Abstract
Purpose of Review
This review examines the restricting factors based on the current situation of implant treatments in elderly people and describes how they should be handled. In addition, it is suggested to establish an environment in which the oral cavity of the patient can be managed at the end of treatment with an implant card detailing the implant treatments provided, while anticipating the patient’s aging.
Recent Findings
Implant treatments now account for a large proportion of dental prosthetic treatment options. Meanwhile, aging is accelerating globally, with Japan at the top of the list. This has resulted in an increase in the number of implant patients who are elderly and require care and who have systemic problems. Furthermore, with the growing number of people in need of nursing care, there is a growing need to care elderly people who have received implant treatments in the past, and there are various issues in handling such cases. It is also important to properly evaluate the systemic conditions, conduct less-invasive surgeries using appropriate types of implant system based on estimated life expectancy, and provide treatments using prosthetic devices that can be easily managed and modified.
Summary
The systemic conditions and aging of the oral cavity need to be taken into consideration regarding the risks of implant surgery. As to the worsening of maintenance condition, changing to a removable superstructure as well as awareness-raising activities should be examined. In addition, we suggest that policy measures be taken to address some issues regarding training, manufacturers, and medical insurance. We hope that implant treatments will continue to contribute to patients as we head toward becoming a super-aging society.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Implant treatments now account for a large proportion of dental prosthetic treatment options. Meanwhile, aging is accelerating globally, with Japan at the top of the list [1]. This has resulted in an increase in the number of implant patients who are elderly and require care and who have systemic problems. Furthermore, with the growing number of people in need of nursing care, there is a growing need to care elderly people who have received implant treatments in the past, and there are various issues in handling such cases. This review examines the factors that restrict implant treatments in elderly people based on the actual states of implants and describes how they should be handled.
Implants in Japan and the World in the Era of Aging Societies
According to a survey on dental diseases [2], approximately 3% of elderly people in Japan had implants in 2011. However, this ratio increased to 3.9% in 2016 (Fig. 1). Furthermore, the ratio of elderly people (aged 65 and older) among implant patients increased from 49 to 59%. A report on dental implants among dependent elderlies [3••] also found that 360 (3%) out of 12,356 elderly people had implants. Internationally, the proportion of implant patients aged over 70 increased rapidly from 2002 to 2014 (from 7.7 to 21.0%) [4,5,6].
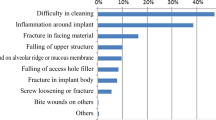
While there are many reports on implant troubles, few reports describe the actual states of elderly people, and in particular those of elderly people who require nursing care. In a survey conducted by the authors [7], among implant-related troubles encountered by dentists during visiting care, difficulty in cleaning (47%) and peri-implantitis (38%) accounted for very high ratios. Many of the measures adopted in these cases were medication and anti-inflammatory treatments (32%) and observation (22%). That is, there were many troubles, but they were not being handled sufficiently.
At present, the number of remaining teeth in elderly people is increasing [2], and the ratio of patients who require a prosthesis for missing teeth is decreasing. However, as the absolute number of elderly people is increasing, the actual number of patients requiring partial dentures has not significantly decreased (Fig. 2) [7]; conversely, the number of such patients is increasing among the very elderly. Denture treatment becomes even more difficult in very elderly people due to reasons such as flattening of the alveolar ridge, thinning of the mucous membrane [8], reduced keratinization [9], lowered pain threshold [10], reduced amount of saliva due to medications [11], reduced tongue pressure [12], reduced dexterity in the fingers, and worsening of systemic conditions (Table 1). That is, the number of intractable cases and the number of implant treatments are expected to increase.
Restrictions on Using Implants in Elderly People
Table 2 shows the restricting factors. These factors and the necessary measures are explained below.
