Abstract
Angular pregnancy is a rare entity which is commonly confused with interstitial or cornual pregnancies. A lack of consensus about the specific ultrasound features of these 3 entities leads to inappropriate interchange between them among the literature. An angular pregnancy should be considered as a potentially viable intra-uterine eccentric pregnancy as it might be carried to term and result in a live-born baby whereas interstitial or cornual pregnancies should be considered as ectopic pregnancies which should be interrupted. We report here two cases of women at 8 weeks of pregnancy with an angular pregnancy diagnosed by vaginal 2D and 3D ultrasound and discuss about specific ultrasound features and alternative imaging modalities to distinguish it from interstitial and cornual pregnancies.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Angular pregnancy is a rare entity which was initially described in 1898 by Kelly as implantation of the embryo in the endometrial cavity at the superior and lateral angle of the uterine cavity and medially to the utero-tubal junction [1]. Due to its location close to the utero-tubal junction, angular pregnancy is commonly confused with interstitial or cornual pregnancies.
Ectopic pregnancies correspond to pregnancies which are located outside of the endometrial cavity but inside the uterus such as interstitial, caesarean scar or cervical pregnancies. Interstitial pregnancies represent 2–4% of ectopic pregnancies [2, 3]. They are implanted at the origin of the proximal fallopian tube segment in the myometrium and laterally to the round ligament.
“Cornual” pregnancy designs an intrauterine implantation in an abnormal unicornuate, bicornuate, or septate uterus [4] whereas a trophoblastic peripherical implantation in a normal uterus may rather correspond to an “interstitial” or “angular” pregnancy.
A lack of consensus about the specific ultrasound features of these 3 entities leads to inappropriate interchange between them among the literature. Nonetheless, the recent 2020 ESHRE recommendation aims to standardize the terminology to describe embryo site implantation [5, 6].
In this setting, the clinical challenge is to avoid managing an ectopic pregnancy (such as interstitial), as an intrauterine pregnancy (such as angular pregnancy) [7,8,9,10]. Indeed, interstitial pregnancies should be interrupted since it may lead to major complications such as uterine rupture, hemorrhagic shock, and death. By contrast, an angular pregnancy should be considered as a potentially viable intra-uterine eccentric pregnancy and managed expectantly after discussion with the patient [11,12,13] since it might be carried to term [14, 15] with a live-born baby although obstetrical outcomes remains controversial [16, 17].
We report hereby two cases of women who had an 8-week angular pregnancy diagnosed by vaginal 2D and 3D ultrasound and discuss about specific ultrasound features and alternative imaging modalities to distinguish it from interstitial and pregnancies.
Case-report
Case-report 1
A 38-year-old woman, G3P1, was referred to our center by her own practitioner for a second-look ultrasound for a suspicion of ectopic tubal pregnancy. In her history, she had a prior cesarean section eighteen years ago for an unexplained in utero fetal death at 28 weeks, and an early miscarriage in 2020. The current pregnancy was estimated at 8 weeks of gestational age according to the date of her last period. Clinically, she was paucisymptomatic, except for small vaginal bleeding for 3 days. The physical examination was normal. The blood pressure was 125/70 mmHg, the heart rate was 65 bpm and the oxygen saturation was 100%.
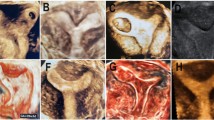
Transvaginal pelvic sonography was performed and did not induce any pelvic pain. The transvaginal 2D revealed an anteverted uterus measuring 110 × 63 × 72 mm, with a 16 × 17 mm anterior intra-mural myoma, and no pelvic fluid in the Douglas’s pouch. There was an evolutive 8w0d-pregnancy with a crown rump length embryo of 16.3 mm and a normal heart activity of 135 bpm. The pregnancy was localized in the uterine upper left angle of the uterus and was fully surrounded by endometrium without any interstitial line sign. Around the gestational sac, a subchorionic hematoma of 25 × 22 × 20 mm was present (Fig. 1 and Supplementary material 1). Considering that the localization remained unclear, a 3D vaginal ultrasound was carried out (Fig. 2 and Supplementary material 2). In the left upper angle of the uterus, the gestational sac was fully surrounded by endometrium, and the myometrial thickness was 3.9 mm (Fig. 3). At the lower part of the gestational sac, the subchorionic hematoma was confirmed. After discussion with the patient about potential evolution and complications, she chose to keep the pregnancy and an expectant strategy was decided. Finally, a miscarriage occurred one week later without any complications.
