Abstract
Introduction
The treatment of multiple myeloma (MM) remains a challenge as patients eventually progress through several lines of therapy (LOTs), requiring use of multiple MM drug classes. In this retrospective US claims-database study, we examined the healthcare costs of patients with MM who received ≥ 4 prior LOTs, including triple-class exposure (TCE).
Methods
Adult patients with MM were selected from the IBM MarketScan Commercial and Medicare claims databases (1 January 2012–30 June 2021). Eligible patients were required to have received at least four prior LOTs, and TCE (i.e., received a proteasome inhibitor, immunomodulatory drug, and anti–CD38-targeted monoclonal antibody) after the first-observed diagnosis of MM. The index date was defined as the initiation date of the first subsequent LOT after meeting the eligibility criteria for the study, and this date had to be after 1 January 2017 to capture contemporary cost estimates. The primary outcome measurements were all-cause and MM-related healthcare costs after the index date.
Results
The study population included 68 patients with MM (63% men), with a mean age of 59.8 years. Mean duration from first-observed MM diagnosis until index date averaged 46.7 months. During a mean follow-up of 21.9 months, total all-cause healthcare costs averaged US$757,386 per patient (equivalent to US$34,610 per patient per month). MM-related healthcare costs (US$670,561 per patient) contributed on average 88.5% to the total all-cause healthcare costs; the majority (67.2%) of MM-related healthcare costs were attributed to drug and infusion costs (US$450,952 per patient).
Conclusions
In this retrospective US claims-database study, patients with MM with ≥ 4 prior LOTs, including TCE, continued to experience high healthcare costs that were mostly attributable to anti-myeloma drugs and their administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Treatment of multiple myeloma (MM) remains a challenge as patients eventually progress through several lines of therapy (LOTs), requiring the use of multiple MM drug classes. |
In a previous study, we examined the healthcare costs incurred by patients with MM after they had triple-class exposure (TCE) and had received at least one subsequent LOT. |
In this follow-up analysis, we have specifically examined the healthcare costs of patients with MM who received ≥ 4 prior LOTs, including TCE, to provide an assessment of the potential value of newer treatment options for these patients. |
What was learned from the study? |
During a mean follow-up of 21.9 months, total all-cause healthcare costs averaged US$757,386 per patient (equivalent to US$34,610 per patient per month). |
MM-related healthcare costs (US$670,561 per patient) contributed on average 88.5% to the total all-cause healthcare costs; the majority (67.2%) of MM-related healthcare costs were attributed to drug and infusion costs (US$450,952 per patient). |
In this retrospective US claims-database study, patients with MM who received ≥ 4 prior LOTs, including TCE, continued to experience high healthcare costs with most of these costs attributable to anti-myeloma drugs and their administration. |
These findings emphasize the need for novel therapies for heavily pre-treated MM patients to reduce the healthcare economic burden of this patient population and improving patient outcomes. |
Introduction
An estimated 34,920 patients in the United States in 2021 were diagnosed with multiple myeloma (MM), a relatively rare cancer, but the second most common hematological cancer [1, 2]. When initially diagnosed with MM, approximately two-thirds of patients are aged > 65 years, with the median age at diagnosis of 70 years [3]. Currently, MM is an incurable disease, and its clinical course is characterized by a succession of progressively shorter remissions and relapses until patients become refractory to available treatments.
Over the past few decades, the 5-year survival rate of MM patients has more than doubled [4, 5]. Improved patient outcomes have in part been due to the introduction of new MM drug classes, including proteasome inhibitors (PIs), immunomodulatory drugs (IMiDs), and targeted anti-CD38 monoclonal antibodies (mAbs) [5,6,7]. The standard of care for newly diagnosed patients with active symptomatic MM (NDMM) is a triplet regimen containing a PI and/or IMiD in combination with a corticosteroid or chemotherapy. The National Comprehensive Cancer Network (NCCN) clinical practice guideline (v3.2021) recommends the triplet regimens of bortezomib, lenalidomide and dexamethasone, and bortezomib, cyclophosphamide, and dexamethasone as preferred primary therapies for stem cell transplant (SCT)-eligible patients and SCT-ineligible patients with NDMM [8].
