Abstract
Introduction
Patients with cancer often want to spend their final days at home. In Norway, most patients with cancer die in institutions. We hypothesized that full integration of oncology and palliative care services would result in more time spent at home during end-of-life.
Methods
A prospective non-randomized intervention trial was conducted in two rural regions of Mid-Norway. The hospitals’ oncology and palliative care outpatient clinics and surrounding communities participated. An intervention including information, education, and a standardized care pathway was developed and implemented. Adult non-curative patients with cancer were eligible. Proportion of last 90 days of life spent at home was the primary outcome.
Results
We included 129 patients in the intervention group (I) and 76 patients in the comparison group (C), of whom 82% of patients in I and 78% of patients in C died during follow-up. The mean proportion of last 90 days of life spent at home was 0.62 in I and 0.72 in C (p = 0.044), with 23% and 36% (p = 0.073), respectively, dying at home. A higher proportion died at home in both groups compared to pre-study level (12%). During the observation period the comparison region developed and implemented an alternative intervention to the study intervention, with the former more focused on end-of-life care.
Conclusion
A higher proportion of patients with cancer died at home in both groups compared to pre-study level. Patients with cancer in I did not spend more time at home during end-of-life compared to those in C. The study intervention focused on the whole disease trajectory, while the alternative intervention was more directed towards end-of-life care. “Simpler” and more focused interventions on end-of-life care may be relevant for future studies on integration of palliative care into oncology.
Trial Registration
ClinicalTrials.gov Identifier: NCT02170168.
Plain Language Summary
Palliative care is an important part of cancer care to improve patients’ quality of life. To be cared for and die in the preferred place are quality markers in palliative care. Patients with cancer often want to spend their final days at home. In Norway, most patients with cancer die in institutions. We hypothesized that full integration of cancer and palliative care would result in more time spent at home during end-of-life. An intervention that included information, education, and a standardized care pathway was developed and implemented in a region of Mid-Norway (the intervention region, I). A similar region served as comparison region (C). Adult patients with cancer treated with non-curative intent were eligible. Altogether, 129 patients in I and 76 patients in C were included in the study, of whom 82% in I and 78% in C died during follow-up. The mean proportion of time spent at home last 90 days of life was 0.62 in I and 0.72 in C (p = 0.044), and 22.6% and 35.6% (p = 0.073) died at home, respectively. A higher proportion died at home in both groups compared to pre-study national levels (12%). During the study period, C developed and implemented an alternative intervention to the study intervention, with the former placing more focus on end-of-life care compared to the she study intervention that focused on the whole disease trajectory. This may explain why the intervention did not result in more time spent at home during end-of-life as compared to C. “Simpler” interventions directed towards the study’s primary outcome may be relevant for future studies on integration of palliative care into oncology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with cancer often want to spend their final days at home. |
Integration of oncology and palliative care services early in the disease trajectory may contribute to more time at home at the end-of-life. |
What was learned from the study? |
Compared to the control group, the study intervention did not result in patients with cancer spending more time at home at the end-of-life. |
The study intervention was complex and not solely focused on end-of-life care. |
Future studies on integration of oncology and palliative care services should have “simpler” and more focused interventions on end-of-life care. |
Introduction
Modern palliative care (PC) is an important part of oncology, and early introduction is recommended in conjunction with anticancer therapy [1,2,3]. PC can be delivered in a variety of settings, including inpatient units, outpatient clinics, nursing homes, and the home (home-based care) [4, 5]. The increasing incidence and prevalence of cancer warrant rethinking the care delivery models [3]. In scattered populated areas, decentralized PC services are useful [6].
PC interventions are often complex [7, 8]. The use of scientifically recommended methods, such as randomized controlled trials (RCTs) to study their effects may be difficult due to poor recruitment, high attrition rates, bias, confounding, and small sample sizes [7]. However, well-founded study objectives evaluated by sound and time-responsive outcome measures are recommended [7]. Time spent at home is recognized as a valid outcome to assess the quality of end-of-life (EOL) care and is in line with patients’ preferences [9,10,11]. In Norway, the majority of patients with cancer die in institutions, and this represents a pattern strengthened over the past decades [12]. Compared to other European countries, Norway is at bottom of the list of patients with cancer dying at home [13]. Prior to the Covid-19 pandemic, only 10–12% of patients with cancer died at home in Norway [14]; this had increased to 16% in 2021. Being able to spend the last phase of life at home and die at home if preferred depends on several factors, such as family support and easy access to healthcare services [15, 16].
Implementing PC interventions into existing healthcare structures is challenging [17, 18]. Albeit the benefits of early integration of PC in oncology having been known for more than a decade, precise knowledge on which ‘active components’ in PC improve outcomes is still lacking [8]. Published research mainly addresses physical, psychological, social, and EOL care aspects [1, 2, 19,20,21,22], but few studies have addressed the coordination of care.