Case-report 2
The second case was a 37-year-old woman, G2P1. Her ultrasound report was sent to our center for a second look due to peripherical pregnancy localization. In her personal medical history, she had a prior emergency cesarean delivery at 38 weeks for a non-progression of presentation 6 years ago, complicated by a postpartum endometritis. She also had a hysteroscopy two years ago with multiple synechia resection. According to her last period the current pregnancy was estimated at 8 weeks of gestational age. She was clinically asymptomatic; with a blood pressure of 110/60 mmHg, a heart rate of 70 bpm and an oxygen saturation of 100%.
The first 2D and 3D vaginal ultrasound examination did not induce any pain and revealed an 84 × 53 × 75 mm anteverted uterus, no pelvic fluid in the Douglas’s pouch. There was an evolutive 8w3d pregnancy with a crown rump length of 18 mm and a normal heart activity of 160 bpm. The pregnancy was localized in the uterine upper left angle and was fully surrounded by endometrium. The myometrial thickness ranged from 4.0 to 5.7 mm (Fig. 4). After discussion about potential complications the patient chose to keep the pregnancy. Pregnancy viability was assessed each week and the gestational sac localization gradually moved toward the endometrial cavity. Finally, the pregnancy was normally centered in the cavity at 13w0d whereas only the placenta remained fundal and lateralized in the upper left angle. At 37w0d, an emergency cesarean section was done for a suspicion of uterine rupture because of brutal abdominal pain and moderate hemoperitoneum of 200 ml revealed by abdominal tomodensitometry. She gave birth to a 3000 g newborn with a 7–9-10 Apgar score and a good evolution.
During the surgery, no uterine rupture was found but uterine serosa was millimetric on the upper left angle regarding to the placenta position. The surgery was complicated by a massive hemorrhage of 3000 mL, which required successively oxytocin, sulproston, and uterine artery embolization. The patient received 6 red cells units and evolved favorably. At final pathologic examination, a placenta accreta was diagnosed.
Discussion
We reported here two cases of angular pregnancy which were diagnosed by 3D transvaginal ultrasound. This diagnostic is often confused with interstitial pregnancy and this misdiagnosis may lead to unjustified pregnancy termination. Ultrasound features in angular pregnancy are heterogeneous among the literature and most recent cases are summarized in Table 1. One of the main pitfalls is the absence of consensual diagnostic criteria.
To distinguish angular from interstitial pregnancy, Janson and Elliott added a surgical description criteria during laparascopy [16]. In their meta-analysis of 39 cases, angular pregnancy was more likely to induce a lateral uterine enlargement which displaced the round ligament reflection upward and outward whereas interstitial tubal pregnancy was more likely located laterally to the round ligament. They suggested the following clinicosurgical criteria to define angular pregnancy: (1) clinical presentation with painful asymmetric enlargement of the uterus, (2) directly observed (i.e., surgical) lateral distension of the uterus with displacement of the round ligament laterally, (3) retention of the placenta in the uterine angle. However, due to the improvement of ultrasound and other imaging modalities, laparoscopy is not considered anymore as a first-line tool for the diagnosis of ectopic and eccentric pregnancy, including angular pregnancy.
Trimor-Tritsch et al. proposed 3 ultrasound criteria to diagnose interstitial pregnancies: (1) An empty uterine cavity, (2) A chorionic sac seen separately (> 1 cm) from the lateral edge of the uterine cavity, (3) A thin myometrial layer (< 5 mm) surrounding the chorionic sac. The combination of these 3 signs provided a specificity of 88–93% and a poor sensitivity of 40% [18]. In addition, Ackerman et al. (1993) defined the interstitial line sign as an echogenic line in the upper lateral region of the uterus bordering the gestational sac and might correspond to the interstitial portion of the fallopian tube [19]. They reported a 98% specificity, and an 80% sensitivity for the diagnosis of interstitial pregnancy, although only 12 patients were analyzed.
