Abstract
Purpose of Review
In recent years, much attention has focused on the role of poor oral health in the development or worsening of systemic diseases, including COVID-19. The mouth is an important site of cellular infection early in the disease course of COVID-19. We review how oral pathology, and specifically viral infection within the oral cavity, may mediate the disease severity and duration of COVID-19. In particular, the previously reported model of SARS-CoV-2 vascular delivery from the mouth to the lungs via the bloodstream is revisited.
Recent Findings
We previously proposed that an oral-vascular-pulmonary route of infection could facilitate severe lung disease in COVID-19. This pathway could also explain the vital link between periodontitis and COVID-19 severity, including higher mortality risk. This model of pathogenesis is reconsidered in light of recent findings regarding the involvement of the mouth as a viral reservoir, and pathological processes in the blood, pulmonary vasculature, and elsewhere in the body. Oral dysbiosis in COVID-19 and the effect of oral hygiene in mitigating disease severity are discussed. The evidence for viral persistence in the mouth and intravascular viral passage from the mouth to the rest of the body via blood is also discussed in the context of post-acute COVID (long COVID).
Summary
High viral load in the mouth and poor oral health status are associated with COVID-19 disease severity, increasing the risk of death. Pathophysiological links between viral activity in the mouth, oral health status, and disease outcome in the lungs and blood provide a rationale for further evaluation of the oral-vascular-systemic pathway in patients with acute COVID-19 and long COVID. The potential benefits of oral hygiene protocols and periodontal procedures in COVID-19 also warrant further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The connection between oral dysbiosis and the development of systemic diseases is an important emerging field of research. Oral dysbiosis and periodontal diseases are linked directly with the development and/or complications of multiple systemic diseases [1], including type II diabetes [2, 3], cardiovascular disease [4], neurodegenerative diseases [5, 6], and rheumatoid arthritis [7, 8]. Oral organisms have been directly implicated in the pathophysiology of these conditions and in haematological disorders of platelet activation [9], leukocyte production [10], and endothelial dysfunction [11]. A simple anatomical model suggests that specific periodontal pathogens disseminate intravascularly from the subgingival biofilm to other body parts via the bloodstream, impacting the development and progression of systemic diseases. Previously, we proposed an ‘oral-vascular-pulmonary’ route of SARS-CoV-2 infection as a central mechanism in developing acute COVID-19 lung disease, thus framing periodontal disease as a primary risk factor for severe COVID-19 [12]. This review highlights the role of the mouth in this disease model, specifically as a site of viral entry, replication, reservoir formation, and subsequent transfer to the blood. The evidence for the contribution of this anatomical route to severe COVID-19 lung disease is presented, focusing on vascular pathological processes and viral-endothelial interactions in acute and post-acute phases of COVID-19. The impact of poor oral health status, oral hygiene measures, and periodontal therapy on COVID-19 severity are also reviewed.
The Oral-Vascular-Pulmonary Infection Route
Others have hypothesised that the association between periodontitis and increased severity of acute COVID-19 is mediated by oral biofilm overgrowth, predisposing to the adverse effects of aspiration into the airways. [13]. However, because of the distinct vascular pattern of COVID-19 lung disease and the lack of airway inflammation—unlike conventional viral pneumonia [14]—we previously proposed an anatomical oral-vascular-pulmonary route of infection from the upper respiratory tract as the potential main driver of lung parenchymal damage [12] (Fig. 1). Although viral entry into the bloodstream via both the nasal and oral mucosa is possible, viral escape into the blood predominantly from the mouth, rather than the nose, provides the most likely explanation for the increased risk of severe COVID-19 linked to periodontitis. The steps of this proposed pathway are discussed herein with reference to new literature on pathological processes in the mouth, blood, and lungs for acute and long COVID.
Summary of the oral-vascular-pulmonary model of viral transfer. A Initial viral infection of epithelial lining of the upper respiratory tract mucosa (nose and mouth). B Viral reservoir formation in the mouth (saliva, gingival crevicular fluid, dental plaque, periodontal tissues, salivary glands). C Transfer of viral particles/elements into the gingival venous drainage facilitated by micro-ulceration of the sulcular/pocket-lining epithelium due to gingivitis or periodontitis. D Intravascular passage of viral particles/elements from the venous drainage of the mouth to the neck and chest veins (jugulars and superior vena cava), the right side of the heart (E), and into the pulmonary circulation via the pulmonary artery (F), dominantly in the highly vascularized gravity-dependent lung peripheries. G Direct interaction of viral particles/elements with endothelial cells of the pulmonary microvasculature, with intravascular pro-coagulant and pro-inflammatory viral interactions leading to endothelial dysfunction, vasoconstriction and intravascular thrombosis (immunothrombosis) (H). I Normal capillary network. J Vascular congestion and impaired lung perfusion leading to lung damage, dominantly in the lung peripheries, with upstream pulmonary arteriovenous (AV) shunting, with dilated proximal blood vessels, thus explaining preservation of physiological dead space in the airways and ‘silent hypoxemia’
Acute COVID-19
Acute COVID-19: Pathogenesis in the Oral Cavity
The upper respiratory tract is the first site of viral entry and replication of SARS-CoV-2, with ACE2 receptors expressed 200–700 times more intensely in the nasal passages than in the airways of the lungs [15]. The mouth is also an initial entry site with multiple oral epithelial cell types susceptible to infection and replication [16]. Viral load in the mouth can reach 108/ml of saliva [17], and SARS-CoV-2 saliva detection is more sensitive than nasal or nasopharyngeal swab sampling [18,19,20], with 84.2% sensitivity for salivary rt-PCR compared with only 9.5% for nasopharyngeal and throat swabs on paired sampling [18,19,20]. Notably, high viral load in saliva has been reported to predict poor outcomes and mortality in acute COVID-19 more accurately than patient age, irrespective of the nasopharyngeal viral load [21].
Multiple studies have shown periodontitis to be a risk factor for disease severity in acute COVID-19 [22,23,24,25]. An odds ratio for death from COVID-19 of 8.81 has been reported in those with periodontal bone loss [22]. Another study demonstrated odds ratios for hospitalisation, need for mechanical ventilation, and death of 36.52, 7.45, and 14.58 respectively, in COVID-19 patients with clinically confirmed severe periodontitis [23]. Compared to survivors, deceased patients presented with deeper periodontal pockets, worse clinical attachment loss, and gingival recession [23]. Other studies corroborate the increased risk of severe COVID-19 in periodontitis patients [26,27,28,29,30]. Dental plaque and gingival crevicular fluid can harbour SARS-CoV-2 [31, 32], pointing to the oral cavity as a viral reservoir in acute COVID-19.
Oral Dysbiosis/Oral Microbiome in Acute COVID-19
Over the last few years, evidence has emerged regarding the link between oral dysbiosis and systemic diseases [33]. Even the mildest forms of COVID-19 confined to the upper respiratory tract can reflect oral dysbiosis, as SARS-CoV-2 can reach high concentrations in saliva [17]. Evidence for the connection between acute COVID-19 and oral dysbiosis emerges from studies showing altered spectra of oral and gut microorganisms in COVID-19 patients [34,35,36]. In a cross-sectional study, oral dysbiosis was associated with more severe COVID-19 symptoms [37]. SARS-CoV-2 has also been suggested to be a bacteriophage, potentially altering the composition of the microbiome [38].
Oral Manifestations of Acute COVID-19
Altered taste is a common symptom of COVID-19 [39], possibly resulting from direct viral infection of mucosal epithelial cells—specifically of minor salivary glands of the tongue surface [16, 40]—and positively correlates with salivary viral load [16]. Histological findings show papillary inflammation and destruction of taste buds in COVID-19, with infection of the tongue and gingival tissues [39, 41]. Other oral manifestations of COVID-19 are common [42], and could be considered intrinsic to disease pathogenesis.
Oral Immune Barrier, Periodontitis, and Acute COVID-19
The oral mucosa is an immune defence barrier, providing physical and antimicrobial protection in healthy individuals through the beneficial effects of a health-promoting oral microbiome. Oral pathogens or toxins can more readily enter the body via the bloodstream when this barrier is compromised [43,44,45]. Simple actions like toothbrushing can result in transient bacteraemia in those with a healthy mouth [43,44,45], or even chewing in those with periodontitis [45]. Therefore, high titres of SARS-CoV-2 in a healthy mouth could result in viral entry into the bloodstream and to a greater degree in those with periodontal disease.