Risks of Implant Surgery
-
Worsening of systemic conditions can present risks for implant placement. The conditions that require particular care include cardiovascular diseases, diabetes, osteoporosis, cancer, rheumatic diseases, and malnutrition. These diseases, or the effects of drugs used to treat them, can affect the implant surgery, wound healing, osteosynthesis, and long-term implant treatment. It is therefore vital to evaluate the state of the patient’s diseases and suitability for implant treatment. Furthermore, if implant surgery is to be performed, simulations using three-dimensional cone-beam computed tomography, flapless surgery, single-stage surgery, immediate implant placement and loading, use of short and thin implants [13], and so forth should be considered in order to plan a minimally invasive implant surgery [6].
Careful consideration and sufficient maintenance are also necessary if the patient has dry mouth, Parkinson’s disease, dementia, rheumatic disease, and so forth, as these diseases hinder maintenance after surgery.
-
Worsening of periodontal conditions is a problem especially when the patient starts requiring nursing care. It may be better to consider strategic extraction of teeth after examining the prognosis for the teeth. However, sufficient evidence for this measure has not yet been obtained.
-
When considering the deterioration in ability to clean and manage the oral cavity, cleaning properties must be given priority even if esthetics are somewhat compromised. The maintenance of oral hygiene in elderly people is a priority in implant treatments for elderly people. Deterioration in oral hygiene over time should be expected, even if the patient is able to clean and manage the oral cavity at the time of treatment planning.
-
Deterioration in cognitive function may prevent the patient from sufficiently understanding the treatment plan when it is explained. Appropriate evaluation of cognitive function is essential. While there are still many unknown matters regarding dental treatments of patients with dementia, guidelines are finally starting to be published [14].
Deterioration in Implant Functions
-
This means that the implant has been used for a long time when an implant patient becomes elderly, and that the implant body and its upper structure are deteriorating. The types of deterioration most commonly experienced by dentists visiting care facilities were facing material damage (16%), fallen superstructure (10%), fallen access hole filling (8%), and screw loosening (6%) [15]. While these types of deterioration need to be properly handled, there are issues concerning diagnosis and treatment devices as well as the skill of the dentist performing visiting dental care. Such issues have not always been sufficiently handled. These measures are discussed in more detail in a later section.
-
Oral hypofunction occurs in elderly people. The Japanese Society of Gerodontology prepared and presented the standards for diagnosis of oral hypofunction in “Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016” [16•]. In particular, occlusal force, mastication functions, tongue pressure, and tongue and lip movement functions deteriorate in elderly people [11]. The relationship between oral hypofunction and systemic health conditions, degree of nursing care required and longevity has been described in many reports [17,18,19,20,21,22,23,24,25,26,27,28,29,30]. Simply providing an implant prosthesis is not sufficient for these symptoms; appropriate rehabilitation is necessary.
Worsening of Maintenance Condition
When dexterity of the fingers and so forth deteriorates due to reasons such as deterioration of the body and paralysis, it may become difficult for the patient to remove the overdenture and clean the oral cavity. Worsening of the oral cavity environment (periodontal disease, dry mouth, etc.) will make it difficult to keep the area around the implant clean. Worsening of the social environment (admission to a facility, etc.) will also make it more difficult to receive care from implant specialists and specialized dental hygienists.
The following are important to handle these issues [31••]:
-
Correcting to a shape which prioritizes cleaning properties rather than esthetics (increasing the gaps between teeth to make them easier to clean, etc.)
-
Changing from a fixed type to a removable type (back-off strategy [32]: Improvement in cleaning properties and improvement in response to trouble/loss of implant)
-
Removal and sleeping (prevention of jaw counterpart and soft tissue damage) (difficult with one-piece implants)
-
Instructions to care-givers and improvement in their handling skills
-
Communication with the dentist in charge of visiting care and request for care
Another important point is where the dentist who provided the implant treatment cannot continue to provide management. In such cases, it is impossible for the dentist who handles the problem to accurately grasp how the implant treatment was provided in the past and take appropriate measures.
Implant Treatments in Anticipation of the Patient’s Aging
Based on the above restrictions, it is necessary to anticipate the patient’s aging when providing implant treatment for middle-aged and elderly patients.