Although these triplet regimens have been widely utilized in recent years among newly diagnosed patients, most patients eventually relapse or become refractory to treatment [9, 10]. Subsequent treatment regimens typically consist of doublet or triplet regimens that contain different combinations of one or more PIs, IMiDs, or mAbs with corticosteroids and/or chemotherapy. However, these successive lines of therapy (LOTs) have generally resulted in shorter durations of responses, decreased depth of responses, and lower survival rates [11, 12]. Once a patient has relapsed after having received regimens that contained a PI, IMiD, and anti-CD38 mAb, they are considered to be triple-class exposed (TCE). TCE patients have limited treatment options and worse clinical outcomes [13, 14]. In the Monoclonal Antibodies in Multiple Myeloma: Outcomes after Therapy Failure (MAMMOTH) study, median overall survival of TCE patients was 9.2 versus 11.2 months for patients who were refractory to only one other MM drug class; median overall survival further decreased to 5.6 months among TCE patients who were refractory to multiple PIs and IMiDs [14]. Previously, we assessed the healthcare costs incurred by patients with MM after they were TCE and had received at least one subsequent LOT [15]. In this follow-up study, we have specifically examined the healthcare costs of patients with MM who had received ≥ 4 prior LOTs, including TCE, to provide a better understanding of the potential value of new treatment options for these patients.
Methods
Study Design and Data Source
This was a retrospective US claims-database study that used the IBM® MarketScan® Commercial Claims and Encounters (CCAE) and Medicare Supplemental (MDCR) databases. These databases capture utilization and the associated costs of inpatient and outpatient medical services and pharmacy services, in addition to patient demographics and enrollment status. Only de-identified patient data are contained within the CCAE and MDCR databases and they are both fully compliant with the Health Insurance Portability and Accountability Act (HIPAA).
Study Population
Adult patients (≥ 18 years of age) diagnosed with MM between 1 January 2012 and 30 June 2021 were selected from the MarketScan CCAE and MDCR databases. MM was identified according to International Classification of Diseases (ICD), Ninth/Tenth Revision Clinical Modification codes (ICD-9: 203.0x; ICD-10: C90.0x). Patients were required to be continuously enrolled in medical/pharmacy benefit plans and not exposed to MM treatments for at least 12 months prior to their first-observed MM diagnosis. Patients diagnosed with other malignancies prior to the first-observed MM diagnosis date were excluded from the study.
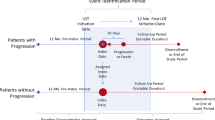
At the index date, patients were required to have received at least four prior LOTs, including TCE, defined as having received a PI, IMiD, and anti-CD38 targeted mAb recommended by the NCCN guideline [8] after their first-observed MM diagnosis. The index date was defined as the initiation date of the first subsequent LOT after meeting the eligibility criteria for the study. Additionally, the index date was required to have occurred after 1 January 2017 in order to capture contemporary cost estimates. Lastly, patients were required to have had continuous enrollment in a medical/pharmacy benefit plan and to have survived at least 1 year after index date. Patients were followed until the end of the study period, continuous enrollment, or death, whichever occurred first.
Treatment Regimens and LOT Definitions
Treatment regimens and LOT definitions have been described in detail previously [15]. A summary of these methods is provided below. Each treatment regimen was defined by a start and end date and was comprised of ≥ 1 MM medications recommended by the NCCN guidelines [8]. Medical and pharmacy claims were used to identify treatment regimens during the first 60 days after study initiation. The initiation date of the first (i.e., index) treatment regimen was the date of the first claim for an identified MM treatment, and that regimen ended on the discontinuation date or date of treatment change (i.e., augmentation or switching), whichever occurred first. Each treatment regimen change or start of a new regimen was considered to be a LOT change. Changes in any agent (‘targeted’ or chemotherapy) within 60 days of first treatment was not considered a LOT change.
A treatment gap was the number of days from the last day of supply to next date of dispensing, with a maximum allowable gap of 90 days. SCT before the end of a gap added a 6-month allowed gap. No medication refilled within the maximum allowed gap after supply days expired was considered to be a treatment discontinuation. Medications identified from the Healthcare Common Procedure Coding System (HCPCS) codes used the number of days supplied from the recommended treatment schedule.
Augmentations were when a patient started a new MM medication recommended by the NCCN guideline within 60 days prior to discontinuation of any of the treatments in the current regimen. A switch was when a new MM medication recommended by the NCCN guideline was started and at least one medication in the current regimen was discontinued within 60 days of beginning the new medication. Addition of chemotherapy agents (e.g., cyclophosphamide, doxorubicin, melphalan) was considered to be a LOT change.
