Abstract
Background and Aims
Attention-Deficit/Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD) represent two of the most prevalent neurodevelopmental conditions, with prevalence rates of 5–7% and 0.6–1%, respectively. Despite their conceptually distinct phenotypes, ADHD and ASD are highly comorbid. This review is aimed at examining and synthesising the prevalence and profile of ASD-like symptoms in individuals with a primary diagnosis of ADHD across the lifespan in accordance with the Diagnostic and Statistical Manual, Fifth Edition (DSM-5; APA, 2013) diagnostic criteria.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, as discussed by (Moher et al. in PLOS Medicine, 6(7), e1000097, 2009; Page et al. in Systematic Reviews, 10(1), 89, 2021). Studies were identified through a systematic literature search of the databases: PsycINFO, Medline, CINAHL, Psychology and Behavioural Sciences Collection, and Scopus (N = 12,633). Articles were critically appraised according to established quality methodology criteria, and findings were summarised using narrative synthesis.
Results and Conclusion
A total of nine studies (ADHD individuals n = 548) were identified and included in the review. Of these studies, three were classified as having ‘good’ methodological quality, five as ‘fair’, and one as ‘poor’. These studies varied considerably in their methodological approach and assessment procedures. Overall, higher levels of ASD symptoms were found in individuals with ADHD compared to the general population. There was considerable variation in the reported prevalence of clinically significant ASD symptoms in individuals with ADHD, ranging from 15 to 64.3%. Clinical implications and considerations for further research are discussed.
Similar content being viewed by others
Attention-Deficit/Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD) represent two of the most prevalent neurodevelopmental conditions that are diagnosed in childhood (APA, 2013). Despite their conceptually distinct phenotypes, ADHD and ASD are highly comorbid (Grzadzinski et al., 2011). However, there is considerable variability in the reported rates of comorbid ASD identified in children and adolescents with a primary diagnosis of ADHD. Variability in findings can impede on accurate diagnosis and estimates of prevalence and, ultimately, on clinical management and treatment outcomes.
Despite being distinct conditions, several studies have also reported some overlap in symptoms between ADHD and ASD, including difficulties with attention, behaviour, social communication, sensory sensitivity, and cognitive flexibility/rigidity (Karalunas et al., 2018; Nijmeijer et al., 2009; Ronald et al., 2014). Overlap in some symptoms and behavioural parallels, at least at face value, can often lead to difficulties distinguishing between clinical presentations and misdiagnosis, especially in less experienced health professionals (Grzadzinski et al., 2016; Hollingdale et al., 2019). Synthesising our current understanding of the shared and unique challenges faced by individuals with both ADHD and ASD is an important research topic addressed in the present systematic review. The current systematic review aimed to examine and synthesise the prevalence and profile of ASD-like symptoms in individuals with a primary diagnosis of ADHD across the lifespan, with the hope to inform early and accurate differential diagnoses, as well as more accurate and targeted treatment plans.
Attention-Deficit/Hyperactivity Disorder (ADHD)
ADHD is one of the most common childhood disorders and is characterised by a persistent pattern of inattentive, hyperactive, or impulsive traits (APA, 2013). The worldwide pooled prevalence rate of ADHD in children is estimated at 5–7% (Hollingdale et al., 2019; Thomas et al., 2015). Studies have found that this estimation increases significantly in clinical samples, with one study identifying 44.5–68.5% of children referred to mental health services meeting diagnostic criteria for ADHD (Hansen et al., 2018). Clinical diagnoses typically fall under one of three presentations or subtypes: predominantly inattentive, hyperactive/impulsive, and combined presentations (APA, 2013). Classification under these subtypes is dependent on the proportion of hyperactive/impulsive and inattentive traits an individual presents with (APA, 2013). In addition to the core symptoms of hyperactivity, impulsivity, and inattention, children and adolescents with ADHD present with a wide range of significant and cascading functional impairments across a number of domains. This includes poorer school-based functioning, which often results in poor academic and educational outcomes (Cherkasova et al., 2013; Green et al., 2015; Larsson et al., 2011; Sciberras et al., 2014), as well as interpersonal difficulties (Gardner & Gerdes, 2015).
Autism Spectrum Disorder (ASD)
ASD is a neurodevelopmental disorder that is characterised by persistent impairments in social communication, social interaction, and restricted, repetitive patterns of behaviour, which may manifest through restricted interests or activities (APA, 2013). The estimated worldwide prevalence of ASD is between 0.6% and 1% (Elsabbagh et al., 2012; Hollingdale et al., 2019); however, the severity and presentation of ASD often differ between individuals. As the name suggests, ASD is increasingly understood as a dimensional condition (Constantino & Todd, 2003). It represents the extremes of the autistic spectrum, which extends throughout the general population (Constantino & Todd, 2003). In addition to the three core diagnostic domains, individuals with ASD present with a number of additional difficulties in a multitude of areas. As with ADHD, individuals with ASD often present with poorer educational and academic outcomes, social isolation, and reduced levels of autonomy (Posar & Visconti, 2019).
Diagnostic Overlap and Dual Diagnosis
In addition to those symptoms which are specific to ADHD or ASD, there are high rates of comorbidities amongst the two conditions, as is common in many neurodevelopmental conditions (May et al., 2016). Individuals diagnosed with ADHD or ASD are often subject to significant mood and behavioural disorders, such as anxiety or oppositional defiant disorder (Hollingdale et al., 2019). They are also at an elevated risk for a number of developmental conditions, including intellectual disability, specific learning disorder, and communication disorders (May et al., 2016). Given the profile of impairments seen in ADHD and ASD, as well as the increased risk of numerous comorbidities, it is not surprising that these conditions are often associated with poor long-term life outcomes. Although approximately one-third of individuals diagnosed with ADHD will show some improvement in clinical severity over time, impairments are lifelong and generally persist into adulthood (Cherkasova et al., 2013). Studies have reliably demonstrated that early diagnosis followed by comprehensive intervention is paramount in fostering more positive outcomes for affected individuals (May et al., 2016; Posar & Visconti, 2019). Consideration for early intervention is particularly important in cases where diagnostic overlap and comorbidity may obscure accurate diagnosis.
Prevalence Rates
Individuals with ADHD, on average, have significantly higher scores on measures of ASD symptomatology compared to the general population (Hollingdale et al., 2019). According to research across both clinical and community samples, between 4.68% and 50% of children and adolescents with a primary diagnosis of ADHD also meet diagnostic criteria for ASD (Green et al., 2015; Ronald et al., 2008a, 2008b; Van Der Meer et al., 2012). Variability in the frequency of co-occurring ADHD and ASD in children and adolescents is likely due to fundamental differences in methodological approaches to sampling, the ASD measures utilised, and clinical thresholds, such as the cut-off score used and different diagnostic approaches (Grzadzinski et al., 2011; Hollingdale et al., 2019). Indeed, the majority of the literature utilises symptom checklists and screeners—such as the Social Communication Questionnaire (SCQ), the Social Responsiveness Scale (SRS), and the Autism Spectrum Quotient (AQ)—over diagnostic tools or interviews, such as the ADOS or ADI-R (Antshel & Russo, 2019; Hollingdale et al., 2019; Reiersen et al., 2007). Moreover, most symptom checklists/screeners do not provide a comprehensive measure of the full set of ASD diagnostic criteria. It is important to understand social functioning in ADHD and how social dysfunction manifests in children and adolescents with ADHD, comparing and contrasting the social difficulties that occur in children and adolescents with ADHD alone, versus those with co-morbid diagnoses of ASD. It is also important to consider how the prevalence of ASD in children and adolescents with a primary diagnosis of ADHD is potentially impacted by methodological and clinical considerations, as discussed further in the section below.