Periodontitis is strongly associated with chronic inflammatory diseases, such as type-2 diabetes mellitus, atherogenic cardiovascular disease, chronic kidney disease, inflammatory lung diseases, cognitive decline, and rheumatoid arthritis [1,2,3,4,5,6,7,8, 46, 47]. Periodontitis plays a role in the worsening of systemic inflammation by cytokine production and recruitment of primed polymorphonuclear neutrophils [48, 49]. Inflammatory cytokines in periodontitis have been hypothesised to contribute to COVID-19 severity [50, 51]. However, the degree to which oral disease contributes to the overall cytokine burden in acute COVID-19 has not been established. We propose that direct viral translocation from the mouth to the blood could constitute a significant disease mechanism.
Acute COVID-19: Translocation of SARS-CoV-2 from the Mouth to Blood
Considering the oro-systemic link and the impact of periodontitis upon the systemic environment, it is crucial to appreciate existing evidence for the translocation of specific pathogens to other body parts. For example, the periodontal pathogen Porphyromonas gingivalis (P. gingivalis) has been implicated in the pathogenesis of multiple systemic diseases. It has been identified in the brain of individuals with Alzheimer’s disease, confirming its ability to cross the blood–brain barrier [52]. Findings from animal studies suggest it contributes to amyloid production, the underlying pathological driver of Alzheimer’s [53]. P. gingivalis can translocate to the vascular endothelium, being implicated in atheroma formation and instability in cardiovascular disease [4]. The DNA of P. gingivalis has also been found in the synovium of rheumatoid arthritis patients, with potential involvement in the production of anti-citrullinated protein autoantibodies, which mediate rheumatoid arthritis pathology [54]. Given that oral microbes can be transferred systemically, it is plausible that periodontitis facilitates the translocation of SARS-CoV-2 from oral reservoirs via the bloodstream to the lungs and elsewhere in the body.
Inhabitants of the oral microbiome, such as Streptococcus viridans species, are primary pathogens of infective endocarditis [55, 56]. Their translocation to the heart valves in endocarditis provides further plausibility to the proposed oral-vascular-pulmonary infection route for SARS-CoV-2.
Acute COVID-19: Pathogenesis in the Lungs
Any pathogen that evades the oral immune response can enter gingival blood vessels, reaching the jugular veins, superior vena cava, right atrium, right ventricle, and subsequently the pulmonary vessels. Following this oral-vascular-pulmonary infection route, a pathogen would encounter its first capillary bed in the lungs. Pulmonary arteries predominantly vascularize gravity-dependent areas of the lungs. Slower flow of blood through these peripheral parts of the lower lungs results in increased interaction between circulating pathogens and the pulmonary vascular bed [57]. Thus, viral delivery via this route would explain the distinct vascular phenomena affecting the peripheral, posterior, and lower parts of the lungs in acute COVID-19 [12, 14, 58,59,60,61].
A conventional understanding of the pathogenesis of acute COVID-19 suggests viral inhalation into the lungs, causing respiratory pneumonia. Although SARS-CoV-2 does infect lower respiratory tract cells [62], the disease is not characterized by inflammation of the lung airways [63], suggesting that COVID-19 lung disease pathogenesis significantly differs from influenza and influenza-like pneumonias [14, 64].
The proposed oral-vascular-pulmonary pathway challenges the notion that airway inhalation is the sole route of lung infection. Firstly, ACE2 receptors are expressed with very low intensity in the lower respiratory tract [15] and are absent in healthy individuals [65]. Secondly, the radiological disease pattern does not indicate airway inflammation [14]. The central areas of the lungs, which are those most accessible to inhaled pathogens, are the least affected, and the upper lungs—which are the most aerated on lung ventilation—are spared in acute COVID-19 until late in the disease course [66, 67]. Corresponding with this distribution of lung disease demonstrated radiologically, autopsy findings demonstrate topological correlation of viral loads with histopathological damage; the upper parts of the lungs are not damaged and are negative for viral detection on electron microscopy, and the lower lungs, which are severely damaged, demonstrate high viral loads [68]. These findings further corroborate a vascular distribution of the virus SARS-CoV-2, rather than an inhalational distribution.
The assumption that poor oral health leads to poorer COVID-19 outcomes because of aspiration of oral bacteria is also challenged by radiological, microbiological, and histological findings. In COVID-19, radiological studies have not shown aspirated fluid, mucous secretion, or bronchial inflammation in the central or peripheral airways [14, 63, 67]. Microbiological studies do not support a link between bacterial superinfection and critical care needs in acute COVID-19 [69]. When bacterial superinfection was observed in critical/intensive care, it did not impact the clinical outcomes [70]. Importantly, autopsies show a surprising lack of bacterial superinfection in the lungs of those dying from COVID-19 [71].
COVID-19 lung disease is radiologically characterised by lung parenchymal damage associated with abnormally dilated blood vessels and areas of peripheral consolidation analogous to pulmonary vascular congestion in the lung peripheries, such as in conventional pulmonary thromboembolic disease, a phenomenon referred to as ‘infarct pneumonia’ [72].
Studies using computerised tomography pulmonary angiography (CTPA)—the conventional scan technique for identifying pulmonary thromboembolic disease—show a higher incidence of macroscopic clots in COVID-19 patients (18–50%), compared to 5.9% in influenza [73, 74]. The distribution of macroscopic pulmonary thrombotic disease in COVID-19 also differs from conventional pulmonary emboli. In COVID-19, visible thrombi are more peripheral, smaller, and more likely to be associated with peripheral lung damage due to in situ pro-inflammatory clotting processes (immunothrombosis) [61, 75].
Specialised dual-energy CT scans reveal perfusion defects analogous to thromboembolic processes in 100% of subjects with acute COVID-19 lung disease, irrespective of macroscopic pulmonary thromboembolic disease visible on conventional CTPA [76, 77].
Recent optical coherence tomography (OCT) studies demonstrate clotting in the small distal pulmonary arteries in vivo in acute COVID-19, regardless of macroscopic clots visible on CTPA images [78]. Post-mortem studies using hierarchical phase-contrast tomography (HiP-CT) also reveal material consistent with thrombus in alveolar sacs of those who have died of acute COVID-19 [79]. This further indicates clotting as a central mechanism rather than inflammatory processes of the airways.
The dominant vascular phenomena observed radiologically align with histological autopsy studies showing microangiopathic processes—such as capillary vascular congestion accompanied by microthrombosis and endothelial damage—as critical drivers of COVID-19 lung disease [80,81,82,83,84]. Microthrombosis is present on both sides of the capillary bed, in the small pulmonary arteries and venules [71]. Upstream pulmonary arteriovenous shunting and impaired perfusion follow these microvascular events, thereby explaining the preservation of physiological dead space in the airways and ‘silent hypoxemia’ [58].
Thus, acute COVID-19 lung disease is primarily driven by microvasculopathic processes, rather than airway inflammation. Aspiration of oral bacteria does not adequately explain the connections between poor oral health and COVID-19 severity, and this model cannot account for the differences between COVID-19 (vascular disease) and influenza pneumonia (airway disease) [14]. This crucial difference requires a new pathophysiological model, explained by vascular delivery of SARS-CoV-2 to the lungs [12].
Acute COVID-19: Pathogenesis in the Blood
In considering the delivery of SARS-CoV-2 via damaged oral mucosa in the bloodstream to the pulmonary vessels, it is essential to discuss haematological processes and endothelial interactions. Autopsy studies indicate that SARS-CoV-2 is found in most organs, including the lungs, brain, heart, and kidneys [85, 86], providing clear evidence of vascular viral delivery around the body. Thus, direct primary intravascular delivery to the lungs is also possible if the virus can reach other organs via the blood. Importantly, endothelial cells are a site of direct viral infection in the lungs and other organs via endothelial ACE2 receptors [80, 81].