A treatment regimen was discontinued once all medication in the regimen (corticosteroids not considered) were discontinued or an augmentation/switching occurred. Use of maintenance therapy (e.g., lenalidomide or bortezomib monotherapy) within 6 months after SCT was not considered to be switching or a LOT change. The regimen discontinuation date was extended until the discontinuation of maintenance therapy.
Demographic and Clinical Characteristics
For each MM patient included in the study population, demographic and clinical characteristics, (including age, sex, health plan type, insurance type [Commercial or Medicare], US region of residence, Quan Charlson Comorbidity Index [QCI] score, and year of index date) were evaluated on their index date or during the 12-month baseline period.
Healthcare Resource Utilization and Associated Costs
Over the 12-month period prior to index date, all-cause and MM-related (i.e., claims including an ICD-9/10 code indicating an MM diagnosis) healthcare resource utilization (HCRU) costs and associated costs were examined for each patient. HCRU included the number of hospitalizations and days of inpatient stays, number of emergency room (ER) visits, number of outpatient visits, and number of pharmacy fills (all-cause only). Average MM-related healthcare costs were reported for inpatient cost, ER cost, outpatient cost, drug costs, drug infusion cost, SCT cost, and other healthcare costs.
The primary outcome measures of this study were all-cause and MM-related healthcare costs that occurred after a patient’s index date. These costs were reported as the mean cost per patient (such as total all-cause healthcare cost) or mean cost per patient per month (PPPM). Results are provided for the overall study cohort, in addition to the subset of patients who were < 65 years of age (Commercially insured), who made up the majority (91.2%) of the sample. The average monthly total all-cause healthcare costs per patient were also extrapolated to estimate the total all-cause healthcare costs incurred for up to 36 months after a patient’s index date.
Statistical Analyses
All statistical analyses were descriptive and conducted using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Patient Characteristics
A total of 68 patients with MM were included in this study. The mean duration from first-observed MM diagnosis until the index date averaged 46.7 months (Table 1). Among this patient sample, the mean age on index date was 59.8 years and 60.3% were male (Table 1). Most patients had a preferred provider organization (PPO) health plan (39.7%) (Table 1). Mean QCI score was 5.2 (Table 1).
HCRU and Associated Costs Prior to Index Date
During the 12 months prior to the index date, the average number of all-cause hospitalizations, ER visits, and outpatient visits were 1.6, 0.6, and 58.6, respectively, per patient (Table 2). The mean length of stay for all-cause hospitalizations was 15.6 days per patient (Table 2). Total all-cause healthcare costs per patient were a mean of $468,514 (all costs reported here are in US dollars) (Table 2).
Further, during this 12-month period, the average number of MM-related hospitalizations, ER visits, and outpatient visits per patient were 1.4, 0.2, and 45.9, respectively (Table 2). The mean duration of stay for MM-related hospitalizations was 15.2 days per patient (Table 2). Mean total MM-related healthcare costs per patient were $432,366, accounting for 93.1% of total all-cause healthcare costs on average (Table 2). Of the total MM-related healthcare costs, hospitalizations accounted for 10.7%, outpatient visits for 12.6%, and MM drug and infusion costs for 69.8% (Table 2).
Healthcare Costs Incurred After the Index Date
The mean duration of follow-up after the index date was 21.9 months (Table 3). During this follow-up period, total all-cause healthcare costs averaged $757,386 per patient (equivalent to $34,610 PPPM; Table 3). Among patients who were aged < 65 years (N = 62), the total all-cause healthcare costs averaged $793,640 per patient (equivalent to $35,760 PPPM; Table 3).
During patient follow-up, MM-related healthcare costs ($670,561 per patient) contributed on average 88.5% to the total all-cause healthcare costs (Table 3). The majority (67.2%) of the MM-related healthcare costs were attributed to MM drug and infusion costs ($450,952 per patient; Table 3). Similarly, among patients who were aged < 65 years, mean total MM-related healthcare costs per patient were $700,541, representing on average 88.3% of the total all-cause healthcare costs per patient (Table 3).
When the average monthly all-cause healthcare costs incurred per patient were extrapolated, the cumulative costs incurred at 24 and 36 months after the index date were estimated at $830,632 and $1,245,948, respectively (Table 4).
Discussion
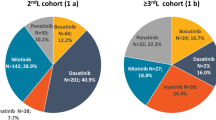
In this retrospective US claims-database study of patients with MM who received ≥ 4 prior LOTs, including TCE, total all-cause healthcare costs averaged $757,386 per patient during a mean follow-up of approximately 22 months (equivalent to $34,610 PPPM). Approximately 88.5% of these costs were MM-related, with the majority (67%) of these costs largely attributed to MM drug and infusion costs ($450,952 per patient). These study findings are similar to those published previously among a larger sample of patients with MM who had TCE (N = 85) where total all-cause healthcare costs averaged $34,578 PPPM over a 21-month follow-up, amounting to $722,992 per patient, of which approximately 91% were MM-related (MM drug/infusion costs: 66% of MM-related costs) [15].
