Abstract
Purpose of Review
The COVID-19 pandemic and its associated restrictions have had a significant impact on people’s everyday lives, including the lives of Autistic adults. We aimed to (a) synthesise all papers currently published on the impact of the COVID-19 pandemic on autistic adults and (b) identify lessons for the care and support of Autistic adults in pandemic and post-pandemic times.
Recent Findings
Fifty-five papers met the inclusion criteria. Most studies focused on the pandemic’s impact on the wellbeing of Autistic adults. Several studies focused on the use of (telehealth) services or the risk of COVID-19 infection/hospitalisation.
Summary
Autistic adults were significantly impacted by the pandemic, both directly as indicated by higher COVID-19 infection and hospitalisation rates, but also indirectly due to severe service disruptions and social restrictions. Even though there were large differences observed both between as well as within individuals in terms of the negative/positive effects of the COVID-19 pandemic, most studies reported a negative effect on Autistic adults’ mental health. We draw several lessons from this review for the future care and support of Autistic adults, all of which must be underpinned by participatory research methods, that is, where Autistic community members are actively involved in setting research questions, testing the acceptability of the methods and interpreting and disseminating the results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The catastrophic impacts — both direct and indirect — of the COVID-19 pandemic on the lives of millions of people across the world are becoming increasingly clear. Some of these impacts have been the direct consequence of the virus itself, including a significant rise in serious acute ill-health and early death, to which disabled people [1], including Autistic people,Footnote 1 may have been particularly at risk [5, 6]. Other impacts have been caused by the measures put in place to try to curb the spread of the virus, including restricted access to face-to-face health and other social services; the closure of schools and other educational institutions; and the frequent requirement for people to stay at, and work from, home to dramatically constrain their physical and social interactions — measures that have varied substantially across and within regions [7]. Some of these measures may have had occasional positive effects above and beyond their impact on slowing the spread of the virus [8]. Yet, there are good reasons to believe that these measures imposed a particularly heavy burden on Autistic people [5, 6], especially as this group is at greater risk of experiencing mental health problems [9, 10] and may depend significantly on formal and informal support from others to maintain quality of life.
The current scoping review sought to synthesise evidence of the impact of the COVID-19 pandemic on the lives of Autistic adults. We focus on Autistic adults specifically given that they are an under-represented group in current autism research [11, 12]; are more likely to have co-occurring physical and mental health conditions [10, 13•], which place them at risk of health complications following COVID-19 infection; and have poorer life outcomes across many domains, often due to systemic and social failures to provide the requisite support [14].
Method
We addressed the following research questions:
-
1.
What has been the impact of the COVID-19 pandemic on Autistic adults?
-
2.
Which individual and/or contextual factors during the COVID-19 pandemic are associated with a more positive outcome for Autistic adults?
Based on research on the impact of the pandemic, we sought to identify lessons for the future care and support of Autistic adults. The review protocol was registered on Open Science Framework (https://doi.org/10.17605/OSF.IO/B73QN).
Eligibility Criteria
We used the following criteria to determine study eligibility:
-
1.
An empirical quantitative and/or qualitative study on the impact of the COVID-19 pandemic and its associated restrictions on the mental health or wellbeing of at least one Autistic adult (> 18 years), based on self-report and/or observation/proxy-report. Autistic adult(s) should be mentioned explicitly in the paper’s “Method” section.
-
2.
The sample should consist of adult(s) with a clinical diagnosis of autism or who self-identify as Autistic, and/or consists of informants for the Autistic adults. In cases where the sample also included Autistic children (< 18 years) or people with diagnoses other than autism (e.g. intellectual disability), the study is included only where Autistic adults’ data (a) are described separately in the paper or (b) make up ≥ 50% of the total sample.
-
3.
English language.
-
4.
Published in a peer-reviewed journal or as a pre-print on a pre-print service provider.
Search Strategy
On 24–25th May 2022, we searched through the electronic databases of PubMed, EMBASE, CYNAHL, Psychinfo and Science Citation Index (Web of Science) using the following search terms: [1] COVID-19 OR coronavirus OR SARS-CoV-2 OR pandemic AND [2] autis* OR developmental disorder AND [3] adult. Additionally, we searched through the major autism-related journals, including Autism, Autism Research, Journal of Autism and Developmental Disorders, Molecular Autism, Autism in Adulthood, Research in Autism Spectrum Disorders and Research in Developmental Disabilities using the following search terms: [1] COVID-19 OR coronavirus OR SARS-CoV-2 OR pandemic AND [2] adult. On 8th August 2022, we screened the same databases and journals for any newly published journal articles or pre-prints in the period from 26th May to 8th August.