Although periodontal diseases may indirectly contribute to systemic disease through circulating inflammatory mediators, critical illness in COVID-19 is directly linked to circulating SARS-CoV-2 plasma levels [87, 88]. Many complex pathways account for thrombotic processes in acute COVID-19 [89, 90], characterized as a hypercoagulable state with impaired breakdown of blood clots. [91, 92]. This is likely partly mediated by increased angiotensin II levels resulting from direct viral interaction via ACE2 receptors. This hormone triggers vasoconstriction, pro-thrombotic, and pro-inflammatory events. [93]. Direct viral interaction with endothelial ACE2 receptors has been proposed to be responsible for immunothrombosis and lung endothelial dysfunction [94, 95]. Moreover, COVID-19 has also been widely described as a disease of the endothelium [80, 81, 96].
In addition to activating clotting cascades [97], binding of the SARS-CoV-2 spike protein to ACE2 receptors on platelets enhances thrombosis [98]. The viral lipid membrane also exposes pro-coagulant phospholipids—such as are found on the surface of activated platelets—significantly accelerating plasma coagulation [99]. Viral interaction with the pro-coagulant heparinase/heparan sulphate pathway is potentially involved in the induction of coagulation. [100]. Furthermore, the plasminogen/plasmin pathway is implicated in oral viral entry, activation of the complement cascade, and impaired clot breakdown in COVID-19 [101].
These multiple examples of viral-triggered coagulation pathways point to the intravascular delivery of SARS-CoV-2 resulting in clotting if complete virions or viral elements, such as the spike protein or the lipid membrane, were to enter the blood.
Long COVID
Potential for an Oral-Vascular-Pulmonary/Systemic Pathological Route in Long COVID
Post-acute COVID (also known as long COVID) is defined by the World Health Organization as—the continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least 2 months with no other explanation [102]. This condition affects two million people in the UK alone (May 2023) [103]. Although long COVID disease pathogenesis has not been fully established, progress in understanding has been made. The disease shares characteristics of other post-viral conditions, such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) [104]. Possible long COVID mechanisms include dysbiosis, endothelial dysfunction, abnormal persistence of circulating fibrinoid microclots, autoimmune processes, and persistent viral reservoirs [104].
Long COVID: Pathophysiology in the Mouth
The detection of SARS-CoV-2 genetic material in the faeces of individuals with long COVID symptoms months after initial infection points to the gut as a potential viral reservoir [105]. The oral cavity has not been fully investigated as a potential viral reservoir in long COVID despite multiple oral niches being proven long-term reservoir sites for other viruses, including human immunodeficiency virus, cytomegalovirus, and herpesviruses. [106,107,108,109]. Importantly, SARS-CoV-2 is detectable in saliva for much longer than is widely understood—for over 2 months in some individuals who were symptomatic in the acute phase and up to 3.5 weeks in those without symptoms [16]. The tongue and tonsils have also been shown to remain a reservoir for SARS-CoV-2 for several months [110, 111].
Autopsy studies of individuals previously infected with SARS-CoV-2 have shown its presence in many organs [85, 86], suggesting persistent intravascular viral distribution. In addition, immune dysfunction indicative of viral persistence and mucosal involvement has been demonstrated in long COVID [112].
An in vitro study simulating acute and long COVID infection reports direct SARS-CoV-2 infection of human periodontal fibroblasts, causing fibrosis through impaired mitochondrial oxidation [41], suggesting that the virus can contribute to periodontal inflammation. This also implies a bi-directional relationship, where periodontal inflammation increases the risk for acute COVID-19 and potentially long COVID, and SARS-CoV-2 can worsen periodontal status. This bi-directional link has been demonstrated in other periodontal-systemic disease relationships such as type 2 diabetes [2, 113], chronic kidney disease [46], and rheumatoid arthritis [114].
Whether prolonged oral viral detection relates to long-term COVID-19 symptoms is unknown. In addition to its potential as a long-term viral reservoir, the oral cavity may also foster the reactivation of latent oral epithelial viruses, including Epstein-Barr Virus (EBV). Of note, EBV reactivation has been reported in individuals with long COVID symptoms. [115].
Oral manifestations are commonly reported in patients with long COVID, including ulceration, discolouration, haemorrhagic changes, mycosis, aphthous-like lesions, and cheilitis [116].
Perhaps the most substantial evidence for the role of the oral cavity in long COVID is the finding that oral dysbiosis can predict the onset of systemic long COVID symptoms. A study by Haran et al. demonstrated that the spectrum of an inflammatory-type dysbiosis represented in the context of long COVID is similar to that seen in other post-viral illnesses such as ME/CFS. Specific lipopolysaccharide-producing oral microorganisms are implicated [117].
Long COVID: Pathophysiology in the Lungs
In post-acute COVID, imaging reveals persistent lung damage in some patients following severe lung disease during the acute phase [118, 119]. A study using dual-energy CT (DECT) in patients previously hospitalised with COVID-19 who had persistent respiratory symptoms 6 months after acute infection showed macroscopic pulmonary artery clots (acute or chronic) in 7.5% and persistent lung perfusion defects in 87% of patients [120]. In some patients, these defects were detected even when the lung parenchyma was macroscopically normal. This suggests that persistent hypercoagulation and endothelial dysregulation in pulmonary capillaries are mechanistically involved in long COVID, similar to the acute phase [120, 121].
Nuclear medicine scans, which specifically detect lung perfusion defects, have been advocated as the most appropriate technique for investigating respiratory symptoms in long COVID, as conventional scans (CTPA) can underestimate thromboembolic disease in this context [122].
Furthermore, xenon MRI studies show persistent gas transfer failure in the lungs for a year following acute COVID-19 infection [123, 124]. This phenomenon has been demonstrated even in structurally normal lungs in long COVID and regardless of acute phase severity. These findings indicate thrombosis of alveolar capillaries as the primary pathology in long COVID, rather than disease of the airways [123,124,125,126].
Long COVID: Pathophysiology in the Blood and Vascular Endothelium
As well as evidence for viral persistence, current hypotheses relating to long COVID pathology include the presence of persistent circulating ‘microclots’. Microclots are amyloid fibrin(ogen) particles which are resistant to breakdown via normal fibrinolytic pathways and are proposed as a contributing factor to long COVID. [121, 127]. This phenomenon is not unique to long COVID. It has also been described in ME/CFS and in diabetes, but it is more severe in long COVID. [128]. Although it is currently unclear whether microclots directly cause symptoms, discovering their anatomical origin could be critical. Regarding anatomical vascular chambers, if the mouth is a persistent viral reservoir, virus/blood interactions could lead to clotting on entry into the venous drainage of the mouth or on arrival in the pulmonary vasculature. This may provide a model for impaired pulmonary gas transfer in long COVID, as this would be the first capillary bed to be reached, just as is proposed above for acute COVID-19 [12]. Studies are required relating to the mouth being a potential source of persistent microclots, especially in view of the potential for SARS-CoV-2 to interact with oral cellular infection routes which may dysregulate fibrinolytic factors [101].
Videomicroscopy of the sublingual area of the mouth demonstrates significantly lower vascular density in long COVID patients than in healthy individuals. This rarefication of capillaries may contribute to long COVID symptoms. It is demonstrated irrespective of the need for hospitalisation or oxygen in the acute phase of COVID-19 [129].
As well as gut viral persistence [105], SARS-CoV-2 RNA is detectable in plasma in 45% of patients with long COVID symptoms. [130]. Spike antigen also persists in the plasma of those with long COVID for up to 12 months [131], suggesting ongoing viral reservoirs in the body. If the mouth is a reservoir and poor oral health impacts long COVID, the intravascular route from the mouth to the lungs and rest of the body via the systemic circulation may be a plausible pathogenic model, the oral cavity being upstream of all other anatomical sites.
Evidence for the Benefits of Oral Hygiene and Periodontal Therapy
Based on the potential translocation of SARS-CoV-2 from the mouth to the blood, the role of oral hygiene measures and periodontal treatment in reducing disease severity should be considered.
Some specific ingredients of readily available oral rinses have anti-viral properties against SARS-CoV-2 to the extent that the virus is completely eradicated in vitro by disrupting the viral lipid membrane, leading to undetectable viral load in vivo, in saliva, for a prolonged period [99, 132].