Symptomatology
Individuals with ADHD share a number of cognitive, behavioural, and functional difficulties with individuals diagnosed with ASD (May et al., 2016). Whilst some studies report that individuals with ADHD present with elevated ASD symptoms across the three core domains of ASD—social interaction, communication, and repetitive behaviours (Nijmeijer et al., 2009)—others have reported elevations in social interaction (Ros & Garziano, 2018), communication (Kochhar et al., 2011), or repetitive behaviours alone (Polderman et al., 2014). Some studies have even found an overlap in communicative difficulties, as well as stereotyped and repetitive behaviours (Santosh & Mijovic, 2004). For instance, social difficulties are often reported in individuals with ADHD (Ros & Garziano, 2018). However, these difficulties are typically interpreted as secondary outcomes resulting from core ADHD symptoms, such as executive dysfunction, rather than those reflecting impairments in social skills and social motivation as seen in ASD (Grzadzinski et al., 2011). Children and adolescents with ADHD do not, for example, typically display social awkwardness or display core deficits in social reasoning or in recognising emotions in others, as is the case for their ASD counterparts.
Methodologically, it is also important for clinicians and researchers to consider the validity of the ASD measures when utilised in an ADHD population. That is, it may be unclear whether the constructs measured on ASD symptom rating scales are measuring the same constructs amongst those with ADHD (Antshel & Russo. 2019). Methodological variation in the literature, as well as the discrepancy seen in reports on behavioural and diagnostic parallels, may obscure clinically relevant information (Hollingdale et al., 2019). This can lead to difficulties in attempting to distinguish between the disorders and increased rates of missed or incorrect diagnoses and, ultimately, impact the quality of care available to affected individuals and families. This underscores the importance of understanding the boundaries and common factors between these disorders, both independently, and as comorbidities.
Diagnostic and Statistical Manual, 5th Edition
Prior to publication of the DSM-5, a dual diagnosis of both ADHD and ASD was not permitted, despite the overwhelming evidence of these being two distinct disorders (Hollingdale et al., 2019). The DSM-IV listed ADHD as an exclusionary criterion for the diagnosis of ASD (APA, 2000). It also prohibited the diagnosis of ADHD if inattentive or hyperactive/impulsive traits presented during the course of a pervasive developmental disorder (APA, 2000). This often resulted in children and their families being underdiagnosed which ultimately restricted their access to more comprehensive and targeted clinical care (Hollingdale et al., 2019). However, the DSM-5 takes more recent findings into consideration. This includes the high rates of comorbidity found between ADHD and ASD in epidemiological studies (Simonoff et al., 2008; Zablotsky et al., 2020), as well as the significant symptom overlap in population-based twin studies (Pinto et al., 2016; Ronald et al., 2008a, 2008b). As such, the DSM-5 now permits a dual diagnosis of both ADHD and ASD. In recent years, this has provided clinicians and researchers with the opportunity to acknowledge and further investigate discrete and clinically converging presentations of ADHD and ASD (Grzadzinski et al., 2016; Ronald et al., 2014). Although our understanding of the characteristics and challenges that are unique to a dual diagnosis is growing, the literature remains limited and, in most cases, significantly varied.
Current Study
When considering all factors—the overlap in some symptoms, the high comorbidity, the inconsistency in the literature, and the recent changes to the DSM-5—there is a clear need to better synthesise and develop our understanding not only of the prevalence, but also of the clinical presentation of comorbid ADHD and ASD. To date, few studies have attempted to examine and synthesise the profile of ASD-like symptoms in individuals with ADHD, for example, which ASD symptoms most commonly overlap in individuals with ADHD, and which are distinct. These studies have utilised varying methodologies and assessment techniques, which may have contributed to the inconsistencies seen in the literature. As such, combining the findings from these studies may provide a more accurate representation not only of the prevalence of ASD in individuals with ADHD but also of their unique and distinct clinical profiles. This systematic review sought to answer the following core questions: (1) what proportion of individuals with ADHD across the life span meet DSM-5 diagnostic criteria or clinical cut-off for ASD and (2) which ASD-like symptoms are most commonly shared amongst individuals with ADHD. Ultimately, these findings will broaden our understanding of the unique and shared difficulties that affected individuals face in their day-to-day lives.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009; Page et al., 2021).
Eligibility Criteria
Inclusion and Exclusion Criteria
To be included in this review, published studies were required to meet the following criteria: (1) participants had a diagnosis of ADHD made by a qualified clinician and/or documented in medical records as per DSM-5 criteria; (2) ASD symptoms were measured using a standardised questionnaire, screening tool, or diagnostic tool; (3) the study reports original empirical data; (4) the article was published in a peer-reviewed journal; and (5) studies were published in the English language.
The current systematic review excluded studies where measures of ASD symptoms in participants with ADHD could not be isolated from other participant groups (i.e. other developmental/genetic disorders or acquired brain injury). Dissertations, book chapters, expert reviews, and conference abstracts without full text or original data were excluded. Restrictions were not placed on the age of participants, sample size, or publication date.
Information Sources
Studies were identified through a systematic literature search of the following databases: PsycINFO, Medline, CINAHL, and Scopus and Psychology and Behavioural Sciences Collection. No date limit was applied. The last search was run in June 2022. Subject headings and keywords were used where available.
Search Strategy
The search strategy was adapted for each specific database. The search terms were as follows: ((attention deficit hyperactivity disorder) OR (ADHD) OR (attention deficit disorder) OR (ADD) OR (hyperkinetic disorder)) AND ((autism spectrum disorder) OR (autism) OR (ASD) OR (asperger’s syndrome) OR (pervasive developmental disorder) OR (PDD)). We maintained DSM-IV terminology (e.g. asperger’s syndrome) in our search, as the literature often lags behind clinical updates, and these DSM-IV terms have been used in many studies, even after introduction of the DSM-5.
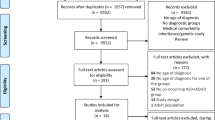
Study Selection
The study selection process was carried out in accordance with the PRISMA guidelines (Moher et al., 2009; Page et al., 2021). Duplicate articles were removed via Rayyan, and studies were reviewed for their suitability in accordance with the eligibility criteria. Studies were screened by title, abstract, and full text for inclusion. The screening process was completed independently by two researchers and yielded a 99.98% agreement rate. Disagreements were resolved through discussion and consensus.
