweden (FORSS); JDRF Wallenberg Foundation, Grant/Award Number: K 98-99D-12813-01A; ALF-and LFoU grants from Region Östergötland and Linköping university, Sweden and Joanna Cocozza Foundation.
Author information
Authors and Affiliations
Contributions
JL created ABIS and conceptualized and designed this study, drafted the initial manuscript, and critically reviewed and revised the manuscript. Ass professor ÅOF made the statistical analyses, the Tables and the Figure and critically reviewed and revised the manuscript. Both authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Research Ethics Committees of the Faculty of Health Science at Linköping University Sweden have given an ethical approvement to the ABIS study. Dnr. 287–96, 2011/52-53 and 2003–092. The parents of the participating children gave informed consent to participate in the ABIS-study after being provided oral, written, or video information. Participants were free to opt in or out of the study whenever they wanted to.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ludvigsson, J., Olsen Faresjö, Å. The importance of factors early in life for development of eating disorders in young people, with some focus on type 1 diabetes. Eat Weight Disord 29, 5 (2024). https://doi.org/10.1007/s40519-023-01633-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40519-023-01633-5