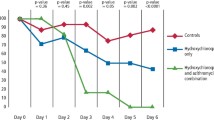
Use of a mouthwash containing a phthalocyanine derivative—active against SARS-CoV-2—was evaluated as a single addition to standard hospital care [133]. A non-active mouthwash was used as a control. The study showed beneficial outcomes with reduced length of hospital stay (7 days on average in the non-active mouthwash group, reduced to 4 days in the active group), reduced admission rates to intensive care (28% in the non-active group, 0% in the active mouthwash group), and reduced mortality (50% of those admitted to intensive care in the non-active group, 0% in the active mouthwash group). This specific ingredient is not widely available outside of Brazil, but the authors concluded that other mouthwashes capable of reducing SARS-CoV-2 viral load in the mouth may have similar positive effects in mitigating disease progression [133]. A systematic review of the ingredient cetylpyridinium chloride (CPC) suggests superior potential in reducing SARS-CoV-2 load in vivo in the saliva of patients with acute COVID-19 compared with mouthwashes containing other anti-viral ingredients. [134].
Saliva is an essential source of transmission of SARS-CoV-2 infection via droplets small enough to mediate aerosol transmission on coughing, sneezing, and talking [18]. Therefore, mouthwashes with anti-viral activity are potentially valuable in reducing infection risk in certain settings [134].
Given the pathological links between periodontitis and COVID-19, periodontal interventions are potentially beneficial in both acute and post-acute COVID-19. Periodontitis triggers platelet activation [135], and periodontal treatment can improve endothelial dysfunction [136]. In a case–control study, COVID-19 patients presenting with complications were compared to those without complications following experience of previous periodontal treatment. Volunteers with untreated periodontitis exhibited an increased risk of COVID-19 complications compared to those with a history of periodontal therapy or periodontally healthy individuals [137]. Thus, periodontitis management has the potential to lower the severity of acute and post-acute COVID-19, as it reduces local inflammation and restores the gingival immune barrier. Hence, sufferers of long COVID may benefit from a periodontal examination, as periodontitis typically presents asymptomatically. Studies evaluating the effect of oral hygiene measures and periodontal therapy are required in the context of long COVID.
Summary
A unifying understanding of acute and post-acute COVID-19 pathology is enhanced by considering pathogenesis from a broad anatomical perspective. Acute lung disease, coagulation abnormalities, systemic vascular phenomena, and the persistence of viral elements implicate the subgingival biofilm as a source of repeated viraemia via the ulcerated sulcular or periodontal pocket lining epithelium. The proposed oral-vascular-pulmonary route of infection provides a model to explain why the severity of acute COVID-19 is associated with high viral load in the mouth and with periodontitis. It also offers an anatomically based explanation for the vascular characteristics and distribution of severe lung disease, endothelial dysfunction, and clotting disorders in both acute and post-acute COVID-19.
In this review, our original hypothesis is enhanced by a discussion of recent studies highlighting the dominance of vascular processes in the lungs and a growing awareness that endothelial dysfunction and clotting processes are primary in the pathogenesis and development of COVID-19. Recent studies increasingly support the potential for a persistent oral reservoir in the post-acute COVID-19 phase. This is important because, given the potential for vascular viral translocation, the mouth is anatomically upstream of all other organs. Detailed analysis of a range of oral niches is required in those with persistent symptoms of long COVID.
Conclusion
The proposed disease model of the oral cavity as a SARS-CoV-2 reservoir combined with a breach of the oral mucosal immune barrier facilitating vascular viral delivery to the lungs and body remains compelling. Thus, the mouth can act as a mediator for disease severity via intravascular viral translocation. This oral-vascular-pulmonary infection route provides an anatomical model for the dominant vascular pathological mechanisms characteristic of the acute-phase COVID-19 lung disease and a potential model for long COVID. Detailed studies are required to enhance evidence for this pathway and to determine the role of oral hygiene measures and periodontal therapy, particularly in the context of long COVID.
References
Monsarrat P, Blaizot A, Kémoun P, Ravaud P, Nabet C, Sixou M, et al. Clinical research activity in periodontal medicine: a systematic mapping of trial registers. J Clin Periodontol. 2016;43:390–400. https://doi.org/10.1111/JCPE.12534.
Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55:21–31. https://doi.org/10.1007/s00125-011-2342-y.
Chapple ILC, Genco R. Diabetes and periodontal diseases: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J Periodontol. 2013;84:S106–12. https://doi.org/10.1902/jop.2013.1340011.
Sanz M, Marco del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D’Aiuto F, Bouchard P, et al. Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol. 2020;47:268–88. https://doi.org/10.1111/jcpe.13189.
Nascimento PC, Castro MML, Magno MB, Almeida APCPSC, Fagundes NCF, Maia LC, et al. Association between periodontitis and cognitive impairment in adults: a systematic review. Front Neurol. 2019;10:323. https://doi.org/10.3389/fneur.2019.00323.
Jungbauer G, Stähli A, Zhu X, Auber Alberi L, Sculean A, Eick S. Periodontal microorganisms and Alzheimer disease—a causative relationship? Periodontol. 2000;2022(89):59–82. https://doi.org/10.1111/PRD.12429.
De Pablo P, Dietrich T, Chapple ILC, Milward M, Chowdhury M, Charles PJ, et al. The autoantibody repertoire in periodontitis: a role in the induction of autoimmunity to citrullinated proteins in rheumatoid arthritis? Ann Rheum Dis. 2014;73:580–6. https://doi.org/10.1136/ANNRHEUMDIS-2012-202701.
González-Febles J, Sanz M. Periodontitis and rheumatoid arthritis: what have we learned about their connection and their treatment? Periodontol. 2000;2021(87):181–203. https://doi.org/10.1111/PRD.12385.
Herzberg MC, Weyer MW. Dental plaque, platelets, and cardiovascular diseases. Ann Periodontol. 1998;3:151–60. https://doi.org/10.1902/ANNALS.1998.3.1.151.
Hajishengallis G, Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021;21:426–40. https://doi.org/10.1038/S41577-020-00488-6.
Xie M, Tang Q, Yu S, Sun J, Mei F, Zhao J, et al. Porphyromonas gingivalis disrupts vascular endothelial homeostasis in a TLR-NF-κB axis dependent manner. Int J Oral Sci. 2020;12:1–9. https://doi.org/10.1038/s41368-020-00096-z.
Lloyd-Jones G, Molayem S, Pontes CC, Chapple I. The COVID-19 pathway: a proposed oral-vascular-pulmonary route of SARS-CoV-2 infection and the importance of oral healthcare measures. J Oral Med Dental Res. 2021;2:1–25. https://doi.org/10.52793/JOMDR.2020.2(1)-13.
Sampson V, Kamona N, Sampson A. Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? Br Dent J. 2020;228:971–5. https://doi.org/10.1038/s41415-020-1747-8.
Shuai W, Chen X, Shan Y, Li W, Ma W, Lu Q, et al. Clinical characteristics and CT findings in 148 non-COVID-19 influenza-like illness cases: a retrospective control study. Front Public Health. 2021;9:25. https://doi.org/10.3389/FPUBH.2021.616963/BIBTEX.
Chen M, Shen W, Rowan NR, Kulaga H, Hillel A, Ramanathan M, et al. Elevated ACE-2 expression in the olfactory neuroepithelium: implications for anosmia and upper respiratory SARS-CoV-2 entry and replication. Eur Respir J. 2020;56. https://doi.org/10.1183/13993003.01948-2020
Huang N, Pérez P, Kato T, Mikami Y, Okuda K, Gilmore RC, et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat Med. 2021. https://doi.org/10.1038/s41591-021-01296-8.
Zhu J, Guo J, Xu Y, Chen X. Viral dynamics of SARS-CoV-2 in saliva from infected patients. J Infect. 2020;81:e48-50. https://doi.org/10.1016/j.jinf.2020.06.059.
Baghizadeh FM. Oral saliva and COVID-19. Oral Oncol. 2020;108:104821. https://doi.org/10.1016/J.ORALONCOLOGY.2020.104821.
