Abstract
Introduction
Smoking cessation following lung cancer diagnosis is recommended to improve patient outcomes. Electronic Patient Reported Outcome Measures (ePROMs) may be useful for identifying and facilitating cessation support in patients that continue to smoke after a cancer diagnosis. The primary aim was to investigate the level of agreement between clinician-reported and self-reported patient smoking status during the first visit to a cancer centre (I). Secondary aims included investigating differences between cancer-specific characteristics between never smokers and current/ex-smokers (IIA), and the self-reported frequency of smoking cessation after diagnosis of lung cancer (IIB).
Methods
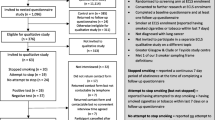
Retrospective single-centre study carried out at a tertiary cancer centre in the UK. Lung cancer patients that completed at least one ePROM questionnaire within 6 weeks of their first visit to the cancer centre (baseline), between February 2019 and February 2020, were included in the study. All ePROM questionnaires included a question regarding smoking status to allow comparison with the clinician records. Patients were offered these electronic questionnaires at each subsequent visit to the hospital.
Results
Of 195 patients included, 24 (12.3%) demonstrated discordance between clinician-reported and self-reported smoking status at the baseline assessment. Clinician-reported ‘current smokers’ were more likely to be discordant with self-reported smoking status, compared with clinician-reported ‘ex-smokers’ and ‘never smokers’ (P = 0.017). Never smokers were more likely to have adenocarcinoma (P < 0.005), present with stage IV cancer (P = 0.023) and receive treatment with palliative intention (P = 0.042), compared with current and ex-smokers. Of those that were reported by clinicians as being current smokers, 9/38 (23.7%) were self-reported ex-smokers. A sub-group of 137 patients completed at least one additional ePROM questionnaire after the baseline and were included in the smoking cessation analysis. Thirty-eight patients were clinician-reported as ‘current smokers’ at baseline. Of these, 9 subsequently stopped smoking, 17 continued and 3 had short periods of cessation, identified through self-reporting.
Conclusion
In most cases, there is concordance between clinician- and self-reported smoking status. A small area of discordance was identified where clinicians reported some patients as ‘current smokers’, whilst patients self-reported having stopped. The causes for this were not explored and require further investigation. This study supports the use of ePROMs as a helpful tool to assess smoking status, and it can be used to identify patients for smoking cessation referral.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is recognised that those patients who continue smoking following a lung cancer report having a lower quality of life and worse physical health outcomes. |
Therefore, it is important to identify those that are still smoking and make appropriate referrals to smoking cessation services. An independent questionnaire, such as an electronic Patient Reported Outcome Measure (ePROM), would be well poised to aid in identifying those patients that still smoke. |
Do patients report a different smoking status on an electronic independent questionnaire compared with what they report to clinicians at their initial clinic visit? |
Patients that self reported as current smokers were more likely to have discordant records than never/ex-smokers (P < 0.05). |
Discordance between patient and clinician warrants follow-up or immediate referral to smoking cessation services. |
Introduction
Lung cancer is the second most common form of cancer for males and females in the UK, with an incidence of 94 per 100,000 per year [1, 2]. In 2015, the National Institute for Health and Care Excellence (NICE) reported that 86% of new lung cancer diagnoses that year were linked to smoking – the most common modifiable risk factor listed [3].
Tobacco smoking causes negative physical health consequences such as impaired wound healing, reduced efficacy of cancer therapy, decreased survival, and an increased risk of recurrence and second cancers [4]. It has also been demonstrated that continued smoking causes a significant reduction in quality of life (QoL) when compared with a non-smoking cohort with lung cancer [5]. In patients with small cell lung cancer (SCLC), it was shown that smoking significantly reduced quality of life. [6]. With the effects of continued smoking on physical and mental health, smoking cessation should be an integral part of the cancer management plan for patients with lung cancer.
Studies suggest that 40–50% of patients are smokers at the time of lung cancer diagnosis, with about half of this cohort stopping after the diagnosis has been made [5, 7]. Importantly, one must also be aware of those who resume smoking after considering themselves as ex-smokers and so continuous follow-up is needed. One study reports that 66/154 (42.9%) of lung cancer patients reported smoking within 12 months after a period of abstinence following lung cancer resection [8]. Of the patients that relapsed, 60% did so in the first 2 months.