In previously publications, we described the development and implementation of a regional oncology and PC program [17, 23]. The program consisted of a complex intervention and represented full integration of oncology and PC throughout the entire disease trajectory, including improved care coordination within and between services at different levels of healthcare [23]. The development of the program was based on results from earlier studies in the areas of oncology and PC care and focused on increasing time spent at home at the EOL for patients with cancer [2, 17, 23,24,25]. From this studies, we concluded that development of the program was feasible, and healthcare providers reported that it improved cancer care. However, the program was only used to a limited extent in clinical practice. To evaluate its effectiveness on clinical outcomes, we conducted a prospective controlled non-randomized intervention trial in two health regions in Mid-Norway. This paper presents the clinical outcomes of this intervention trial. We hypothesized that the measurable effects of the complex intervention would increase during the project period, and that a major part of this change would be caused by the complex intervention and not only by general work to improve healthcare services. Time spent at home during the last 90 days of life was chosen as primary clinical outcome.
Methods
Design and Participants
This prospective controlled non-randomized intervention trial was conducted in two regions of Mid-Norway, the Orkdal Region [23] and the Romsdal Region. Two hospitals in these regions, Orkdal Hospital and Molde Hospital, respectively, coordinated the trial. Characteristics of the two regions are given in Table 1.
Patients in the intervention group (I) resided in 13 municipalities neighboring Orkdal Hospital. Patients in the comparison group (C) were recruited from Molde Hospital and nine adjacent municipalities.
Inclusion and Exclusion
Eligibility criteria were: advanced loco-regional and/or metastatic cancer; adult residents (> 18 years of age) of the participating municipalities; and capability to comply with study procedures and read and write Norwegian. Patients receiving anticancer therapy with a curative intent were excluded.
The Intervention Group
A complex intervention focusing on introducing PC along the entire disease trajectory was introduced in the intervention group. The intervention was based on previous studies and complied with national standards for palliative cancer care [24,25,26,27,28,29]. The activities and strategies included in the intervention are summarized in Table 2, and details on implementation have been described elsewhere [17, 23]. The main components were:
-
1.
A standardized care pathway (SCP) with integrated and coordinated oncology and PC services throughout the disease trajectory and across healthcare levels.
-
2.
An educational program intended to improve healthcare professionals’ (HCPs’) knowledge and skills in oncology and PC.
-
3.
An information program on oncology and PC aimed at the public, patients, and carers.
The intervention hospital had an outpatient clinic providing integrated oncology and PC services at all stages of the disease, delivered by one team of HCPs consisting of an oncologist and oncology nurse, a physiotherapist, an occupational therapist, a chaplain, a dietitian, and a social worker [23]. The patients were thus not referred to PC when needed. Due to the lack of oncologists with formal training in palliative medicine in Norway, medical residents in oncology trained in palliative medicine in cancer during their oncology fellowship provided care and advice [23]. Home care nurses, nurses at nursing homes, and general practitioners (GPs) in the communities could contact the intervention hospital around the clock, where they had access to nurses and physicians trained in oncology and PC at the outpatient clinic Monday to Friday between 08 a.m. and 16 p.m [23]. Out of hours, the internal medicine department at Orkdal Hospital or Cancer Clinic at Trondheim University Hospital could be contacted.
The Comparison Group
The comparison hospital had a cancer outpatient clinic and a PC team of whom 50% were physicians with formal training in palliative medicine (Table 1). Patients were referred to the PC team based on needs and symptom burden. The primary focus of the team was providing PC and included home visits upon request and providing support for the patients and their families. Nurses from the communities and the local hospital collaborated on education in a PC network at least once a year. PC physicians collaborated with GPs through visits to the GP offices, visits with the GP to patients at home or in nursing homes, and through bi-annual PC training courses. In addition, home care nurses, nursing home nurses, and GPs could contact a hospital PC physician around the clock. A project focusing on structured advance care planning (ACP) and a palliative plan in primary healthcare to all individuals with life-limiting illnesses, such as incurable cancer, was launched in the comparison region in 2015, and systematically implemented from January to June 2018 (Table 3) [30].
Data Collection and Assessments
Data were managed by 29 community nurses and The Trial Office, Trondheim University Hospital. Paper-based forms were used. At inclusion, information on patient demographics, cancer diagnosis, disease stage and location of metastases, present anticancer treatment, medications, place of care, and performance status were registered. Updates on the patients’ general condition, use of hospital services and admissions, and use of community healthcare services (days in rehabilitation and nursing homes included) were collected every 4 weeks. Date and place of death were recorded.