Wyllie AL, Fournier J, Casanovas-Massana A, Campbell M, Tokuyama M, Vijayakumar P, et al. Saliva is more sensitive for SARS-CoV-2 detection in COVID-19 patients than nasopharyngeal swabs. MedRxiv 2020;3:2020.04.16.20067835. https://doi.org/10.1101/2020.04.16.20067835
Pasomsub E, Watcharananan SP, Boonyawat K, Janchompoo P, Wongtabtim G, Suksuwan W, et al. Saliva sample as a non-invasive specimen for the diagnosis of coronavirus disease 2019: a cross-sectional study. Clin Microbiol Infect. 2021;27:285.e1-285.e4. https://doi.org/10.1016/J.CMI.2020.05.001.
Silva J, Lucas C, Sundaram M, Israelow B, Wong P, Klein J, et al. Saliva viral load is a dynamic unifying correlate of COVID-19 severity and mortality. MedRxiv. 2021. https://doi.org/10.1101/2021.01.04.21249236.
Marouf N, Cai W, Said KN, Daas H, Diab H, Chinta VR, et al. Association between periodontitis and severity of COVID‐19 infection: a case–control study. J Clin Periodontol. 2021:jcpe.13435. https://doi.org/10.1111/jcpe.13435
Gupta S, Mohindra R, Singla M, Khera S, Sahni V, Kanta P, et al. The clinical association between periodontitis and COVID-19. Clin Oral Investig. 2022;26:1. https://doi.org/10.1007/S00784-021-04111-3.
Baima G, Marruganti C, Sanz M, Aimetti M, Romandini M. Periodontitis and COVID-19: biological mechanisms and meta-analyses of epidemiological evidence. J Dent Res. 2022;101:1430–40. https://doi.org/10.1177/00220345221104725.
Kamel AHM, Basuoni A, Salem ZA, AbuBakr N. The impact of oral health status on COVID-19 severity, recovery period and C-reactive protein values. British Dental J. 2021:1–7. https://doi.org/10.1038/s41415-021-2656-1
Bemquerer LM, Oliveira SR, de Arruda JAA, Costa FPD, Miguita L, Bemquerer ALM, et al. Clinical, immunological, and microbiological analysis of the association between periodontitis and COVID-19: a case-control study. Odontol. 2023:1–13. https://doi.org/10.1007/S10266-023-00811-2
Chisini LA, dos Santos Costa F, Salvi LC, Poletto Neto V, Varella de Carvalho R, Demarco FF. Is the effect of COVID-19 on periodontal treatment similar to that in general dental care and primary medical care? an observational study in Brazil. Int J Environ Health Res. 2022:1–10. https://doi.org/10.1080/09603123.2022.2043250
Larvin H, Wilmott S, Wu J, Kang J. The impact of periodontal disease on hospital admission and mortality during COVID-19 pandemic. Front Med (Lausanne). 2020;7:604980. https://doi.org/10.3389/FMED.2020.604980.
Larvin H, Wilmott S, Kang J, Aggarwal VR, Pavitt S, Wu J. Additive effect of periodontal disease and obesity on COVID-19 outcomes. J Dent Res. 2021;100:1228–35. https://doi.org/10.1177/00220345211029638.
Costa CA, Vilela ACS, Oliveira SA, Gomes TD, Andrade AAC, Leles CR, et al. Poor oral health status and adverse COVID-19 outcomes: a preliminary study in hospitalized patients. J Periodontol. 2022;93(12):1889–901. https://doi.org/10.1002/JPER.21-0624.
Gomes SC, da Fonseca JG, Miller LM, Manenti L, Angst PDM, Lamers ML, et al. SARS-CoV-2 RNA in dental biofilms: supragingival and subgingival findings from inpatients in a COVID-19 intensive care unit. J Periodontol. 2022;93(10):1476–85. https://doi.org/10.1002/JPER.21-0623.
Gupta S, Mohindra R, Chauhan PK, Singla V, Goyal K, Sahni V, et al. SARS-CoV-2 Detection in gingival crevicular fluid. J Dent Res. 2021;100:187–93. https://doi.org/10.1177/0022034520970536.
Herrera D, Sanz M, Shapira L, Brotons C, Chapple I, Frese T, et al. Association between periodontal diseases and cardiovascular diseases, diabetes and respiratory diseases: consensus report of the Joint Workshop by the European Federation of Periodontology (EFP) and the European arm of the World Organization of Family Doctors (WONCA Europe). J Clin Periodontol. 2023;50(6):819–41. https://doi.org/10.1111/JCPE.13807.
Rafiqul Islam SM, Foysal MJ, Hoque MN, Mehedi HMH, Rob MA, Salauddin A, et al. Dysbiosis of oral and gut microbiomes in SARS-CoV-2 infected patients in Bangladesh: elucidating the role of opportunistic gut microbes. Front Med (Lausanne). 2022;9:163. https://doi.org/10.3389/FMED.2022.821777/BIBTEX.
Gupta A, Bhanushali S, Sanap A, Shekatkar M, Kharat A, Raut C, et al. Oral dysbiosis and its linkage with SARS-CoV-2 infection. Microbiol Res. 2022;261:127055. https://doi.org/10.1016/J.MICRES.2022.127055.
Miller EH, Annavajhala MK, Chong AM, Park H, Nobel YR, Soroush A, et al. Oral microbiome alterations and SARS-CoV-2 saliva viral load in patients with COVID-19. Microbiol Spectr. 2021;9:e0005521. https://doi.org/10.1128/SPECTRUM.00055-21.
Soffritti I, D’Accolti M, Fabbri C, Passaro A, Manfredini R, Zuliani G, et al. Oral microbiome dysbiosis is associated with symptoms severity and local immune/inflammatory response in COVID-19 patients: a cross-sectional study. Front Microbiol. 2021;12: 687513. https://doi.org/10.3389/FMICB.2021.687513.
Brogna C, Brogna B, Bisaccia DR, Lauritano F, Marino G, Montano L, et al. Could SARS-CoV-2 have bacteriophage behavior or induce the activity of other bacteriophages? Vaccines (Basel). 2022;10:708. https://doi.org/10.3390/VACCINES10050708/S1.
Henin D, Pellegrini G, Carmagnola D, Lanza Attisano GC, Lopez G, Ferrero S, et al. Morphological and immunopathological aspects of lingual tissues in COVID-19. Cells. 2022;11:1248. https://doi.org/10.3390/CELLS11071248.
Kessler AT, Bhatt AA. Review of the major and minor salivary glands, Part 1: anatomy, infectious, and inflammatory processes. J Clin Imaging Sci. 2018;8:47. https://doi.org/10.4103/JCIS.JCIS_45_18.
Gao Y, Kok WL, Sharma V, Illsley C, Hanks S, Tredwin C, et al. SARS-CoV-2 infection causes fibrotic pathogenesis through deregulating mitochondrial beta-oxidation. Cell Death Discov. 2023;9(1):1752023. https://doi.org/10.21203/RS.3.RS-2557548/V1.
Qi X, Northridge ME, Hu M, Wu B. Oral health conditions and COVID-19: a systematic review and meta-analysis of the current evidence. Aging Health Res. 2022;2:100064. https://doi.org/10.1016/J.AHR.2022.100064.
Lockhart PB, Brennan MT, Thornhill M, Michalowicz BS, Noll J, Bahrani-Mougeot FK, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dental Assoc. 2009;140:1238–44. https://doi.org/10.14219/jada.archive.2009.0046.
Artese HPC, Longo PL, Kawamoto D, Gomes GH, Mayer MPA, Romito GA, et al. Bacteremia after chewing in a patient with severe chronic periodontitis and diabetes mellitus type 2: a brief report. J Clin Transl Endocrinol Case Rep. 2017;6:1–3. https://doi.org/10.1016/J.JECR.2017.06.001.
Forner L, Larsen T, Kilian M, Holmstrup P. Incidence of bacteremia after chewing, tooth brushing and scaling in individuals with periodontal inflammation. J Clin Periodontol. 2006;33:401–7. https://doi.org/10.1111/J.1600-051X.2006.00924.X.