Smoking is less of a causative factor in adenocarcinomas [9]. This subtypes has an incidence of 17.1 and 14.7 per 100,000 person-years in men and women, respectively [10]. Discerning smoking status is of importance in a healthcare setting so that appropriate smoking cessation advice can be given. In-/outpatient settings are an ideal opportunity for discussions with patients regarding smoking cessation. However, time pressures upon clinical teams can restrict the opportunity for this important intervention. Self-reported smoking status has been reported as accurate for never smokers, current smokers and those that quit more than 1 year ago [13]. Electronic Patient Reported Outcome Measures (ePROMs) may represent an efficient and accurate medium to collect and analyse patient smoking information.
A Patient Reported Outcome (PRO) is a unit of information that comes directly from the patient without alteration or interpretation by anyone else [14]. PROs are reported using Patient Reported Outcome Measures (PROMs) which often take the form of self-completed questionnaires [14]. PROMs provide extremely important information on a multitude of metrics as determined by the tool creator – most often the clinical team at one specific trust [14]. Data from PROMs is utilised mainly in two ways: informing individual patient care and informing health services/facilitating policy development [15].
Electronic Patient Reported Outcome Measures (ePROMs) are self-reported questionnaires administered electronically rather than on paper. With the increasing prevalence of smart phones and laptops allowing patient’s to complete ePROMs remotely from their own home or outside a clinical setting, ePROMs have come to the fore as a method of collecting remote patient data [15].
A 1994 meta-analysis which included papers with biochemical validation as a means of confirmation, reported high levels of sensitivity and specificity for patient reported smoking status through either self-reporting questionnaires or clinician interviews [16]. The meta-analysis concluded that interview-reported status had a slightly higher sensitivity and specificity that self-reporting questionnaires. However, with service pressures it may not always possible to obtain patient smoking status from interviews. With the emergence of electronic PROMs, it is pertinent to discern their ability to accurately identify smoking status.
Objectives
The primary aim of this study was to identify, describe and analyse agreement between clinician-reported smoking status and patient self-reported using an ePROM questionnaire in patients with lung cancer. Secondary aims include investigating differences between cancer-specific characteristics based on smoking status in patients with lung cancer and describing the self-reported frequency of smoking cessation after diagnosis of lung cancer using ePROM follow-up data.
Methods
A comprehensive UK cancer centre introduced an ePROM initiative routinely into patient care pathways in January 2019. Patients that completed a baseline ePROM questionnaire within 6 weeks of clinicians completing the standard ‘Diagnosis and Staging (DS)’ baseline form for new patients in clinic between February 2019 and February 2020 were included in this study. Patients with no information regarding smoking status and/or no completed ePROMs were excluded.
Patients with lung cancer at a comprehensive UK cancer centre are initially seen in clinic by an oncologist. At this first appointment, the clinician completes a DS baseline form, which includes patient baseline information and tumour characteristics. This form includes the clinician-reported smoking status (options include ‘current smoker’, ‘ex-smoker’ and ‘never smoker’) and the option of recording pack years. Clinician-reported smoking status is obtained via a direct question from clinician to patient during the consultation and without biochemical testing. Independently of this, patients are also asked to complete an ePROM questionnaire before the appointment via an email or text message (at this first appointment and all subsequent visits), which is optional but if completed provides self-reported smoking status data. The ePROMS platform has been operational since January 2019 and uses electronic questionnaires that include symptom-based questions (developed using the Common Terminology Criteria for Adverse Events Version 5.0 and patient and clinician feedback) and QoL questions (EQ-5D-5L) [17]. Patients are asked to ‘Please select the statement about smoking most applicable to you’ by answering with ‘current smoker’, ‘ex-smoker’ or ‘I have never smoked’. No further definitions of these terms are offered in the ePROM. In March 2020, a statement regarding smoking cessation was added to the tool: ‘Please tick this box if you wish to be referred to the smoking cessation service’. The smoking cessation service uses a number of cessation methods including group and one-to-one sessions and pharmaceutical treatment. Smoking cessation management was tailored based on patient preference. Subsequent smoking cessation was determined solely by ePROM response and without biochemical testing.
Medical records were reviewed to collect data for analysis. As per the meta-analysis discussed above, clinician-reported patient smoking status was used to stratify patients on smoking status for further analysis [16]. Primary aims were analysed using a chi-squared test owing to the categorical nature of the variables. The test was carried out using R [18]. Following the initial chi-squared test, a chi-squared test with Yates’ correction was carried out to reduce the risk of a type 1 error. Secondary aims were analysed using a descriptive analysis, chi-squared test for categorical variables and unpaired two-tailed t-test for continuous variables. For all statistical tests significance was set at P = 0.05.
