Abstract
Purpose
Ultrasound is a non-invasive quantitative method to characterize sonographic textures of skeletal muscles. To date, there is no information available on the trapezius muscle. This study assessed the trapezius muscles of patients with myofascial pain compared with normal healthy participants.
Methods
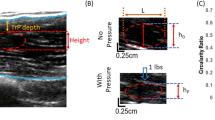
The trapezius muscles of 15 healthy and 17 myofascial pain participants were assessed using B-mode ultrasound to obtain 120 images for healthy and 162 images from myofascial pain participants. Texture features such as blob area, count and local binary patterns (LBP) were calculated. Multi-feature classification and analysis were performed using principal component analysis (PCA) and MANOVA to determine whether there were statistical differences.
Results
We demonstrate the two principal components composed of a combination of LBP and blob parameters which explain 92.55% of the cumulative variance of our data set. In addition, blob characteristics were significantly different between healthy and myofascial pain participants.
Conclusion
Our study provides evidence that texture analysis techniques can differentiate between healthy and myofascial pain affected trapezius muscles. Further research is necessary to evaluate the nature of these differences.
Sommario
Obiettivi
L’ecografia è un metodo quantitativo non invasivo utile per caratterizzare la texture sonografica dei muscoli scheletrici. Allo stato attuale, vi sono pochi dati in letteratura riguardo il muscolo trapezio. Questo studio ha valutato i muscoli trapezi dei pazienti con dolore miofasciale confrontandoli con quelli dei soggetti sani.
Metodi
L’ecografia B-mode è stata utilizzata per valutare i muscoli trapezi di 15 soggetti sani e di 17 pazienti con dolore miofasciale , ottenendo 120 immagini per i soggetti sani e 162 per i pazienti con dolore miofasciale. Sono state calcolate caratteristiche di texture come la blob area, i count ed i local binary pattern (LBP). La classificazione e l'analisi multiparametrica sono state eseguite utilizzando l'analisi delle componenti principali (PCA) e MANOVA per valutare se vi fossero differenze statistiche.
Risultati
Abbiamo dimostrato che due componenti principali, composte da una combinazione di LBP e parametri blob, spiegano il 92.55% della varianza cumulativa dei nostri dati. Inoltre, le caratteristiche blob erano significativamente differenti tra i pazienti con dolore miofasciale ed i soggetti sani.
Conclusioni
Il nostro studio fornisce l’evidenza che le tecniche di texture analysis possono differenziare i muscoli trapezi dei soggetti sani da quelli dei pazienti affetti da dolore miofasciale. Ulteriori studi sono necessari per valutare la natura di tali differenze.




Similar content being viewed by others
References
Harden RN, Bruehl SP, Gass S, Niemiec C, Barbick B (2000) Signs and symptoms of the myofascial pain syndrome: a national survey of pain management providers. Clin J Pain 16(1):64–72
Gerwin RD (2001) Classification, epidemiology, and natural history of myofascial pain syndrome. Curr Pain Headache Rep 5(5):412–420
Skootsky SA, Jaeger B, Oye RK (1989) Prevalence of myofascical pain in general internal medicine practice. Retrieved From West J Med 151(20):157–160
Fishbain DA, Goldberg M, Meagher BR, Steele R, Rosomoff H (1986) Male and female chronic pain patients categorized by DSM-III psychiatric diagnostic criteria. Pain 26(2):181–197
Fleckenstein J, Zaps D, Ruger LJ, Lehmeyer L, Freiberg F, Lang PM, Irnich D (2010) Discrepancy between prevalence and perceived effectiveness of treatment methods in myofascial pain syndrome: results of a cross-sectional, nationwide survey. BMC Musculoskelet Disord 11:32
Mourtzakis M, Wischmeyer P (2014) Bedside ultrasound measurement of skeletal muscle. Curr Opin Clin Nutr Metab Care 17:389–395
Shirley IM, Blackwell R, Cusick G, Farman DJ, Vicary FR (1988) Ultrasound. In: Shirley IM, Blackwell R, Cusick G, Farman DJ, Vicary FR (eds) A user’s guide to diagnostic ultrasound. Pitman Medical Publishing Co LtD, London, pp 32–39
