Abstract
Purpose of Review
Sarcopenia is highly prevalent in end-stage liver disease (ESLD) patients and has been linked to poor outcomes on the wait list and post-transplantation. This current perspectives article reviews the ongoing challenges to define sarcopenia in ESLD patients, describes associations of sarcopenia with wait list and post-transplantation outcomes, and provides summarized data on efforts to prevent and treat sarcopenia through novel interventions.
Recent Findings
Supervised exercise programs improve muscle strength, but muscle mass outcomes are limited by short study follow-up times. Branched-chain amino acid supplementation may ameliorate sarcopenia in ESLD patients, but studies are limited by low participant numbers and confounding. Myostatin inhibition is shown to improve sarcopenia in elderly, frail patients; further study is needed in ESLD patients. Correction of low testosterone improves sarcopenia in male ESLD patients.
Summary
Recent literature supports sarcopenia as an independent risk factor for poor outcomes in ESLD patients. Ongoing study is limited by poor standardization of sarcopenia definition and relevant muscle mass cutoffs. Supervised exercise programs should be encouraged for all ESLD patients. More advanced therapies require further clinical investigation before their widespread use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia was originally proposed by Irwin Rosenberg as a term to describe an age-related decrease in muscle mass and strength [1]. Initially, “primary” sarcopenia was envisioned as a complex, multifactorial geriatric syndrome akin to dementia and falls with high incidence and associated costs [2]. Since then, elements of sarcopenia have been observed in non-geriatric populations such as those with chronic medical conditions, malnutrition, and sedentary lifestyle [3,4,5,6,7,8,9]. These patients with “secondary” sarcopenia are now recognized to have worse outcomes independent of the standard disease-related risk factors.
Liver transplantation candidates are exceptionally prone to sarcopenia given their chronic illness, malnutrition, persistent inflammatory state, and hypermetabolic condition. It is estimated that 22–70% of patients with end-stage liver disease (ESLD) have sarcopenia [10]. The association between sarcopenia and morbidity/mortality in ESLD patients is a relatively new area of research, with the first published study occurring in 2010 [11]. Since then, it has been found to be a strong, independent predictor of adverse outcomes on both the wait list and post-transplantation [12,13,14,15].
Efforts to standardize the definition of sarcopenia in ESLD patients with precise cutoffs for muscle mass and strength have been challenging. This current perspectives article reviews the ongoing challenges to define sarcopenia in ESLD patients, describes associations of sarcopenia with wait list and post-transplantation outcomes, and provides summarized data on efforts to prevent and treat sarcopenia through novel interventions such as supervised exercise programs, branched-chain amino acid supplementation, myostatin inhibition, and testosterone supplementation.
Measuring Sarcopenia
The first consensus definition of sarcopenia for the general patient comes from the European Working Group on Sarcopenia in Older People 2010 guidelines [2]. This group required the presence of both low muscle mass and low muscle function (strength or performance, also known as dynapenia) for the diagnosis of sarcopenia. However, the definition was entirely qualitative, with no defined cutoffs for muscle mass or strength. As a result, its adoption has been limited in the global study of sarcopenia, and contemporary methods to measure and diagnose sarcopenia are varied and inconsistent [16,17,18,19].
Most sarcopenia studies (93.3%) utilize some form of skeletal muscle mass measurement, with 70% of studies using a single skeletal muscle mass measurement alone [16]. Examples include dual-energy X-ray absorptiometry, bioelectrical impedance analysis, L3 total psoas index, L3 skeletal muscle index, dorsal muscle group area, and total quadriceps area (Fig. 1). Only a minority of studies (25.8%) include a functional assessment of strength or performance, with the handgrip strength test being the most common additional criteria. Other examples of functional criteria include a test of walking speed, 6-min walking distance, and physical performance battery. These differences in measurement have been important limitations for comparing studies and outcomes between centers.