-
Life expectancy: It is necessary to estimate the life expectancy based on the systemic conditions of the patient. At present, the sum of actual age and average life expectancy for elderly people is longer than the average life span [33]. Those who live to an old age live longer than the average life span. Therefore, we must consider how many more years the implants must function on average, based on the systemic conditions of the patient. The average life span for women is 87.05, but this does not mean that an 80-year-old woman will live only 7 more years; she is likely to live another 12 years or more on average.
-
As the patient’s care may be transferred to a different clinic, it is necessary to communicate the treatment information to the next dentist. According to a survey on elderly people who require nursing care [3••], two-thirds of implant patients had been treated by dentists who were not the dentists in charge of visiting care. To ensure such communication, it is recommended that an implant card/passport be issued at the end of treatment [34]. However, more than half of the dentists who provided implant treatments did not use such card/passport [3••]. Establishment and popularization of a standard are desired.
-
Removable upper structures are easier to handle when the situation changes later. While it is possible to handle with temporary cementation, performing final cementation makes it more difficult to handle in the future.
-
Two-piece implants are easier to handle in various ways later than one-piece implants. It is possible to remove the abutment and let the implant sleep. While it is of course possible to grind a one-piece type implant, it is extremely difficult to grind a titanium alloy in the environment of visiting care [35].
-
It is desirable to unify the type of implants present in the oral cavity. As it may become necessary to add implants and remanufacture the upper structure in the future due to the loss of remaining teeth, the implants in the oral cavity of one patient should be unified to one system. Especially when the care of the patient is transferred to a different clinic, it is more convenient to be able to handle with one implant system. Unless it is unavoidable, a patient should not be given a mixture of multiple systems. However, note that there may be dramatic structural changes even when the same system is adopted.
-
It is desirable to use a system from a manufacturer who can supply the components over long periods. At present, implant systems are supplied by more than 30 companies in Japan. It is safer to use a system from a manufacturer who will be supplying the components even after 10 or 20 years. While it is difficult to predict the future, it may be risky to adopt a brand-new system from an emerging manufacturer. We hope that replacement parts and tools will continue to be supplied in the future.
-
The patient will have reserve power and suffer fewer problems even when the functions deteriorate somewhat, if we can provide appropriate rehabilitation and so forth and improve the oral cavity functions in advance by anticipating the deterioration in oral cavity functions due to aging.
Policy Recommendations
-
It will become necessary for dentists who provide visiting dental care to learn knowledge and skills related to implants.
-
It is also necessary to provide education so that dentists who provide implant treatments can also provide visiting care.
-
It is important to ensure compatibility of tools. At present, the specifications of the screws that fix the super structure vary by manufacturer, and there are 10 or more different types in Japan. Different drivers are used for each of these, and using a driver of a different specification may damage the screw. Considering the handling in visiting dental care, it is difficult to keep many tools and also to determine the type of screw from its appearance. While standardizing the screw specifications would resolve this problem, this remains difficult due to the interests of respective manufacturers. It is important for academic societies and the government to take the initiative and promote standardization.
-
Implant treatments are not covered by insurance in Japan except for some cases of loss of jaw parts. Implant management and repair are not covered by health insurance, either. However, elderly patients who are admitted to facilities often face financial difficulties, and at present, the dentists in charge provide extremely troublesome implant management for free. Accordingly, positive measures by academic societies and the government are desired.
Conclusion
There are restrictions in implant treatments for elderly people such as risks in implant surgery, deterioration in implant functions, and deterioration in maintenance condition. The systemic conditions and aging of the oral cavity need to be taken into consideration regarding the risks of implant surgery. Appropriate evaluation and rehabilitation are important regarding deterioration in implant functions. As to the worsening of maintenance condition, changing to a removable superstructure as well as awareness-raising activities should be examined. In addition, we suggest that policy measures be taken to address some issues regarding training, manufacturers, and medical insurance. We hope that implant treatments will continue to contribute to patients as we head toward becoming a super-aging society.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
UN, World Population Ageing 2019: Highlights, Aging Report. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf [accessed 01.29.20].