This study was reviewed and approved as a service evaluation by the Quality Improvement and Clinical Audit Committee at a comprehensive UK cancer centre in June 2021. Ethical approval was not required for this study and no identifying patient information has been published.
Results
Primary Aim Analysis
One hundred ninety-five patients were included in the primary analysis. Patient demographics and disease characteristics are presented in Table 1.
Overall, 24/195 (12.3%) patients demonstrated discordance between clinician-reported and self-reported smoking status. Table 2 demonstrates the smoking status of patients as per clinician and self-reporting at baseline. Similar proportions of patients were reported as ex-smokers by clinician reporting 143/195 (73.3%) and self-reporting 140/195 (71.8%). Figure 1 shows how discordance varied depending on clinician-reported patient smoking status at baseline. Of those that were reported by clinicians as being current smokers, 9/38 (23.7%) were self-reported ex-smokers. Comparatively, for baseline clinician-reported ex-smokers and never smokers, 14/143 (9.8%) and 1/14 (7.1%) respectively showed discordance with their self-reported smoking status. When discordance was analysed based on current smoking status as per baseline clinician reporting [current smokers versus (ex-smokers + never smokers)] the difference was statistically significant according to a chi-squared analysis; X2(1, N = 195) = 5.57, P = 0.017 [with Yate’s correction; X2 (1, N = 195) = 4.43, P < 0.05]. See Supplementary Table 1 for the completed contingency table used.
Secondary Aims Analysis
Table 3 presents patient information stratified by the smoking status according to baseline clinician reporting. Never smokers with lung cancer were more likely to be female (P = 0.023), to have an adenocarcinoma (P < 0.005) and were more likely to present at Stage IV (P = 0.023). Whilst smokers (ex or current) were more likely to develop a squamous NSCLC (P = 0.047) and to present at Stage III (P = 0.031). In keeping with this finding, palliation was a more likely treatment intention for never smokers than for smokers and ex-smokers (P = 0.042). Table 4 demonstrates the significant (P = 0.046) correlation between clinician-reported smoking status and Eastern Cooperative Oncology Group (ECOG) performance status.
The median number of ePROMs completed per patient per month of follow-up was 0.79, with a range of 1–3.5. Of the 195 patients included in the final analysis, 58 had only completed one ePROM. Hence, it was not possible to comment on their continued smoking status after lung cancer diagnosis. Figure 2 provides a proportional representation of smoking status whilst patients were being followed up with ePROMs. Of the 137 patients with more than one ePROM, 97 (70.8%) were clinician reported as ex-smokers at baseline and of this cohort, 86 (88.7%) patients self-reported continued cessation and 11 (11.3%) patients restarted smoking. Ten patients (7.3%) stopped smoking after reporting that they were current smokers at some stage after lung cancer diagnosis. Of the 30 patients that completed an ePROM after March 2020 (following the introduction of the option of requesting referral to the smoking referral team) and self-reported as current smokers, only 3/30 (10%) requested referral to smoking cessation. These three patients requested cessation referral in 7/8 (87.5%), 2/4 (50.0%) and 1/13 (7.7%) of their ePROMs, respectively. A regression analysis of lung cancer stage and smoking cessation status at the end of the ePROM follow-up period showed no significant correlation (R2 = 0.005, P = 0.414).
Discussion
This study demonstrated that 24/195 (12.3%) patients showed discordance between self-reported and clinician-reported patient smoking status. The discordance rates were higher in those patients who are current smokers compared with never/ex-smokers. Although this was not investigated as part of the study, this could be owing to a variance in how patients and clinicians define smoker and ex-smoker. Furthermore, a lag time between clinician reporting and patient reporting may allow time in which a genuine change to smoking status may occur. Clear definitions of smoker and ex-smoker and encouragement from clinical teams for patients to complete the ePROM as soon as possible may help to decrease the rate of discordance.
Some of the patients in this group are also likely to be patients that have started trying to stop smoking in the past year. Morales et al. [13] highlight this as a time of discrepancy in reporting. Therefore, recent cessation may require increased support/follow-up. Other possible reasons for the discrepancies include limited consultation time leading to incorrect reporting of smoking status, patient difficulties in completing ePROM, patient belief of prejudice or bias against smokers, different definitions of ‘ex-smoker’ and difficult communication between patient and clinician [19,20,21]. The presence of these discordances strongly supports the use of ePROMs as a method of data collection, as an important clinical aim is that current smokers should be identified and referred for cessation. Having a second method of capturing smoking status easily at a different timepoint allows for maximum cessation treatment to be provided. However, our results show that the median number of ePROMs completed per month of follow-up was less than one, and that 58 (29.7%) patients completed only one ePROM. This reiterates that, although a useful avenue for collecting information about smoking status, smoking must also be discussed separately in clinic. Importantly, this may identify patients who have had interval relapses which the ePROM may not have captured. To better capture these patients, asking about smoking status ‘since the last ePROM was completed’ rather than asking about smoking status ‘in the last week’ may prove beneficial.