Sample CT scan of cirrhotic patient. Axial CT scan of cirrhotic patient at L3. Blue outline = bilateral psoas muscles. Red outline = bilateral dorsal muscle groups. Yellow outline = abdominal wall muscles. Red + blue + yellow outlines = total skeletal muscle area at L3. Indices such as L3 skeletal muscle index are calculated by the total respective muscle area normalized to patient height
For liver transplantation candidates, several recent studies have shown weak or absent correlation between measurements of muscle mass and function [17,18,19]. Additionally, there is evidence that sex may play a role in correlation between muscle mass and function. For instance, Wang et al. found handgrip strength to be correlated with muscle mass in men (ρ = 0.26, p < 0.001), but not in women (ρ = 0.002, p = 0.99) [17]. It is also possible that different ways of measuring muscle mass or function can be more or less predictive of particular outcomes. For example, Wada et al. used muscle mass alone to predict post-transplantation respiratory complications and found that normalized total psoas volume (nTPV) was significantly associated with adverse events (OR 15.00, 95%CI 1.03 to 218.31), whereas normalized total psoas area (nTPA) did not reach statistical significance but was suggestive of an association (OR 3.33, 95%CI 0.36 to 30.70) [20]. These findings highlight the methodological challenges of defining sarcopenia in ESLD patients, especially when it is possible that different tests or cutoffs will better suit particular demographics or predict certain outcomes.
However, attempts are being made to standardize the cutoffs for muscle mass measurements in ESLD patients. In a multicenter study of 396 newly listed ESLD patients awaiting liver transplantation, Carey et al. utilized a grid search guided by log-rank test statistics to create sex-specific cutoff values of L3 skeletal muscle index (L3SMI) in predicting wait list mortality [21]. In this study, optimal search method yielded L3SMI cutoffs of 50 cm2/m2 for men and 39 cm2/m2 for women. Alternatively, Golse et al. prospectively analyzed the receiver operating characteristic curves comparing psoas muscle area (PMA), PMA normalized by height or body surface area, and L3SMI in 256 patients who underwent transplantation at a single center and found PMA to be the best predictor of 1-year mortality [22]. In this case, the Youden index was used to assign PMA cutoffs of 1561 mm2 for men and 1464 mm2 for women. For each of these studies, further prospective validation and correlation with muscle function will need to be performed.
Even with the major shortcomings of inconsistent modalities for measuring sarcopenia components and absence of standardized cutoffs, sarcopenia has still outperformed the Model for End-Stage Liver Disease (MELD) score as an independent predictor of outcomes in several studies [12, 13, 23,24,25]. These include outcomes such as mortality, infection, development of hepatic encephalopathy, and post-transjugular intrahepatic portosystemic shunt complications. Inclusion of sarcopenia into the MELD score has also been suggested, particularly in patients with refractory ascites or MELD < 15 [26]. Prospective validation of the MELD-sarcopenia score (MELD + 10.35 x sarcopenia) showed significant but modest improvement over the existing MELD score [27].
The study of sarcopenia in ESLD patients and associated outcomes needs an exact, quantifiable definition with international consensus. Only after this is established will accurate comparisons between studies be possible.
Sarcopenia Outcomes
Waiting List
Regardless of particular sarcopenia definitions or cutoffs, several historical studies have established sarcopenia as a risk factor for wait list mortality [12, 13, 28]. The seminal study was performed by Tandon et al. as a retrospective analysis of 142 patients on the University of Alberta liver transplant wait list from 2005 to 2009 [13]. After adjusting for age and MELD score, sarcopenia was found to be a 2.4-fold independent risk factor for mortality. Interestingly, sarcopenia had the greatest influence on mortality for patients with MELD < 15. Similarly, the degree of sarcopenia has also been shown to influence wait list mortality. In a study of 376 wait list patients during the MELD era (2007–2011), Durand et al. found a 15% increase in mortality risk per-unit decrease in transverse psoas muscle thickness (TMPT)/height ratio [12]. This relationship remained significant independent of MELD and MELD-Na scores.
However, two recent studies have challenged the association of sarcopenia with wait list mortality. First, Yadav et al. performed a retrospective, single-center analysis of 213 patients on the wait list, exploring the relationship between sarcopenia, 6-min walk distance (6MWD), and health-related quality of life (HRQOL) [18]. On multivariate analysis, a trend towards wait list mortality was found in patients that had a 6MWD < 250 m (HR 2.1, 95%CI 0.9 to 4.7). Conversely, sarcopenia was not associated with mortality on univariate (HR 1.3, 95%CI 0.6 to 2.6) or multivariate (HR 1.0, 95%CI 1.0 to 1.0) analysis. There was a poor correlation between sarcopenia and 6MWD (r = 0.19, p = 0.007), and no correlation with the physical component score of the HRQOL (r = 0.03, p = 0.71).