Patients received questionnaires at inclusion every 4 weeks for 2 years or until death. Patients included in the study for > 2 years received questionnaires every 6 months after 2 years to avoid loss of motivation to participate. Data on symptom intensity and quality of life (QoL) were collected using the European Association for Palliative Care (EAPC) basic dataset [31] and European Organization for Research and Treatment of Cancer “Quality of Life Questionnaire Core 15 palliative” (EORTC QLQ C15-PAL) [32]. Furthermore, every 12 weeks the patients stated preferred places of terminal care and death. These questions formulated were introduced by: “We know from experience that you might change your mind over time. We would like to get your opinion about the next questions again, independently of what you have answered earlier.” (1) “Many persons, sick and healthy, think of where they, once in time, prefer to die. When time comes, and you yourself could chose, where would you prefer to die?” (2) “If you could choose where to be cared for at the end of life, where would you prefer to receive treatment and care?” Response categories were “Home”, “Nursing home”, “Hospital,” or “Others.” The last recorded response was used for analysis.
Pre-study data on cancer deaths and place of death were obtained from the Norwegian Cause of Death Registry. The Norwegian Cancer Registry provided data on cancer incidence and prevalence (Table 1).
Outcomes
The primary outcome was the proportion of the final 90 days of life spent at home. The secondary outcome was the number of home deaths. Death at preferred place and patients’ health-related QoL as measured by EORTC QLQ C15-PAL served as exploratory outcomes [32].
Data Analyses and Statistics
We calculated that 250 deaths would allow a power of 90% for the detection of at least a 20% difference in the mean proportions of time spent at home during the final 90 days of life between I and C, provided a C proportion of 45% and with a two-sided significance level of 5%.
The proportion of the final 90 days of life spent at home was calculated by subtracting the number of days spent in hospital, nursing homes, or rehabilitation institutions from the number of days at home. Residency in sheltered municipal housing was defined as “home,” while residency in a nursing home was not. Day of discharge was counted as inpatient-day and day of admission was not. For patients who died prior to 90 days after inclusion, the proportion of remaining lifespan spent at home was used. Home death was analyzed as dying at home compared to dying elsewhere. The global QoL item of the EORTC QLQ-C15-PAL was used for analysis of QoL at inclusion and before death.
Descriptive statistics were used to analyze population characteristics and calculate death at preferred place. Pearson’s Chi-square test was used for group comparisons, and the Welch t-test was used in case of unequal variances. The proportion of the final 90 days of life spent at home was approximately normally distributed. A two-sided independent t-test was used to compare means of proportions. Logistic regression was used to estimate odds ratio (OR) for dying at home in the compared groups. To compare deaths at preferred place between the two groups, Pearson’s Chi-square test was used. The global QoL item of EORTC QLQ-C15-PAL was scored from 1 (“very poor”) to 7 (“excellent”), and the result was calculated following the procedures of the EORTC QLQ-C15-PAL Scoring Manual: Score = ([Raw score − 1]/6) × 100 [33].
Kaplan–Meier estimates were used to calculate time from inclusion to end of follow-up or death, and to calculate time from last reported preferred place of terminal care and preferred place of death to death. Linear and logistic regression models were used to explore possible influences by demographic and clinical differences on the proportion of the final 90 days spent at home and home deaths, respectively. For both models, a univariate analysis with “region” as the independent variable was performed as the first step; this was followed by multivariate analyses that were performed to adjust for variables differing between the two compared groups.
P values ≤ 0.05 were considered to be statistically significant.
For all analyses, Stata Statistical Software Release 16.0 and 17.0 (StataCorp LP, College Station, TX, USA) were applied.
Ethics and Consent
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Regional Committee for Medical Research Ethics Central Norway, REK Central (2014/212). Written informed consent was obtained from all participants included in the study. In cases where the participant was competent to give oral informed consent but not able to write, an adult family member or HCP signed a proxy consent.
Results
Protocol Deviations
Patients were entered in the study from November 2014 to December 2017; the follow-up period ended December 2019 (Table 3). Due to the inclusion rates and survival rates being different from assumed, the preplanned inclusion and follow-up periods were prolonged by 1 and 2 years, respectively. The study was closed before reaching the planned 250 analyzable deaths and, in addition, the C proportion was smaller (36%) than assumed in the study power calculations.
Patient Characteristics
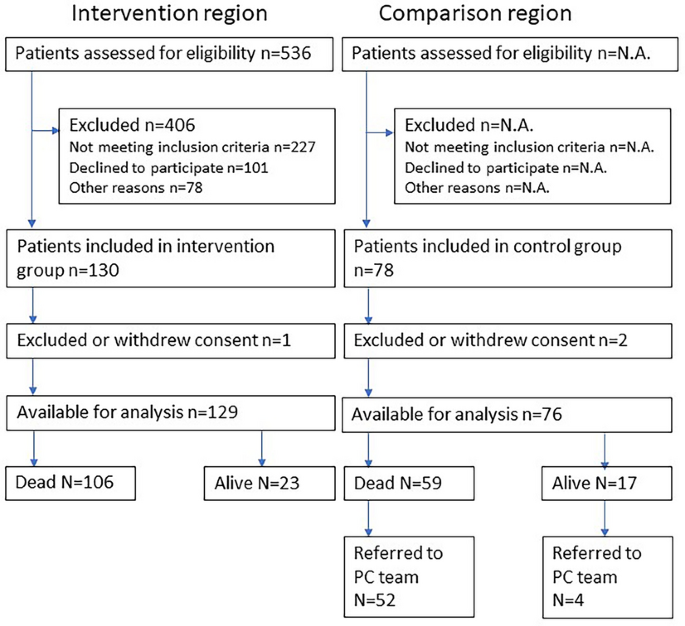
Eligible patients were recruited from the outpatient clinics, with 130 patients included in I and 78 patients included in C (Fig. 1). One patient in each group withdrew consent and one patient in the comparison group did not fulfill inclusion criteria.