Sharma P, Fenton A, Dias IHK, Heaton B, Brown CLR, Sidhu A, et al. Oxidative stress links periodontal inflammation and renal function. J Clin Periodontol. 2020;48. https://doi.org/10.1111/jcpe.13414
Molina A, Huck O, Herrera D, Montero E. The association between respiratory diseases and periodontitis: a systematic review and meta-analysis. J Clin Periodontol. 2023;50(6):842–87. https://doi.org/10.1111/JCPE.13767.
Ling MR, Chapple ILC, Matthews JB. Peripheral blood neutrophil cytokine hyper-reactivity in chronic periodontitis. Innate Immun. 2015;21:714–25. https://doi.org/10.1177/1753425915589387.
Dias IHK, Matthews JB, Chapple ILC, Wright HJ, Dunston CR, Griffiths HR. Activation of the neutrophil respiratory burst by plasma from periodontitis patients is mediated by pro-inflammatory cytokines. J Clin Periodontol. 2011;38:1–7. https://doi.org/10.1111/J.1600-051X.2010.01628.X.
Sahni V, Gupta S. COVID-19 & periodontitis: the cytokine connection. Med Hypotheses. 2020;144: 109908. https://doi.org/10.1016/j.mehy.2020.109908.
Molayem S, Pontes C. COVID-19 and periodontal conditions—a narrative review of implications for oral health providers. J Calif Dental Assoc. 2023;51:2177375. https://doi.org/10.1080/19424396.2023.2177375.
Lei S, Li J, Yu J, Li F, Pan Y, Chen X, et al. Porphyromonas gingivalis bacteremia increases the permeability of the blood-brain barrier via the Mfsd2a/Caveolin-1 mediated transcytosis pathway. Int J Oral Sci. 2022;15:1–12. https://doi.org/10.1038/s41368-022-00215-y.
Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5:eaau3333. https://doi.org/10.1126/SCIADV.AAU3333.
Farquharson D, Butcher JP, Culshaw S. Periodontitis, Porphyromonas, and the pathogenesis of rheumatoid arthritis. Mucosal Immunol. 2012;5:112–20. https://doi.org/10.1038/mi.2011.66.
Carinci F, Martinelli M, Contaldo M, Santoro R, Lauritano D, Candotto V, et al. Focus on periodontal disease and development of endocarditis. J Biol Regul Homeost. 2018;32:143–7.
Del Giudice C, Vaia E, Liccardo D, Marzano F, Valletta A, Spagnuolo G, et al. Infective endocarditis: a focus on oral microbiota. Microorganisms. 2021;9:1218. https://doi.org/10.3390/MICROORGANISMS9061218.
Nemec SF, Bankier AA, Eisenberg RL. Lower lobe-predominant diseases of the lung. Am J Roentgenol. 2013;200:712–28. https://doi.org/10.2214/AJR.12.9253.
Patel BV, Arachchillage DJ, Ridge CA, Bianchi P, Doyle JF, Garfield B, et al. Pulmonary angiopathy in severe COVID-19: physiologic, imaging, and hematologic observations. Am J Respir Crit Care Med. 2020;202:690–9. https://doi.org/10.1164/rccm.202004-1412OC.
Lang M, Som A, Carey D, Reid N, Mendoza DP, Flores EJ, et al. Pulmonary vascular manifestations of COVID-19 pneumonia. Radiol Cardiothorac Imaging. 2020;2: e200277. https://doi.org/10.1148/ryct.2020200277.
Eddy RL, Sin DD. Computed tomography vascular tree-in-bud: a novel prognostic imaging biomarker in COVID-19? Am J Respir Crit Care Med. 2020;202:642–4. https://doi.org/10.1164/RCCM.202007-2833ED.
van Dam LF, Kroft LJM, van der Wal LI, Cannegieter SC, Eikenboom J, de Jonge E, et al. Clinical and computed tomography characteristics of COVID-19 associated acute pulmonary embolism: a different phenotype of thrombotic disease? Thromb Res. 2020;193:86–9. https://doi.org/10.1016/j.thromres.2020.06.010.
Mulay A, Konda B, Garcia G, Yao C, Beil S, Villalba JM, et al. SARS-CoV-2 infection of primary human lung epithelium for COVID-19 modeling and drug discovery. Cell Rep. 2021;35: 109055. https://doi.org/10.1016/J.CELREP.2021.109055.
Ufuk F, Savaş R. Chest CT features of the novel coronavirus disease (COVID-19). Turk J Med Sci. 2020;50:664–78. https://doi.org/10.3906/sag-2004-331.
Yin Z, Kang Z, Yang D, Ding S, Luo H, Xiao E. A comparison of clinical and chest CT findings in patients with influenza A (H1N1) virus infection and coronavirus disease (COVID-19). AJR Am J Roentgenol. 2020;215:1065–71. https://doi.org/10.2214/AJR.20.23214.
Hikmet F, Méar L, Edvinsson Å, Micke P, Uhlén M, Lindskog C. The protein expression profile of ACE2 in human tissues. Mol Syst Biol. 2020;16(7):e9610. https://doi.org/10.15252/msb.20209610.
Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425. https://doi.org/10.1016/S1473-3099(20)30086-4.
Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2(1): e200034. https://doi.org/10.1148/RYCT.2020200034.
Deinhardt-Emmer S, Wittschieber D, Sanft J, Kleemann S, Elschner S, Haupt KF, et al. Early postmortem mapping of SARS-CoV-2 RNA in patients with COVID-19 and the correlation with tissue damage. Elife. 2021;10: e60361. https://doi.org/10.7554/ELIFE.60361.
Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in critically ill patients in the Seattle region — case series. N Engl J Med. 2020;382:2012–22. https://doi.org/10.1056/NEJMOA2004500.
Pandolfi L, Fossali T, Frangipane V, Bozzini S, Morosini M, D’Amato M, et al. Broncho-alveolar inflammation in COVID-19 patients: a correlation with clinical outcome. BMC Pulm Med. 2020;20:1–10. https://doi.org/10.1186/S12890-020-01343-Z.
Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8:681–6. https://doi.org/10.1016/S2213-2600(20)30243-5.
Martini K, Blüthgen C, Walter JE, Linh Nguyen-Kim TD, Thienemann F, Frauenfelder T. Patterns of organizing pneumonia and microinfarcts as surrogate for endothelial disruption and microangiopathic thromboembolic events in patients with coronavirus disease 2019. Plos One. 2020;15: e0240078. https://doi.org/10.1371/JOURNAL.PONE.0240078.
Bompard F, Monnier H, Saab I, Tordjman M, Abdoul H, Fournier L, et al. Pulmonary embolism in patients with Covid-19 pneumonia. Eur Respir J. 2020;56:29–32. https://doi.org/10.1183/13993003.01365-2020.
Bunce PE, High SM, Nadjafi M, Stanley K, Liles WC, Christian MD. Pandemic H1N1 influenza infection and vascular thrombosis. Clin Infect Dis. 2011;52:e14–7. https://doi.org/10.1093/CID/CIQ125.
Loo J, Spittle DA, Newnham M. COVID-19, immunothrombosis and venous thromboembolism: biological mechanisms. Thorax. 2021;76:412–20. https://doi.org/10.1136/THORAXJNL-2020-216243.
Ridge CA, Desai SR, Jeyin N, Mahon C, Lother DL, Mirsadraee S, et al. Dual-energy ct pulmonary angiography quantifies vasculopathy in severe Covid-19 pneumonia. Radiol Cardiothorac. Imaging 2020;2. https://doi.org/10.1148/RYCT.2020200428.
Lang M, Som A, Mendoza DP, Flores EJ, Reid N, Carey D, et al. Hypoxaemia related to COVID-19: vascular and perfusion abnormalities on dual-energy CT. Lancet Infect Dis. 2020;20:1365–6. https://doi.org/10.1016/S1473-3099(20)30367-4.
Hajjar LA, Ancona MB, Filho RK, Tresoldi M, Caldas JG, Monti G, et al. Microvascular lung vessels obstructive thromboinflammatory syndrome in patients with COVID-19: insights from lung intravascular optical coherence tomography. Front Med (Lausanne). 2023;10:1050531. https://doi.org/10.3389/FMED.2023.1050531.