In the second study, Wang et al. performed a prospective analysis of 292 liver transplant wait list candidates who were enrolled in the Functional Assessment in Liver Transplantation (FrAILT) study [17]. This study compared the relationship between grip strength, Short Physical Performance Battery (SPPB) score, muscle mass, and muscle quality (as measured by the mean CT attenuation for the entire L3 skeletal muscle area). After adjusting for gender, MELD-Na, hepatocellular carcinoma, and BMI, grip strength (HR 0.74 per 5 kg increase, 95%CI 0.59 to 0.92), SPPB (HR 0.89 per point increase, 95%CI 0.82 to 0.97), and muscle quality (HR 0.77 per 5 Hounsfield unit increase, 95%CI 0.63 to 0.95) were associated with wait list mortality; muscle mass was not (HR 0.91 per 5 cm2/m2 increase, 95%CI 0.75 to 1.11). These studies suggest that functional criteria of sarcopenia may better predict mortality than muscle mass measurement alone in wait list candidates.
However, a subsequent multicenter study has again reinforced the relationship of sarcopenia with wait list mortality. Carey et al. performed a retrospective analysis of 396 ESLD patients who were listed for liver transplantation in 2012 at five North American transplant centers [21]. For measurement of sarcopenia, they used the L3 skeletal muscle index (L3SMI) alone. Patients who died had lower L3SMI than those who survived (45.6 versus 48.5 cm2/m2, p < 0.001), and L3SMI was associated with decreased wait list survival on a per-unit basis (HR 0.95 per 1 cm2/m2 decrease, 95%CI 0.94 to 0.97). These findings were further supported by a recent meta-analysis that included four studies of wait list candidates, with sarcopenic patients having an increased risk of mortality as compared with non-sarcopenic patients (pooled HR 1.72, 95%CI 0.99 to 3.00, p = 0.05) [10].
Finally, sarcopenia is linked to increased costs for liver transplant candidates. In 2018, van Vugt et al. published the clinical and outpatient department costs of 362 consecutive patients with cirrhosis on the wait list at a single European center [29]. Median total costs for sarcopenic patients were $12,289 (IQR $3885 to 50,565), compared with $7484 (IQR $1420 to 22,457) in non-sarcopenic patients. Each unit decrease in L3SMI was associated with an increase in total costs of $495 per incremental SMI (95%CI $12 to 979). Interestingly, the differences in cost were found to be independent of time on the wait list.
Overall, sarcopenia appears to be strongly associated with mortality on the liver transplantation wait list. However, recent studies by Wang et al. and Yadav et al. suggest that the muscle function component of the sarcopenia should not be ignored [17, 18]. Further prospective studies involving measurements of both muscle mass and function are necessary.
Post-transplantation
The association of sarcopenia with increased post-transplantation mortality, length of intensive care unit stay, length of hospital stay, and postoperative infection/sepsis in cirrhotic patients has been well established [11, 14, 23, 30,31,32,33]. It is estimated that patients with sarcopenia have a 4.8 times higher risk of death within 1 year after liver transplantation than non-sarcopenic patients [30]. Multiple recent studies have further supported the association of sarcopenia with post-transplantation mortality [10, 15, 34,35,36,37,38,39]. The largest of these was a 2016 meta-analysis of the impact of CT-assessed skeletal muscle mass on patients who underwent liver transplantation [10]. In this study, van Vugt et al. incorporated 11 studies that revealed a pooled HR of 1.84 (95%CI 1.11 to 3.05) for mortality in sarcopenic patients.