These findings are also consistent with a publication (study period: December 2015-September 2018) by Madduri et al., which reported average total all-cause healthcare costs of $37,033 PPPM among 154 patients with MM who had TCE and had initiated at least one subsequent LOT; MM-related healthcare costs represented 96% of the total all-cause healthcare costs in this study [16]. The findings of Madduri et al. also indicate that MM drug and infusion costs contributed over one-half of the monthly MM-related healthcare costs [16]. The findings of the current study, along with other published studies [15, 16], show that patients with MM who had TCE and advance through multiple LOTs continue to incur high healthcare costs, primarily attributed to MM drug and infusion costs. The high monthly and total healthcare economic burden for this heavily pre-treated MM patient population underscores the possible value from newer treatment options for these patients.
In this study, we specifically required that MM patients had received at least four prior LOTs at the index date, including TCE. These patients have experienced a considerable burden of exposure to multiple MM drug classes and are vulnerable to treatment failure and worsening outcomes in subsequent LOTs. In the MAMMOTH study, median overall survival duration of patients with MM declined as the patients became refractory to more MM medications, with those penta-refractory (refractory to anti-CD38 targeted mAb, 2 PIs and 2 IMiDs) having a median overall survival of only 5.6 months [14]. Across the entire study cohort (N = 275; non-triple refractory: 21%; triple/quad-refractory: 54%; penta-refractory: 25%), median overall survival was only approximately 9 months [14]. Although more recently approved MM treatments, including pomalidomide, carfilzomib, elotuzumab, daratumumab, ixazomib, and bortezomib-lenalidomide combinations, have shown greater effectiveness in real-world populations of patients with MM, their clinical benefits were found to diminish as patients advanced through multiple LOTs [17], with these results indicating that these patients continue to experience a high treatment burden and are in need of novel therapies to improve outcomes.
This study was an observational, retrospective, US claims-database analysis that utilized the MarketScan CCAE and MDCR databases. Thus, the study findings should be interpreted in this context. First, the study population represents patients with US Commercial insurance and/or employer-sponsored Medicare coverage; as such, the study findings may not represent patients with MM who have varying insurance types or live in other countries. The MarketScan databases comprise claims with differing distributions across US regions. Furthermore, the databases consist of claims submitted by healthcare providers for reimbursement; as such, these claims may contain possible coding errors, i.e., coding for the purpose of rule-out rather than actual disease, and under-coding, without the possibility of verifying reported diagnoses. In this study, we defined MM-related HCRU as claims including an ICD-9/10 code indicating an MM diagnosis. This may have led to capturing some HCRU costs unrelated to MM; for example, patients with MM may have sought healthcare for other unrelated comorbidities and medical reasons and the providers may have included a diagnosis code indicating the patient had MM. However, this is a common method for identifying MM-related HCRU in health economics research studies [15, 17]. In the case of the measurement of pharmacy fills (all-cause only), the data only reflect those filled by patients and may not capture all that were actually prescribed. Additionally, the MM treatment regimens examined in this study were approved by the US Food and Drug Administration at different time periods, and MM drug regimens are continuing to evolve. Notably, the time frame of this study was mostly prior to the first approval of chimeric antigen receptor (CAR) T-cell therapy for the treatment of MM, and further study of this type of treatment on patients’ healthcare costs is warranted.
Conclusions
In this retrospective US claims-database study, patients with MM who had received ≥ 4 prior LOTs, including TCE, continued to experience high healthcare costs, with most of these costs attributable to anti-myeloma drugs and their administration. Such findings emphasize that other novel therapies are still needed for improving outcomes and reducing healthcare economic burden in this heavily pre-treated MM patient population.
References
American Cancer Society. Key statistics about multiple myeloma. https://www.cancer.org/cancer/multiple-myeloma/about/key-statistics.html. Accessed 3 Feb 2022.
Kazandjian D. Multiple myeloma epidemiology and survival: a unique malignancy. Semin Oncol. 2016;43:676–81.
Kaweme NM, Changwe GJ, Zhou F. Approaches and challenges in the management of multiple myeloma in the very old: future treatment prospects. Front Med (Lausanne). 2021;8: 612696.