Data Extraction
Table 1 shows key information extracted from eligible papers (where available).
Results
Study Selection
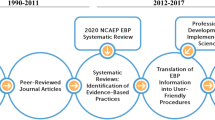
During the initial search (May 2022), we identified 747 abstracts. All abstracts were screened for eligibility by AMS. Almost half (n = 337; 45%) were independently screened by both AMS and LC, for which there was excellent inter-rater agreement (98%). Disagreements (n = 6; 2%) were resolved by discussion. Of the 747 abstracts, we selected 105 (14%) for a full paper read. The same two researchers read all 105 papers to determine final eligibility. Disagreements (n = 6 papers; 6%) were resolved through discussion, leading to a final selection of 47 (45%) papers. During the second search (August 2022), we identified an additional eight eligible papers, yielding a final list of 55 studies (see Fig. 1 [15, 16]).
Critical Appraisal
We assessed the quality of eligible studies using the Mixed Methods Appraisal Tool (MMAT, [17]). Each study was assessed in terms of five methodological quality criteria, which differed according to study methodology (quantitative, qualitative and mixed-methods). For each item, the study was rated ‘yes meets criteria’, ‘no does not meet criteria’ or ‘can’t tell’, where relevant information was not reported. EP rated all eligible studies (n = 55), half of which (n = 27; 49%) were independently coded by MH, with excellent agreement (88%) (LC rated papers for which EP and MH were also authors). Disagreements were discussed and resolved by consensus. The MMAT discourages allocating a numerical score, preferring a narrative description of a paper’s quality (see Supplementary Table 1). No studies were excluded based on their MMAT assessment, but study quality is applied in the interpretation of the findings.
Study Themes and Types
We categorised the 55 eligible papers as follows: 1) direct effects of the COVID-19 virus on Autistic adults including infection risk, hospitalisation, death and vaccination rates (n = 10); 2) effects of COVID-19 restrictive measures on care, support and services for Autistic adults (n = 11); 3) COVID-19-related effects on the wellbeing of Autistic adults (n = 32); and 4) other (n = 2) (see Table 1). Of the 55 studies, 30 (55%) were quantitative, 13 qualitative (24%) and 12 reported mixed-methods (22%). Thirty-five studies (64%) were, at least partly, based on Autistic adults’ self-reports, 10 (18%) on proxy-reports (caregivers or clinicians) and the remaining 10 (18%) on secondary analyses of medical/insurance databases. Eighteen studies (33%) included a non-autistic comparison group. Thirteen studies (24%) included data collected prior to pandemic onset. Most studies (n = 34; 62%) did not report on Autistic community involvement in the research process, and of those studies that did, most reported modest (n = 11; e.g. review of the survey) or no (n = 2) involvement of community members (see Table 1). In eight studies (15%), it was reported that Autistic researchers contributed to the research.
Demographic Data
Most included studies took place predominantly in the USA (n = 13; 24%) and the UK (n = 12; 22%), followed by Italy (n = 5; 9%) and Australia (n = 4; 7%). Thirty-one studies (56%) collected data in (multiple) European countries (including the 17 UK and Italian studies). Three studies took place in Israel, one in Canada, one in South-Africa, one in Turkey and one in Hong Kong (China). No studies presented data on Autistic adults in Central or South-America. Most (n = 34; 62%) collected data at least partly between March and May 2020 (i.e. during the earliest phase of the COVID-19 pandemic and before COVID-19 vaccines were available). The following policy rules applied in most jurisdictions during this time, although their implementation and enforcement varied substantially [7]: physical distancing; wearing face masks; disinfecting hands; cancellation of public events; restriction of international travel; closure of schools, non-essential shops, and restaurants and staying at, and working from, home. Seventeen studies (32%) collected data during a later phase, and three studies did not report timing of data collection. One study, examining risk for COVID-19 infection [13•], based their conclusions solely on pre-pandemic data.
