Abstract
Adults with autism spectrum disorder (ASD) have a lower quality of life (QoL) than neurotypical adults and a higher risk of psychiatric comorbidities. We reviewed the effectiveness of mindfulness-based stress reduction (MBSR) in the treatment of adults with ASD. Data were collected from 6 eligible interventional studies (4 adequate quality, 2 weak quality; 245 total participants). The study quality and certainty of findings were assessed using Evaluative Method for Determining Evidence-Based Practices in Autism and GRADE framework. MBSR was effective in all outcomes: ASD symptoms (n = 4, low certainty), QoL (n = 5, low certainty), symptoms of anxiety and depression (n = 4, low and moderate certainty, respectively). MBSR shows promise for improving QoL, reducing ASD symptoms and alleviating psychiatric comorbidities in adults with ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This systematic review focuses exclusively on mindfulness-based stress reduction (MBSR) in autistic adults. There is limited research into MBSR in autism, and we set out to evaluate with rigor all the available evidence for the benefit(s) of this intervention. In specifying such a specific and narrow research question, it is important to be clear how this focus on MBSR differs from the extensive literature on more general mindfulness therapy in autism and other conditions. In this introduction, we explain the distinctiveness of MBSR, explain the benefit of focussing selectively on MBSR as an intervention, and identify the characteristics of autism and the needs that MBSR might address for this population.
Mindfulness-Based Therapies (MBSR vs MBCT)
In 1979, Jon Kabat-Zinn founded the Stress Reduction Clinic (which would become the centre for mindfulness) while working at the University of Massachusetts. At this clinic, he developed and offered an 8-week stress reduction and relaxation program for patients with chronic illness, this course would later be known as mindfulness-based stress reduction (MBSR) (Kabat-Zinn, 1990). After finding success with his early patients, he began working on building scientific evidence for his course. His results showed the promise and effectiveness of mindfulness-based interventions, which has since been replicated and large numbers of studies have found the effectiveness of mindfulness-based interventions in a variety of patient populations.
In 1990 Kabat-Zinn would release his book ‘Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness’ which would allow his techniques to reach an even larger audience. Kabat-Zinn has since defined mindfulness as ‘the awareness that arises through paying attention, on purpose, in the present moment, non-judgementally’. This simple definition describes some of the key concepts of mindfulness practice which underpins the MBSR course Kabat-Zinn created and other mindfulness-based interventions.
MBSR is based on a standard curriculum, it is an 8-week course comprising of weekly sessions with an all-day retreat which is often placed between weeks 6 and 7. The course also includes daily practices which are to be completed between sessions. It is based on certain principles and each session has an intentional aim and theme. There are also defined attitudes and commitment required to see the benefits of the course. The attitudes required are non-judging, patience, beginners mind, trust, non-striving acceptance and letting go. This is combined with the importance of commitment and self-discipline; this acknowledges the time and effort required to complete the course. Commitment requires not only the time commitment, but purposefully and intentionally committing to a mindfulness practice. The advantages of MBSR are a recognised curriculum with supporting evidence of its efficacy and rigorous standards for MBSR facilitator qualifications. A guide to what takes place in each session alongside the themes and objectives of each session is available in the appendix.
MBCT was developed by a group of researchers who had been assigned to create a cognitive-based therapy (CBT) which could reduce relapses in recurrent depression (Segal, 2002). The group had theorised that by combining MBSR with CBT they could create a course which would best achieve this goal. The researchers attended Kabat-Zinn’s Stress reduction clinic and used this experience to help guide the creation of MBCT. Similar to MBSR, this is also an 8-week course with an all-day retreat. The difference between these therapies is that since MBCT was developed as a therapy to prevent recurrent depression, it teaches specific CBT based coping strategies for clinical depression. In the context of autism and the desired benefits outside depression MBSR is more appropriate and this is why we selected to focus on MBSR. The advantages of this therapy are similar to those of MBSR, also using a defined curriculum and having training standards for facilitators.
Dialectical behaviour therapy (DBT) and acceptance and commitment therapy (ACT) are two other forms of mindfulness-based therapy which have shown promise (Hayes et al., 1999; Linehan, 1993). We did not focus on DBT since it is a therapy primarily developed and used to treat borderline personality disorder. Although ACT makes use of mindfulness-based principles it does not use formal mediation as part of its course and incorporates more individual psychotherapy aspects.
Mindfulness Interventions in Autism
Mindfulness-based therapies have shown promise as an effective treatment for reducing the symptoms of anxiety and depression in adult populations with anxiety and depression (Hofmann & Gómez, 2017). When compared to CBT, a more widely used treatment for anxiety, generally both treatments show similar outcomes, with some studies suggesting that different subgroups of people with anxiety respond differently to the treatments (Arch & Ayers, 2013; Arch et al., 2013; Li et al., 2021). Given the impact of anxiety disorders and depressive disorders on the autistic population it is important to determine whether the same benefits can be achieved. In 2016, a review of mindfulness-based interventions in autism found preliminary evidence for the effectiveness of mindfulness-based interventions (Cachia et al., 2016), but the low quality of evidence and large heterogeneity between studies limits the robustness of findings. Only 2 of the studies involved researched adults, with the other 4 studies focused on children, adolescents, and their caregivers. Hartley et al., (2019) conducted a meta-analysis of studies examining the effect of mindfulness-based interventions on quality of life (QoL) in autistic adults, calculating a medium to large effect size in adults. It was noted that the lack of controlled trials studying mindfulness-based therapies in autism mirrors the poor quality of evidence for interventions in autism in general (Hartley et al., 2019). A common issue is the method of delivery for mindfulness-based intervention. MBT-AS is a form of mindfulness-based intervention which modified existing mindfulness courses for autistic adults (Spek et al., 2013). Although the course takes elements from MBCT, the researchers describe omitting the CBT elements. The finalised protocol more closely resembled MBSR. The formal practices match the practices outlined by the MBSR handbook and there is more focus on mindfulness practice and examining stress with less focus on thought patterns and CBT based practices. Other current research also often considers MBT-AS as a modified form of MBSR (Beck et al., 2020; Sizoo & Kuiper, 2017; Pagni et al., 2020). Therefore, for the purposes of this review, MBT-AS will be considered as an MBSR course.
The risk of psychiatric disease impacting on QoL is raised in autism. Estimated to affect approximately 0.76% of adults worldwide (Baxter et al., 2014), autism carries a significantly increased risk of psychiatric diseases including anxiety disorders, depressive disorders, and attention deficit hyperactivity disorder (ADHD) (Croen et al., 2015; Hofvander et al., 2009). Autistic individuals are over two and a half times more likely than the neurotypical population to have a diagnosis of an anxiety disorder and four times more likely to have a diagnosis of a depressive disorder (Nimmo-Smith, et al., 2019, Hudson, et al., 2018). Increased anxiety persists from childhood through to adulthood. Autistic adults face challenges due to the neurotypical basis for society leading to some autistic adults struggling with change management, sensory stimuli and unpleasant situations (White et al., 2009; Gillott & Standen, 2007). This may explain the increased anxiety seen in autism. Anxiety disorders are an important treatment target in autistic adults. The autistic population reports lower QoL than the neurotypical population, although this was largely assessed using tools which were nonspecific to autistic adults (Sáez-Suanes & Álvarez-Couto, 2021). An investigation into the factors affecting QoL found that a psychopathological co-occurence, most commonly anxiety or depression, stood out as one of the key factors affecting QoL in autistic adults (Sáez-Suanes & Álvarez-Couto, 2021). Improving functional independence and QoL have been identified as the primary principles of autism management, therefore treating anxiety and depression has the potential to greatly benefit the autistic population (Shenoy et al., 2017).
