Abstract
Background
The cerebellum is an important area of the brain implicated in severe mental disorders. It can be therapeutically modulated in a neuroscience-informed manner through transcranial magnetic stimulation (TMS). In this review, our objective was to identify and summarize the findings of studies which have utilized cerebellar TMS as an intervention in psychiatric disorders and primarily reported clinical outcomes.
Methods
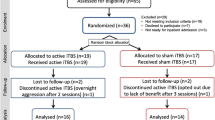
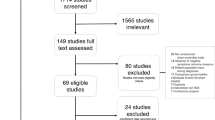
Case reports, open-label studies, and randomized controlled trials (RCTs) which recruited patients with a psychiatric disorder diagnosed as per standard diagnostic criteria who received cerebellar repetitive TMS (rTMS) as an intervention with a primary clinical outcome were included in the review. Neurological studies, animal studies, studies done on healthy participants, investigative TMS studies that study a neurophysiological/neuropsychological outcome, and studies that do not primarily stimulate the cerebellum were excluded. MEDLINE, PsychINFO, and EMBASE were searched till August 2023. The risk of bias was assessed qualitatively, and details of individual studies were tabulated.
Results
Eight studies comprising 215 participants were included in the review out of which 2 were case reports, 1 was an open-label study, and 5 were double-blind sham-controlled RCTs. All the studies recruited participants with schizophrenia, specifically targeting negative symptoms. The open-label trial and case reports demonstrate an improvement in negative symptoms which are not replicated consistently in the double-blind RCTs. Amongst the double-blind RCTs, 2 are positive, one is inconclusive, and 2 are negative.
Discussion
Cerebellar TMS as an intervention for psychiatric disorders is studied primarily in schizophrenia, mostly for negative symptoms. The current evidence is mixed and inconclusive. This is because of the limited number of studies with small sample sizes and significant heterogeneity in the conduct of rTMS trials for negative symptoms of schizophrenia. Future studies may focus on (a) optimizing stimulation parameters and localization techniques and (b) exploring alternative clinical targets (e.g., auditory hallucinations and depressive symptoms) for cerebellar neuromodulation.
Other
This systematic review was funded by the Department of Health Research (DHR) fellowship program for NRI/PIO/OCI, Reference ID: 2021–1004 and Narmadanagar Rural Development Society (NARDES), the CSR arm of GNFC, Gujarat, Reference: NARDES/PH/2023/1205. The systematic review proposal was registered in PROSPERO, International prospective register of systematic reviews (CRD42023459268).

Similar content being viewed by others
References
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Howes OD, Thase ME, Pillinger T. Treatment resistance in psychiatry: state of the art and new directions. Mol Psychiatry. 2022;27(1):58.
Cotovio G, Ventura F, Rodrigues da Silva D, Pereira P, Oliveira-Maia AJ. Regulatory clearance and approval of therapeutic protocols of transcranial magnetic stimulation for psychiatric disorders. Brain Sci. 2023;13(7):1029.
Villanueva R. The cerebellum and neuropsychiatric disorders. Psychiatry Res. 2012;198(3):527–32.
Adamaszek M, D’Agata F, Ferrucci R, Habas C, Keulen S, Kirkby KC, et al. Consensus paper: cerebellum and emotion. Cerebellum Lond Engl. 2017;16(2):552–76.
Schmahmann JD. Emotional disorders and the cerebellum: neurobiological substrates, neuropsychiatry, and therapeutic implications. Handb Clin Neurol. 2021;183:109–54.
Schmahmann JD. The cerebellum and cognition. Neurosci Lett. 2019;1(688):62–75.
Mothersill O, Knee-Zaska C, Donohoe G. Emotion and theory of mind in schizophrenia-investigating the role of the cerebellum. Cerebellum Lond Engl. 2016;15(3):357–68.
Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16(3):367–78.
Brady RO, Gonsalvez I, Lee I, Öngür D, Seidman LJ, Schmahmann JD, et al. Cerebellar-prefrontal network connectivity and negative symptoms in schizophrenia. Am J Psychiatry. 2019;175(7):512.