Only nine studies (16%) focussed, at least in part, on Autistic adults with intellectual disability [13•, 18, 19, 20, 21, 22, 23, 24, 25]. For the 35 studies (64%) including Autistic adults’ self-report data, it is likely that participating adults did not have a co-occurring intellectual disability, since self-report requires the ability to understand and respond to questions (orally or in writing), usually without support. The male-to-female gender/sex ratio varied greatly across studies, with the lowest proportion of women (17%) in an employment study [26] and the highest proportion (94%) in a study with Autistic parents [27]. In studies including self-reports (n = 35), there was a preponderance of Autistic females (either female gender and/or sex) with 19 (54%) sampling > 50% Autistic females. In the 20 studies without any direct participation by Autistic adults (e.g. through the use of proxy-reports or medical records), the highest proportion of Autistic females was 39% [22] (excluding one study, where the single Autistic participant was female [25]). In 12 of 55 studies (22%), Autistic adults’ gender/sex was not reported, mostly because either professionals were the primary informant [28, 29, 30] or the sex ratio was described only for a larger group of participants with an intellectual or developmental disability (IDD) [18, 31].
What Has Been the Impact of the COVID-19 Pandemic on Autistic Adults?
Direct Effects of the COVID-19 Virus
A large-scale study in Israel (n = 32,812; 44% ≥ 16 years) reported that Autistic adults were two times more likely to be infected by COVID-19, compared to sex- and age-matched adults and also two times more likely to develop serious illness, resulting in higher hospitalisation rates [32]. Similarly, Autistic adult COVID-19 patients in the USA — just like those with an IDD — were shown to have a higher risk of Intensive Care Unit admittance and a significantly longer hospital stay, compared to their baseline group of COVID-19 patients without an IDD [33]. The causes for higher infection rates and more severe outcomes among Autistic versus non-autistic adults are not definitive but appear to be linked to contextual factors (e.g. living in a residential facility, receiving services in the home from outside caregivers) [13•, 18].
A review of COVID-19 policies in multiple European countries [34] demonstrated that, despite concerns about an increased risk, most countries did not prioritize COVID-19 testing for Autistic people. Furthermore, survey data showed that 55% of Autistic adults and 51% of caregivers of Autistic adults reported that reasonable adjustments to COVID-19 testing (e.g. a support person or sensory accommodations) were not made possible [34]. Moreover, it appears that Autistic people with an intellectual disability may have been discriminated against, as some countries used cognitive impairments as an exclusion criterion for Intensive Care Unit admittance in case of triage [34].
Given Autistic adults’ increased risk of infection, some advocates called for prioritization of COVID-19 vaccination in this group. During the early phase of a mass vaccination campaign in Israel, Autistic adults were reported as being more likely to be vaccinated, compared to a sex- and age-matched comparison group, particularly in the 21–40 age group (Autistic: 62%; non-autistic: 29%; [35]). In a US-based study, most Autistic adults (78%) were said to have had received or planned to get a COVID-19 vaccine [36].
In sum, Autistic adults appear to be at increased risk for COVID-19 infection and show poorer outcomes following infection compared to non-autistic adults. Despite this risk, COVID-19 testing has not been prioritized for this group. Given that only two studies in this review reported about COVID-19 vaccinations for Autistic adults, it remains uncertain whether COVID-19 vaccinations were consistently prioritized.
Impact on Services and Supports
Autistic adults, caregivers and professionals reported major disruption of services for themselves or those they supported during the COVID-19 pandemic [29, 34, 37]. The barriers to accessing healthcare, which were already excessive for many Autistic people prior to the pandemic [38, 39, 40], were deemed even greater during the pandemic [41•]. Due to physical distancing and stay-at-home orders, many services shifted to remote delivery to ensure continuity of care. Experiences of so-called ‘telehealth’ services varied substantially, linked to the nature of the service. Telehealth services were reported to be an acceptable alternative to in-person service delivery for primary care [42] and diagnostic assessments [43], largely because virtual appointments can minimise barriers to care for Autistic adults (e.g. less stress negotiating travel and waiting rooms; [39]). Yet, remote mental health services were not accepted or preferred by everyone [44••, 45, 46] and were advised against in cases of high psychological distress or intellectual disability [41•]. Autistic adults who accessed remote mental health services reported challenges with sensory issues [44••, 46], body awareness [44••, 46], technological issues [41•, 42, 43, 46] and effective communication with their therapist [44••, 46]. Some reported experiencing discontinuity of care as a result [46], and those who felt they did not benefit from telehealth services early in the pandemic were more likely to experience mental health distress 2 months later, compared to those who felt they benefited [47•]. These mixed findings suggest that, even though telehealth services may be an acceptable and welcome alternative for some Autistic adults, the specific nature of service delivery should depend on individual preference.