Is MBSR Effective as a Treatment for Autistic Adults?
Our review provides a detailed analysis of the current state-of-the-art for evidence of potential benefits of MBSR in autistic adults. We aimed to analyse the strengths and weaknesses of the research in this area, which is at a preliminary stage, and make future research recommendations to discern the promise of this therapy and facilitate its implementation into clinical practice. Our study has a unique focus on MBSR, differentiating it from previous reviews which have considered mindfulness-based interventions in general (Hourston & Atchley, 2017). MBSR was selected based on its clearly defined protocol and training standards for facilitators, which provides consistency in trials and would translate to real world scenarios were MBSR made available to the wider population. Furthermore, MBSR was not developed to target a specific disease, making it more applicable than other mindfulness-based therapies to our range of outcomes. Although Cachia et al., (2016) and Hartley et al., (2019) both found some evidence for the effectiveness of mindfulness-based interventions in autistic children and adults, this review differs by focusing exclusively on MBSR, while including more recent studies on autistic adults which expands the number of included studied by two- and threefold, respectively. MBSR use in autistic adults was discussed in Psychological therapies for adults with autism (2022); however, this is a brief discussion of selected studies, whereas our approach used a systematic approach following a strict protocol with deeper analysis of individual studies. We have undertaken a systematic review to reliably evaluate the available evidence using replicable search terms and providing in depth analysis of included studies. Previous systematic reviews (de Vibe et al., 2017; Khoury, et al., 2015) have shown the effectiveness of MBSR for quality of life, anxiety and depression in a neurotypical population. Given the cognitive differences seen in executive function and information processing in autism (Johnston et al., 2019; Haigh et al., 2018) our review is necessary to show whether these benefits can also be seen in the autistic population. The quality of included studies will be evaluated thoroughly to provide a detailed assessment of (i) the promise of MBSR as a treatment for autistic adults, (ii) the strengths and weaknesses in the current evidence, and (iii) recommendations for the design, nature and reporting of future research to discern the promise of MBSR and facilitate its implementation into clinical practice.
Methods
This review was completed in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting systematic reviews (Page, et al., 2020).
Inclusion/Exclusion Criteria
Study Type
-
Randomised controlled trials were eligible for inclusion
-
Quasi experimental studies were eligible for inclusion
-
Pilot studies were eligible for inclusion
-
Feasibility studies were eligible for inclusion provided they met other inclusion criteria
-
Quantitative studies were eligible for inclusion
-
Qualitative studies were eligible for inclusion
-
Systematic reviews were not eligible for inclusion
-
Meta analyses were not eligible for inclusion
-
Unpublished studies were not eligible for inclusion
All types of interventional studies were eligible for inclusion. This was intentionally broad in order to include as many studies as possible given the low expected number of relevant studies.
Population Studied
-
Participants aged 18 years or older were eligible for inclusion
-
Participants aged less than 18 years old were not eligible for inclusion
-
Participants with a diagnosis of DSM-V ASD were eligible for inclusion
-
Participants with a previous DSM-IV diagnosis now included in ASD (i.e. autistic disorder, Asperger’s syndrome, PDD-NOS) were eligible for inclusion
-
Participants without a diagnosis of autism, Asperger’s syndrome, autistic disorder or PDD-NOS were not eligible for inclusion
-
Studies which did not report the method of diagnosis confirmation were not eligible for inclusion
In order to address the objectives of the review participants must be adults, defined as age 18 years or older. Participants also required a diagnosis of DSM-V autism (Diagnostic and statistical manual of mental disorders: DSM-V, 2013) or a previous diagnosis of a DSM-IV disorder now classified as autism.
Intervention
-
MBSR mindfulness-based intervention was the only intervention eligible
-
MBSR must be a named and described intervention for studies to be eligible
-
MBSR was defined as a minimum of eight weekly in person sessions delivered by a trained facilitator with formally assigned home practices
-
o
Trained facilitators were defined as having a certification as an MBSR instructor or a previously experienced therapist with new MBSR specific training
-
o
-
Studies delivering MBT-AS were eligible for inclusion
-
MBSR must be the only intervention delivered to participant group for which outcomes were measured
-
MBCT, ACT and DBT or any other mindfulness based interventions outside of MBSR were not eligible for inclusion
MBSR duration was given as a minimum in order to include adaptations which provided a course over a longer time period but did not include single-day retreats or home practices. Facilitator training did not require any specific MBSR qualification due to different available training and qualification options but ensures some MBSR specific training was undertaken by instructors. MBT-AS was considered as a form of MBSR due to the final course closely resembling an MBSR course.
Control Group
The use of a control group was not an inclusion criterion for this review but did form part of the study comparison table and quality assessment. A requirement for a control group was not applied due to the low number of eligible anticipated studies.
Outcomes
-
Studies measuring QoL were eligible for inclusion
-
Studies measuring autism-related disability were eligible for inclusion
-
Studies measuring symptoms of co-occurring psychiatric diseases were eligible for inclusion
-
Studies not measuring QoL, autism-related disability or symptoms of co-occurring psychiatric disease as an outcome were not eligible for inclusion
-
Method of outcome measurement was not an inclusion criterion
Although not an inclusion criterion, the primary outcome measures for each outcome is listed below. All outcome measurements related to the objectives of the study were collected regardless of measurement tool. The mean difference between pretreatment score and posttreatment score was the effect measure presented in the results and tables.
-
QoL
-
World Health Organisation Quality of Life brief version (WHOQOL-BREF) - Gold standard includes additional autism specific items (McConachie et al., 2017)
-
Global Mood Score (GMS)
-
-
Depressive disorder symptoms
-
Hospital anxiety and depression Scale – depression (HADS-D)
-
Rumination-reflection questionnaire (RRQ)
-
-
Anxiety
-
Hospital anxiety and depression scale – anxiety (HADS-A)
-
State trait anxiety inventory-II (STAI-II)
-
-
Autism-related disability
-
SRS-A score
-
One study used the WHODAS II as a measure of autism-related disability (Braden et al., 2021). Although this is not an autism specific measurement device, our study considers this an acceptable measure of autism-related disability. This measure has been validated for use as a generic measure for disability in autistic individuals (Park et al., 2019) and provides the additional benefit of a proxy administration option. Combining a self-report and proxy report gives the most comprehensive assessment of current functioning in autistic individuals (Sandercock et al., 2020). One study used the SCL-90-R as a measure for autism-related disability. This is also not autism specific and has not been validated for use in autistic individuals. We decided to accept this as a measurement for autism-related disability since the tool is well supported for measurement of general psychopathology (Derogatis & Savitz, 1999). The subscales assessed by the tool also generally assess features which are seen in autism: interpersonal sensitivity, obsessive thoughts, somatisation, hostility (irritability and anger) and agoraphobia (Derogatis, 1994). While there are some notable exceptions which would not be relevant (psychoticism and paranoia) these subscales were not used by the study. The variety of tools used by different studies, combined with the poor utilisation of autism specific tools which exist is an important limitation which is recognised by the authors and is discussed in this review.