Data Collection Process and Synthesis of Results
Data was extracted from each study by one researcher. Information extracted included country of origin, total sample size, sample source, participant characteristics (i.e. age and sex), recruitment methodology (i.e. inclusion and exclusion criteria), medication use, ASD outcome measure, results (i.e. means and standard deviations), and quality appraisal (i.e. strengths and weaknesses). Study characteristics and findings are summarised and synthesised in Table 1.
Methodological Quality and Risk of Bias
The methodological quality of each article was assessed using established quality assessment tools by the Joanna Briggs Institute (JBI). The JBI has developed a set of quality assessment tools that are tailored to various study designs, including analytical cross-sectional studies and case–control studies. The quality assessment was undertaken by two independent researchers and yielded an 88.9% agreement rate. Disagreements (n = 1) were resolved through further analysis and discussion until a consensus was reached. These tools guided the critical appraisal of each study and helped to inform classification based on a predetermined cut-off criteria which were modelled after a previous review (Camm et al., 2021). Studies were classified as ‘good’ if ≥ 75% of the items were satisfied, ‘fair’ if 50–74% of the items were satisfied, or ‘poor’ if < 50% of the items were satisfied.
Results
A flow diagram of the search strategy and screening process is presented in Fig. 1. A total of nine studies were identified that met all inclusion/exclusion criteria. Table 1 shows the study characteristics of the studies included in the review. Two studies were inaccessible online, and authors were contacted directly (Schwenck et al., 2014; Stordeur et al., 2019). The requests yielded no response from the authors, and, therefore, these papers were omitted from further analysis.
Study Characteristics
Of the nine studies that were selected for the review, the majority were cross-sectional studies (Dellapiazza et al., 2021; Guttentag et al., 2022; Hayashi et al., 2021; Mouti et al., 2019; Nakagawa et al., 2021; Ng et al., 2021; Okyar & Gorker, 2020; Pehlivanidis et al., 2021) and one was a case–control study (Ahmed et al., 2021).
Participants
The selected studies included a total of 1251 participants (ADHD individuals n = 548) from seven countries. The majority of studies included children and adolescents aged 6 to 18 years (Ahmed et al., 2021; Dellapiazza et al., 2021; Guttentag et al., 2022; Mouti et al., 2019; Ng et al., 2021; Okyar & Gorker, 2020). Three studies included adults aged 18 to 65 years (Hayashi et al., 2021; Nakagawa et al., 2021; Pehlivanidis et al., 2021). ADHD diagnoses were confirmed through review of medical documentation (Dellapiazza et al., 2021; Mouti et al., 2019; Pehlivanidis et al., 2021), structured interview (Nakagawa et al., 2021; Okyar & Gorker, 2020), and consensus between qualified clinicians (Guttentag et al., 2022; Hayashi et al., 2021; Ng et al., 2021). Three studies reported the proportions of each ADHD subtype within their sample (Guttentag et al., 2022; Ng et al., 2021; Okyar & Gorker, 2020). These samples consisted predominantly of individuals with the combined or hyperactive/impulsive subtype of ADHD, followed by the inattentive subtype (see Table 1). One study reported a small percentage of ADHD-other specified (Guttentag et al., 2022; APA, 2013). Six studies did not report ADHD subtype within their samples (Ahmed et al., 2021; Dellapiazza et al., 2021; Hayashi et al., 2021; Mouti et al., 2019; Nakagawa et al., 2021; Pehlivanidis et al., 2021). Participants tended to be recruited through convenience, largely from clinical populations. One study recruited participants from both clinical referrals and community populations (i.e. web postings, parent groups, word-of-mouth, mailing lists, and direct mail; Guttentag et al., 2022). All studies were published in 2019 or later, likely reflecting a lag in the literature following implementation of the new DSM-V criteria, whereby, as mentioned, prior to publication of the DSM-5, a dual diagnosis of both ADHD and ASD was not permitted, despite the overwhelming evidence of these being two distinct disorders (Hollingdale et al., 2019).
Six studies reported inclusion (Guttentag et al., 2022; Mouti et al., 2019; Ng et al., 2021; Okyar & Gorker, 2020) and exclusion (Dellapiazza et al., 2021; Hayashi et al., 2021) of participants who were receiving pharmacological intervention for their attention deficits. When included, the majority of individuals with ADHD were receiving pharmacological intervention for ADHD (> 50%), aside from one study which reported only 17% (Guttentag et al., 2022). One study also reported 56.5% of individuals with ADHD receiving other non-pharmaceutical interventions (e.g. psychological intervention; Mouti et al., 2019). Three studies did not specify current or previous use of medication in their samples (Ahmed et al., 2021; Nakagawa et al., 2021; Pehlivanidis et al., 2021). Of note, three studies excluded participants with ADHD who met DSM-5 diagnostic criteria for ASD (Guttentag et al., 2022; Nakagawa et al., 2021; Okyar & Gorker, 2020). Two studies did not exclude participants with ADHD who had clinical levels of ASD symptoms or met diagnostic criteria for ASD (Ahmed et al., 2021; Hayashi et al., 2021). Four studies separated ADHD-only groups (i.e. ADHD without comorbid ASD) and comorbid ASD and ADHD (ASD + ADHD) groups (Dellapiazza et al., 2021; Ng et al., 2021; Pehlivanidis et al., 2021; Mouti et al., 2019).
Methodological Quality
Study strengths and weaknesses were assessed against the JBI quality assessment tools for cross-sectional and cohort studies (see Appendix). All studies were included in the synthesis. Overall, three studies were classified as good, five as fair, and one as poor. Methodological strengths included the following: clearly defined sample inclusion criteria (100%, n = 9) and objective confirmation of ADHD diagnoses according to DSM-5 diagnostic criteria (100%, n = 9). Weakness of the reviewed studies included omission of important sample characteristics (77.8%, n = 7), including ADHD medication use (33.3%, n = 3) and ADHD subtype (66.7%, n = 6), lack of control for potential confounding factors (77.8%, n = 7), and poor quality of ASD-outcome measure, including use of screeners/symptom checklists (66.7%, n = 6).
ASD Measures
The majority of the studies utilised ASD-symptom screeners, including the Autism Quotient (Nakagawa et al., 2021; Pehlivanidis et al., 2021), Social Responsiveness Scale (Dellapiazza et al., 2021), Social Communication Questionnaire (Mouti et al., 2019), Autism Behaviour Checklist (Okyar & Gorker, 2020), and Childhood Autism Spectrum Test (Ahmed et al., 2021). Three studies used the Autism Diagnostic Observation Scale (ADOS; Guttentag et al., 2022; Hayashi et al., 2021; Ng et al., 2021).
ASD Symptoms in ADHD
Autism-Spectrum Quotient (AQ)
The AQ is a 50-item self-report screener for ASD symptoms with five subscales (i.e. social skills, attention switching, attention to detail, communication, and imagination) and a total score (Baron-Cohen et al., 2001). Nakagawa et al. (2021) found that adults with ADHD averaged significantly higher AQ scores when compared to typically developing controls and lower AQ scores compared to adults with ASD. Further domain-specific analyses were not explored. Pehlivanidis et al. (2021) found that most domains of the AQ were significantly lower in adults with ADHD compared to those with ASD (i.e. social skills, attention switching, communication, and imagination), with the exception of attention to detail, which failed to differ significantly between ADHD and ASD groups. Hayashi et al. (2021) found that 64.3% of adults with ADHD met clinical cut-off (≥ 33) on the AQ.