Patient characteristics at inclusion are given in Table 4. Mean age was 70.7 (range 38–92) years in I and 68.1 (range 47–84) years in C. In I and C, 57% and 82% of patients, respectively, had a Karnofsky Performance Status (KPS) of at least 90% [34]. Compared to patients in C, fewer patients in I received medical anticancer therapy at inclusion, and they also lived farther away from the hospital.
Median time from inclusion to end of follow-up or death was 425 (95% CI 272–557) days in I and 403 (95% CI 268–635) days in C. In C, 56 patients (74%) were referred to the PC team. By the end of the study period, 106 (82%) patients in I and 59 (78%) patients in C died (Fig. 1); of these, 16 in I and nine in C died before reaching 90 days of observation.
Primary Outcome
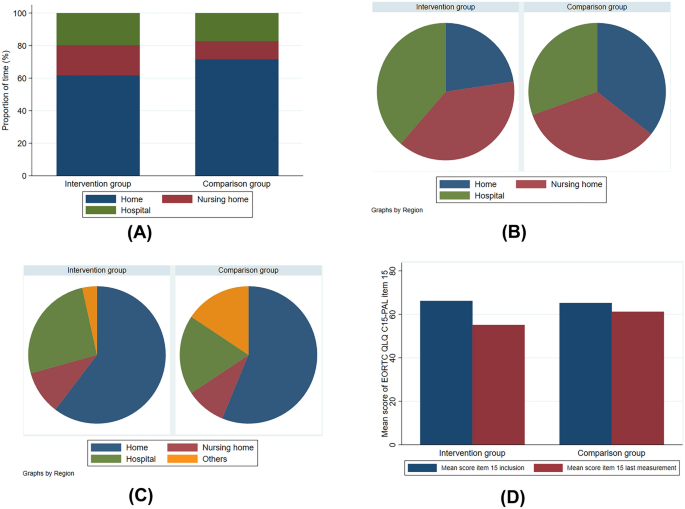
Patients who died before study closure were analyzed for the primary outcome. The mean number of days of inclusion was 81 (range 1–90) in I and 85 (range 20–90) in C. The mean proportion of time spent at home during the last 90 days of life was 0.62 (95% CI 0.56–0.68) in I and 0.72 (95% CI 0.64–0.80) in C (Fig. 2a; Electronic Supplementary Material [ESM] Table S1), with a statistical difference of 0.10 (95% CI 0.00–0.20, p = 0.044) in favor of C. When adjusting for education level, performance score, symptom score (< 4 or ≥ 4), anticancer therapy (yes/no), and distance from home to hospital, the difference was 0.15 (95% CI 0.03–0.27, p = 0.018) in favor of C.
Primary, secondary, and exploratory outcomes. a Mean proportion of time spent in different care settings during the last 90 days of life. b Actual place of death. c Preferred place of death. d Mean score of EORTC QLQ C15-PAL item 15 at inclusion and last measurement before death. EORTC QLQ C15-PAL European Organization for Research and Treatment of Cancer “Quality of Life Questionnaire Core 15 palliative”
Secondary and Exploratory Outcomes
Twenty-four (22.6%) and 21 (35.6%) patients died at home in I and C, respectively (Fig. 2b; ESM Table S2; p = 0.73). Univariate logistic regression analysis showed an OR of 1.9 (95% CI 0.94–3.8; p = 0.075) in favor of dying at home in C. When adjusting for education level, performance score, symptom score (< 4 or ≥ 4), anticancer therapy (yes/no), and distance from home to hospital, the OR was 2.6 (95% CI 0.97–6.7, p = 0.059) in favor of C. Forty-one (38.7%) patients in I and 18 (30.5%) patients in C died in hospital; the corresponding numbers for deaths in nursing homes were 41 (38.7%) and 20 (34.0%), respectively (Fig. 2b; ESM Table S2).
Of the patients who had died, 90 patients (response rate = 85%) in I and 45 patients (response rate = 76%) in C had stated a preferred place of death. In both groups, approximately one third of the responses were collected fewer than 90 days prior to death. In their response to the question on preferred place of death, 57 (63.3%) patients in I and 25 (55.6%) patients in C preferred home death (Fig. 2c; ESM Table S3), while 55 (64.7%) and 32 (69.6%) patients in I and C, respectively, preferred terminal home care. Thirty-four (37.8%) patients in I and 14 (31.1%) patients in C died at the preferred place (Pearson χ2 p = 0.45).