Search Strategy and Search Terms
MEDLINE (via ovid), Embase (via ovid), PsycINFO (via ovid), Scopus, PubMed and Cochranes Central Registry of Controlled Trials were searched from their conception to the current date and updated by rerunning searches weekly throughout the review process. Search strategy was developed based on the principles outlined in the Cochrane Handbook for Systematic Reviews (Higgins et al., 2021). After screening and selecting studies for inclusion, a reference list examination was carried out on included studies to identify additional studies. The last search was carried out on 17/01/2022.
Search terms for autism were deliberately broad (autis* OR ASD OR autistic disorder OR asperger* OR PDD* OR pervasive developmental disorder*) including searches for previously separate disorders now defined as a subtype of autism. Mindfulness terms were also broad (Mindful* OR MBSR) to ensure as many studies as possible were identified. The autism terms were combined with the mindfulness terms and the term adult* to provide the final search results. Searches were limited to studies available in English on all search platforms. The full search terms used for each database are included in the Appendix.
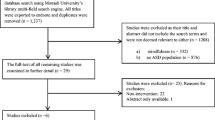
Screening of Identified Studies
Screening was conducted by a single author following the PRISMA guidelines (Page, et al., 2020) and summarised in the PRISMA flowchart (Fig. 1). Studies identified through the search strategy were exported to EndNote™ (Clarivate, Philadelphia, PA 19130, USA), and duplicates were deleted using the automated EndNote feature followed by manual deletion of duplicates missed by this function. Titles and abstracts were screened against inclusion and exclusion criteria, and the reason for exclusion was recorded. The reason for study exclusion was recorded as the first criterion which a study failed to meet from the list below.
-
Study was a review/meta-analysis
-
Study is not autism related
-
Participants studied were caregivers/family and/or u18 year olds
-
Study did not involve an MBSR intervention
-
Undetected duplicates
Following this, the full texts of the remaining studies were retrieved and reassessed against inclusion and exclusion criteria. If a study caused significant uncertainty discussion between authors was used to come to a decision. No studies required discussion between authors.
Following the screening process described in Fig. 1, screening of titles by forward and backwards citation searching was completed for all 6 included studies by a single author, although no additional studies for inclusion were detected through this process. The number of studies screened through forwards and backwards citation searching (including duplicates) is shown in Table 1.
Excluded Studies
Studies excluded after assessment of full text are discussed in line with PRISMA guidelines.
Gaigg et al., (2020) was excluded, despite describing an investigation of the effects of a mindfulness-based therapy in autistic adults, as on closer examination did not meet the inclusion criteria as the method described an ACT therapy. Brewe, et al. (2020) was excluded despite describing a mindfulness-based intervention as it did not use MBSR and its intervention groups did not separate the adults from the adolescents. Conner and White (2017) was removed despite describing an MBCT course with similar changes to MBT-AS; however, this study did not mention removal of cognitive elements and reports the course as a type of MBCT. Jones & Finch, (2020) did meet criteria for intervention, outcomes and control. In the abstract, there was not sufficient detail on the participants for the study to be excluded, but after assessing the full text it was apparent the participants were not required to have autism. Brazeau et al., (2017) was also excluded based on full text assessment, which revealed not all participants had autism, since the abstract did not provide enough information for exclusion.
One potential study identified through this method did not have the full text available in English (Spek et al., 2010).
Data Collection
Data was extracted from included studies by a single author using a data collection template based on Cochranes’s Consumer and Communication Data Extraction Template for Included Studies (Ryan, et al., 2018). The template separates data collection into 7 categories: general review information, methods of the study, risk of bias assessment, participants, interventions and comparisons, outcomes, data and results. Risk of bias assessment was replaced by an autism specific tool. All results for eligible outcomes were collected alongside any effect size (Cohen’s d/Hedges’ g) calculated as part of the study, where the study calculated a p value it was noted whether or not this was significant for a confidence interval of 95%. The effect sizes used in this review were small = 0.2–0.49, medium = 0.5–0.79 and large = 0.8 + to match the boundaries used by the included studies. A blank data collection template and the completed data collection sheets for each study are available in the appendix. Where information was not available in the study, the authors were contacted and information acquired in this way was noted as such.
Quality Assessment
The Evaluative Method for Determining Evidence-Based Practices in Autism was developed for evaluating the quality of studies on the topic of autism (Reichow et al., 2007). The tool provides a guideline for assessment of primary and secondary indicators as well as a framework to combine these results to give an overall research report strength. Assessment of the quality of primary indicators is given as high quality, acceptable quality or unacceptable quality. Secondary indicators are assessed as either evidenced or not evidenced. Research papers were categorised as strong, adequate or weak according to these criteria and this grade was included in the study comparison table. A blank template and the full quality assessment of each study is available in the appendix. Quality assessment was carried out by a single author.
Planned Analysis
Data extracted from all included studies was combined into two separate comparison tables. Table 4 shows the study characteristics including the number of participants, its report strength as determined in the quality assessment, control group, any follow-up period, length of intervention and method of facilitator training. Table 5 shows the outcome measured, measurement tool used, results and the conclusion of included studies. These tables were used to build a narrative synthesis based on the outcomes outlined in the objectives of the study, clinical relevance of results and to make specific recommendations for future research. Mean differences between pre and post intervention groups were calculated as part of the data collection in order to format the data for presentation in Table 5. No other quantitative analysis was completed as part of this review. Due to the low number of studies included, the only criterion for data to be synthesised is that it addressed one of the outcomes described in the objectives. No subgroup, meta regression or sensitivity analyses were carried out as part of this review.
Risk of Bias Across Studies
No formal assessment of publication bias was completed; however, this review acknowledges the risk of publication bias. The risk of publication bias is particularly significant given the rudimentary stage of the research topic and consequent small number of included studies. These factors are known to put systematic reviews at high risk of publication bias (Guyatt et al., 2011). Searching grey literature has been suggested as one way to reduce the impact of publication bias (Paez, 2017). This review did not search sources of grey literature due to the challenges which have been reported previously (Mahood et al., 2013), specifically the lack of available guidance on search strategy and sources, time burden and inability to manage citations due to format of databases. Assessment of selective reporting bias was attempted by comparing the trial protocol outcomes to the results reported. However, only one study registered a protocol, which highlights the importance of protocol registration for future research.
GRADE Assessment
Each outcome was assessed by a single author using the GRADE framework provided in the GRADE handbook recommendations (Schünemann et al., 2013). The GRADE framework is not an objective assessment, GRADE simply provides a transparent presentation of the authors subjective judgements regarding predetermined factors which are combined to give an overall outcome certainty (Schünemann et al., 2013). GRADE assessments consider eight factors: study design, inconsistency of results, indirectness of evidence, imprecision, publication bias, large magnitude of effect, dose–response gradient and effect of plausible residual confounding variables to make an overall assessment of the certainty of evidence (Schünemann et al., 2013). The certainty of outcomes was assessed as either high, moderate, low or very low based on the considerations outlined.