The issue with a modest proportion of discordance in current smokers as reported by a baseline ePROM is that there has been a missed opportunity for cessation advice. As highlighted in the introduction, studies have found that half of all smoking patients cease smoking after a lung cancer diagnosis [5, 7]. Therefore, this first consultation is an important opportunity to provide patients with smoking cessation advice and support. Smoking cessation is important as cigarette smoking reduces the efficacy of and increases resistance to many anticancer agents. [22] For example, Pezzuto et al. [23] showed that patients with advanced NSCLC with epidermal growth factor receptor mutations treated with erlotinib + varenicline had more significantly improved lung function than those treated with erlotinib alone. Furthermore, it has been postulated that chemotoxicity could be increased by concurrent cigarette smoking. [22]
Of the 29 patients with continued ePROM follow-up that reported smoking at their baseline ePROM, 9 ceased smoking, 17 continued smoking and 3 ceased smoking for a finite period. The ePROM had no option for self-referral for smoking cessation advice prior to March 2020, and after this point a passive statement on the desire to be referred for smoking cessation was added which could be left blank by the patient. With only 10% of eligible patients self-referring for cessation, it may be beneficial to change this from a passive statement, ‘Tick if you would like a referral to the smoking cessation services’, to a question that requires patient action such as ‘Please select whether or not you would like to be referred to the smoking cessation services’ or an opt-out statement such as ‘Tick if you would not like a referral to the smoking cessation services’. Having the option for self-referral may also help to capture patients who had initially declined smoking cessation referral [24].
There were some clear demographic differences between current/ex-smokers and never smokers in this cohort. Never smokers with lung cancer, of which women were affected disproportionately, generally presented with later stage disease and were more likely to receive treatment with palliative intent. Never smokers also demonstrated a predisposition to developing an adenocarcinoma. The differences observed here are agreeable with other prominent literature that suggests that lung cancer in never smokers is distinct from lung cancer in tobacco smokers [25].
The main limitations of this study include the limited number of patients and timepoints collected. Further research may consider the optimum interval between ePROM collection that best facilitates smoking cessation. Delineating the most likely period of smoking relapse after lung cancer diagnosis may help clinicians to provide targeted cessation information during this period.
Conclusion
Overall, this study supports the use of ePROMs as a useful tool to obtain data on smoking status and identify patients for smoking cessation referral. Results have shown that clinician-reported current smokers have a 23.7% discordance rate when compared with their self-reported smoking status. Discordance rates in ex-smoker and never smokers are lower, at 9.7% and 7.1%, respectively. Such discordance supports the use of ePROMs as an important tool for recording patient smoking status and should be considered when determining support for smoking cessation. Owing to a non-negligible number of patients continuing to smoke following diagnosis, it is important that cessation is encouraged when possible. A change in the wording of the ePROM question relating to smoking cessation should be considered to increase self-referrals. The data and analysis provided will help to inform further research regarding more intense follow-up and cessation discussions within patients who are current smokers.
References
Cancer Research UK. Lung cancer statistics (2020).
Cancer Research UK. Cancer incidence for common cancers (2020).
NICE. Lung cancer: diagnosis and management (2019).
Daniel M, Keefe FJ, Lyna P, et al. Persistent smoking after a diagnosis of lung cancer is associated with higher reported pain levels. J Pain. 2009;10:323–8. https://doi.org/10.1016/j.jpain.2008.10.006.
Garces YI, Yang P, Parkinson J, et al. The relationship between cigarette smoking and quality of life after lung cancer diagnosis. Chest. 2004;126:1733–41. https://doi.org/10.1378/chest.126.6.1733.
Chen J, Qi Y, Wampfler JA, et al. Effect of cigarette smoking on quality of life in small cell lung cancer patients. Eur J Cancer. 2012;48:1593–601. https://doi.org/10.1016/j.ejca.2011.12.002.
Baser S, Shannon VR, Eapen GA, et al. Smoking cessation after diagnosis of lung cancer is associated with a beneficial effect on performance status. Chest. 2006;130:1784–90. https://doi.org/10.1378/chest.130.6.1784.