QoL, as scored by EORTC QLQ C15-PAL item 15, revealed no mean group differences at inclusion: 66.2 (n = 99, 95% CI 61.3–71.0) in I versus 65.2 (n = 46, 95% CI 58.0–72.4) in C (p = 0.82) (Fig. 2d). Comparison of the mean decline in scores from inclusion to last measurement revealed a significant difference in favor of C: − 18.3 (n = 73, 95% CI − 24.5 to − 12.1) in I versus − 7.2 (n = 44, 95% CI − 16.3 to 1.9) in C (p = 0.04) (Fig. 2d).
Discussion
Statement of Principal Findings
In both groups, the proportion of home deaths among patients with cancer increased from the pre-study period of 12% to 22.6% (I) and 35.6% (C). It also increased more than in the general population of Norway during the same period (12% in 2019) [14].
We assumed that C represented the general situation for PC in Norway. However, during the study period, an intervention directed towards EOL care was initiated in C [30]. Consequently, the study consisted of two different interventions, both of which were having a positive effect on the proportion of home deaths in both groups, as compared to pre-study levels. Patients in C spent more time at home compared to patients receiving the intervention measures in I during the final 90 days of life. Hence, measurable effects of the complex intervention did not increase during the project period as we hypothesized. The difference between the groups in proportion of home deaths did not reach statistical significance. There were no group differences in deaths at preferred place. The decline in QoL during the study period for the patients who died was larger in I.
Appraisal of Methods
We chose a study design consisting of an intervention group and a control group. The rationale for a control group was to better be able to measure a potential intervention effect. An RCT or a cluster-randomized trial was not feasible due to small-scale conditions and the system-level nature of the intervention. Given the complex nature of the intervention, a study design with baseline observations before implementation of the complex intervention may also be an appropriate design.
Since the effect of the intervention in C was larger than anticipated, we compared the content of the interventions related specifically towards EOL care. The interventions in both groups included those that focused on EOL care and, in particular, home care. The actual study intervention had a broader aim and included the entire disease trajectory. Patients were exposed to the intervention for a mean of 14 months prior to death. In C, the applied intervention was more directed towards EOL, with ACP introduced in primary care to the patients at a mean of 114 days prior to death [30]. The comparison region (C) had a PC specialist who worked 50%, and the nurses and GPs had special training in PC. Consequently, an unintended intervention with focus on EOL was implemented in the comparison region during the study period. The intervention region lacked a physician with formal competence in PC, which may also had a negative influence on the results.
Patients with advanced cancer were recruited regardless of life expectancy and PC needs. A median follow-up of > 1 year is unusual in PC trials [35]. The long follow-up in the present study was in line with our aim to provide the patients with the intervention over a substantial period before they reached the final phase of their life. One may argue whether study endpoints focusing on the entire disease trajectory, such as regular measurement of symptom burden, quality of life, and satisfaction with care, would have been more appropriate in this case than study endpoints directed towards EOL, and whether the study design at all allowed for assumptions on causality [36, 37].
Previously published results revealed that the SCP was used to a limited extent [17]. Hence, insufficient implementation of the intervention and lack of adherence may also have affected the results. Potential effects of the intervention were measured as early as at the initiation of the implementation process, possibly before effects were evident. Furthermore, no pilot study on intervention acceptance and uptake in clinical practice was conducted.
The study was conducted with protocol deviations. The preplanned inclusion and follow-up periods were prolonged, and the study was closed before reaching the number of patients and group proportions used for power calculations [38]. Temporal trends are likely to occur and be evident in a long study period [39]. In our case, implementation of the intervention in the comparison region started before the end of the follow-up period of our study [30].
Comparison with Previous Work and Possible Reasons Why the Intervention Failed
Implementing complex interventions with the intentions to alter HCPs’ behavior is difficult [18, 39, 40]. A cluster-randomized trial in Mid-Norway evaluating a care pathway for home-dwelling elderly after hospital discharge was inconclusive due to incomplete use of the intervention [41]. The authors of that study suggested that intervention adherence should be ensured before study start. Another Norwegian cluster-randomized trial investigating the effect of PC on the use of anticancer treatment at the EOL found no differences between the groups [42]. As in our study, the intervention did not have the desired effect, probably due to the HCPs having a too low fidelity to the intervention to change clinical practice [42]. The reasons for insufficient implementation in our study are heterogenous and may include factors such as differences in hospital and primary care cultures, lack of management anchoring, different information and communications technology systems, and preconceptions about PC referrals [17, 18, 43, 44]. Implementation of the intervention stretched over a 5-year period, and change in key staff during this period may have contributed negatively to the follow-up of adherence to the SCP [17]. Data from the comparison region showed that 50% of patients with advanced cancer got an ACP in primary care between 2018 and 2020 [30]. The intervention in the Romsdal Region was simpler, had a stronger focus on EOL care, and involved HCPs who had devoted their time and focus on EOL care.