Results
Participant Information
Our combined sample included 245 participants. All studies excluded participants based on intellectual ability. Two studies required an IQ ≥ 85, three studies required an IQ ≥ 70 and one study used clinical impression. Three studies also excluded participants based on verbal intelligence. Only two studies excluded participants based on previous experience with MBSR or mindfulness-based interventions. Only two studies excluded participants who had medication changes during the study. These factors could impact the results and future studies should consider these factors, either including them in exclusion criteria or separating in the analysis. Quality assessment of each individual study is shown in Table 2. Details of diagnosis and intelligence testing is given in Table 3.
Although this review found 6 separate studies which met our criteria, the total number of participants given is larger than the number of independent participants. This is because the recruitment processes significantly overlap, meaning participants have participated in multiple studies. For example, Spek et al., (2013) and Kiep et al., (2014) both recruited individuals from the Adult Autism Centre in Eindhoven. Both studies also describe similar processes and inclusion/exclusion criteria. Kiep et al., (2014) reported that 20 of the participants in their study had previously participated in the study conducted by Spek et al., (2013). This reduces our number of independent participants to 225. Similarly, Pagni et al., (2020) and Braden et al., (2021) both recruited using the Southwest Autism Research and Resource Center. However, these studies did not report the overlap in their samples so the extent of any overlap is unknown.
This reduces the total number of independent participants. The overlap between Kiep et al., (2014) and Spek et al., (2013) means 40% of the sample analysed by Kiep et al., (2014) had already been represented in our review by Spek et al., (2013). This reduces the certainty of our results in outcomes which include these results: autism-related disability (RRQ), depression and anxiety. Despite this, Kiep et al., (2014) provides valuable results for 30 new participants and additional data at a 9-week follow-up for the previously analysed participants. Although there is potential for participant overlap between Pagni et al., (2020) and Braden et al., (2021), the outcomes measured by the two studies were different. This means that although the samples have a potential overlap the impact of this on results should be low.
Fidelity Assessments
Only two studies reported a fidelity assessment of the MBSR intervention used. Only Beck et al., (2020) used the gold standard assessment tool MBI-TAC (Crane & Kuyken, 2019). They assessed 2 randomly selected sessions and used audio recordings of the sessions to allow independent assessment by an expert reviewer. Both sessions assessed were given an overall rating as proficient delivery of sessions. Sizoo & Kuiper, (2017) reported that the majority of participants were not comfortable having sessions recorded and this was why random visits by two senior therapists were used. They reported that each of the eight visits were judged to be in accordance with the protocol but did not give specific details of how this assessment was made. The lack of fidelity assessment in other studies reduces the reliability of the results since it cannot be certain that the exact same intervention is being delivered in each study. To improve the reliability of findings, all future studies should make use of the MBI-TAC framework for assessment regardless of how the assessment is being made.
Outcome Measurements
Autism-related disability was measured using 3 different tools: the social responsiveness scale for adults (SRS-A), self and proxy-related disability assessment scale (DAS) and the Symptom checklist 90 revised (SCL-90-R). Rumination was measured using the rumination reflection questionnaire (RRQ). QoL was measured using 3 different tools: the global mood scale (GMS), the world health organisation quality of life abbreviated assessment (WHOQoL) with/without ASD specific developments and the satisfaction with life score (SWLS). Anxiety was measured using 3 different tools: Hospital anxiety and depression scale for anxiety (HADS-A), the SCL-90-R and the state trait anxiety index (STAI). Depression was measured using 3 different tools: hospital anxiety and depression scale for depression (HADS-D), the SCL-90-R and the beck depression index II (BDI-II).
Synthesis of Results
The early stages of research must be considered when assessing the quality of studies. Although studies ranged between weak and adequate quality this is partially inherent due to the design and nature of pilot/feasibility studies. These studies provide valuable information about the development, challenges and potential of MBSR in autism and have many strengths. The autism specific quality assessment for each study classified 4 studies as adequate quality and 2 studies as weak quality (Table 2). A lack of control group was the reason for the classification of both weak quality studies. Secondary indicators identified that only half of the controlled studies randomised the assignment of participants, reported blinding of the raters to participant group, assessed the fidelity of the intervention and reported long-term maintenance of effects. The characteristics of different studies are collated in Table 4. Considering the early stages of research and level of commitment involved in participation, the participant numbers in the included studies is notable with 4 of the 6 studies including over 40 participants. The variability between studies in terms of control groups and details of the intervention is highlighted. Three different types of comparison groups were used across the 4 studies using a control. The interventions varied in number of sessions, length of sessions and the availability and length of the retreat. There is also wide variation in the outcome measurement tools used in individual studies (Table 5). Future studies may wish to conduct statistical analysis allowing standardised comparisons. Of the 31 measurements reviewed, 24 found statistically significant improvements in either autism-related disability or QoL following MBSR. No measurements showed a deterioration in either autism-related disability or QoL following MBSR. The risk of publication bias and selective reporting bias affecting these results must be noted given the overwhelmingly positive results. The GRADE assessment of finding certainty by outcome shows that autism-related disability, QoL and anxiety had low certainty and depression had moderate certainty (Table 6). In general, the direct comparisons and effect sizes were the upgrading factors. Poor study design, inconsistency in effect sizes and very high risk of publication bias were negative contributing factors to the overall certainty.
Autism-Related Disability
All four studies assessing autism-related disability found a statistically significant improvement in autism-related disability in adults following MBSR intervention.
Autism-related disability scores were assessed in 3 studies, all of which used a different assessment tool; Sizoo & Kuiper, (2017) used the SRS-64, Braden et al., (2021) used the WHODAS and Kiep et al. used the SCL-90-R. A significant decrease in overall autism-related disability was found, regardless of which assessment tool was used, and 2 studies found that the decrease was maintained at follow-up (Kiep et al., 2014; Sizoo & Kuiper, 2017). Like the effect on rumination, Sizoo & Kuiper, (2017) found no significant difference between MBSR- and CBT-treated groups. Kiep et al., (2014) also found significant decreases in 5 of the 6 subdomains assessed by the SCL-90-R, all of which were maintained at 9-week follow-up. Hostility was the only subdomain which did not show a significant decrease following MBSR treatment. Braden et al., (2021) reported a significant decrease in overall score in both self-report and proxy report groups using the WHODAS assessment tool. Both the WHODAS tool and the SRS-A tools have been validated for use within the autistic population (Park et al., 2019; Chan et al., 2017). It is interesting to note that no significant difference was found between CBT and MBSR, however a significant difference was found between MBSR and a support and education control group. This suggests indirectly that both MBSR and CBT provide meaningful benefits beyond those which could be attributed to clinician interaction time or active relaxation, although direct comparison is necessary to test this implication.