Other recent studies have established sarcopenia as a risk factor for failure to rescue and poor post-transplantation pulmonary outcomes [20, 40, 41]. Underwood et al. retrospectively reviewed 348 liver transplant recipients and found that patients in the smallest tertile of total psoas area had a 1.4-fold higher adjusted complication rate (91% versus 66%) and 2.8-fold higher adjusted failure-to-rescue rate (22% versus 8%, p < 0.001) within the first year after transplantation [40]. Shirai et al. found psoas muscle mass index, intramuscular adipose tissue, and grip strength to be associated with decreased preoperative vital capacity and forced expiratory volume after transplantation [41]. Finally, Wada et al. found preoperative normalized total psoas volume to be strongly associated with postoperative pneumonia within 30 days, need for tracheostomy after surgery, or greater than 8 days on a ventilator [20]. Given the association of sarcopenia with poor post-transplantation outcomes, some centers have even excluded patients with muscle wasting and increased visceral adiposity from consideration for living-donor liver transplantation. Outcomes after this change have not yet been reported [42].
One additional area of new research is the impact of de novo perioperative sarcopenia on post-transplantation outcomes. In a retrospective study of 145 patients who underwent liver transplantation at a single center with follow-up CT scan 1 year later, Jeon et al. found that 14 of the 93 (15%) patients without pre-transplantation sarcopenia went on to develop post-transplantation sarcopenia [43]. Further analysis found newly developed sarcopenia to be a strong, independent predictor of post-transplantation mortality (HR 10.53, 95%CI 1.37 to 80.93). However, this study was limited by selection bias given the non-standardized nature of CT scans and exclusion of patients who died within 6 months of transplantation. Another study by Chae et al. found that even changes in psoas muscle index (PMI) as early as postoperative day 7 had an impact on post-transplantation survival [44]. In this case, a PMI decrease of ≤ − 11.7% was an independent risk factor for mortality (HR 1.87, 95%CI 1.07 to 3.25). Surprisingly, 25% of patients studied had a PMI decrease of this magnitude (median overall decrease was − 4.8%, IQR − 11.7 to 1.2%). Further analysis needs to be performed to identify preoperative risk factors for the development of de novo post-transplantation sarcopenia and devise interventions accordingly.
Overall, sarcopenia is strongly associated with poor post-transplantation outcomes. Additionally, recognition of de novo post-transplantation sarcopenia is an exciting area of research that may provide insight into why certain patients never truly overcome the stress of their operation and succumb to illnesses afterwards. However, the most important question is what interventions can be done ahead of time to treat or prevent sarcopenia in ESLD patients.
Interventions
Exercise Programs
It has previously been shown that poor exercise tolerance correlates with poor survival and increasing this tolerance improves survival among liver transplantation wait list patients [45, 46]. In one study, a 6-min walking distance of < 250 m had a 90% predictive value for identifying patients with increased risk of mortality before liver transplantation, and every 100-m improvement in this test begat at 52% reduction in mortality [45]. Supervised exercise programs for cirrhotic patients have been linked to improved cardiopulmonary endurance and health-related quality of life, lower hepatic venous portal gradient, and decreased incidence of metabolic syndrome [47,48,49,50,51].
Additional prospective studies have shown improvement in sarcopenia measures with supervised exercise regimens [52, 53••]. In a single-center RCT, Zenith et al. recruited 19 patients with Child-Pugh A or B cirrhosis who were randomly assigned to exercise training (n = 9) or usual care (n = 10) for 8 weeks; all participants received nutritional counseling as well [53••]. At the end of the study, peak exercise oxygen uptake was 5.3 mL/kg/min higher in the exercise group compared with controls (95%CI 2.9 to 7.8 mL/kg/min), thigh muscle circumference increased (p = 0.001), and thigh muscle thickness also increased (p = 0.01). Of note, thigh muscle thickness is associated with muscle mass at L3 on cross-sectional imaging (correlation coefficient 0.6, p = 0.001) [54].
The main limitations for studies of supervised exercise programs in sarcopenic ESLD patients are low numbers of study participants and limited length of follow-up. Even so, there is considerable evidence to support their utility in this population. It must be stressed that each exercise regimen must be tailored to the individual patient. As illustrated by Tandon et al., exercise program individualization should include a multidisciplinary assessment for cirrhosis-related safety concerns (i.e., untreated esophageal varices, thrombocytopenia, and hepatic encephalopathy), cardiopulmonary safety screening per American College of Sports Medicine guidelines, malnutrition assessment, baseline exercise ability, and screening for comorbidities that may alter exercise tolerance (i.e., recent falls, peripheral arterial disease, osteoarthritis) [55, 56]. Clinically, exercise programs for cirrhotic patience can be challenging to implement. In the USA, there is no reliable way to bill for these incremental services. Many patients with high MELD scores are unlikely to be able to participate safely in unsupervised exercise programs. Traveling for exercise training can also be a significant hardship for many patients.