Ministry of Health Labour and Welfare, Survey of Dental Diseases Fiscal Year 2016. https://www.mhlw.go.jp/toukei/list/dl/62-28-02.pdf (in Japanese) [accessed 01.29.20].
•• Sato Y, et al. A report on dental implants among dependent elderlies. From a survey of dental practitioners on actual conditions of dependent implant patients. Int J Implant Dent. 2018;14(4). https://doi.org/10.1186/s40729-018-0125-7This manuscript is a questionnaire survey asked about the situation of patients after implant treatment, the situation of implants in the context of home-visit dental care, and the usage status of the implant card.
Bornstein MM, Halbritter S, Harnisch H, Weber HP, Buser D. A retrospective analysis of patients referred for implant placement to a specialty clinic: indications, surgical procedures, and early failures. Int J Oral Maxillofac Implants. 2008;23(6):1109–16.
Brugger OE, Bornstein MM, Kuchler U, Janner SF, Chappuis V, Buser D. Implant therapy in a surgical specialty clinic: an analysis of patients, indications, surgical procedures, risk factors, and early failures. Int J Oral Maxillofac Implants. 2015;30(1):151–60.
Schimmel M, Müller F, Suter V, Buser D. Implants for elderly patients. Periodontol. 2017;73(1):228–40.
Sato Y, et al. Estimation of denture patients’ absolute number in elderly from survey of dental disease and vital statistics. Jpn J Dent Practice Administration. 2014;49(1):162–7 (in Japanese).
Shklar G. The effects of aging upon oral mucosa. J Invest Dermatol. 1966;47(2):115–20.
Löe H, Karring T. The three-dimensional morphology of the epithelium-connective tissue interface of the gingiva as related to age and sex. Scand J Dent Res. 1971;79(5):315–26.
Kotani Y, Sato Y, Kitagawa N, Shimodaira O, Takeuchi S, Isobe A, et al. Relationship between palatal mucosa properties and pressure-pain threshold in young dentulous and elderly edentulous subjects. Jap J Gerodont. 2015;30(1):68–79.
Bing L, et al. Xerostomia and salivary hypofunction in vulnerable elders, prevalence and etiology. Oral Surg Oral Me Oral Pathol Oral Radiol. 2012;114(1):52–60.
Tsuga K, Yoshikawa M, Oue H, Okazaki Y, Tsuchioka H, Maruyama M, et al. Maximal voluntary tongue pressure is decreased in Japanese frail elderly persons. Gerodontology. 2012;29(2):e1078–85.
Schwahn C, Polzer I, Haring R, Dörr M, Wallaschofski H, Kocher T, et al. Missing, unreplaced teeth and risk of all-cause and cardiovascular mortality. Int J Cardiol. 2013;167(4):1430–7.
Japanese Society of Gerodontology. Guidelines for dental treatment for people with dementia. Tokyo: Ishiyaku publishing; 2019. (in Japanese)
The Japanese Society of Oral Implantology, A report: survey of implant treatment in dental visits. https://www.shika-implant.org/publication/investigation.html (in Japanese) [accessed 01.29.20].
• Minakuchi S, et al. Oral hypofunction in the older population: position paper of the Japanese Society of Gerodontology in 2016. Gerodontology. 2018;35(4):317–24 This manuscript presents diagnostic criteria and management strategies to reduce the risk of oral hypofunction among older people.
Nakanishi N, Fukuda H, Takatorige T, Tatara K. Relationship between self-assessed masticatory disability and 9-year mortality in a cohort of community-residing elderly people. J Am Geriatr Soc. 2005;53(1):54–8.
Yoshida M, Morikawa H, Yoshikawa M, Tsuga K, Akagawa Y. Eight-year mortality associated with dental occlusion and denture use in community-dwelling elderly persons. Gerodontology. 2005;22(4):234–7.
Semba RD, Blaum CS, Bartali B, Xue QL, Ricks MO, Guralnik JM, et al. Denture use, malnutrition, frailty, and mortality among older women living in the community. J Nutr Health Aging. 2006;10(2):161–7.