Walsh CL, Tafforeau P, Wagner WL, Jafree DJ, Bellier A, Werlein C, et al. Imaging intact human organs with local resolution of cellular structures using hierarchical phase-contrast tomography. Nat Methods. 2021;18:1532–41. https://doi.org/10.1038/S41592-021-01317-X.
Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–8. https://doi.org/10.1056/NEJMOA2015432.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. The Lancet. 2020;395:1417–8. https://doi.org/10.1016/S0140-6736(20)30937-5.
Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, Zerbi P, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis. 2020;20:1135–40. https://doi.org/10.1016/S1473-3099(20)30434-5.
Henkel M, Weikert T, Marston K, Schwab N, Sommer G, Haslbauer J, et al. Lethal covid-19: radiologic-pathologic correlation of the lungs. Radiol Cardiothorac Imaging. 2020;2(6): e200406. https://doi.org/10.1148/RYCT.2020200406.
Kianzad A, Meijboom LJ, Nossent EJ, Roos E, Schurink B, Bonta PI, et al. COVID-19: Histopathological correlates of imaging patterns on chest computed tomography. Respirol. 2021;26:869–77. https://doi.org/10.1111/RESP.14101.
Hanley B, Naresh KN, Roufosse C, Nicholson AG, Weir J, Cooke GS, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe. 2020;1:e245–53. https://doi.org/10.1016/S2666-5247(20)30115-4.
Stein SR, Ramelli SC, Grazioli A, Chung JY, Singh M, Yinda CK, et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nat. 2022;612:758–63. https://doi.org/10.1038/s41586-022-05542-y.
Bermejo-Martin JF, González-Rivera M, Almansa R, Micheloud D, Tedim AP, Domínguez-Gil M, et al. Viral RNA load in plasma is associated with critical illness and a dysregulated host response in COVID-19. Crit Care. 2020;24(1):691. https://doi.org/10.1186/s13054-020-03398-0.
Gutmann C, Takov K, Burnap SA, Singh B, Ali H, Theofilatos K, et al. SARS-CoV-2 RNAemia and proteomic trajectories inform prognostication in COVID-19 patients admitted to intensive care. Nat Commun. 2021;12:1–17. https://doi.org/10.1038/s41467-021-23494-1.
Steadman E, Fandaros M, Yin W. SARS-CoV-2 and plasma hypercoagulability. Cell Mole Bioeng. 2021;14:513–22. https://doi.org/10.1007/S12195-021-00685-W.
Cappelletto A, Allan HE, Crescente M, Schneider E, Bussani R, Ali H, et al. SARS-CoV-2 Spike protein activates TMEM16F-mediated platelet procoagulant activity. Front Cardiovasc Med 2023;9. https://doi.org/10.3389/FCVM.2022.1013262/FULL
Weiss E, Roux O, Moyer JD, Paugam-Burtz C, Boudaoud L, Ajzenberg N, et al. Fibrinolysis resistance: a potential mechanism underlying COVID-19 coagulopathy. Thromb Haemost. 2020;120:1343–5. https://doi.org/10.1055/S-0040-1713637/ID/JR200328-6.
Watson O, Pillai S, Howard M, Zaldua JC, Whitley J, Burgess B, et al. Impaired fibrinolysis in severe Covid-19 infection is detectable in early stages of the disease. Clin Hemorheol Microcirc. 2022;82:183–91. https://doi.org/10.3233/CH-221491.
Senchenkova EY, Russell J, Vital SA, Yildirim A, Wayne Orr A, Neil Granger D, et al. A critical role for both CD40 and VLA5 in angiotensin Il–mediated thrombosis and inflammation. FASEB J. 2018;32:3448–56. https://doi.org/10.1096/FJ.201701068R.
Lloyd-Jones G, Oudkerk M. COVID-19: angiotensin II in development of lung immunothrombosis and vasculitis mimics. Lancet Rheumatol. 2021;3(5): e326. https://doi.org/10.1016/S2665-9913(21)00068-0.
Saba L, Gerosa C, Fanni D, Marongiu F, Nasa GLA, Caocci G, et al. Molecular pathways triggered by COVID-19 in different organs: ACE2 receptor-expressing cells under attack? A review. Eur Rev Med Pharmacol Sci. 2020;24:12609–22. https://doi.org/10.26355/EURREV_202012_24058.
Lei Y, Zhang J, Schiavon CR, He M, Chen L, Shen H, et al. SARS-CoV-2 spike protein impairs endothelial function via downregulation of ACE 2. Circ Res. 2021;128:1323–6. https://doi.org/10.1161/CIRCRESAHA.121.318902.
Biswas S, Thakur V, Kaur P, Khan A, Kulshrestha S, Kumar P. Blood clots in COVID-19 patients: simplifying the curious mystery. Med Hypotheses. 2021;146: 110371. https://doi.org/10.1016/J.MEHY.2020.110371.
Zhang S, Liu Y, Wang X, Yang L, Li H, Wang Y, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J Hematol Oncol. 2020;13:1–22. https://doi.org/10.1186/S13045-020-00954-7.
Saud Z, Tyrrell VJ, Zaragkoulias A, Protty MB, Statkute E, Rubina A, et al. The SARS-CoV2 envelope differs from host cells, exposes procoagulant lipids, and is disrupted in vivo by oral rinses. J Lipid Res. 2022;63(6): 100208. https://doi.org/10.1016/j.jlr.2022.100208.
Kinaneh S, Khamaysi I, Karram T, Hamoud S. Heparanase as a potential player in SARS-CoV-2 infection and induced coagulopathy. Biosci Rep. 2021;41:20210290. https://doi.org/10.1042/BSR20210290.
Yatsenko T, Skrypnyk M, Troyanovska O, Tobita M, Osada T, Takahashi S, et al. The Cells. 2023;12(3):445. https://doi.org/10.3390/CELLS12030445.
Post COVID-19 condition (Long COVID) n.d. https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition (accessed May 11, 2023).
Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK - Office for National Statistics n.d. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/2february2023 (accessed May 11, 2023).
Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133. https://doi.org/10.1038/S41579-022-00846-2.
Natarajan A, Zlitni S, Brooks EF, Vance SE, Dahlen A, Hedlin H, et al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med (N Y). 2022;3:371. https://doi.org/10.1016/J.MEDJ.2022.04.001.
Pallos D, Ruivo GF, Ferrari-Junior SH, Pannuti CS, Perozini C, Sarmento DJS, et al. Periodontal disease and detection of human herpesviruses in saliva and gingival crevicular fluid of chronic kidney disease patients. J Periodontol. 2020;91:1139–47. https://doi.org/10.1002/JPER.19-0583.
Contreras A, Nowzari H, Slots J. Herpesviruses in periodontal pocket and gingival tissue specimens. Oral Microbiol Immunol. 2000;15:15–8. https://doi.org/10.1034/j.1399-302X.2000.150103.x.
Matičić M, Poljak M, Kramar B, Tomažić J, Vidmar L, Zakotnik B, et al. Proviral HIV-1 DNA in gingival crevicular fluid of HIV-1-infected patients in various stages of HIV disease. J Dent Res. 2000;79:1496–501. https://doi.org/10.1177/00220345000790071101.
Parra B, Slots J. Detection of human viruses in periodontal pockets using polymerase chain reaction. Oral Microbiol Immunol. 1996;11:289–93. https://doi.org/10.1111/j.1399-302X.1996.tb00183.x.
Lima TM, Martins RB, Miura CS, Souza MVO, Cassiano MHA, Rodrigues TS, et al. Tonsils are major sites of prolonged sars-cov-2 infection in children. MedRxiv 2023:2023.01.21.23284592. https://doi.org/10.1101/2023.01.21.23284592.I
Yao Q, Doyle ME, Liu Q-R, Appleton A, O’Connell JF, Weng N, et al. Long-term dysfunction of taste papillae in SARS-CoV-2. NEJM Evidence 2023;2(9). https://doi.org/10.1056/EVIDOA2300046.I
Santa Cruz A, Mendes-Frias A, Azarias-da-Silva M, André S, Oliveira AI, Pires O, et al. Post-acute sequelae of COVID-19 is characterized by diminished peripheral CD8+β7 integrin+ T cells and anti-SARS-CoV-2 IgA response. Nat Commun. 2023;14:1–14. https://doi.org/10.1038/s41467-023-37368-1.
Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol. 2001;6:99–112. https://doi.org/10.1902/ANNALS.2001.6.1.99.
de Pablo P, Chapple IL, Buckley CD, Dietrich T. Periodontitis in systemic rheumatic diseases. Nat Rev Rheumatol. 2009;5(4):218–24. https://doi.org/10.1038/nrrheum.2009.28.
Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185:881. https://doi.org/10.1016/J.CELL.2022.01.014.
Rafałowicz B, Wagner L, Rafałowicz J. Long COVID oral cavity symptoms based on selected clinical cases. Eur J Dent. 2022;16:458–63. https://doi.org/10.1055/S-0041-1739445.
Haran JP, Bradley E, Zeamer AL, Cincotta L, Salive MC, Dutta P, et al. Inflammation-type dysbiosis of the oral microbiome associates with the duration of COVID-19 symptoms and long COVID. JCI Insight. 2021;20: e152346. https://doi.org/10.1172/JCI.INSIGHT.152346.
Han X, Fan Y, Alwalid O, Li N, Jia X, Yuan M, et al. Six-month follow-up Chest CT findings after severe COVID-19 pneumonia. Radiol. 2021;299:E177–86. https://doi.org/10.1148/RADIOL.2021203153.
Solomon JJ, Heyman B, Ko JP, Condos R, Lynch DA. CT of post-acute lung complications of COVID-19. Radiol. 2021;301:E383–95. https://doi.org/10.1148/RADIOL.2021211396.
Mohamed I, de Broucker V, Duhamel A, Giordano J, Ego A, Fonne N, et al. Pulmonary circulation abnormalities in post-acute COVID-19 syndrome: dual-energy CT angiographic findings in 79 patients. Eur Radiol. 2023;33:4700–12. https://doi.org/10.1007/s00330-023-09618-9.
Turner S, Khan MA, Putrino D, Woodcock A, Kell DB, Pretorius E. Long COVID: pathophysiological factors and abnormalities of coagulation. Trends Endocrinol Metab. 2023;34:321–44. https://doi.org/10.1016/J.TEM.2023.03.002.
Dhawan RT, Gopalan D, Howard L, Vicente A, Park M, Manalan K, et al. Beyond the clot: perfusion imaging of the pulmonary vasculature after COVID-19. Lancet Respir Med. 2021;9:107–16. https://doi.org/10.1016/S2213-2600(20)30407-0.
Saunders LC, Guilhem ;, Collier J, Chan H-F, Hughes PJC, Smith LJ, et al. Longitudinal lung function assessment of patients hospitalized with COVID-19 using 1H and 129Xe Lung MRI. Chest 2023;24:S0012–3692(23)00441–5. https://doi.org/10.1016/J.CHEST.2023.03.024
Li H, Zhao X, Wang Y, Lou X, Chen S, Deng H, et al. Damaged lung gas exchange function of discharged COVID-19 patients detected by hyperpolarized 129Xe MRI. Sci Adv. 2021;7(1):eabc8180. https://doi.org/10.1126/SCIADV.ABC8180.
Grist JT, Chen M, Collier GJ, Raman B, Abueid G, McIntyre A, et al. Hyperpolarized 129Xe MRI abnormalities in dyspneic participants 3 months after COVID-19 pneumonia: preliminary results. Radiol. 2021;301:E353–60. https://doi.org/10.1148/RADIOL.2021210033.
Matheson AM, McIntosh MJ, Kooner HK, Lee J, Desaigoudar V, Bier E, et al. Persistent 129Xe MRI pulmonary and CT vascular abnormalities in symptomatic individuals with post-acute COVID-19 syndrome. Radiol. 2022;305:466. https://doi.org/10.1148/RADIOL.220492.
Pretorius E, Vlok M, Venter C, Bezuidenhout JA, Laubscher GJ, Steenkamp J, et al. Persistent clotting protein pathology in long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc Diabetol. 2021;20(1):172. https://doi.org/10.1186/S12933-021-01359-7.
Nunes JM, Kruger A, Proal A, Kell DB, Pretorius E. The occurrence of hyperactivated platelets and fibrinaloid microclots in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Pharm (Basel). 2022;15:931. https://doi.org/10.3390/PH15080931.
Osiaevi I, Schulze A, Evers G, Harmening K, Vink H, Kümpers P, et al. Persistent capillary rarefication in long COVID syndrome. Angiogenesis. 2023;26:53–61. https://doi.org/10.1007/S10456-022-09850-9.
Tejerina F, Catalan P, Rodriguez-Grande C, Adan J, Rodriguez-Gonzalez C, Muñoz P, et al. Post-COVID-19 syndrome. SARS-CoV-2 RNA detection in plasma, stool, and urine in patients with persistent symptoms after COVID-19. BMC Infect Dis. 2022;22:1–8. https://doi.org/10.1186/S12879-022-07153-4.
Yang C, Zhao H, Espín E, Tebbutt SJ. Association of SARS-CoV-2 infection and persistence with long COVID. Lancet Respir Med. 2023;11(6):504–6. https://doi.org/10.1016/S2213-2600(23)00142-X.
Seneviratne CJ, Balan P, Ko KKK, Udawatte NS, Lai D, Ng DHL, et al. Efficacy of commercial mouth-rinses on SARS-CoV-2 viral load in saliva: randomized control trial in Singapore. Infect. 2021;49:305–11. https://doi.org/10.1007/S15010-020-01563-9.
da Silva Santos PS, da Fonseca Orcina B, Machado RRG, Vilhena FV, da Costa Alves LM, Zangrando MSR, et al. Beneficial effects of a mouthwash containing an antiviral phthalocyanine derivative on the length of hospital stay for COVID-19: randomised trial. Sci Rep. 2021;11:1–10. https://doi.org/10.1038/s41598-021-99013-5.
Filippo D, Matteo M, Marco S, Marilena M, Cilona MB, Lloyd-Jones G, et al. Efficacy of cetylpyridinium chloride mouthwash against SARS-CoV-2: a systematic review of randomized controlled trials. Mol Oral Microbiol. 2023;38:171–80. https://doi.org/10.1111/OMI.12408.
Mutthineni R, Ramishetty A, Gojja P, Muralidaran G, Burle V. Platelet indices be a new biomarker for periodontal disease. Contemp Clin Dent. 2021;12:289. https://doi.org/10.4103/CCD.CCD_461_20.
Laky M, Anscheringer I, Wolschner L, Heber S, Haririan H, Schrottmaier WC, et al. Periodontal treatment limits platelet activation in patients with periodontitis—a controlled-randomized intervention trial. J Clin Periodontol. 2018;45:1090–7. https://doi.org/10.1111/JCPE.12980.
Said KN, Al-Momani AM, Almaseeh JA, Marouf N, Shatta A, Al-Abdulla J, et al. Association of periodontal therapy, with inflammatory biomarkers and complications in COVID-19 patients: a case control study. Clin Oral Investig. 2022;26:6721–32. https://doi.org/10.1007/S00784-022-04631-6.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Dr Graham Lloyd-Jones is Director of Radiology Masterclass, a member of the Whole Body Health task team of the FDI World Dental Federation, an advisory board member for Long COVID support (patient led charity), and a member of the National Institute for Clinical Excellence (UK) thromboembolic disease committee.
Dr Carla Pontes has no interests to declare.
Dr Shervin Molayem has no interests to declare.
Prof Iain Chapple is the co-chair of the European Federation of Periodontology, chair of the Whole Body Health task team of the FDI World Dental Federation, an executive board scientific advisor to the British Society of Periodontology, and has previously received fees from GSK, J&J, Philips, P&G, and Unilever, grants from GSK, DEBRA, NIHR, and Unilever, book royalties from Quintessence, and travel fees for international lectures.
Human and Animal Rights and Informed Consent
No work was performed on humans or animals as part of this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lloyd-Jones, G., Pontes, C.C., Molayem, S. et al. The Oral-Vascular-Pulmonary Infection Route: a Pathogenic Mechanism Linking Oral Health Status to Acute and Post-Acute COVID-19. Curr Oral Health Rep 10, 163–174 (2023). https://doi.org/10.1007/s40496-023-00354-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-023-00354-z