Impact on Wellbeing
Of the 32 studies examining the pandemic’s effects on wellbeing, 13 (41%) were quantitative, 10 (31%) qualitative and nine (28%) used a combination of qualitative and quantitative methodologies. Most studies assessed the pandemic’s effects on the wellbeing of Autistic adults (either via self-report or proxy-report) in a retrospective way, that is, by asking participants to reflect on and estimate the impact of the pandemic, compared to their memory of pre-pandemic experience. Almost all retrospective studies indicated an overall decrease in wellbeing during the pandemic. Only 10 (31%) studies were prospective, where the wellbeing of Autistic adults was assessed repeatedly over time. These prospective studies revealed mixed experiences, demonstrating either overall stability of psychopathology symptoms, loneliness and stress in Autistic adults during the first months of the pandemic [47•, 48, 49], an overall decrease in psychopathology symptoms [44••] or an increase in acute psychiatric distress, as evidenced by increased psychiatric emergency admissions of Autistic adults before and during lockdown [50].
Perhaps unsurprisingly, there were large individual differences reported within these prospective studies, even for those reporting negligible overall effects — suggesting that, for some Autistic adults, the COVID-19 pandemic and its restrictions may have had positive effects on their wellbeing, while for others, it had negative effects. This variability was confirmed by studies adopting in-depth qualitative retrospective approaches, which also revealed potential reasons for this variability. Most studies reported differences between individuals, with some Autistic adults highlighting benefits of the restrictions (e.g. relief of pressures from the external world, control over sensory stimulation, ability to spend quality time with family) and others reporting serious and damaging effects of these same restrictions (e.g. loss of social contacts and friendships, no access to professional support, and loss of independence) [44••, 45, 46, 51, 52••]. Unsurprisingly, some of these studies also reported substantial differences within individuals, with some Autistic adults experiencing both positive and negative effects of the stay-at-home orders at different points during the pandemic [27, 44••, 46, 52••, 53]. This latter finding might provide one explanation for the apparent stability in psychological wellbeing reported by several prospective, quantitative studies [47•, 48, 49]. Another possibility is that such stability is driven more by the consistently deeply unsatisfactory quality of life and poor mental health experienced by many Autistic adults pre-pandemic (see [14], for review) than the impact of the pandemic itself.
Which Individual and/or Contextual Factors During the COVID-19 Pandemic Are Associated with a More Positive Outcome for Autistic Adults?
Individual Factors
Many studies identified individual characteristics that were reportedly predictive of better mental health in Autistic adults during the pandemic, including being male gender/sex [47•, 49], older [47•, 48], having relatively good mental health prior to the pandemic [44••, 47•, 48, 49], low COVID-19-related stress [27, 48, 49], high perceived social support [46, 48, 52••] and being able to maintain routines or develop new ones [44••, 52••, 54]. Caution is warranted, however, as these effects (particularly regarding gender/sex and age) were not consistently replicated [44••, 48].
Contextual Factors
There were several contextual factors that appear to have had a positive effect on Autistic people’s mental health or wellbeing during the pandemic, including (continued) access to (professional) support [27, 44••, 52••, 53], reduced pressure to conform to societal rules [27, 46, 51, 53], reduced sensory overload or greater control over the sensory environment [44••, 52••, 55], absence of COVID-19 infection [47•], strong social connections and activities (including maintaining contact with friends, family and community online) [44••, 46] and clear and accessible public health messaging with regard to COVID-19-related information and rules [52••]. Societal inclusion and acceptance are also likely protective factors of Autistic adults’ mental health in general [53].
Discussion
Through our scoping review, we have demonstrated that Autistic adults are likely to have been disproportionately impacted by the COVID-19 pandemic in several ways: [1] they were at increased risk of contracting COVID-19 and developing serious illness; [2] they often struggled to access critical services and supports as a result of stay-at-home restrictions implemented in many jurisdictions; and [3] despite some positive uplift due to reduced external pressures, many experienced challenges to their mental health — particularly those who were female, had pre-existing mental health issues and had limited social connections and support. These findings are consistent with the pandemic’s detrimental effects on disabled people more broadly, referred to as the “triple jeopardy” [1].
While these findings are already deeply concerning, our review likely significantly underestimates the negative impact of COVID-19 on Autistic adults’ health and wellbeing, since most reviewed studies relied on selective samples. For instance, almost all studies were conducted in high-income countries, meaning we know virtually nothing of the experiences of Autistic adults residing in low- and middle-income countries, many of whom may be undiagnosed and with limited or no access to appropriate mental health care [56, 57]. We also know little of the experiences of Autistic adults from seldom-heard groups in autism research, including those who face economic hardship, are of minority racial/ethnic backgrounds, use non-traditional forms of communication, and/or have an intellectual disability. Autistic adults identifying with one or more of these groups were vastly under-represented in the studies we identified, which makes it difficult to draw conclusions about their experiences of COVID-19. It is likely, however, that those who are multiply marginalized and those living in low- and middle-income countries will have responded far worse than the identified studies suggest.