Social Responsiveness Scale (SRS)
The SRS is a 65-item screener for ASD symptoms with five subscales (social awareness, social cognition, social communication, social motivation, and restrictive and repetitive behaviours) and a total score (Constantino & Gruber, 2012). Dellapiazza et al. (2021) found that, overall, children with ADHD had significant levels of social impairment across all domains of the SRS. However, children with ASD and ASD + ADHD had significantly higher scores than the ADHD group alone across every domain, aside from social awareness which was lower for the ADHD group than those in the ASD, ASD + ADHD, and typically developing groups. Children with ADHD were also found to have comparable scores on social motivation with typically developing controls. Conversely, Ng et al. (2021) found no group differences between children with ADHD, ASD, or combined ASD and ADHD on parent ratings for the SRS.
Social Communication Questionnaire (SCQ)
The SCQ is a 40-item screener for ASD symptoms with three subscales (reciprocal social interaction, language and communication, and stereotyped patterns of behaviour) and a total score (Rutter et al., 2003). Mouti et al. (2019) found that children and adolescents with ADHD had significantly higher mean scores across the SCQ when compared to typically developing controls. However, the ADHD group was found to have significantly lower mean scores on SCQ total, as well as the social communication and repetitive behaviour domains compared to the ASD and ASD + ADHD groups.
Autism Behaviour Checklist (ABC)
The ABC is a 57-item screener for ASD symptoms with five subscales (sensory, relating, body and object use, language, and social skills) and a total score. Okyar and Gorker (2020) found that children and adolescents with ADHD had significantly higher scores across all domains of the ABC compared to typically developing controls. There were significantly higher total scores in males compared to females with ADHD. Impairments in social skills were significantly higher in individuals with combined ADHD compared to predominantly inattentive or hyperactive/impulsive subtypes.
Childhood Autism Spectrum Test (CAST)
The CAST is a 37-item screener for ASD symptoms, measuring social, and communication skills (Scott et al., 2002). Ahmed et al. (2021) found a low occurrence of clinically significant levels of autistic symptoms in children with ADHD (15%); however, this rate did not reach statistically significant when compared to typically developing controls.
Autism Diagnostic Observation Scale (ADOS)
The ADOS is a semi-structured, diagnostic assessment of ASD which can be utilised across age groups, developmental levels, and language skills (Lord et al., 2012). The ADOS is designed to elicit behaviours directly related to a diagnosis of ASD, ranging across domains of communication, social interaction, play, and restrictive and repetitive behaviours (Lord et al., 2012). Using Module 4 of the ADOS-2, Hayashi et al. (2021) found that social reciprocal interaction scores tended to be higher, whilst restricted and repetitive behaviour scores were lower in an adult ADHD sample. Overall, 23.3% of the ADHD sample met diagnostic criteria for autism on the ADOS-2. Items constituting language and communication, reciprocal social interaction, and imagination differentiated between ASD and non-ASD individuals with ADHD, whilst restrictive and repetitive behaviours and other abnormal behaviours did not. Guttentag et al. (2022) and Ng et al. (2021) found that, in children and adolescents, group mean scores across Module 3 of the ADOS were significantly higher in the ASD group relative to the ADHD group.
Prevalence of ASD in ADHD
Two studies reported on the clinical prevalence of ASD within their ADHD samples. Prevalence ranged widely depending on the measures used. It is important to note that only one of the two studies used a diagnostic measure—the ADOS-2 (Hayashi et al., 2021). In children with ADHD aged 6–11 years, Ahmed et al. (2021) reported a prevalence of 15% in terms of clinical levels of ASD on the CAST, though this did not reach statistical significance when compared to typically developing controls. Amongst adults with ADHD, 64.3% endorsed clinical levels of ASD symptoms on the AQ. However, in the same sample, only 23.3% met diagnostic criteria for ASD on the ADOS-2 (Hayashi et al., 2021). Pehlivanidis et al. (2021) found that in a sample of 238 adults who were assessed over a three-year period at an adult neurodevelopmental outpatient clinic, 16.1% of adults diagnosed with ADHD also met diagnostic criteria for ASD. These diagnoses were made by consensus of multidisciplinary teams, based on results of screening measures (namely, the AQ and Barkley Adult ADHD Rating Scale-IV) and diagnostic measures in complex cases (i.e. diagnostic interview for ADHD in adults and the ADOS). No studies included in the current systematic review reported on ASD level or severity.
ADHD Severity
Whilst not the primary focus of the present systematic review, studies assessing the association between ADHD severity and ASD symptoms are summarised below. In children aged 6–12 years, Dellapiazza et al. (2021) found that as ADHD severity increased (qualified as the DSM-oriented scale of the Child Behaviour Checklist), so too did social impairments. Likewise, Ng et al. (2021) found that greater social impairment (as measured by the SRS) was associated with greater parent-reported inattentive and hyperactive/impulsive symptoms in children and adolescents (as measured by the Connors Third Edition—Parent Report). Social skill subscale scores (as measured by the ABC) were significantly higher in children diagnosed with the predominantly combined ADHD presentation than the predominantly inattentive or hyperactive/impulsive presentations (Okyar & Gorker, 2020). There were no significant differences between ADHD subtypes and all other ABC subscales (i.e. sensory, relating, body and object use, and language).
Discussion
To the authors’ knowledge, this was the first systematic review to examine and synthesise the prevalence and profile of ASD-like symptoms in individuals with a primary diagnosis of ADHD across the lifespan in accordance with the DSM-5 diagnostic criteria. In the nine studies reviewed, higher levels of ASD symptoms were found in individuals with ADHD compared to non-ADHD controls. Mean scores reported across five studies suggested that individuals with ADHD were more impaired on domains of social cognition/communication than domains of restrictive and repetitive behaviours. However, it should be noted that only one study directly assessed this trend using Module 4 of the ADOS-2 (Hayashi et al., 2021), which has been critiqued on its ability to elicit restrictive and repetitive behaviours even in adults with ASD (Hus & Lord, 2014). Finally, there was significant variation in the proportion of individuals with ADHD who also presented with clinically significant levels of ASD symptoms, ranging from 15% (Ahmed et al., 2021) to 64.3% (Hayashi et al., 2021). This wide range most likely reflects methodological differences across studies, such as the quality of the ASD measure used (e.g. whether it was simply a symptom checklist, a diagnostic screener, or a gold standard diagnostic instrument). Overall, paucity of the current literature and variation in assessment tools and analytical methods between studies reduced comparability between findings and limited the conclusions that could be drawn from the wider literature.