Onder G, Liperoti R, Soldato M, Cipriani MC, Bernabei R, Landi F. Chewing problems and mortality in older adults in home care: results from the Aged in Home Care study. J Am Geriatr Soc. 2007;55(12):1961–6.
Lee MS, Huang Y-C, Wahlqvist ML. Chewing ability in conjunction with food intake and energy status in later life affects survival in Taiwanese with the metabolic syndrome. J Am Geriatr Soc. 2010;58(6):1072–80.
Tsai AC, Chang TL. Association of dental prosthetic condition with food consumption and risk of malnutrition and follow-up 4-year mortality risk in elderly Taiwanese. J Nutr Health Aging. 2011;15(4):265–70.
Ansai T, Takata Y, Soh I, Akifusa S, Sogame A, Shimada N, et al. Relationship between chewing ability and 4-year mortality in a cohort of 80-year-old Japanese people. Oral Dis. 2007;13(2):214–9.
Shimazaki Y, Soh I, Saito T, Yamashita Y, Koga T, Miyazaki H, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res. 2001;80(1):340–5.
Watt RG, Tsakos G, De Oliveira C, Hamer M. Tooth loss and cardiovascular disease mortality risk-results from the Scottish Health Survey. PLoS One. 2012;7(2):e30797.
Schwahn C, Polzer I, Haring R, Dörr M, Wallaschofski H, Kocher T, et al. Missing, unreplaced teeth and risk of allcause and cardiovascular mortality. Int J Cardiol. 2013;167(4):1430–7.
Saarela RK, Soini H, Hiltunen K, Muurinen S, Suominen M, Pitkälä K. Dentition status, malnutrition and mortality among older service housing residents. J Nutr Health Aging. 2014;18(1):34–8.
Janket SJ, Surakka M, Jones JA, Lam A, Schnell RA, Rose LM, et al. Removable dental prostheses and cardiovascular survival: a 15-year follow-up study. J Dent. 2013;41(8):740–6.
Ansai T, Takata Y, Soh I, Yoshida A, Hamasaki T, Awano S, et al. Association of chewing ability with cardiovascular disease mortality in the 80-year-old Japanese population. Eur J Cardiovasc Prev Rehabil. 2008;15(1):104–6.
Aida J, Kondo K, Yamamoto T, Hirai H, Nakade M, Osaka K, et al. Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. J Dent Res. 2011;90(9):1129–35.
•• Sato Y, Kitagawa N, Isobe A. Implant treatment in ultra-aged society. Jpn Dent Sci Rev. 2018;54(2):45–51 This article presents the review for the treatment of implant treatment in ultra-aged society.
Müller F, Schimmel M. Revised success criteria: GUEST EDITORIAL: revised success criteria: a vision to meet frailty and dependency in implant patients. Int J Oral Maxillofac Implants. 2016;31(1):15.
Ministry of Health Labour and Welfare, Abridged life tables for Japan 2015. https://www.mhlw.go.jp/english/database/db-hw/lifetb15/index.html [accessed 01.29.20].
Visser A, de Baat C, Hoeksema AR, Vissink A. Oral implants in dependent elderly persons: blessing or burden? Gerodontology. 2011;28(1):76–80.
Greenbaum DS, Masri R, Driscoll CF. Prosthodontic rehabilitation of dental implants with exposed threads: a clinical report. J Prosthet Dent. 2011;105(6):351–5.
Acknowledgments
We address special thanks to members of Department of Geriatric Dentistry, Showa University School of Dentistry.
Funding
This work was financially supported by Grant-in-Aid for Scientific Research (C) (Nos. 26462935, 16K11657) from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oral Disease and Nutrition
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sato, Y., Kitagawa, N. & Isobe, A. Current Consensus of Dental Implants in the Elderly—What Are the Limitations?. Curr Oral Health Rep 7, 321–326 (2020). https://doi.org/10.1007/s40496-020-00268-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-020-00268-0