Using the GRADE framework, the certainty of findings for autism-related disability was assessed as low. While preliminary findings suggest MBSR may decrease both rumination and autism-related disability, serious study limitations and high risk of publication bias limit the robustness of these findings. The full GRADE assessment is shown in Table 6.
Rumination
Rumination was assessed using the RRQ tool in 3 studies (Kiep et al., 2014; Sizoo & Kuiper, 2017; Spek et al., 2013), all of which found a significant decrease in rumination following MBSR treatment. The study comparing the result with a control group which received CBT (Sizoo & Kuiper, 2017) found no significant difference between these two groups, suggesting both MBSR and CBT may be equally effective. Only 1 study calculated an effect size (d = 0.78) (Spek et al., 2013) and 2 studies found that decreases in rumination were maintained at follow-up (Kiep et al., 2014; Sizoo & Kuiper, 2017).
QoL
Three of the five studies assessing QoL found statistically significant increases in QoL in autistic adults following MBSR intervention.
Three studies used the GMS to measure QoL and found a significant improvement in QoL following MBSR treatment (Kiep et al., 2014; Sizoo & Kuiper, 2017; Spek et al., 2013). Two studies (Kiep et al., 2014; Spek et al., 2013) reported larger mean differences on the GMS-P results than the other (Sizoo & Kuiper, 2017). This may be due to heterogeneity in the interventions; Spek et al., (2013) and Kiep et al., (2014) used 9 weekly 2.5-h sessions whereas Sizoo & Kuiper, (2017) used 13 weekly 1.5-h sessions. The latter was the only study that used both the positive and negative components of this tool, finding significant improvement in QoL on both measures. Like findings for autism-related disability, Sizoo & Kuiper, (2017) found no significant difference between the MBSR group and the CBT group. Only 1 study using the GMS calculated an effect size (d = 0.76) (Spek et al., 2013).
Two studies used the WHOQoL-BREF-ID to assess QoL (Beck et al., 2020; Braden et al., 2021). Only one of these studies (Braden et al., 2021) used the autism validated WHOQoL-BREF-ID items, finding statistically significant increases in only the psychological QoL domain. Unfortunately, the other study using this measure (Beck et al., 2020) did not separate the physical and psychological domains so these cannot be compared. Beck et al., (2020) found statistically insignificant increases in QoL using the WHOQoL-BREF-ID, the SWLS and the WHOQoL-DIS-ID assessments, calculating effect sizes for all 3 tools (WHOQoL-BREF-ID: d = 1.06, WHOQoL-DIS-ID: d = 0.793, SWLS: d = 1.08). However, these effect sizes were calculated using Cohen’s d, despite the sample size < 20 indicating Hedges’ g should be used, which could lead to overestimation of effect size (Turner & Bernard, 2006).
Using the GRADE framework, the certainty of findings for QoL was assessed as low (Table 6). The findings suggest that MBSR may cause improvements in QoL; however, serious limitations in study designs, failure to demonstrate statistical significance in some studies and high risk of publication bias limit the robustness of this conclusion. However, the medium to large effect sizes found in some studies do encourage further research into the use of MBSR therapy in autistic adults to improve QoL.
Anxiety
Three out of four studies assessing anxiety showed statistically significant improvement in anxiety symptoms in autistic adults following MBSR intervention.
Two studies used the SCL-90-R anxiety section as an assessment tool found a significant decrease in symptoms of anxiety (Kiep et al., 2014; Spek et al., 2013); however, only 1 of these calculated an effect size (d = 0.79) (Spek et al., 2013). One study used the HADS-A score to measure symptoms of anxiety and found a significant decrease in symptoms of anxiety (Sizoo & Kuiper, 2017). This study also found no significant difference between MBSR and CBT groups, like findings in autism-related disability and QoL. The fourth study (Pagni et al., 2020) used the STAI tool to measure symptoms of anxiety and showed a decrease in symptoms of anxiety which was not statistically significant. This was the only study assessing anxiety which did not use symptoms of anxiety/depression as a participation inclusion criterion, possibly leading to a lower baseline anxiety in the population studied and explaining why this study was the only study not to find a significant difference (Pagni et al., 2020). Both studies which included follow up found that decreased symptoms of anxiety were maintained (Kiep et al., 2014; Sizoo & Kuiper, 2017).
Using the GRADE framework, the certainty of findings for anxiety symptoms was assessed as low (Table 6). Findings suggest MBSR may decrease anxiety in autistic adults, although variation in study designs, inconsistent findings regarding statistical significance of results and high risk of publication bias limit the robustness of this conclusion.
Depression
All 4 studies assessing depression found a statistically significant decrease in symptoms of depression in autistic adults following MBSR intervention.
Both studies that used the SCL-90-R depression section as an assessment tool and found a significant decrease in symptoms of depression (Kiep et al., 2014; Spek et al., 2013) and only one calculated an effect size (d = 1.25) (Spek et al., 2013). One study used the HADS-D score to measure symptoms of depression and found a significant decrease in symptoms of depression (Sizoo & Kuiper, 2017). As with the changes in rumination, QoL and anxiety, the changes found were not significantly different between CBT and MBSR groups. The fourth study used the BDI-II score to assess symptoms of depression and found a significant decrease in symptoms of depression and measured the effect size (d = 0.68) (Pagni et al., 2020). Both studies that included a follow-up assessment (Kiep et al., 2014; Sizoo & Kuiper, 2017) found that decreased symptoms of depression were maintained.
Using the GRADE framework, the certainty of findings for symptoms of depression was assessed as moderate (Table 6). All studies found that MBSR significantly reduced the symptoms of depression in adults with MBSR, with medium to large effect sizes where measured. Despite limitations in study design, and a high risk of publication bias, these findings warrant further study on the benefits of MBSR for autistic adults that exhibit symptoms of depression.
Harm and Challenges
No included studies reported a direct measurement of harm, adverse events or side effects. This is something which should be considered in future studies. There were 25 participants who began interventions but did not complete the study. Eight of these the reasons for withdrawal were not reported. Four participants were removed due to disruptive behaviour, which could potentially impact removed participants mental health. Three withdrew due to unrelated medical issues. Five participants did not attend the number of classes required by the study. Similarly, one participant withdrew due to disinterest. Two participants withdrew due to scheduling conflicts. Two withdrew due to unspecified adverse life events. Due to the lack of controls in many studies the attrition rates cannot be analysed thoroughly as there is no comparison data. Beck et al., (2020) reported the main challenges when attempting to use traditional (unmodified) MBSR were additional time needed for practical arrangements (such as travel or downloading practices) and sensory overwhelming when attempting everyday activities mindfully.
Discussion
This Review in Context of Previous Research
This review identified and analysed the results of six studies using MBSR in autistic adults. This is the first review to examine the effectiveness of MBSR as a treatment for autistic adults. This review follows the work of Cachia et al., (2016) and Hartley et al., (2019) which reported promising findings for mindfulness-based interventions in children, adults and caregivers. The findings of this review must be interpreted with caution given the low certainty in three of the four outcomes and limited number of studies. Our findings showing improvements in QoL consistent with findings reported previously (Hartley et al., 2019), and expanded on these by looking at effects on autism-related disability, depression and anxiety. Consistent with the findings of Cachia et al., (2016), we found that MBSR reduces anxiety, depression and rumination. Building on these findings, our review presents preliminary findings that MBSR also reduces autism-related disability and improves QoL.