All studies included in the present systematic review utilised standardised measures of ASD symptomatology. However, there was considerable variability in their quality, with most studies favouring screeners over more comprehensive diagnostic tools. These screeners often provided a limited and unidimensional perspective of the full ASD continuum. For instance, ASD screeners developed under previous diagnostic understandings often have a focus on social impairment and omit items assessing for restrictive and repetitive behaviours—the presence of which would be required to make a clinical diagnosis under the current DSM-5 (APA, 2013). This calls into question their suitability to validly measure a continuum of ASD symptoms as per the DSM-5. Moving forward, care should be taken in the selection of ASD measurement tools such that diagnostic measures are utilised over symptom checklists. Future studies should also endeavour to assess the validity of existing tools against current diagnostic standards.
Similarly, the majority of studies included in the present systematic review largely relied on informant- and self-report measures over and above clinician-administered measures or diagnostic interviews. Care should be taken in the interpretation of self-reported findings in neurodevelopmental populations where metacognitive and introspective skills may be impaired (Grainger et al., 2014; Johnson et al., 2009). Poor insight and awareness of ASD traits may result in an over-reporting of social and functional competencies and an under-reporting of ASD symptoms (Johnson et al., 2009). Similarly, the extent to which informants agree on measures of social impairment varies significantly, with some studies reporting only poor to fair agreement between parents and teacher (Kaat et al., 2013). Several studies have also reported that parents generally rate their children as more impairment than other informants. This has been shown across the core symptoms of ASD (Ronald et al., 2008a, 2008b) as well as specific social (Murray et al., 2009) and behavioural impairments (Foley-Nicpon et al., 2010). Ideally, future research should endeavour to utilise more objective diagnostic assessments of ASD symptomatology, including the ADOS (Lord et al., 2012), preferably in combination with a diagnostic interview such as the ADI-R (Lord et al., 1994). These challenges may also be alleviated, in part, through use of multiple informants (Möricke et al., 2016). This is especially relevant in the context of both ADHD and ASD where behaviour between contexts may vary and the ability to generalise skills across contexts and settings may be impaired.
Many of the studies included in this systematic review omitted important information regarding sample characteristics, such as the use of ADHD medication, and other concurrent interventions. Clinical practise is often informed by empirical literature, and research should adequately and systematically reflect the population under consideration. In recent years, use of ADHD medication has markedly increased across all age groups (Bachmann et al., 2017; Johansen et al., 2015). As this trend continues to grow, there is a need to better understand the implications of medication on subsequent non-core ADHD symptoms. For instance, medically managing overt inattentive or hyperactive/impulsive symptoms may allow for more accurate assessment of underlying social impairment. This may inform clinical practise for reassessment of social impairment following pharmaceutical intervention. Despite this, there is no clear delineation of the effects of medication on subsequent ASD-symptom expression in the current literature. Three studies included in this review failed to report use of medication, two studies excluded participants receiving pharmaceutical intervention and, when medication use was reported in four studies, the effects of medication on ASD symptom presentation were not explored. Overlooking the effects of pharmacological intervention may result in an underestimation of ASD symptoms in individuals with ADHD, as ADHD symptoms may, for example, mask the ASD, if unmedicated (Levy et al., 2010). As such, future studies should investigate the difference in ASD symptomatology between drug-naive and medicated individuals with ADHD as well as the effect of other co-occurring interventions.
Similarly, only three studies included in the current systematic review reported on specific ADHD subtypes/presentations (inattentive, hyperactive/impulsive, or combined; APA, 2013) within their samples. Within these three studies, there was an overrepresentation of the predominantly combined and inattentive ADHD presentations compared to the predominantly hyperactive/impulsive presentation (see Table 1). Averaging across ADHD subtypes may mask important distinctions in ASD symptomatology between groups. For instance, previous studies have found that individuals with the predominantly combined ADHD presentation are generally reported to experience more severe ASD symptomatology followed by the predominantly inattentive presentation and finally the predominantly hyperactive/impulsive presentation (Murray, 2010). However, it is unclear how changes within the DSM-5, which have lowered symptom threshold for ADHD diagnoses and increased symptom requirements for ASD diagnoses, may affect these trends. As such, further research is needed to assess whether ASD symptoms vary as a function of ADHD subtype against the current DSM-5 criteria. These findings will also pose significant implications for subsequent therapeutic approaches and may inform more specific and targeted interventions.
Individuals diagnosed with ADHD are often subject to a number of co-occurring conditions. In the current review, only two studies reported on the proportion of individuals with co-occurring mood or anxiety disorder within their samples (Guttentag et al., 2022; Ng et al., 2021). However, no studies systematically analysed the potential impact of these psychiatric comorbidities on subsequent ASD symptomatology. It is important to note that psychiatric comorbidities such as depression and anxiety may differentially influence social skills and repetitive behaviours under unique mechanisms separate to those typically seen in ASD (Becker et al., 2015; Joyce et al., 2017). As such, future studies should include more comprehensive inventories of mood and other psychiatric disorders to assess and help elucidate mood- and ASD-specific aetiology.
It is also important to consider the populations in which samples were drawn throughout the literature. All studies included in this systematic review utilised convenience samples that drew largely from clinical populations. Individuals drawn from clinical samples tend to be more severely impaired (Bauermeister et al., 2007). In a previous study, clinical samples of children and adolescents with ADHD tended to report higher prevalence rates of ASD symptomatology and degree of impairment than community samples (Bauermeister et al., 2007; Hollingdale et al., 2019). As such, favour for clinical samples in the current literature may reduce the generalisability of subsequent findings to the wider ADHD population. Future studies should endeavour to draw samples from more representative populations with a wider range of functioning. Consideration for whether the presentation of ASD symptoms in individuals with ADHD varies across both clinical and community populations may also be warranted.
Limitations of the Current Systematic Review
The current PRISMA-guided systematic review (Moher et al., 2009; Page et al., 2021) had a number of limitations that must be considered. First, only studies published in the English language were included. Although the nine studies included in this systematic review spanned seven different countries and five continents, this still represents a point of potential bias and may reduce the overall generalisability of results. Moreover, this systematic review was limited to published studies, which, whilst ensuring a peer-reviewed process, increased the risk of publication bias and may limit the current review representation of the wider literature, particularly those studies that report null or non-significant results. Finally, this systematic review included a relatively small number of studies. These studies varied significantly in their approach to methodology and assessment of ASD symptomatology, and most were rated as having poor or fair methodological quality according to JBI critical appraisal tools, all of which also limited the conclusions that could be made.
Notably, this systematic review also considered literature on both child and adolescent as well as adult populations. However, given the limited empirical evidence available, as well as the variability in methodology, no reliable comparisons could be made between age groups at the current time. There was also an underrepresentation of literature on adults with ADHD in the studies included in this systematic review, with only three studies including participants over 18 years of age. Moreover, two of the three studies did not report an age range for their samples, further clouding the interpretation of these findings. Previous literature has suggested that both ADHD and ASD symptoms are not stable across the lifespan, with some symptom dimensions being more persistent than others, such as social communication and restrictive and repetitive behaviours, respectively (Hartman et al., 2016). Given that both ADHD and ASD often extend well into adulthood (Cherkasova et al., 2013), there is a clear necessity to better understand how the profile and stability of ASD symptomatology in individuals with ADHD may change across the lifespan.