Branched-Chain Amino Acid Supplementation
During liver failure, ammonia is shunted from hepatic metabolism into skeletal muscle where its metabolism requires utilization of branched-chain amino acids (BCAA; valine, leucine, isoleucine) to generate the glutamate needed for ammonia detoxification, thereby diverting the availability of BCAAs for protein synthesis and maintenance of muscle mass [57]. Additionally, it has been previously shown that BCAAs act as the preferred skeletal muscle protein substrate and energy substrate in cirrhotic patients and supplementation leads to decreased hyperammonemia-induced skeletal muscle autophagy [58,59,60].
Given the central role of BCAAs in skeletal muscle homeostasis, it is unsurprising that lower BCAA levels have been linked to sarcopenia in cirrhotic patients [61]. More recently, Kinny-Köster et al. found an association between low BCAA levels, high aromatic amino acid (AAA; phenylalanine, tyrosine, tryptophan) levels, and reduced BCAA to AAA ratio (Fischer’s ratio) with decreased survival in cirrhotic patients [62]. However, the impact of BCAA supplementation on mortality in cirrhotic patients in general and sarcopenic patients in particular is less well established.
In 2005, Muto et al. performed a landmark multicenter RCT comparing oral BCAA supplementation versus diet therapy on 622 adults with decompensated cirrhosis (defined as (1) serum albumin ≤ 3.5 g/dL and (2) presence of ascites, peripheral edema, or hepatic encephalopathy, or a history of any one of these conditions), over a 2-year period [63]. The BCAA group consisted of 314 patients and the diet group had 308 patients. Using a composite end point of all-cause death, development of liver cancer, rupture of esophageal varices, or progress of hepatic failure, this study found a significant improvement in the BCAA group (HR 0.67, 95%CI 0.49 to 0.93). This difference was primarily driven by decreased progression of liver failure in the BCAA group (HR 0.45, 95%CI 0.23 to 0.88), whereas mortality was not statistically significant (HR 1.18, 95%CI 0.41 to 3.41). This was likely due to the low number of deaths during the study period (6 deaths in each cohort). Interestingly, there were no differences in total energy or protein intake between the study groups. For secondary outcomes, serum albumin levels increased significantly (p = 0.018), as did health-related quality of life (QOL) measured by Short Form-36 questionnaire (p = 0.003) in the BCAA cohort. Given the improvement in outcomes, this study was discontinued 10 months early and later formed the basis for BCAA supplementation in Japanese cirrhotic patients for stabilizing liver function [64].
Several small Japanese studies have assessed whether BCAA supplementation improves or prevents sarcopenia in cirrhotic patients; however, most of these are limited by low patient numbers, confounding, poor long-term follow-up, and lack of appropriate control groups [65, 66••]. Hiraoka et al. prospectively studied 33 patients with cirrhosis who underwent BCAA supplementation as a late evening snack and also walking exercise (additional 2000 steps/day), over a 3-month period [65]. With patients acting as their own controls, this study found improved BCAA/tyrosine ratio (4.3 ± 1.35 to 5.24 ± 2.04, p = 0.001), average daily step ratio (1.595, p = 0.02), muscle volume ratio (1.013, p < 0.01), leg strength ratio (1.110, p < 0.01), and handgrip strength ratio (1.056, p < 0.01). Interestingly, the study participants’ BCAA/tyrosine ratios improved even though they had normal pre-supplementation albumin levels (4.3 g/dL, IQR 3.9 to 4.6 g/dL). However, inclusion of a walking exercise in the intervention with participants acting as their own controls was a significant confounder, and it is therefore impossible to tease out the impact of exercise from BCAA supplementation in this study.