In a review of the literature, Lewiss et al. assessed the sonographic measurement of the endomyometrial mantle as a criterion for diagnosing an abnormal implantation location and concluded to a near-uniform acceptance of less than 5 mm as being highly suspicious for an interstitial pregnancy [2]. By contrast, Bollig and Schust considered that a cut-off < 10 mm as part of an angular pregnancy criteria [17]. In our cases, the smallest myometrial thickness were 3.9 mm and 4.2 mm respectively. Comparing our findings with previous published case-reports, the myometrial thickness cut-off was not precised [7, 9, 12,13,14] or appeared to be heterogeneous with a thickness between 5 and 10 mm [8, 10, 11, 15]. We support the idea that clear standardized recommendations are needed about the cut-off and the myometrial thickness landmarks measurement. As highlighted by our second case, the presence of placental accretism is a frequent event in angular pregnancy due to the reduced thickness of the endometrial decidua in this area.
Recently, the ESHRE society guidelines [6] suggested the following criteria for the interstitial pregnancy diagnosis: (1) a thin intramural/interstitial segment of Fallopian tube adjoining the medial aspect of the gestational sac and the lateral aspect of the uterine cavity” (interstitial line sign). (2) The gestational sac must be at least partially enveloped by the myometrium. These guidelines also individualized a subtype as “partial” interstitial which designs a partial protrusion of the gestational sac from the tubal ostium to the uterine cavity. Performing a sonohysterography by using saline infusion may help to over cross these limitations [20].
In a prospective cohort of 42 patients with angular pregnancy, Bollig and Schust suggested the following criteria: (1) Non anomalous uterus, (2) Implantation of the embryo in the lateral angle of the uterus, (3) < 10 mm of myometrial thickness from the gestational sac to the outer border of the uterus, (4) Completely circumferential endometrium surrounding the gestational sac, (5) Lack of the interstitial line sign [17]. Main differences between interstitial and angular pregnancy ultrasonographic features are summarized in Table 2. In the first case, all these signs were present. The 3D ultrasound was of paramount interest for acquiring an accurate coronal view of the uterus fundus [21] since this imaging modality enhanced to confirm that endometrium was fully surrounded the pregnancy and thus considered as intrauterine. However, ultrasound might be limited by several factors such as interference with intestinal gas, obesity, or operator experience.
In case of unclear situation after performing a vaginal ultrasound, magnetic resonance imaging (MRI) appears to be a suitable alternative as second line exam [22, 23]. MRI presents some advantages: no patient premedication, no ionizing radiation, the possibility of multiplaning imaging, and a really good soft tissue contrast [24]. Nonetheless, gadolinium injection should be avoided since it crosses the placenta. In T2-weighted ponderation sequence, interstitial pregnancy appears as a gestational sac in the uterine angle, with an intact junctional zone between the gestational sac and the endometrial cavity [22].
In our two cases, the lack of the interstitial line sign and the fully surrounded endometrium sign were present. Although these both signs are rarely described in most of recent case-reports (Table 1), they enhanced us to diagnose the angular localization of those pregnancies. These case-reports deserved to underline that these both signs may be more discriminant for angular pregnancy diagnosis than isolated myometrial thickness measurement. Nevertheless, larger prospective cohorts are needed to clarify ultrasonographic features of angular pregnancy.
Despite all these descriptions, diagnosis of angular pregnancy may remain difficult and repeated exams by experienced ultrasonographist and close follow up should be required before considering exploratory laparoscopy.
Conclusion
Angular pregnancy is uncommon, and the eventuality of such unusual localization should be remembered to avoid confusing with cornual and interstitial topography. Those cases highlight the role of the 3D ultrasonography to help for diagnosing angular pregnancy which may be considered as a viable intra-endometrial eccentric pregnancy and may be managed to term.