Limitations of Included Evidence
The small number of studies included in this review limits the robustness of findings and the application of findings. Given the broadness of search terms and inclusion/exclusion criteria, this small number of studies reflects the overall lack of research available on this topic. Only 2 studies used an appropriate active control group (Braden et al., 2021; Pagni et al., 2020); 2 studies had no control group (Beck et al., 2020; Kiep et al., 2014); Spek et al., (2013) used a waitlist control group for comparison and Sizoo & Kuiper, (2017) compared MBSR and CBT. This highlights the need for high quality randomised controlled trials and is consistent the GRADE assessment findings, which found low certainty for three of the four outcomes. Waitlist control groups can overestimate effect size due to participants in the waitlist group seeing less improvement than would be expected. This may be explained by waitlist group participants having lowered expectations that they are ‘waiting’ for treatment and therefore will not see improvement until they receive this treatment (Cunningham et al., 2013). This must be factored when considering the results of Spek et al., who used a waitlist control group and found positive results for all primary outcomes. GRADE assessments were all majorly affected by the high risk of publication bias, which will improve as more research is conducted and a more thorough analysis of publication bias can be completed. Only 1 of the 5 studies which assessed QoL used the AS validated WHOQoL-BREF-ID (Braden, et al., 2020) to ensure that the true QoL of participants was represented. All included studies used participants without intellectual disability, which is understandable given the nature of the intervention, limiting the potential application of findings in the wider autistic adult population. Only 2 of the included studies completed a long term follow up, providing limited understanding of the long-term effects of MBSR. Only the study of Braden et al. (2020) measured an outcome through a proxy report to avoid the risk of social desirability bias—which has now been confirmed as a risk even in autistic individuals (Gernsbacher et al., 2019).
Limitations of This Review
The risk of bias within this review was increased given one author completed the analysis, with the second author reviewing work and offering general guidance. One of the most obvious examples of this is the use of one reviewer to complete the quality assessments, unfortunately, this is due to the different time commitments of the researchers and could not be avoided. This risk of bias is recognised by this review and was mitigated by following PRISMA guidelines and strict adherence to the review protocol. Only published studies available in English were eligible for inclusion, introducing risk of publication bias as well as possibly missing studies which were unavailable in English.
Implications of Results
The research on the use of MBSR in autistic adults is in its infancy and due to the small number of included studies, combined with the low certainty of results, there is unlikely to be any practice or policy change in the near future. However, as the research improves and more studies become available, MBSR could become a valuable tool for use in the supportive management of autism.
The finding of Sizoo & Kuiper, (2017) that modified MBSR and modified CBT are equally effective is particularly important. If this can be replicated in future research with a larger sample, the cost-effectiveness and feasibility of applying these modified protocols in practice should be compared. Another finding of note is that modifications to MBSR courses may not be necessary for effects in autistic adults (Beck et al., 2020). If these findings are replicable with an active control group, given the growing and relatively widespread availability of standard MBSR courses, this could have massive implications for the uptake and dissemination of treatment should future evidence support a recommendation of MBSR. A randomised controlled trial comparing modified MBSR protocols to the standard MBSR course with an active control group would ascertain whether this is a viable option.
Given the heterogeneity of the interventions used, research into a dose–effect relationship could be useful for developing an understanding of how mindfulness-based interventions work. For example, a study could investigate the effectiveness of mindfulness interventions given over 9 weekly sessions, with the session length as the independent variable. Another example of this would be a trial which investigated how the number of sessions attended affects the primary outcomes of QoL, depression, anxiety and autism-related disability. It may also be useful to compare MBSR effects to other forms of mindfulness-based interventions such as MBCT, ACT or DBT to determine the optimal form of therapy.
Braden et al., (2021) report that only female participants improved on physical WHOQoL-BREF-ID scores and female participants improved more than male on the mental WHOQoL-BREF-ID. These results suggest trials analysing which subgroups of autistic adults are susceptible to the effects of mindfulness may be useful. IQ, sex and autism symptomatology may be useful subgroups which could be analysed in future studies. Investigating whether the positive effects of MBSR on QoL are also found in patients without clinical depression or anxiety would also be useful in directing real life applications of research. Subgroup analysis could also help compare MBSR and CBT, possibly identifying which subgroups are more susceptible to different treatments.
Outcomes measured in these studies included QoL, autism-related disability and symptoms of anxiety, depression and rumination. Another outcome which could be useful in future is emotional regulation, given the qualitative findings of Beck et al., (2020) which suggested this may be one of the most impactful benefits which participants noticed. Sleep problems are more likely in autism (Morgan, et al., 2020) and MBSR has been shown to have a positive effect on neurotypical adults with sleep problems. Therefore, another outcome which may be interesting to investigate would be sleep quality.
General Recommendations for Future Studies
All studies should have a registered protocol which will minimise reporting bias and improve study design.
Studies focusing on QoL in autism should make use of the AS validated WHOQoL-BREF-ID, which is the only validated autism specific measure of QoL. All studies on MBSR should use the MBI-TAC framework for assessment of fidelity. Studies should also include harm and negative impact assessments as part of their predefined outcomes. Where possible, studies should exclude participants who have medications changed during the study or participants who have previous experience of MBSR. Where this is not possible it may be useful to subgroup these categories.
Conclusions
This review identified six studies which used MBSR in autistic adults and assessed at least one relevant outcome (autism-related disability, QoL, anxiety, depression). All studies found MBSR to be effective in reducing measured symptoms and improving QoL. However, the number of studies included in the review was low, reflecting the small volume of research reported, and as a result the conclusions must be interpreted with caution. The evidence for the effect of MBSR on autism-related disability, AS, QoL and anxiety was assessed as having low certainty, with the effectiveness in reducing depression assessed as having moderate certainty. Recommendations are made to improve the design of future studies in terms of participants, interventions and comparison groups. Research to establish a dose response gradient and replicating studies reporting estimated effects using a non-modified version of MBSR are important next steps towards acceptance and adoption of this therapy.
References
Arch, J., Ayers, C. (2013). Which treatment worked better for whom? Moderators of group cognitive behavioral therapy versus adapted mindfulness based stress reduction for anxiety disorders. Behaviour Research and Therapy [Internet]. 2013 [cited 3 December 2021];51(8):434–442. https://www.sciencedirect.com/science/article/pii/S0005796713000715?via%3Dihub
Arch, J., Ayers, C., Baker, A., Almklov, E., Dean, D., Craske, M. (2013). Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behaviour Research and Therapy [Internet]. 2013 [cited 3 December 2021];51(4–5):185–196. https://www.sciencedirect.com/science/article/pii/S0005796713000144
Baxter, A., Brugha, T., Erskine, H., Scheurer, R., Vos, T., & Scott, J. (2014). The epidemiology and global burden of autism spectrum disorders. Psychological Medicine, 45(3), 601–613.