Moreno-Rius J. The cerebellum in fear and anxiety-related disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;13(85):23–32.
Amaral DG, Schumann CM, Nordahl CW. Neuroanatomy of autism. Trends Neurosci. 2008;31(3):137–45.
Moberget T, Doan NT, Alnæs D, Kaufmann T, Córdova-Palomera A, Lagerberg TV, et al. Cerebellar volume and cerebellocerebral structural covariance in schizophrenia: a multisite mega-analysis of 983 patients and 1349 healthy controls. Mol Psychiatry. 2018;23(6):1512–20.
Moberget T, Ivry RB. Prediction, psychosis, and the cerebellum. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4(9):820–31.
Laidi C, Floris DL, Tillmann J, Elandaloussi Y, Zabihi M, Charman T, et al. Cerebellar atypicalities in autism? Biol Psychiatry. 2022;92(8):674–82.
Phillips JR, Hewedi DH, Eissa AM, Moustafa AA. The cerebellum and psychiatric disorders. Front Public Health. 2015;5(3):66.
Andreasen NC, Paradiso S, O’Leary DS. “Cognitive dysmetria” as an integrative theory of schizophrenia: a dysfunction in cortical-subcortical-cerebellar circuitry? Schizophr Bull. 1998;24(2):203–18.
Palesi F, Tournier JD, Calamante F, Muhlert N, Castellazzi G, Chard D, et al. Contralateral cerebello-thalamo-cortical pathways with prominent involvement of associative areas in humans in vivo. Brain Struct Funct. 2015;220(6):3369–84.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372):n71.
Basavaraju R, Ithal D, Ramalingaiah AH, Thirthalli J, Mehta UM, Kesavan M. “Apathetic to hypomanic/manic”: a case series-illustration of emergent mood symptoms during intermittent theta burst stimulation (iTBS) of cerebellar vermis in schizophrenia with predominant negative symptoms. Schizophr Res. 2020;222:501–2.
Tikka SK, Garg S, Sinha VK, Nizamie SH, Goyal N. Resting state dense array gamma oscillatory activity as a response marker for cerebellar-repetitive transcranial magnetic stimulation (rTMS) in schizophrenia. J ECT. 2015;31(4):258–62.
Basavaraju R, Mehta U, Ithal D, Thanki M, Thirthalli J, Brady R, et al. Intermittent theta burst stimulation of cerebellar vermis in schizophrenia: impact on negative symptoms and brain connectivity. Brain Stimul Basic Transl Clin Res Neuromodulation. 2019;12(2):489–90.
Garg S, Sinha VK, Tikka SK, Mishra P, Goyal N. The efficacy of cerebellar vermal deep high frequency (theta range) repetitive transcranial magnetic stimulation (rTMS) in schizophrenia: a randomized rater blind-sham controlled study. Psychiatry Res. 2016;30(243):413–20.
De Vidovich GZ, Muffatti R, Monaco J, Caramia N, Broglia D, Caverzasi E, et al. Repetitive TMS on left cerebellum affects impulsivity in borderline personality disorder: a pilot study. Front Hum Neurosci [Internet]. 2016 [cited 2023 Nov 15];10. Available from: https://www.frontiersin.org/articles/10.3389/fnhum.2016.00582
Naro A, Marra A, Billeri L, Portaro S, De Luca R, Maresca G, et al. New horizons in early dementia diagnosis: can cerebellar stimulation untangle the knot? J Clin Med. 2019;8(9):1470.
Garg S, Tikka SK, Goyal N, Sinha VK, Nizamie SH. Amelioration of anergia and thought disorder with adjunctive high frequency cerebellar vermal repetitive transcranial magnetic stimulation in schizophrenia: a case report. Schizophr Res. 2013;143(1):225–7.
Garg S, Goyal N, Tikka SK, Sinha VK. Exacerbation of auditory verbal hallucinations with adjunctive high-frequency cerebellar vermal repetitive transcranial magnetic stimulation in schizophrenia: a case report. J ECT. 2013;29(1):65–6.
Demirtas-Tatlidede A, Freitas C, Cromer JR, Safar L, Ongur D, Stone WS, et al. Safety and proof of principle study of cerebellar vermal theta burst stimulation in refractory schizophrenia. Schizophr Res. 2010;124(1–3):91–100.