A study comparing hospital expenditures for dying patients with cancer demonstrated that Norway is at the top of the list in terms of per capita hospital days during the last 180 days of life [45]. Currently there is a national political effort to better facilitate EOL home care and home death [46]. In 2010, 44% of all cancer deaths in Norway occurred in hospitals; by 2019 this proportion had decreased to 33% [14]. During the same period, the proportion of cancer deaths at home was stable (11% vs. 12%) [14]. In our study, we found that more than half of the patients preferred home death, which is not in line with what happens in “real life.”
Implications for Further Work
Our intervention was complex and insufficiently implemented [17]. In the comparison group (C), the ACP project in primary healthcare probably had a higher uptake than the more comprehensive SCP in I [30]. The ACP intervention was highly anchored and represented a ‘simpler’ intervention than the SCP, with the former more focused on the clinical endpoints chosen for this study. One may reflect whether an SCP containing fewer ‘active PC components’ would be less challenging to implement, and whether it represents possible strategy for the future efforts to study integration of PC into “main stream” oncology. Still, the dilemma remains: Which are the most important components of early integrated PC, and how do we develop interventions simple enough for practicality and complex enough for effect [47]?
In the current study, most of the patients in both groups were cared for close to their homes and died in their municipalities [15]. Care and death where preferred are regarded as important healthcare quality measures [46]. Most of the included patients preferred to be cared for and die at home. However, a substantial fraction preferred to be cared for and die in nursing homes or hospitals. Identifying these patients is important both from research and healthcare planning perspectives.
Conclusion
Patients in the intervention group (I) did not spend more of their final 90 days of life at home than patients in the comparison group (C). The situation in C differs from the general situation in Norway in general. The study intervention focused on the whole disease trajectory, while an alternative intervention in C was more directed towards EOL care. “Simpler” interventions may be relevant for future studies of integration of PC into oncology.
Data Availability
The data analysed during the current study are available from the corresponding author on reasonable request.
References
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014;383(9930):1721–30.
Kaasa S, Loge JH, Aapro M, et al. Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol. 2018;19(11):e588–653.
Rocque GB, Cleary JF. Palliative care reduces morbidity and mortality in cancer. Nat Rev Clin Oncol. 2013;10(2):80–9.
World Health Organization. Palliative care. Key facts 2018. https://www.who.int/news-room/fact-sheets/detail/palliative-care. Accessed 24 Oct 2019.
Official Norwegian Report. NOU 2017:16 På liv og død-Palliasjon til alvorlig syke og døende (In Norwegian). Oslo: Departementenes sikkerhets-og serviceorganisasjon; 2017.
Higginson IJ, Evans CJ, Grande G, et al. Evaluating complex interventions in end of life care: the MORECare statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Med. 2013;11:111.
Fulton JJ, LeBlanc TW, Cutson TM, et al. Integrated outpatient palliative care for patients with advanced cancer: A systematic review and meta-analysis. Palliat Med. 2019;33(2):123–34.
Groff AC, Colla CH, Lee TH. Days spent at home—a patient-centered goal and outcome. N Engl J Med. 2016;375(17):1610–2.
Andersen SK, Croxford R, Earle CC, Singh S, Cheung MC. Days at home in the last 6 months of life: a patient-determined quality indicator for cancer care. J Oncol Pract. 2019;15(4):e308–15.
Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000;3(3):287–300.
Kalseth J, Theisen OM. Trends in place of death: The role of demographic and epidemiological shifts in end-of-life care policy. Palliat Med. 2017;31(10):964–74.
Cohen J, Houttekier D, Onwuteaka-Philipsen B, et al. Which patients with cancer die at home? A study of six European countries using death certificate data. J Clin Oncol. 2010;28(13):2267–73.
Norwegian Institute of Public Health. Norwegian Cause of Death Registry [Web page]. Oslo: Norwegian Institute of Public Health; 2022 [updated 09 June 2022 June 09]. https://statistikkbank.fhi.no/dar/index.jsp?headers=DODSSTED&stubs=EU_SHORT_CODE&measure=common&virtualslice=Freq_value&layers=DAAR&layers=virtual&study=http%3A%2F%2F10.0.3.47%3A80%2Fobj%2FfStudy%2Fd3b.eu-shortlist.dodssted&DAARsubset=2020&DAARslice=2020&mode=cube&DODSSTEDslice=Total&virtualsubset=Freq_value&v=2&EU_SHORT_CODEslice=Total&DODSSTEDsubset=Total%2C1+-+9&measuretype=4&cube=http%3A%2F%2F10.0.3.47%3A80%2Fobj%2FfCube%2Fd3b.eu-shortlist.dodssted_C1&EU_SHORT_CODEsubset=Total%2C02_1&top=yes. Accessed 06 Feb 2023.
Barlund AS, Andre B, Sand K, Brenne AT. A qualitative study of bereaved family caregivers: feeling of security, facilitators and barriers for rural home care and death for persons with advanced cancer. BMC Palliat Care. 2021;20(1):7.