Beck, K., Greco, C., Terhorst, L., Skidmore, E., Kulzer, J., McCue, M. (2020). Mindfulness-based stress reduction for adults with autism spectrum disorder: Feasibility and estimated effects. Mindfulness [Internet]. 2020;11(5):1286–1297. https://link.springer.com/article/10.1007/s12671-020-01345-2
Braden, B., Pagni, B., Monahan, L., Walsh, M., Dixon, M., Delaney, S. et al. (2021). Quality of life in adults with autism spectrum disorder: influence of age, sex, and a controlled, randomized mindfulness-based stress reduction pilot intervention. Quality of Life Research [Internet]. 2021;. https://link.springer.com/article/10.1007/s11136-021-03013-x#Tab5
Brazeau, K., Rehfeldt, R., Mazo, A., Smalley, S., Krus, S., Henson, L. (2017). On the efficacy of mindfulness, defusion, and behavioral skills training on job interviewing skills in dually-diagnosed adults with developmental disorders. Journal of Contextual Behavioral Science [Internet]. 2017;6(2):145–151. https://www.sciencedirect.com/science/article/pii/S221214471730025X
Brewe, A., Mazefsky, C., White, S. (2020). Therapeutic alliance formation for adolescents and young adults with autism: Relation to treatment outcomes and client characteristics. Journal of Autism and Developmental Disorders [Internet]. 2020;51(5):1446–1457. https://link.springer.com/article/10.1007%2Fs10803-020-04623-z
Cachia, R., Anderson, A., Moore, D. (2016). Mindfulness in individuals with autism spectrum disorder: A systematic review and narrative analysis. Review Journal of Autism and Developmental Disorders [Internet]. 2016;3(2):165–178. https://link.springer.com/article/10.1007%2Fs40489-016-0074-0
Chan, W., Smith, L., Hong, J., Greenberg, J., Mailick, M. (2017). Validating the social responsiveness scale for adults with autism. Autism Research [Internet]. 2017 [cited 3 December 2021];10(10):1663–1671. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5648615/
Cochrane Consumers and Communication La Trobe University; Ryan, Rebecca; Synnot, Anneliese; M, Prictor; Hill, Sophie (2018): Data extraction template. La Trobe. Journal contribution. https://doi.org/10.26181/5b57cfd711743
Conner, C., White, S. (2017). Brief report: Feasibility and preliminary efficacy of individual mindfulness therapy for adults with autism spectrum disorder. Journal of Autism and Developmental Disorders [Internet]. 2017;48(1):290–300. https://link.springer.com/article/10.1007%2Fs10803-017-3312-0
Crane, RS., Kuyken, W. (2019). The mindfulness-based interventions: Teaching assessment criteria (MBI:TAC): Reflections on implementation and development. Current Opinion in Psychology 28:6–10. https://www.sciencedirect.com/science/article/pii/S2352250X18301507
Croen, L., Zerbo, O., Qian, Y., Massolo, M., Rich, S., Sidney, S. et al. (2015). The health status of adults on the autism spectrum. Autism [Internet]. [cited 3 December 2021];19(7):814–823 https://doi.org/10.1177/1362361315577517
Cunningham, JA., Kypri, K., McCambridge, J. (2013). Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Medical Research Methodology 13(1).
Derogatis, L. R. (1994). SCL-90-R: Administration, scoring and procedures manual (3rd ed.). NCS Pearson.
Derogatis, L. R., & Savitz, K. L. (1999). The SCL-90-R, Brief Symptom Inventory, and Matching Clinical Rating Scales. In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment (pp. 679–724). Lawrence Erlbaum Associates Publishers.
de Vibe, M., Bjørndal, A., Fattah, S., Dyrdal, G. M., Halland, E., & Tanner-Smith, E. E. (2017). Mindfulness-Based stress reduction (MBSR) for improving health, quality of life and social functioning in adults: A systematic review and meta-analysis. Campbell Systematic Reviews, 13(1), 1–264. https://doi.org/10.4073/csr.2017.11
Diagnostic and statistical manual of mental disorders: DSM-5. (2013). American Psychiatric Association (5th ed.). Washington, DC.
Gaigg, S., Flaxman, P., McLaven, G., Shah, R., Bowler, D., Meyer, B., et al. (2020). Self-guided mindfulness and cognitive behavioural practices reduce anxiety in autistic adults: A pilot 8-month waitlist-controlled trial of widely available online tools. Autism, 24(4), 867–883. https://doi.org/10.1177/1362361320909184
Gernsbacher. M., Stevenson, J., Dern, S. (2019). Autistic people do enhance their selves. Social Psychological and Personality Science [Internet]. [cited 3 December 2021];11(5):605–615. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7310997/
Gillott, A., Standen, P. (2007). Levels of anxiety and sources of stress in adults with autism. Journal of Intellectual Disabilities [Internet]. [cited 3 December 2021];11(4):359–370. https://journals.sagepub.com/doi/10.1177/1744629507083585
Guyatt, G., Oxman, A., Montori, V., Vist, G., Kunz, R., Brozek, J. et al. (2011). GRADE guidelines: 5. Rating the quality of evidence—publication bias. Journal of Clinical Epidemiology [Internet]. [cited 3 December 2021];64(12):1277–1282. Available from: https://www.jclinepi.com/article/S0895-4356(11)00181-8/fulltext
Haigh, SM., Walsh, JA., Mazefsky, CA., Minshew, NJ., Eack, SM. (2018). Processing speed is impaired in adults with autism spectrum disorder, and relates to social communication abilities. Journal of Autism and Developmental Disorders 48(8):2653–62. https://pubmed.ncbi.nlm.nih.gov/29500756/
Hartley, M., Dorstyn, D., & Due, C. (2019). Mindfulness for children and adults with autism spectrum disorder and their caregivers: A meta-analysis. Journal of Autism and Developmental Disorders [Internet]., 49(10), 4306–4319. https://doi.org/10.1007/s10803-019-04145-3
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. Guilford Press.
Higgins, JPT., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, MJ., Welch, VA (editors). (2021). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. www.training.cochrane.org/handbook
Hofmann, S., Gómez, A. (2017). Mindfulness-based interventions for anxiety and depression. Psychiatric Clinics of North America [Internet]. [cited 3 December 2021];40(4):739–749. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5679245/
Hofvander, B., Delorme, R., Chaste, P., Nydén, A., Wentz, E., Ståhlberg, O et al. (2009). Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry [Internet]. 9(1). https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-9-35
Hourston, S., Atchley, R. (2017). Autism and mind–body therapies: A systematic review. The Journal of Alternative and Complementary Medicine [Internet]. [cited 3 December 2021];23(5):331–339. https://www.liebertpub.com/doi/full/10.1089/acm.2016.0336
Hudson, C. C., Hall, L., & Harkness, K. L. (2018). Prevalence of depressive disorders in individuals with autism spectrum disorder: A meta-analysis. Journal of Abnormal Child Psychology, 47(1), 165–75. https://doi.org/10.1007/s10802-018-0402-1
Johnston, K., Murray, K., Spain, D., Walker, I., Russell, A. (2019). Executive function: Cognition and behaviour in adults with autism spectrum disorders (ASD). Journal of Autism and Developmental Disorders 49(10):4181–92. https://pubmed.ncbi.nlm.nih.gov/31281952/
Jones, S., & Finch, M. (2020). A group intervention incorporating mindfulness-informed techniques and relaxation strategies for individuals with learning disabilities. British Journal of Learning Disabilities [Internet], 48(3), 175–189. https://doi.org/10.1111/bld.12337?saml_referrer
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta.