Aside from the sampling issues outlined above, many of the identified studies were also of relatively poor methodological quality. While there was an urgent need to understand the impact of COVID-19 on the Autistic and autism communities, many studies relied, often for logistical and practical reasons, on retrospective designs as well as measures of often questionable reliability, validity and generalisability. For instance, several studies relied on bespoke rating scales, single items or failed to report a measure’s reliability within an Autistic sample (see also Supplementary Table 1). Many studies also did not account for potential confounding factors, especially the extent and nature of COVID-19-related restrictions at the time of study. Despite clear research recommendations formulated early on in the pandemic [58], concerns regarding the scientific rigor of the COVID-19 literature are not limited to autism research [59, 60]. Such concerns are worrying nevertheless because conclusions based on less-than-sound science can pose significant challenges to clinical and policy-relevant decision making and may also reduce trust in autism science.
Our review may also be limited in other ways. We acknowledge that our search strategies may not have been exhaustive, especially regarding the exclusion of non-English language studies, and that our review included several studies of our own, which may have increased the risk of bias. It also may have over-represented issues faced during the first phase of the pandemic (likely due to lags between study completion and publication), rendering it important to examine later and long-term impacts of COVID-19 and its associated restrictions. Further limitations of the reviewed studies likely transcend the pandemic situation. For example, level of community involvement was rarely reported or was very modest (e.g. questionnaire review), indicating many missed opportunities to actively learn from and be guided by the needs and expertise of the Autistic community [58]. Such opportunities may have been particularly pertinent during the unprecedented pandemic situation.
Lessons Learned
Despite the aforementioned concerns, there are several important lessons we can draw from this review on the future care and support of Autistic adults. First, Autistic adults have been disproportionately affected by the COVID-19 pandemic — both by the effects of the virus itself and the social measures used by governments to curtail it. We therefore need a distinct strategy to support Autistic adults during times of crisis and beyond. Such a strategy must be deeply informed by, and actively co-produced with, the Autistic community to ensure it is responsive, respectful and relevant to Autistic adults’ lives.
Second, continued access to effective, knowledgeable and tailored care and services was vital for Autistic adults’ wellbeing during the pandemic. We need greater investment in the development — and rigorous testing — of services and supports that are tailored to the needs, preferences and abilities of individual Autistic adults, particularly those that optimise the person-environment fit [61]. Autistic adults should also be actively involved in making decisions about specific, formal supports (in terms of personnel and delivery) and be able to shape the systems and policies enabling access to these supports, even during health crises.
Third, although our review revealed much variability in the extent and nature of the impact of the pandemic on Autistic adults’ mental health, many experienced acute loneliness and social isolation, with some reporting severe mental health distress. This finding challenges prevailing stereotypes of autism — that is, that Autistic people prefer a life of self-isolation. In future, more concerted efforts, ideally led by Autistic-led organisations, must be made to implement and maintain social support structures for the Autistic community [46, 48], especially during times when social supports are otherwise curtailed.
Finally, few studies in our review reported actively including Autistic adults or their allies in the research process. Participatory autism research is still in its infancy, with researchers often reporting that it can be time-consuming and challenging [62]. The pandemic may well have exacerbated these challenges [63]. Researchers should seek to deepen their involvement with the Autistic community so that they can respond rapidly and flexibly in time of crises such as this one. Doing so will ensure that future research, clinical services and care are aligned with the needs and priorities of Autistic people [27], accelerate translational research and enable Autistic people to have their perspectives and experiences fully taken into account.
Data Availability
Data are available upon reasonable request.
Notes
In the autistic community, identity-first language e.g. ‘autistic person’, is often preferred to, and considered less stigmatizing than, person-first language e.g. ‘person with autism’ (2–3; although see 4). We therefore use identity-first language throughout this paper. We also use ‘Autistic’ with a capital A. Similar to the Deaf community, many autistic adults spell Autistic with a capital A to emphasise their belonging to a shared community and to recognise their struggles to achieve acceptance and social justice.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shakespeare T, Ndagire F, Seketi QE. Triple jeopardy: disabled people and the COVID-19 pandemic. Lancet. 2021;397(10282):1331–3.
Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016;20(4):442–62.
Gernsbacher MA. Editorial perspective: the use of person-first language in scholarly writing may accentuate stigma. J Child Psychol Psychiatry. 2017;58(7):859–61.