Clinical Implications
At present, the high rates of comorbidity and frequency of overlap in symptomatology reported in the literature indicate the necessity to consider the presence of ASD traits and a possibly co-occurring ASD diagnosis when working clinically with individuals with ADHD. Although levels of ASD symptoms may not meet clinical significance in the wider ADHD population, even the presence of subclinical levels can still impede on therapeutic and functional outcomes. For instance, restrictive thought processes and poor metacognitive skills typically associated with ASD may make generalising strategies across multiple contexts difficult for some individuals with ADHD who also experience symptoms of ASD (Hollingdale et al., 2019). This further highlights the necessity for clinical practise to move away from specialised ADHD or ASD services and accommodate for the complexities and nuances of both clinical and subclinical ASD symptom co-occurrence in ADHD. Ultimately, a clearer understanding on the presence and nature of ASD symptoms in individuals with ADHD will more accurately inform intervention strategies and policy development.
Summary and Conclusion
The current systematic review evaluated studies of ASD prevalence and symptoms in individuals with a primary diagnosis of ADHD across the lifespan and was the first of its kind. The findings from this systematic review suggest high levels of ASD symptoms in both children and adults with ADHD compared to the general population. However, the literature remains sparse and inconsistencies in methodological and assessment procedures limit the conclusions that can be drawn at this time, warranting the need for further research in this field. At the least, findings from the present review indicate high rates of ASD symptomology in individuals with ADHD with diagnoses made in accordance with the DSM-5.
This systematic review highlights a clear need for the use of more scientifically rigorous methodology and more research on this important topic. Future studies should endeavour to utilise psychometrically robust ASD diagnostic measures based on the DSM-5, such as the ADOS-2 in combination with diagnostic interviews, over symptom checklists, which may not provide a comprehensive or valid profile/diagnosis. This should incorporate both clinician-rated measures and input from multiple informants. Future studies should also ensure that ADHD samples adequately and systematically reflect the population under consideration. This may include extending analyses across specific ADHD subtypes and a stronger consideration for the effects of intervention on symptom expression, including the use of ADHD medication. Care should also be taken to ensure that samples represent the full spectrum of ADHD and ASD by drawing samples from both clinical and community population with a wider range of functioning. This will ultimately go on to inform early and accurate differential diagnoses, as well as more accurate and targeted treatment plans.
References
Ahmed, G. K., Darwish, A. M., Khalifa, H., & Khashbah, M. A. (2021). Evaluation of psychiatric comorbidity in attention-deficit hyperactivity disorder with epilepsy: A case-control study. Epilepsy Research, 169, 106505. https://doi.org/10.1016/j.eplepsyres.2020.106505
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). American Psychiatric Association.
American Psychiatric Association, & Psychiatry Online. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5TH ed.). American Psychiatric Association.
Bachmann, C. J., Wijlaars, L. P., Kalverdijk, L. J., Burcu, M., Glaeske, G., Schuiling-Veninga, C. C. M., Hoffmann, F., Aagaard, L., & Zito, J. M. (2017). Trends in ADHD medication use in children and adolescents in five western countries, 2005–2012. European Neuropsychopharmacology, 27(5), 484–493. https://doi.org/10.1016/j.euroneuro.2017.03.002
Baron-Cohen, S., Wheelwright, S., Skinner, R., Martin, J., & Clubley, E. (2001). The autism-spectrum quotient (AQ): Evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders, 31(1), 5–17. https://doi.org/10.1023/A:1005653411471
Bauermeister, J. J., Shrout, P. E., Ramirez, R., Bravo, M., Alegria, M., Martinez-Taboas, A., Chavez, L., Rubio-Stipec, M., Garcia, P., Ribera, J. C., & Canino, G. (2007). ADHD correlates, comorbidity, and impairment in community and treated samples of children and adolescents. Journal of Abnormal Child Psychology, 35(6), 883–898. https://doi.org/10.1007/s10802-007-9141-4
Becker, S. P., Langberg, J. M., Evans, S. W., Girio-Herrera, E., & Vaughn, A. J. (2015). Differentiating anxiety and depression in relation to the social functioning of young adolescents with ADHD. Journal of Clinical Child and Adolescent Psychology, 44(6), 1015–1029. https://doi.org/10.1080/15374416.2014.930689
Camm, S., Porter, M., Brooks, A., Boulton, K., & Veloso, G. C. (2021). Cognitive interventions for children with acquired brain injury: A systematic review. Neuropsychological Rehabilitation, 31(4), 621–666. https://doi.org/10.1080/09602011.2020.1722714
Cherkasova, M., Sulla, E. M., Dalena, K. L., Pondé, M. P., & Hechtman, L. (2013). Developmental course of attention deficit hyperactivity disorder and its predictors. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 22(1), 47–54.
Constantino, J. N., & Gruber, C. P. (2012). Social responsiveness scale (second edition): SRS-2. Western psychological services.
Constantino, J. N., & Todd, R. D. (2003). Autistic traits in the general population: A twin study. Archives of General Psychiatry, 60(5), 524–530. https://doi.org/10.1001/archpsyc.60.5.524
Dellapiazza, F., Audras-Torrent, L., Michelon, C., & Baghdadli, A. (2021). Clinical characteristics of children with ASD and comorbid ADHD: Association with social impairment and externalizing and internalizing behaviours. Research in Developmental Disabilities, 113, 103930. https://doi.org/10.1016/j.ridd.2021.103930
Elsabbagh, M., Divan, G., Koh, Y., Kim, Y. S., Kauchali, S., Marcín, C., Montiel-Nava, C., Patel, V., Paula, C. S., Wang, C., Yasamy, M. T., & Fombonne, E. (2012). Global prevalence of autism and other pervasive developmental disorders. Autism Research, 5(3), 160–179. https://doi.org/10.1002/aur.239
Foley-Nicpon, M., Doobay, A. F., & Assouline, S. G. (2010). Parent, teacher, and self-perceptions of psychosocial functioning in intellectually gifted children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 40(8), 1028–1038. https://doi.org/10.1007/s10803-010-0952-8
Gardner, D. M., & Gerdes, A. C. (2015). A review of peer relationships and friendships in youth with ADHD. Journal of Attention Disorders, 19(10), 844–855. https://doi.org/10.1177/1087054713501552