Uojima et al. prospectively studied 82 cirrhotic patients with persistent hypoalbuminemia (albumin < 3.5 g/dL) after undergoing standard nutrition therapy for at least 28 days, who then underwent BCAA supplementation for 24 weeks and again acted as their own controls [66••]. After completing the study period, participants had improved muscle strength as measured by handgrip strength test (pre-treatment 22.2 ± 6.3 kg, post-treatment 23.9 ± 6.4 kg, p < 0.001); however, there was no difference in skeletal muscle mass index as measured by bioelectrical impedance analysis divided by height squared (pre-treatment 7.40 ± 1.62, post-treatment 7.30 ± 1.49, p = 0.333). Given the short length of follow-up, it is not surprising that the skeletal muscle mass index was unchanged.
Overall, the impact of BCAA supplementation on sarcopenic cirrhotic patients remains enticing but under-studied. It is a relatively benign intervention with few side effects and low risk profile, but its efficacy has not been addressed with an RCT or prospective study of US participants [63, 65, 66••]. Given the dietary differences between Asian and US populations, it will be important to study BCAA in a US population before its practice can be adopted. Additionally, particular indications for its use in sarcopenic patients are not established; for instance, should its use be based on laboratory values (i.e., low BCAA or albumin cutoff), functional status, or diagnosis of sarcopenia alone? Further US studies are necessary to address these topics.
Myostatin Inhibition
In addition to lowering BCAA levels, hyperammonemia has also been linked to increased production of the paracrine/endocrine factor myostatin via the NF-kB pathway [67]. Myostatin is a cytokine member of the TGFβ superfamily that acts as a negative regulator of muscle protein synthesis, thereby strongly suppressing skeletal muscle growth [68, 69]. Elevated levels have been shown to be associated with sarcopenia and linked to worsened survival in cirrhotic patients [68].
Given its role in suppression of protein synthesis and skeletal muscle growth, myostatin is being targeted as a novel pathway to treat and/or prevent sarcopenia. Although there are no studies in cirrhotic patients yet, one recent multicenter, double-blinded phase 2 RCT study analyzed the impact of a humanized myostatin antibody (LY2495655) on appendicular lean body mass (aLBM) in frail patients age ≥ 75 who had fallen within the past year [70••]. Of the 201 participants recruited, 99 were randomly assigned to receive placebo and 102 received the myostatin antibody (LY group). After 24 weeks of therapy, the least-squares mean change in aLBM was − 0.123 kg (95%CI − 0.287 to 0.040) in the placebo group and + 0.303 kg (95%CI 0.135 to 0.470) in the LY group, a difference of 0.430 kg (95%CI 0.192 to 0.660). For secondary outcomes, the LY group also had a greater increase in total body lean mass (p = 0.0007), a larger reduction in total body fat mass (p < 0.0001), and improvements in several performance-based measures including four-step stair climb test, 12-step stair climb test and power, five-chair rise using arms, and fast gait speed. However, there were no significant differences in other performance-based measures such as 6-min walking distance, leg extension strength, usual gait speed, or handgrip strength. No significant differences in adverse events were reported. The ability for this intervention to improve aLBM over a relatively short trial period merits further analysis in cirrhotic patients.
Testosterone Supplementation
For male patients with ESLD undergoing transplantation evaluation, low testosterone levels are associated with sarcopenia and predict mortality independent of MELD score [71, 72]. In an observational study of 171 ESLD patients undergoing transplantation evaluation in Australia, Grossmann et al. discovered that 61% of male patients had low total testosterone levels (TT, < 10 nmol/L), and 90% had low calculated free testosterone levels (cFT, < 230 pmol/L) [71]. Each was independently associated with mortality, and a decrease in TT by 1 nM or cFT by 10 pM was each associated with an 8% increase in mortality.
These findings were supported by a prospective observational study of 268 ESLD patients at the same center from 2013 to 2014 [73]. Using more restrictive cutoffs for low TT (< 8.3 nmol/L) and cFT (< 139 pmol/L), this study found TT to be an independent risk factor for major infection (HR 3.61, IQR 1.61 to 8.06) with a trend towards predicting a composite outcome of mortality or transplantation (HR 2.39, IQR 0.97 to 5.88). Low calculated free testosterone was similarly associated with infection (HR 3.30, IQR 1.46 to 7.46) with a trend towards predicting the composite outcome (HR 2.30, IQR 0.83 to 6.39). Of note, the incidence of transplant was quite low in this study, with only 18 (6.7%) of patients undergoing liver transplantation.