Buijsman R, Begeer S, Scheeren AM. ‘Autistic person’ or ‘person with autism’? Person-first language preference in Dutch adults with autism and parents. Autism. 2022;136:13623613221117914.
den Houting J. Stepping out of isolation: autistic people and COVID-19. Autism in Adulthood. 2020;2(2):103–5.
Pellicano E, Stears M. The hidden inequalities of COVID-19. Autism. 2020;24(6):1309–10.
Han Q, Zheng B, Cristea M, Agostini M, Bélanger JJ, Gützkow B, et al. Trust in government regarding COVID-19 and its associations with preventive health behaviour and prosocial behaviour during the pandemic: a cross-sectional and longitudinal study. Psychological Medicine. 2021:1–11.
Stock S, Bu F, Fancourt D, Mak HW. Longitudinal associations between going outdoors and mental health and wellbeing during a COVID-19 lockdown in the UK. Sci Rep. 2022;12(1):10580.
Hollocks MJ, Lerh JW, Magiati I, Meiser-Stedman R, Brugha TS. Anxiety and depression in adults with autism spectrum disorder: a systematic review and meta-analysis. Psychol Med. 2019;49(4):559–72.
Lai MC, Kassee C, Besney R, Bonato S, Hull L, Mandy W, et al. Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(10):819–29.
Jang J, Matson JL, Adams HL, Konst MJ, Cervantes PE, Goldin RL. What are the ages of persons studied in autism research: a 20-year review. Res Autism Spectr Disord. 2014;8(12):1756–60.
Nicolaidis C. Autism in adulthood: the new home for our emerging field. Autism Adulthood. 2019;1(1):1–3.
• Schott W, Tao S, Shea L. COVID-19 risk: Adult Medicaid beneficiaries with autism, intellectual disability, and mental health conditions. Autism. 2021;26(4):975–87 This insurance database study identified an increased COVID-19 risk among Autistic adults.
Pellicano E, Fatima U, Hall G, Heyworth M, Lawson W, Lilley R, et al. A capabilities approach to understanding and supporting autistic adulthood. Nat Rev Psychol. 2022;1(11):624–39.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372: n160.
Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459–67.
Hansford R, Ouellette-Kuntz H, Martin L. Short report: the influence of congregate setting on positive COVID-19 tests among a high-risk sample of adults with intellectual and developmental disability in Ontario. Res Dev Disabil. 2022;122: 104178.
Levante A, Petrocchi S, Colombi C, Keller R, Narzisi A, Masi G, et al. The effect of sleep-wake routines on the negative emotional states and aggressive behaviors in adults with autism spectrum disorders (ASD) during the COVID-19 outbreak. Int J Environ Res Public Health. 2022;19(9):4957.
Mupaku WM, Breda AD, Kelly B. Transitioning to adulthood from residential childcare during Covid-19: experiences of young people with intellectual disabilities and/or autism spectrum disorder in South Africa. Br J Learn Disabil. 2021;9(3):341–51.
Brondino N, Bertoglio F, Forneris F, Faravelli S, Borghesi A, Damiani S, et al. A pilot study on covid and autism: prevalence, clinical presentation and vaccine side effects. Brain Sci. 2021;11(7):860.
Brondino N, Damiani S, Politi P. Effective strategies for managing COVID-19 emergency restrictions for adults with severe ASD in a daycare center in Italy. Brain Sci. 2020;10(7):463.
Perera B, Laugharne R, Henley W, Zabel A, Lamb K, Branford D, et al. COVID-19 deaths in people with intellectual disability in the UK and Ireland: descriptive study. BJPsych Open. 2020;6(6):123.
Nollace L, Cravero C, Abbou A, Mazda-Walter B, Bleibtreu A, Pereirra N, et al. Autism and COVID-19: a case series in a neurodevelopmental unit. J Clin Med. 2020;9(9):1–11.
Vereijken FR, Giesbers SAH, Jahoda A, Embregts P. Homeward bound: exploring the motives of mothers who brought their offspring with intellectual disabilities home from residential settings during the COVID-19 pandemic. J Appl Res Intellect Disabil. 2022;35(1):150–9.
Goldfarb Y, Gal E, Golan O. Implications of employment changes caused by COVID-19 on mental health and work-related psychological need satisfaction of autistic employees: a mixed-methods longitudinal study. J Autism Dev Disord. 2022;52(1):89–102.
Heyworth M, Brett S, den Houting J, Magiati I, Steward R, Urbanowicz A, et al. “I’m the family ringmaster and juggler”: autistic parents' experiences of parenting during the COVID-19 pandemic. Autism in Adulthood. 2022.