Nysaeter TM, Olsson C, Sandsdalen T, Wilde-Larsson B, Hov R, Larsson M. Preferences for home care to enable home death among adult patients with cancer in late palliative phase—a grounded theory study. BMC Palliat Care. 2022;21(1):49.
Brenne AT, Lohre ET, Knudsen AK, et al. Implementing a standardized care pathway integrating oncology, palliative care and community care in a rural region of mid-Norway. Oncol Ther. 2021;9(2):671–93.
Hjermstad MJ, Hamfjord J, Aass N, et al. Using process indicators to monitor documentation of patient-centred variables in an integrated oncology and palliative care pathway-results from a cluster randomized trial. Cancers (Basel). 2021;13(9):2194.
Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol. 2017;35(8):834–41.
Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009;302(7):741–9.
Groenvold M, Petersen MA, Damkier A, et al. Randomised clinical trial of early specialist palliative care plus standard care versus standard care alone in patients with advanced cancer: the Danish Palliative Care Trial. Palliat Med. 2017;31(9):814–24.
Vanbutsele G, Pardon K, Van Belle S, et al. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol. 2018;19(3):394–404.
Brenne AT, Knudsen AK, Raj SX, et al. Fully integrated oncology and palliative care services at a local hospital in mid-Norway: development and operation of an innovative care delivery model. Pain Ther. 2020;9(1):297–318.
Jordhoy MS, Fayers P, Saltnes T, Ahlner-Elmqvist M, Jannert M, Kaasa S. A palliative-care intervention and death at home: a cluster randomised trial. Lancet. 2000;356(9233):888–93.
Morita T, Miyashita M, Yamagishi A, et al. Effects of a programme of interventions on regional comprehensive palliative care for patients with cancer: a mixed-methods study. Lancet Oncol. 2013;14(7):638–46.
Morita T, Miyashita M, Yamagishi A, et al. A region-based palliative care intervention trial using the mixed-method approach: Japan OPTIM study. BMC Palliat Care. 2012;11:2.
St. Olavs Hospital HF. Forbedringsprogram 2013. https://ekstranett.helse-midt.no/1010/Sakspapirer/41-12%20Vedlegg%202%20Forbedringsprogram%20for%202013.pdf. (In Norwegian only]. Accessed 12 Dec 2017.
Norwegian Ministry of Health and Care Services. The Coordination Reform Proper Treatment—at the right place and right time (white paper). Norwegian Ministry of Health and Care Services; 2009. Report No. 47 (2008–2009) to the Storting. https://www.regjeringen.no/contentassets/d4f0e16ad32e4bbd8d8ab5c21445a5dc/en-gb/pdfs/stm200820090047000en_pdfs.pdf. Accessed 11 Dec 2017.
The Norwegian Directorate of Health. Nasjonalt handlingsprogram for palliasjon i kreftomsorgen [Norwegian National Giudelines]. Oslo: The Norwegian Directorate of Health; 2019. https://www.helsedirektoratet.no/tema/palliasjon. (In Norwegian). Accessed 18 Oct 2019
Driller B, Talseth-Palmer B, Hole T, Stromskag KE, Brenne AT. Cancer patients spend more time at home and more often die at home with advance care planning conversations in primary health care: a retrospective observational cohort study. BMC Palliat Care. 2022;21(1):61.
Sigurdardottir KR, Kaasa S, Rosland JH, et al. The European Association for Palliative Care basic dataset to describe a palliative care cancer population: results from an international Delphi process. Palliat Med. 2014;28(6):463–73.
Groenvold M, Petersen MA, Aaronson NK, et al. The development of the EORTC QLQ-C15-PAL: a shortened questionnaire for cancer patients in palliative care. Eur J Cancer. 2006;42(1):55–64.
Groenvold M, Petersen MA, on behalf of the EORTC Quality of Life Group EQoL. Addendum to the EORTC QLQ-C30 Scoring Manual: scoring of the EORTC QLQ-C15-PAL. 2006. http://www.dmcgpal.dk/files/addendum%20to%20the%20eortc%20qlq%20final%20july%202006.pdf. Accessed 09 Sept 2021.
Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer. 1980;45(8):2220–4.
Bouca-Machado R, Rosario M, Alarcao J, Correia-Guedes L, Abreu D, Ferreira JJ. Clinical trials in palliative care: a systematic review of their methodological characteristics and of the quality of their reporting. BMC Palliat Care. 2017;16(1):10.
Sourial N, Longo C, Vedel I, Schuster T. Daring to draw causal claims from non-randomized studies of primary care interventions. Fam Pract. 2018;35(5):639–43.
Kacha AK, Nizamuddin SL, Nizamuddin J, Ramakrishna H, Shahul SS. Clinical study designs and sources of error in medical research. J Cardiothorac Vasc Anesth. 2018;32(6):2789–801.
Haun MW, Estel S, Rucker G, et al. Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev. 2017; 6:CD011129.