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528.
Kiep, M., Spek, A. A., & Hoeben, L. (2014). Mindfulness-based therapy in adults with an autism spectrum disorder: Do treatment effects last? Mindfulness, 6(3), 637–44. https://doi.org/10.1007/s12671-014-0299-x
Li, J., Cai, Z., Li, X., Du, R., Shi, Z., Hua, Q. et al. (2021). Mindfulness-based therapy versus cognitive behavioral therapy for people with anxiety symptoms: a systematic review and meta-analysis of random controlled trials. Annals of Palliative Medicine [Internet]. [cited 3 December 2021];0(0):0–0. https://pubmed.ncbi.nlm.nih.gov/34353047/
Linehan, M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford press.
Mahood, Q., Van Eerd, D., Irvin, E. (2013). Searching for grey literature for systematic reviews: Challenges and benefits. Research Synthesis Methods [Internet]. [cited 3 December 2021];5(3):221–234 https://onlinelibrary.wiley.com/doi/full/10.1002/jrsm.1106?saml_referrer
McConachie, H., Mason, D., Parr, J., Garland, D., Wilson, C., Rodgers, J. (2017). Enhancing the validity of a quality of life measure for autistic people. Journal of Autism and Developmental Disorders [Internet]. 48(5):1596–1611. https://link.springer.com/article/10.1007%2Fs10803-017-3402-z
Morgan, B., Nageye, F., Masi, G., Cortese, S. (2020). Sleep in adults with autism spectrum disorder: A systematic review and meta-analysis of subjective and objective studies. Sleep Medicine 65:113–20. https://pubmed.ncbi.nlm.nih.gov/31739229/
Nimmo-Smith, V., Heuvelman, H., Dalman, C., Lundberg, M., Idring, S., Carpenter, P., et al. (2019). Anxiety disorders in adults with autism spectrum disorder: A population-based study. Journal of Autism and Developmental Disorders, 50(1), 308–318. https://doi.org/10.1007/s10803-019-04234-3
Paez, A. (2017). Gray literature: An important resource in systematic reviews. Journal of Evidence-Based Medicine [Internet]. 10(3):233–240. https://pubmed.ncbi.nlm.nih.gov/29266844/
Page, M., Moher, D., Bossuyt, P., Boutron, I., Hoffmann, T., Mulrow, C. et al. PRISMA. (2020). Explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ [Internet]. 2021 [cited 3 December 2021]. https://www.bmj.com/content/372/bmj.n160
Pagni, B., Walsh, M., Foldes, E., Sebren, A., Dixon, M., Guerithault, N. et al. (2020). The neural correlates of mindfulness‐induced depression reduction in adults with autism spectrum disorder: A pilot study. Journal of Neuroscience Research [Internet]. [cited 3 December 2021];98(6):1150–1161. https://onlinelibrary.wiley.com/doi/full/10.1002/jnr.24600?saml_referrer
Park, S., Demetriou, E., Pepper, K., Song, Y., Thomas, E., Hickie, I. et al. (2019). Validation of the 36‐item and 12‐item self‐report World Health Organization Disability Assessment Schedule II (WHODAS‐II) in individuals with autism spectrum disorder. Autism Research [Internet]. [cited 3 December 2021];12(7):1101–1111. https://onlinelibrary.wiley.com/doi/full/10.1002/aur.2115?saml_referrer
Reichow, B., Volkmar, F., & Cicchetti, D. (2007). Development of the evaluative method for evaluating and determining evidence-based practices in autism. Journal of Autism and Developmental Disorders [Internet], 38(7), 1311–1319. https://doi.org/10.1007/s10803-007-0517-7
Sáez-Suanes, G., Álvarez-Couto, M. (2021). Factors associated with quality of life in adults with autism spectrum disorder: A systematic review. Review Journal of Autism and Developmental Disorders [Internet]. https://link.springer.com/article/10.1007/s40489-021-00254-x
Sandercock, R. K., Lamarche, E. M., Klinger, M. R., & Klinger, L. G. (2020). Assessing the convergence of self-report and informant measures for adults with autism spectrum disorder. Autism, 24(8), 2256–68. https://doi.org/10.1177/1362361320942981
Schünemann, H., Brożek, J., Guyatt, G., Oxman, A., editors. (2013). GRADE handbook for grading quality of evidence and strength of recommendations. Updated October. The GRADE Working Group, 2013. Available from https://www.guidelinedevelopment.org/handbook.
Segal, Z. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press.
Shenoy, M., Indla, V., Reddy, H .(2017). Comprehensive management of autism: Current evidence. Indian Journal of Psychological Medicine [Internet]. [cited 3 December 2021];39(6):727–731. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5733418/
Sizoo, B., Kuiper, E .(2017).Cognitive behavioural therapy and mindfulness based stress reduction may be equally effective in reducing anxiety and depression in adults with autism spectrum disorders. Research in Developmental Disabilities [Internet]. [cited 3 December 2021];64:47–55. https://www.sciencedirect.com/science/article/pii/S0891422217300823#bib0210
Spek, A. A., van Ham, N. C., & van Lieshout, H. (2010). Effectiviteit van Effectiviteit van Mindfulness Based Stress Reduction bij volwassenen met een autismespectrumstoornis. Wetenschappelijk Tijdschrift Autisme, 9(3), 82–88.
Spek, A., van Ham, N., Nyklíček, I. (2013). Mindfulness-based therapy in adults with an autism spectrum disorder: A randomized controlled trial. Research in Developmental Disabilities [Internet]. [cited 3 December 2021];34(1):246–253. https://doi.org/10.1016/j.ridd.2012.08.009
Turner, H., Bernard, R. (2006). Calculating and synthesizing effect sizes. contemporary issues in communication science and disorders [Internet]. [cited 3 December 2021];33(Spring):42–55. https://doi.org/10.1044/cicsd_33_S_42
White, S., Oswald, D., Ollendick, T., Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review [Internet]. [cited 3 December 2021];29(3):216–229. https://www.sciencedirect.com/science/article/pii/S027273580900004X?via%3Dihub5
Funding
This review did not receive any direct external funding. The review was completed in partial fulfillment of the MBBS programme by one author, which is funded by the Student Awards Agency for Scotland (SAAS). SAAS was not involved in the review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
One of our authors is trained to deliver mindfulness-based interventions and teaches a mindfulness course at the University of Aberdeen. This potential conflict was mitigated by strict adherence to PRISMA guidelines, and the protocol registered for this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Forbes, Z.N.M., Miller, K. Mindfulness-Based Stress Reduction in the Treatment of Adults with Autism Spectrum Disorder: a Systematic Review of Interventional Studies. Rev J Autism Dev Disord (2023). https://doi.org/10.1007/s40489-023-00398-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40489-023-00398-y