Adams L, Adamo N, Hollocks MJ, Valmaggia L, Brewster A, Watson J, et al. Examining clinicians’ concerns delivering telemental health interventions directly to autistic individuals during COVID-19. Res Autism Spectr Disord. 2022;94: 101956.
Spain D, Mason D, Capp SJ, Stoppelbein L, White SW, Happé F. “This may be a really good opportunity to make the world a more autism friendly place”: professionals’ perspectives on the effects of COVID-19 on autistic individuals. Res Autism Spectr Disord. 2021;83:101.
Spain D, Stewart GR, Mason D, Robinson J, Capp SJ, Gillan N, et al. Autism diagnostic assessments with children, adolescents, and adults prior to and during the COVID-19 pandemic: a cross-sectional survey of professionals. Front Psychiatry. 2022;13.
Friedman C. The COVID-19 pandemic and quality of life outcomes of people with intellectual and developmental disabilities. Disabil Health J. 2021;14(4):101.
Krieger I, Erez G, Weinstein O, Cohen AD, Tzur Bitan D. COVID-19 morbidity among individuals with autistic spectrum disorder: a matched controlled population-based study. J Autism Dev Disord. 2021.
Koyama AK, Koumans EH, Sircar K, Lavery A, Hsu J, Ryerson AB, et al. Severe outcomes, readmission, and length of stay among COVID-19 patients with intellectual and developmental disabilities. Int J Infect Dis. 2022;116:328–30.
Oakley B, Tillmann J, Ruigrok A, Baranger A, Takow C, Charman T, et al. COVID-19 health and social care access for autistic people: European policy review. Bmj Open. 2021;11(6):e045341.
Weinstein O, Krieger I, Cohen AD, Tzur BD. COVID-19 vaccination among individuals with autism spectrum disorder: a population-based study. Res Autism Spectr Disord. 2021;89: 101865.
Shea LL, Becker A, Lee BK, Miller KK, Cooper D, Anderson K, et al. Self-reported COVID-19 vaccination acceptance and hesitancy among autistic adults. Vaccine. 2022;40(24):3288–93.
White LC, Law JK, Daniels AM, Toroney J, Vernoia B, Xiao S, et al. Brief report: impact of COVID-19 on individuals with ASD and their caregivers: a perspective from the SPARK cohort. J Autism Dev Disord. 2021;51(10):3766–73.
Camm-Crosbie L, Bradley L, Shaw R, Baron-Cohen S, Cassidy S. ‘People like me don’t get support’: autistic adults’ experiences of support and treatment for mental health difficulties, self-injury and suicidality. Autism. 2019;23(6):1431–41.
Mason D, Ingham B, Urbanowicz A, Michael C, Birtles H, Woodbury-Smith M, et al. A systematic review of what barriers and facilitators prevent and enable physical healthcare services access for autistic adults. J Autism Dev Disord. 2019;49(8):3387–400.
Doherty M, Neilson S, Sullivan J, Carravallah L, Johnson M, Cullen W, et al. Barriers to healthcare and self-reported adverse outcomes for autistic adults: a cross-sectional study. BMJ Open. 2022;12(2): e056904.
• Ali D, O'Brien S, Hull L, Kenny L, Mandy W. ‘The key to this is not so much the technology. It’s the individual who is using the technology’: perspectives on telehealth delivery for autistic adults during the COVID-19 pandemic. Autism. 2022:13623613221108010. This study explored the benefits and pitfalls of telehealth services for Autistic adults.
Harris L, Gilmore D, Hanks C, Coury D, Moffatt-Bruce S, Garvin JH, et al. “It was surprisingly equivalent to the appointment I had in person”: advantages and disadvantages of synchronous telehealth for delivering primary care for autistic adults. Autism. 2021.
Gibbs V, Cai RY, Aldridge F, Wong M. Autism assessment via telehealth during the Covid 19 pandemic: experiences and perspectives of autistic adults, parents/carers and clinicians. Res Autism Spectr Disord. 2021;88:101.
•• Bundy R, Mandy W, Crane L, Belcher H, Bourne L, Brede J, et al. The impact of early stages of COVID-19 on the mental health of autistic adults in the United Kingdom: a longitudinal mixed-methods study. Autism. 2022. This study used a mixed-methods design to examine the pandemic’s impact on Autistic adults retrospectively and prospectively.
Maljaars J, Gijbels E, Evers K, Spain D, Rumball F, Happé F, et al. Impact of the COVID-19 pandemic on daily life: diverse experiences for autistic adults. J Autism Dev Disord. 2022.