Grainger, C., Williams, D. M., & Lind, S. E. (2014). Metacognition, metamemory, and mindreading in high-functioning adults with autism spectrum disorder. Journal of Abnormal Psychology, 123(3), 650–659. https://doi.org/10.1037/a0036531
Green, J. L., Rinehart, N., Anderson, V., Nicholson, J. M., Jongeling, B., & Sciberras, E. (2015). Autism spectrum disorder symptoms in children with ADHD: A community-based study. Research in Developmental Disabilities, 47, 175–184. https://doi.org/10.1016/j.ridd.2015.09.016
Grzadzinski, R., Di Martino, A., Brady, E., Mairena, M., O’Neale, A., Petkova, M., Lord, E., & Castellanos, C. (2011). Examining autistic traits in children with ADHD: Does the autism spectrum extend to ADHD? Journal of Autism and Developmental Disorders, 41(9), 1178–1191. https://doi.org/10.1007/s10803-010-1135-3
Grzadzinski, R., Dick, C., Lord, C., & Bishop, S. (2016). Parent-reported and clinician-observed autism spectrum disorder (ASD) symptoms in children with attention deficit/hyperactivity disorder (ADHD): Implications for practice under DSM-5. Molecular Autism, 7(4), 7. https://doi.org/10.1186/s13229-016-0072-1
Guttentag, S., Bishop, S., Doggett, R., Shalev, R., Kaplan, M., Dyson, M., Cohen, M., Lord, C., & Di Martino, A. (2022). The utility of parent-report screening tools in differentiating autism versus attention-deficit/hyperactivity disorder in school-age children. Autism: The International Journal of Research and Practice, 26(2), 473–487. https://doi.org/10.1177/13623613211030071
Hansen, B. H., Oerbeck, B., Skirbekk, B., Petrovski, B. É., & Kristensen, H. (2018). Neurodevelopmental disorders: prevalence and comorbidity in children referred to mental health services. Nordic Journal of Psychiatry, 72(4), 285–291. https://doi.org/10.1080/08039488.2018.1444087
Hartman, C. A., Geurts, H. M., Franke, B., Buitelaar, J. K., & Rommelse, N. N. (2016). Changing ASD-ADHD symptom co-occurrence across the lifespan with adolescence as crucial time window: Illustrating the need to go beyond childhood. Neuroscience & Biobehavioral Reviews, 71, 529–541. https://doi.org/10.1016/j.neubiorev.2016.09.003
Hayashi, W., Hanawa, Y., Yuriko, I., Aoyagi, K., Saga, N., Nakamura, D., & Iwanami, A. (2021). ASD symptoms in adults with ADHD: A preliminary study using the ADOS-2. European Archives of Psychiatry and Clinical Neuroscience, 272(2), 217–232. https://doi.org/10.1007/s00406-021-01250-2
Hollingdale, J., Woodhouse, E., Young, S., Fridman, A., & Mandy, W. (2019). Autistic spectrum disorder symptoms in children and adolescents with attention-deficit/hyperactivity disorder: A meta-analytical review. Psychological Medicine, 50(13), 2240–2253. https://doi.org/10.1017/S0033291719002368
Hus, V., & Lord, C. (2014). The autism diagnostic observation schedule, module 4: Revised algorithm and standardized severity scores. Journal of Autism and Developmental Disorders, 44(8), 1996–2012. https://doi.org/10.1007/s10803-014-2080-3
Johansen, M. E., Matic, K., & McAlearney, A. S. (2015). Attention deficit hyperactivity disorder medication use among teens and young adults. Journal of Adolescent Health, 57(2), 192–197. https://doi.org/10.1016/j.jadohealth.2015.04.009
Johnson, S. A., Filliter, J. H., & Murphy, R. R. (2009). Discrepancies between self- and parent-perceptions of autistic traits and empathy in high functioning children and adolescents on the autism spectrum. Journal of Autism and Developmental Disorders, 39(12), 1706–1714. https://doi.org/10.1007/s10803-009-0809-1
Joyce, C., Honey, E., Leekam, S. R., Barrett, S. L., & Rodgers, J. (2017). Anxiety, intolerance of uncertainty and restricted and repetitive behaviour: Insights directly from young people with ASD. Journal of Autism and Developmental Disorders, 47(12), 3789–3802. https://doi.org/10.1007/s10803-017-3027-2
Kaat, A. J., Gadow, K. D., & Lecavalier, L. (2013). Psychiatric symptom impairment in children with autism spectrum disorders. Journal of Abnormal Child Psychology, 41(6), 959–969. https://doi.org/10.1007/s10802-013-9739-7
Karalunas, S., Hawkey, L., Gustafsson, E., Miller, H., Langhorst, M., Cordova, M., Fair, M., & Nigg, D. (2018). Overlapping and distinct cognitive impairments in attention-deficit/hyperactivity and autism spectrum disorder without intellectual disability. Journal of Abnormal Child Psychology, 46(8), 1705–1716. https://doi.org/10.1007/s10802-017-0394-2
Kochhar, P., Batty, M. J., Liddle, E. B., Groom, M. J., Scerif, G., Liddle, P. F., & Hollis, C. P. (2011). Autistic spectrum disorder traits in children with attention deficit hyperactivity disorder. Child: Care, Health and Development, 37(1), 103–110. https://doi.org/10.1111/j.1365-2214.2010.01123.x
Krug, D. A., Arick, J., & Almond, P. (1980). Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. Journal of Child Psychology and Psychiatry and Allied Disciplines, 21(3), 221–229. https://doi.org/10.1111/j.1469-7610.1980.tb01797.x
Larsson, H., Dilshad, R., Lichtenstein, P., & Barker, E. D. (2011). Developmental trajectories of DSM-IV symptoms of attention-deficit/hyperactivity disorder: Genetic effects, family risk and associated psychopathology. Journal of Child Psychology and Psychiatry, 52(9), 954–963. https://doi.org/10.1111/j.1469-7610.2011.02379.x
Levy, S. E., Giarelli, E., Lee, L. C., Schieve, L. A., Kirby, R. S., Cunniff, C., Nicholas, J., Raven, J., & Rice, C. E. (2010). Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. Journal of Developmental & Behavioral Pediatrics, 31(4), 267–275. https://doi.org/10.1097/DBP.0b013e3181d5d03b
Lord, C., Rutter, M., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. (2012). Autism diagnostic observation schedule, second edition (ADOS-2) manual (Part 1): Modeules 1–4. Torrance: Western Psychological Services.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. https://doi.org/10.1007/BF02172145
May, T., Sciberras, E., Hiscock, H., & Rinehart, N. (2016). The comorbid diagnosis of ASD and ADHD: Clinical and neuropsychological perspectives. In J. Matson (Eds.) Handbook of assessment and diagnosis of autism spectrum disorder (pp. 259–284). Springer, Cham. https://doi.org/10.1007/978-3-319-27171-2_14
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Möricke, E., Buitelaar, J. K., & Rommelse, N. N. J. (2016). Do we need multiple informants when assessing autistic traits? The degree of report bias on offspring, self, and spouse ratings. Journal of Autism and Developmental Disorders, 46(1), 164–175. https://doi.org/10.1007/s10803-015-2562-y
Mouti, A., Dryer, R., & Kohn, M. (2019). Differentiating autism spectrum disorder from ADHD using the social communication questionnaire. Journal of Attention Disorders, 23(8), 828–837. https://doi.org/10.1177/1087054718781945
Murray, D. S., Ruble, L. A., Willis, H., & Molloy, C. A. (2009). Parent and teacher report of social skills in children with autism spectrum disorders. Language, Speech & Hearing Services in Schools, 40(2), 109–115. https://doi.org/10.1044/0161-1461(2008/07-0089)