Zhu L, Zhang W, Zhu Y, Mu X, Zhang Q, Wang Y, et al. Cerebellar theta burst stimulation for the treatment of negative symptoms of schizophrenia: a multicenter, double-blind, randomized controlled trial. Psychiatry Res. 2021;5(305):114204.
Chauhan P, Garg S, Tikka SK, Khattri S. Efficacy of intensive cerebellar intermittent theta burst stimulation (iCiTBS) in treatment-resistant schizophrenia: a randomized placebo-controlled study. Cerebellum Lond Engl. 2021;20(1):116–23.
Basavaraju R, Ithal D, Thanki MV, Ramalingaiah AH, Thirthalli J, Reddy RP, et al. Intermittent theta burst stimulation of cerebellar vermis enhances fronto-cerebellar resting state functional connectivity in schizophrenia with predominant negative symptoms: a randomized clinical trial. Schizophr Res. 2021;238:108–20.
Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet Lond Engl. 2018;391(10131):1683–92.
Hurtado-Puerto AM, Nestor K, Eldaief M, Camprodon JA. Safety considerations for cerebellar theta burst stimulation. Clin Ther. 2020;42(7):1169-1190.e1.
Fernandez L, Rogasch NC, Do M, Clark G, Major BP, Teo WP, et al. Cerebral cortical activity following non-invasive cerebellar stimulation-a systematic review of combined TMS and EEG studies. Cerebellum Lond Engl. 2020;19(2):309–35.
Marder SR, Daniel DG, Alphs L, Awad AG, Keefe RSE. Methodological issues in negative symptom trials. Schizophr Bull. 2011;37(2):250–4.
Ferri J, Ford JM, Roach BJ, Turner JA, van Erp TG, Voyvodic J, et al. Resting-state thalamic dysconnectivity in schizophrenia and relationships with symptoms. Psychol Med. 2018;48(15):2492–9.
Cao H, Wei X, Zhang W, Xiao Y, Zeng J, Sweeney JA, et al. Cerebellar functional dysconnectivity in drug-naïve patients with first-episode schizophrenia. Schizophr Bull. 2022;49(2):417–27.
Cole EJ, Phillips AL, Bentzley BS, Stimpson KH, Nejad R, Barmak F, et al. Stanford neuromodulation therapy (SNT): a double-blind randomized controlled trial. Am J Psychiatry. 2021;179(2):132–41.
Hird EJ, Diederen K, Leucht S, Jensen KB, McGuire P. The Placebo effect in psychosis: why it matters and how to measure it. Biol Psychiatry Glob Open Sci. 2023;3(4):605–13.
Kim NY, Hsu J, Talmasov D, Joutsa J, Soussand L, Wu O, et al. Lesions causing hallucinations localize to one common brain network. Mol Psychiatry. 2021;26(4):1299–309.
Schmahmann JD, Weilburg JB, Sherman JC. The neuropsychiatry of the cerebellum - insights from the clinic. Cerebellum Lond Engl. 2007;6(3):254–67.
Carta I, Chen CH, Schott AL, Dorizan S, Khodakhah K. Cerebellar modulation of the reward circuitry and social behavior. Science. 2019;363(6424):eaav0581.
Funding
We acknowledge the support from the Department of Health Research (DHR) fellowship program for NRI/PIO/OCI, Project Id: 2021–1004 (to RB) and Narmadanagar Rural Development Society (NARDES), the CSR arm of GNFC, Gujarat, Reference: NARDES/PH/2023/1205 (to UMM).
Author information
Authors and Affiliations
Contributions
SK, RB, and UMM performed the review. RB and UMM interpreted the results. RB prepared the manuscript, and UMM edited the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Nil.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Basavaraju, R., Kaur, S. & Mehta, U.M. Cerebellar Transcranial Magnetic Stimulation in Psychiatric Disorders: A Systematic Review. Curr Behav Neurosci Rep 11, 23–32 (2024). https://doi.org/10.1007/s40473-024-00270-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40473-024-00270-1