Pellicano E, Brett S, den Houting J, Heyworth M, Magiati I, Steward R, et al. COVID-19, social isolation and the mental health of autistic people and their families: a qualitative study. Autism. 2021;26(4):914–27.
• Bal VH, Wilkinson E, White LC, Law JK, Consortium TS, Feliciano P, et al. Early pandemic experiences of autistic adults: predictors of psychological distress. Autism Research. 2021;14(6):1209–19. This quantitative study examined the pandemic’s early impact on the wellbeing of Autistic adults.
Scheeren AM, Howlin P, Pellicano L, Magiati I, Begeer S. Continuity and change in loneliness and stress during the COVID-19 pandemic: a longitudinal study of autistic and non-autistic adults. Autism Res. 2022;15(9):1621–35.
Adams RE, Zheng S, Taylor JL, Bishop SL. Ten weeks in: COVID-19-related distress in adults with autism spectrum disorder. Autism. 2021;25(7):2140–5.
Gómez-Ramiro M, Fico G, Anmella G, Vázquez M, Sagué-Vilavella M, Hidalgo-Mazzei D, et al. Changing trends in psychiatric emergency service admissions during the COVID-19 outbreak: report from a worldwide epicentre. J Affect Disord. 2021;282:26–32.
Fridell A, Norrman HN, Girke L, Bolte S. Effects of the early phase of COVID-19 on the autistic community in Sweden: a qualitative multi-informant study linking to ICF. Int J Environ Res Public Health. 2022;19(3):126.
•• Oomen D, Nijhof AD, Wiersema JR. The psychological impact of the COVID-19 pandemic on adults with autism a survey study across three countries. Mol Autism. 2021;12(1):21 This study combined quantitative and qualitative methods to examine the pandemic’s impact on Autistic adults.
Lois Mosquera M, Mandy W, Pavlopoulou G, Dimitriou D. Autistic adults’ personal experiences of navigating a social world prior to and during Covid-19 lockdown in Spain. Research in Developmental Disabilities. 2021;117.
Davidson CJ, Lodge K, Kam A. The impact of the COVID-19 pandemic on autistic adults - a survey. Advances in Autism. 2021;7(4):311–21.
Wood R, Crane L, Happé F, Moyse R. Learning from autistic teachers: lessons about change in an era of COVID-19. Educ Rev. 2022:1–23.
Bruckner TA, Scheffler RM, Shen G, Yoon J, Chisholm D, Morris J, et al. The mental health workforce gap in low- and middle-income countries: a needs-based approach. Bull World Health Organ. 2011;89(3):184–94.
Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515–25.
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60.
London AJ, Kimmelman J. Against pandemic research exceptionalism. Science. 2020;368(6490):476–7.
Jung RG, Di Santo P, Clifford C, Prosperi-Porta G, Skanes S, Hung A, et al. Methodological quality of COVID-19 clinical research. Nat Commun. 2021;12(1):943.
Lai M-C, Anagnostou E, Wiznitzer M, Allison C, Baron-Cohen S. Evidence-based support for autistic people across the lifespan: maximising potential, minimising barriers, and optimising the person–environment fit. Lancet Neurology. 2020;19(5):434–51.
den Houting J, Higgins J, Isaacs K, Mahony J, Pellicano E. ‘I’m not just a guinea pig’: academic and community perceptions of participatory autism research. Autism. 2021;25(1):148-
Rudd D, Hwang SK. Participatory research in a pandemic: the impact of Covid-19 on co-designing research with autistic people. Qual Soc Work. 2022;21(5):869–79.
Acknowledgements
We also thank Marc Stears for comments and edits on a previous version of this manuscript.
Funding
EP was supported by an Australian Research Council Future Fellowship (FT190100077). The views expressed are the views of the authors alone and do not necessarily represent the views of their organisations or funding sources.
Author information
Authors and Affiliations
Contributions
Anke Scheeren: conceptualisation, data curation, formal analysis, methodology, writing — original draft (lead); Laura Crane: conceptualisation, methodology, validation, writing — original draft; Melanie Heyworth: conceptualisation, methodology, validation, writing — original draft; Elizabeth Pellicano: conceptualisation, methodology, validation, supervision, writing — original draft.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Scheeren, A.M., Crane, L., Heyworth, M. et al. Impact of the COVID-19 Pandemic on Autistic Adults: a Scoping Review. Curr Dev Disord Rep 10, 92–122 (2023). https://doi.org/10.1007/s40474-023-00268-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-023-00268-6