Murray, M. J. (2010). Attention-deficit/hyperactivity disorder in the context of autism spectrum disorders. Current Psychiatry Reports, 12(5), 382–388. https://doi.org/10.1007/s11920-010-0145-3
Nakagawa, A., Hayashi, W., Nishio, T., Hanawa, Y., Aoyagi, K., Okajima, Y., & Iwanami, A. (2021). Similarity of subjective symptoms between autism spectrum disorder and attention-deficit/hyperactivity disorder in adults: Preliminary findings. Neuropsychopharmacology Reports, 41(2), 237–241. https://doi.org/10.1002/npr2.12170
Ng, A., Heinrich, K., & Hodges, E. (2021). Associations between ADHD subtype symptomatology and social functioning in children with ADHD, autism spectrum disorder, and comorbid diagnosis: Utility of diagnostic tools in treatment considerations. Journal of Attention Disorders, 25(6), 820–828. https://doi.org/10.1177/1087054719855680
Nijmeijer, J., Hoekstra, S., Minderaa, P., Buitelaar, R., Altink, B., Buschgens, K., Fliers, M., Rommelse, E., Sergeant, C., & Hartman, A. (2009). PDD symptoms in ADHD, an independent familial trait? Journal of Abnormal Child Psychology, 37(3), 443–453. https://doi.org/10.1007/s10802-008-9282-0
Okyar, E., & Gorker, I. (2020). Examining the autistic traits in children and adolescents diagnosed with attention-deficit hyperactivity disorder and their parents. BMC Psychiatry, 20(1), 285–285. https://doi.org/10.1186/s12888-020-02703-z
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews, 10(1), 89. https://doi.org/10.1186/s13643-021-01626-4
Pehlivanidis, A., Papanikolaou, K., Korobili, K., Kalantzi, E., Mantas, V., Pappa, D., & Papageorgiou, C. (2021). Trait-based dimensions discriminating adults with attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and co-occurring ADHD/ASD. Brain Sciences, 11(1), 18. https://doi.org/10.3390/brainsci11010018
Pinto, R., Rijsdijk, F., Ronald, A., Asherson, P., & Kuntsi, J. (2016). The genetic overlap of attention-deficit/hyperactivity disorder and autistic-like traits: an investigation of individual symptom scales and cognitive markers. Journal of Abnormal Child Psychology, 44(2), 335–345. Brain Sciences, 11(1), 18. https://doi.org/10.1007/s10802-015-0037-4
Polderman, T. J. C., Hoekstra, R. A., Posthuma, D., & Larsson, H. (2014). The co-occurrence of autistic and ADHD dimensions in adults: An etiological study in 17 770 twins. Translational Psychiatry, 4(9), e435. https://doi.org/10.1038/tp.2014.84
Posar, A., & Visconti, P. (2019). Long-term outcome of autism spectrum disorder. Turk Pediatri Arsivi, 54(4), 207–212. https://doi.org/10.14744/TurkPediatriArs.2019.16768
Reiersen, A. M., Constantino, J. N., Volk, H. E., & Todd, R. D. (2007). Autistic traits in a population-based ADHD twin sample. Journal of Child Psychology and Psychiatry, 48(5), 464–472. https://doi.org/10.1111/j.1469-7610.2006.01720.x
Ronald, A., Happé, F., & Plomin, R. (2008a). A twin study investigating the genetic and environmental aetiologies of parent, teacher and child ratings of autistic-like traits and their overlap. European Child & Adolescent Psychiatry, 17(8), 473–483. https://doi.org/10.1007/s00787-008-0689-5
Ronald, A., Larsson, H., Anckarsäter, H., & Lichtenstein, P. (2014). Symptoms of autism and ADHD: A Swedish twin study examining their overlap. Journal of Abnormal Psychology, 123(2), 440–451. https://doi.org/10.1037/a0036088
Ronald, A., Simonoff, E., Kuntsi, J., Asherson, P., & Plomin, R. (2008b). Evidence for overlapping genetic influences on autistic and ADHD behaviours in a community twin sample. Journal of Child Psychology and Psychiatry, 49(5), 535–542. https://doi.org/10.1111/j.1469-7610.2007.01857.x
Ros, R., & Graziano, P. A. (2018). Social functioning in children with or at risk for attention deficit/hyperactivity disorder: a meta-analytic review. Journal of Clinical Child and Adolescent Psychology, 47(2), 213–235. https://doi.org/10.1080/15374416.2016.1266644
Rutter, M., Bailey, A., & Lord, C. (2003). The social communication questionnaire: Manual. Western Psychological Services.
Santosh, P., & Mijovic, J. (2004). Social impairment in hyperkinetic disorder. European Child & Adolescent Psychiatry, 13(3), 141–150. https://doi.org/10.1007/s00787-004-0372-4
Schwenck, C., & Freitag, C. M. (2014). Differentiation between attention-deficit/hyperactivity disorder and autism spectrum disorder by the social communication questionnaire. ADHD Attention Deficit and Hyperactivity Disorders, 6(3), 221–229. https://doi.org/10.1007/s12402-014-0147-9
Sciberras, E., Mueller, K. L., Efron, D., Bisset, M., Anderson, V., Schilpzand, E. J., Jongeling, B., & Nicholson, J. M. (2014). Language problems in children with ADHD: A community-based study. Pediatrics, 133(5), 793–800. https://doi.org/10.1542/peds.2013-3355
Scott, F. J., Baron-Cohen, S., Bolton, P., & Brayne, C. (2002). The CAST (Childhood Asperger Syndrome Test) Preliminary development of a UK screen for mainstream primary-school-age children. Autism, 6(1), 9–31. https://doi.org/10.1177/1362361302006001003
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/CHI.0b013e318179964f
Stordeur, C., Boele, A., Peyre, H., Delorme, R., & Acquaviva, E. (2019). Psychometric properties of the French Version of the Social Responsiveness Scale in autism spectrum disorder with or without attention deficit hyperactivity disorder. L’encephale, 45(4), 285–289. https://doi.org/10.1016/j.encep.2018.08.004
Thomas, R., Sanders, S., Doust, J., Beller, E., & Glasziou, P. (2015). Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics, 135(4), e994-1001. https://doi.org/10.1542/peds.2014-3482
Van Der Meer, J. M., Oerlemans, A. M., van Steijn, D. J., Lappenschaar, M. G., de Sonneville, L. M., Buitelaar, J. K., & Rommelse, N. N. (2012). Are autism spectrum disorder and attention-deficit/hyperactivity disorder different manifestations of one overarching disorder? Cognitive and symptom evidence from a clinical and population-based sample. Journal of the American Academy of Child and Adolescent Psychiatry, 51(11), 1160-1172.e3. https://doi.org/10.1016/j.jaac.2012.08.024
Zablotsky, B., Bramlett, M. D., & Blumberg, S. J. (2020). The co-occurrence of autism spectrum disorder in children with ADHD. Journal of Attention Disorders, 24(1), 94–103. https://doi.org/10.1177/1087054717713638
Acknowledgements
We extend our gratitude to the research assistants for their contribution to this manuscript.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhong, Q., Porter, M. Autism Spectrum Disorder Symptoms in Individuals with a Primary Diagnosis of Attention-Deficit/Hyperactivity Disorder: A Systematic Review. Rev J Autism Dev Disord (2024). https://doi.org/10.1007/s40489-024-00443-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40489-024-00443-4