Shanbhag D, Graham ID, Harlos K, et al. Effectiveness of implementation interventions in improving physician adherence to guideline recommendations in heart failure: a systematic review. BMJ Open. 2018;8(3): e017765.
Evans-Lacko S, Jarrett M, McCrone P, Thornicroft G. Facilitators and barriers to implementing clinical care pathways. BMC Health Serv Res. 2010;10:182.
Rosstad T, Salvesen O, Steinsbekk A, Grimsmo A, Sletvold O, Garasen H. Generic care pathway for elderly patients in need of home care services after discharge from hospital: a cluster randomised controlled trial. BMC Health Serv Res. 2017;17(1):275.
Hjermstad MJ, Pirnat A, Aass N, et al. PALLiative care in ONcology (PALLiON): a cluster-randomised trial investigating the effect of palliative care on the use of anticancer treatment at the end of life. Palliat Med. 2024;38(2):229–39.
Rosstad T, Garasen H, Steinsbekk A, Sletvold O, Grimsmo A. Development of a patient-centred care pathway across healthcare providers: a qualitative study. BMC Health Serv Res. 2013;13:121.
Sommerbakk R, Haugen DF, Tjora A, Kaasa S, Hjermstad MJ. Barriers to and facilitators for implementing quality improvements in palliative care—results from a qualitative interview study in Norway. BMC Palliat Care. 2016;15:61.
Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272–83.
Norwegian Ministry of Health and Care Services. Lindrende behandling og omsorg—Vi skal alle dø en dag. Men alle andre dager skal vi leve (white paper). Norwegian Ministry of Health and Care Services; 2020. Report No. 24 (2019–2020) to the Storting. https://www.regjeringen.no/no/dokumenter/meld.-st.-24-20192020/id2700942/. Accessed 1 Oct 2020.
Lohre ET, Thronaes M, Brunelli C, Kaasa S, Klepstad P. An in-hospital clinical care pathway with integrated decision support for cancer pain management reduced pain intensity and needs for hospital stay. Support Care Cancer. 2019;28(2):671–82.
Acknowledgements
The authors thank the Norwegian Cause of Death Registry and Cancer Registry of Norway for providing data. We also thank the study nurses Kjellrun Gravdal and Randi Sunde for their work in the inclusion of participants and data collection, the Study Office at the Cancer Clinic, St. Olav’s Hospital Trondheim University Hospital, and all healthcare professionals at Orkdal Hospital, Molde Hospital, and in the 22 participating municipalities, for their contribution. Finally, we express our gratitude to all patients who participated.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Funding
This work was supported by Norwegian Foundation Dam for Health and Rehabilitation [grant number 148113], the Norwegian Cancer Society, the Norwegian Directorate of Health [grant number 11/2341-26], Norwegian Women’s Public Health Association Orkdal, European Palliative Care Research Centre (PRC), St. Olavs’ Hospital Trondheim University Hospital, and Norwegian University of Science and Technology. The Rapid Service Fee was funded by Norwegian University of Science and Technology. The funding sources were not involved in preparation of the article.
Author information
Authors and Affiliations
Contributions
Anne Kari Knudsen, Jo-Åsmund Lund, Morten Thronæs, and Stein Kaasa designed the study. Anne-Tove Brenne, Erik Torbjørn Løhre, Anne Kari Knudsen, and Bardo Driller recruited participants and collected data. Anne-Tove Brenne, Anne Kari Knudsen, and Cinzia Brunelli analyzed the data. Anne-Tove Brenne, Erik Torbjørn Løhre, and Stein Kaasa wrote the manuscript. Anne-Tove Brenne had the primary responsibility for the final content. All authors commented on previous versions of the manuscript, read, and approved the final version and consented to submission.
Corresponding author
Ethics declarations
Conflict of Interest
Anne-Tove Benne, Erik Torbjørn Løhre, Anne Kari Knudsen, Jo-Åsmund Lund, Morten Thronæs, Bardo Driller, and Cinzia Brunelli declare that they have no competing interests. Stein Kaasa led the committee constituted by the Government from May 2016 to December 2017 that published the Official Norwegian Report on palliative care [6]. Anne Kari Knudsen’s affiliation has changed since the time of the study, and is now affiliated with County Governor Oslo and Viken, Oslo, Norway.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Regional Committee for Medical Research Ethics Central Norway, REK Central (2014/212). Written informed consent was obtained from all individual participants included in the study. In cases where the participant was competent to give oral informed consent but not able to write, an adult family member or HCP signed a proxy consent.
Additional information
Anne Kari Knudsen’s affiliations have changed since the time of this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Brenne, AT., Løhre, E.T., Knudsen, A.K. et al. Standardizing Integrated Oncology and Palliative Care Across Service Levels: Challenges in Demonstrating Effects in a Prospective Controlled Intervention Trial. Oncol Ther (2024). https://doi.org/10.1007/s40487-024-00278-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40487-024-00278-3