Heckmatt JZ, Leeman S, Dubowitz V (1982) Ultrasound imaging in the diagnosis of muscle disease. J Pediatr 101:656–660
Scholten RR, Pillen S, Verrips A, Zwarts MJ (2003) Quantitative ultrasonography of skeletal muscles in children: normal values. Muscle Nerve 27:693–698
Pillen S, van Keimpema M, Nievelstein RA, Verrips A, Kruijsbergen-Raijmann W, Zwarts MJ (2006) Skeletal muscle ultrasonography: visual versus quantitative evaluation. Ultrasound Med Biol 32:1315–1321
Arts IMP, Pillen S, Schelhaas HJ, Overeem S, Zwarts MJ (2010) Normal values for quantitative muscle ultrasonography in adults. Muscle Nerve 41:32–41
Jensen BR, Bakke M (1998) Prolonged work with shoulder muscles and other small muscle groups: use, function, and pain. In: Capodaglio P, Narici MV (eds) Muscle atrophy: disuse and disease. Le Collane della Fondazione Salvatore Maugeri, Pavia, pp 149–161
Nielsen PK, Jensen BR, Darvann T et al (2006) Quantitative ultrasound tissue characterization in supraspinatus and thigh muscles—a new approach. BMC Musculoskel Disord 7:2–13
Pillen S (2010) Skeletal muscle ultrasound. Eur J Transl Myol 20(4):145–156
Rivers WE, Garrigues D, Graciosa J, Harden RN (2015) Signs and symptoms of myofascial pain: an international survey of pain management providers and proposed preliminary set of diagnostic criteria. Pain Med 16(9):1794–1805
Gerwin RD (2014) Diagnosis of myofascial pain syndrome. Phys Med Rehabil Clin N Am 25(2):341–355
Tough EA, White AR, Richards S, Campbell J (2007) Variability of criteria used to diagnose myofascial trigger point pain syndrome—evidence from a review of the literature. Clin J Pain 23:278–286
Turo D, Otto P, Shah JP, Heimur J, Gebreab T, Zaazhoa M, Armstrong K, Gerber LH, Sikdar S (2013) Ultrasonic characterization of the upper trapezius muscle in patients with chronic neck pain. Ultrason Imaging 35:173–187
Shah JP, Thaker N, Heimur J, Aredo JV, Sikdar S, Gerber L (2015) Myofascial trigger points then and now: a historical and scientific perspective. PM&R 7(7):746–761
Simons DG, Travell JG, Simons PT (1999) Travell and Simon’s myofascial pain and dysfunction: the trigger point manual, vol 1, 2nd edn. Williams and Wilkins, Baltimore
McDermid J, Gross AR, Galea V, McLaughlin LM, Parkinson W, Woodhouse L (2009) Developing biologically based assessment tools for physical therapy management of neck pain. J Orthop Sports Phys Ther 39(5):388–399
Nielsen PK, Jensen BR, Darvann T, Jørgensen K, Bakke M (2000) Quantitative ultrasound image analyses of the supraspinatus muscle. Clin Biomech 15(Suppl 1):S13–S16
Lindeberg T (1991) Discrete scale-space theory and the scale-space primal sketch (Doctoral dissertation, KTH Royal Institute of Technology)
Ojala T, Pietikäinen M, Harwood D (1996) A comparative study of texture measures with classification based on featured distributions. Pattern Recogn 29(1):51–59
Ojala T, Pietikainen M, Maenpaa T (2002) Multiresolution gray-scale and rotation invariant texture classification with local binary patterns. IEEE Trans Pattern Anal Mach Intell 24(7):971–987
Myburgh C, Lauridsen HH, Larsen AH, Hartvigsen J (2011) Standardized manual palpation of myofascial trigger points in relation to neck/shoulder pain; the influence of clinical experience on inter-examiner reproducibility. Man Ther 16(2):136–140
Rathbone AT, Grosman-Rimon L, Kumbhare DA (2017) Interrater agreement of manual palpation for identification of myofascial trigger points. Clin J Pain 33(8):715–729
Pillen S, Arts IM, Zwarts MJ (2008) Muscle ultrasound in neuromuscular disorders. Muscle Nerve 37(6):679–693
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors and author institutions have no conflict of interest to declare. This includes financial or personal relationships, dual commitments, competing interests or competing loyalties.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumbhare, D., Shaw, S., Ahmed, S. et al. Quantitative ultrasound of trapezius muscle involvement in myofascial pain: comparison of clinical and healthy population using texture analysis. J Ultrasound 23, 23–30 (2020). https://doi.org/10.1007/s40477-018-0330-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-018-0330-5