National Cancer Institute: SEER. Cancer Stat Facts: Myeloma. https://seer.cancer.gov/statfacts/html/mulmy.html. Accessed 3 Feb 2022.
Padala SA, Barsouk A, Barsouk A, et al. Epidemiology, staging, and management of multiple myeloma. Med Sci (Basel). 2021;9:3.
Noonan K, Colson K. Immunomodulatory agents and proteasome inhibitors in the treatment of multiple myeloma. Semin Oncol Nurs. 2017;33:279–91.
Radocha J, van de Donk N, Weisel K. Monoclonal antibodies and antibody drug conjugates in multiple myeloma. Cancers (Basel). 2021;13:1571.
Kumar SK, Callander NS, Adekola K, et al. Multiple myeloma, version 3.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020;18:1685–717.
Bobin A, Liuu E, Moya N, et al. Multiple myeloma: an overview of the current and novel therapeutic approaches in 2020. Cancers (Basel). 2020;12:2885.
Pinto V, Bergantim R, Caires HR, Seca H, Guimaraes JE, Vasconcelos MH. Multiple myeloma: available therapies and causes of drug resistance. Cancers (Basel). 2020;12:407.
Yong K, Delforge M, Driessen C, et al. Multiple myeloma: patient outcomes in real-world practice. Br J Haematol. 2016;175:252–64.
Braunlin M, Belani R, Buchanan J, Wheeling T, Kim C. Trends in the multiple myeloma treatment landscape and survival: a U.S. analysis using 2011–2019 oncology clinic electronic health record data. Leuk Lymphoma. 2021;62:377–86.
Mikhael J. Treatment options for triple-class refractory multiple myeloma. Clin Lymphoma Myeloma Leuk. 2020;20:1–7.
Gandhi UH, Cornell RF, Lakshman A, et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia. 2019;33:2266–75.
Jagannath S, Joseph N, He J, et al. Healthcare costs incurred by patients with multiple myeloma following triple class exposure (TCE) in the US. Oncol Ther. 2021;9:659–69.
Madduri D, Hagiwara M, Parikh K, et al. Real-world treatment patterns, healthcare use and costs in triple-class exposed relapsed and refractory multiple myeloma patients in the USA. Future Oncol. 2021;17:503–15.
Bruno AS, Wilson JL, Opalinska JM, et al. Recent real-world treatment patterns and outcomes in US patients with relapsed/refractory multiple myeloma. Expert Rev Hematol. 2020;13:1017–25.
Acknowledgements
Funding
Sponsorship for this study and the Journal’s Rapid Service Fee were funded by Janssen Scientific Affairs, LLC and Legend Biotech, Inc.
Medical writing and/or editorial assistance
Medical writing and editorial assistance in the preparation of this article were provided by Melissa Lingohr-Smith and Jay Lin of Novosys Health and was funded by Janssen Scientific Affairs, LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship contributions
All named authors contributed to concept, design and data interpretation. Jinghua He and Alex Z Fu contributed to statistical analyses. All named authors contributed to drafting of the manuscript.
Disclosures
Sundar Jagannath has been or is a consultant to Bristol-Myers Squibb, Janssen Pharmaceuticals, Karyopharm Therapeutics, Legend Biotech, Sanofi, and Takeda. Nedra Joseph, Jinghua He, Concetta Crivera, and Alex Z Fu are employees of Janssen Scientific Affairs, LLC and own company stock. Ashraf Garret is an employee of Legend Biotech and owns company stock. Nina Shah has been or is a consultant to GlaxoSmithKline, Amgen, Indapta Therapeutics, Sanofi, Bristol-Myers Squibb, CareDx, Kite, and Karyopharm, and has received research funding from Celgene/Bristol-Myers Squibb, Janssen, Bluebird Bio, Sutro Biopharma, Teneobio, and Poseida.
Compliance with ethics guidelines
The data sources used in this study (i.e., the IBM® MarketScan® Commercial Claims and Encounters (CCAE) and Medicare Supplemental (MDCR) databases) contain de-identified patient data sets and are fully compliant with the Health Insurance Portability and Accountability Act (HIPAA).
Data availability
All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jagannath, S., Joseph, N., He, J. et al. Healthcare Costs of Multiple Myeloma Patients with Four or More Prior Lines of Therapy, Including Triple-Class Exposure in the United States. Oncol Ther 10, 411–420 (2022). https://doi.org/10.1007/s40487-022-00198-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40487-022-00198-0