Walker MS, Vidrine DJ, Gritz ER, et al. Smoking relapse during the first year after treatment for early-stage non-small-cell lung cancer. Cancer Epidemiol Prev Biomark. 2006;15:2370–7. https://doi.org/10.1158/1055-9965.EPI-06-0509.
Kabat GC, Wynder EL. Lung cancer in nonsmokers. Cancer. 1984;53:1214–21. https://doi.org/10.1002/1097-0142(19840301)53:5%3c1214::AID-CNCR2820530532%3e3.0.CO;2-8.
Thun MJ, Henley SJ, Burns D, Jemal A, Shanks TG, Calle EE. Lung cancer death rates in lifelong nonsmokers. J Natl Cancer Inst. 2006;98:691–9. https://doi.org/10.1093/jnci/djj187.
Laugsand EA, Sprangers MAG, Bjordal K, Skorpen F, Kaasa S, Klepstad P. Health care providers underestimate symptom intensities of cancer patients: a multicenter European study. Health Quality Life Outcomes. 2010. https://doi.org/10.1186/1477-7525-8-104.
Basch E, Jia X, Heller G, et al. Adverse symptom event reporting by patients vs clinicians: relationships with clinical outcomes. J Natl Cancer Inst. 2009;101:1624–32. https://doi.org/10.1093/jnci/djp386.
Morales NA, Romano MA, Michael Cummings K, et al. Accuracy of self-reported tobacco use in newly diagnosed cancer patients. Cancer Causes Control. 2013;24:1223–30. https://doi.org/10.1007/s10552-013-0202-4.
Weldring T, Smith SMS. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013;6:61. https://doi.org/10.4137/HSI.S11093.
Chen J, Ou L, Hollis SJ. A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv Res. 2013. https://doi.org/10.1186/1472-6963-13-211.
Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84:1086. https://doi.org/10.2105/AJPH.84.7.1086.
Christodoulou M, Khalil N, Rust P, et al. The use of electronic patient reported outcome measures (ePROMs) to revolutionise cancer care. In: NCRI cancer conference (National Cancer Research Institute (2019)
R Core Team. R: a language and environment for statistical computing. (2021)
Takeuchi EE, Keding A, Awad N, et al. Impact of patient-reported outcomes in oncology: a longitudinal analysis of patient-physician communication. J Clin Oncol. 2011;29:2910–7. https://doi.org/10.1200/JCO.2010.32.2453.
Basch E, Iasonos A, Barz A, et al. Long-term toxicity monitoring via electronic patient-reported outcomes in patients receiving chemotherapy. J Clin Oncol. 2007;25:5374–80. https://doi.org/10.1200/JCO.2007.11.2243.
Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. Br Med J. 2004;328:1470–3. https://doi.org/10.1136/bmj.38111.639734.7c.
Condoluci A, Mazzara C, Zoccoli A, Pezzuto A, Tonini G. Impact of smoking on lung cancer treatment effectiveness: a review. Future Oncol. 2016;12(18):2149–61. https://doi.org/10.2217/fon-2015-0055.
Pezzuto A, Stumbo L, Russano M, et al. Impact of smoking cessation treatment on lung function and response rate in EGFR mutated patients: a short-term cohort study. Recent Pat Anticancer Drug Discov. 2015;10(3):342–51. https://doi.org/10.2174/1574892810666150806111014.
May JR, Klass E, Davis K, et al. Leveraging patient reported outcomes measurement via the electronic health record to connect patients with cancer to smoking cessation treatment. Int J Environ Res Public Health. 2020;17:1–13. https://doi.org/10.3390/ijerph17145034.
Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers—a different disease. Nat Rev Cancer. 2007;7:778–90. https://doi.org/10.1038/nrc2190.
Acknowledgements
The authors would like to thank the participants of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by James Convill, Fabio Gomes and Fiona Blackhall. The first draft of the manuscript was written by James Convill and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
James Convill, Janelle York, Corrine Faivre-Finn, Fiona Blackhall and Fabio Gomes declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Ethical approval was not required for this study and no identifying patient information has been published. Patient anonymity was ensured and informed consent was obtained at the time of original data collection. This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments.
Data Availability
The datasets generated during and/or analysed during the current study are not publicly available due to the use of patient identifiable information in the main dataset.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Convill, J., Blackhall, F., Yorke, J. et al. The Role of Electronic Patient-Reported Outcome Measures in Assessing Smoking Status and Cessation for Patients with Lung Cancer. Oncol Ther 10, 481–491 (2022). https://doi.org/10.1007/s40487-022-00210-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-022-00210-7