References
Kelly HA (1898) Operative gynecology. Appleton & Company, New York, p 189
Lewiss RE, Shaukat NM, Saul T (2014) The endomyometrial thickness measurement for abnormal implantation evaluation by pelvic sonography. J Ultrasound Med Off J Am Inst Ultrasound Med 33(7):1143–1146
Arleo EK, DeFilippis EM (2014) Cornual, interstitial, and angular pregnancies: clarifying the terms and a review of the literature. Clin Imaging 38(6):763–770
Jansen R, Elliott P (1983) Angular and interstitial pregnancies should not be called “cornual.” Aust N Z J Obstet Gynaecol 23(2):123–124
(2016) Diagnosis and Management of Ectopic Pregnancy: Green-top Guideline No. 21. BJOG Int J Obstet Gynaecol 123(13):e15–55
ESHRE working group on Ectopic Pregnancy, Kirk E, Ankum P, Jakab A, Le Clef N, Ludwin A et al (2020) Terminology for describing normally sited and ectopic pregnancies on ultrasound: ESHRE recommendations for good practice. Hum Reprod Open. 2020(4):hoaa055
Tarim E, Ulusan S, Kilicdag E, Yildirim T, Bagis T, Kuscu E (2004) Angular pregnancy. J Obstet Gynaecol Res 30:377–379
Kambhampati L, Kitova-John M, Allahdin S, Voigt S (2012) Suction curettage under laparoscopic vision for advanced angular pregnancy. J Obstet Gynaecol 32(6):601–602. https://doi.org/10.3109/01443615.2012.689892
Cordeiro DEF, Alves JAG, Feitosa FEL (2018) Interstitial and angular pregnancies: Case reports and differential diagnosis. J Obstet Gynaecol Res. https://doi.org/10.1111/jog.13748
Katharina Laus MD, Pooja Louis MMS, Laura Douglass MD (2019) A novel approach to management of angular pregnancies: a case series. J Minim Invasive Gynecol 26(178–181):2018
Adam Ash DO, Patrick Ko MD, Christopher Dewar MD, Christopher Raio MD (2010) Eccentrically located intrauterine pregnancy misdiagnosed as interstitial ectopic pregnancy. Am Coll Emerg Physicians. https://doi.org/10.1016/j.annemergmed.2010.04.001
Kwon JY, Hwang SJ, Shin JE, Yoon WS, Shin JC, Park IY (2011) Two cases of angular pregnancy complicated by preterm labor and placental abruption at mid-pregnancy. J Obstet Gynaecol Res 37(7):958–962
Alanbay İ, Öztürk M, Karaşahin KE, Yenen MC (2016) Angular pregnancy. Turk J Obstet Gynecol 13:218–220
Mayer RB, Yaman C, Ebner T, Shebl O, Sommergruber M, Hartl J, Tews G (2012) Ectopic pregnancies with unusual location and an angular pregnancy: report of eight cases. Cent Eur J Med 124:193–197
Marfori CQ, Kotzen M (2018) Angular vs. interstitial pregnancy: a case report highlighting diagnostic nuances with stark management differences. 2214-9112/© 2018 Published by Elsevier
Jansen RP, Elliott PM (1981) Angular intrauterine pregnancy. Obstet Gynecol 58(2):167–175
Bollig KJ, Schust DJ (2020) Refining angular pregnancy diagnosis in the first trimester: a case series of expectant management. Obstet Gynecol 135(1):175–184
Timor-Tritsch IE, Monteagudo A, Matera C, Veit CR (1992) Sonographic evolution of cornual pregnancies treated without surgery. Obstet Gynecol 79(6):1044–1049
Ackerman TE, Levi CS, Dashefsky SM, Holt SC, Lindsay DJ (1993) Interstitial line: sonographic finding in interstitial (cornual) ectopic pregnancy. Radiology 189(1):83–87
Liao C-Y (2018) Distinguishing between interstitial and angular pregnancies: is there a role for saline infusion sonohysterography? Taiwan J Obstet Gynecol 57(4):605–607
Benacerraf BR (2019) Three-dimensional volume imaging in gynecology. Obstet Gynecol Clin North Am 46(4):755–781
Srisajjakul S, Prapaisilp P, Bangchokdee S (2017) Magnetic resonance imaging in tubal and non-tubal ectopic pregnancy. Eur J Radiol 93:76–89
Ramanathan S, Raghu V, Ladumor SB, Nagadi AN, Palaniappan Y, Dogra V et al (2018) Magnetic resonance imaging of common, uncommon, and rare implantation sites in ectopic pregnancy. Abdom Radiol N Y 43(12):3425–3435
Masselli G, Brunelli R, Casciani E, Polettini E, Bertini L, Laghi F et al (2011) Acute abdominal and pelvic pain in pregnancy: MR imaging as a valuable adjunct to ultrasound? Abdom Imaging 36(5):596–603
Funding
Open access funding provided by University of Lausanne.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Patient consent
Written informed consent was obtained from patients for the publication of these case reports and accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 5148 KB)
Supplementary file2 (MP4 1146 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Durand, Y.G., Capoccia-Brugger, R., Vial, Y. et al. Diagnostic dilemma between angular and interstitial ectopic pregnancy: 3D ultrasound features. J Ultrasound 25, 989–994 (2022). https://doi.org/10.1007/s40477-022-00668-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-022-00668-1