More recently, a double-blinded, single-center RCT was performed by Sinclair et al. investigating intramuscular testosterone undecanoate compared with placebo in 101 men with cirrhosis and low serum testosterone (TT < 12 nmol/L or cFT < 230 pmol/L) [74••]. Participants were followed for 54 weeks following randomization with body composition assessment using dual-energy X-ray absorptiometry. At study conclusion, testosterone-treated subjects (n = 50) had significantly higher mean adjusted difference (MAD) in appendicular lean mass (MAD + 1.69 kg, 95%CI + 0.40 to 2.97 kg); total lean mass (MAD + 4.74 kg, 95%CI + 1.75 to 7.74 kg); total bone mass (MAD + 0.08 kg, 95%CI + 0.01 to 0.15 kg); bone mineral density at the femoral neck (MAD + 0.287 points, 95%CI + 0.140 to 0.434 points); and hemoglobin level (MAD + 1.02 g/dL, 95%CI + 0.150 to 1.89 g/dL). These changes were matched with a decrease in overall body fat mass (MAD − 4.34 kg, 95%CI − 2.04 to − 6.65 kg) and decreased percentage glycosylated hemoglobin (MAD − 0.35%, 95%CI − 0.05 to − 0.54%). No increase in adverse events in the testosterone-treated group was observed, including incidence of hepatocellular carcinoma, new portal vein thrombosis, polycythemia, or prostate disease.
The effects of testosterone supplementation in cirrhotic patients are encouraging but still need to be supported in a larger cohort of patients at multiple centers. In the general population, restoring testosterone to physiological levels is well tolerated with few side effects; further studies in cirrhotic patients will assist in better understanding its safety profile particular to this population. For instance, testosterone supplementation has been associated with fluid retention in patients with poorly controlled congestive heart failure, and existing studies in cirrhotic patients may be underpowered to detect this complication [75]. The impact of pre-transplantation testosterone supplementation on post-transplantation outcomes also requires further investigation, as one retrospective study has shown a lower incidence of early acute allograft rejection and lower histological severity of rejection in patients with low pre-transplantation testosterone levels [76]. It is uncertain whether pre-transplant restoration of testosterone to physiological levels results in increased risk of transplant rejection.
Conclusion
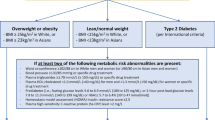
Sarcopenia is a relatively common, multifactorial comorbidity in cirrhotic patients surrounding liver transplantation (Fig. 2). Its presence has been linked to mortality and multiple complications on the wait list and after transplantation. Given its increasing recognition, numerous novel interventions are being investigated to treat or prevent it. However, its ongoing study is limited by heterogeneous definitions and muscle mass cutoffs. In attempting to quantify the “eyeball test” for liver transplantation patients, we all need to be eyeing the same data points. Pragmatic advice for cirrhotic patients is to encourage exercise and attention to nutrition. More advanced therapies require further clinical investigation before their widespread use.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Rosenberg I. Summary comments: epidemiological and methodological problems in determining nutritional status of older persons. Am J Clin Nutr. 1989;50:1231–4.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–23.
Jones SE, Maddocks M, Kon SS, et al. Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax. 2015;70(3):213–8.
Androga L, Sharma D, Amodu A, Abramowitz MK. Sarcopenia, obesity, and mortality in US adults with and without chronic kidney disease. Kidney Int Rep. 2017;2(2):201–11.
Sinclair AJ, Abdelhafiz AH, Rodriguez-Manas L. Frailty and sarcopenia - newly emerging and high impact complications of diabetes. J Diabetes Complicat. 2017;31(9):1465–73.
Caimmi C, Caramaschi P, Venturini A, Bertoldo E, Vantaggiato E, Viapiana O, et al. Malnutrition and sarcopenia in a large cohort of patients with systemic sclerosis. Clin Rheumatol. 2018;37(4):987–97.
Cramer JT, Cruz-Jentoft AJ, Landi F, Hickson M, Zamboni M, Pereira SL, et al. Impacts of high-protein oral nutritional supplements among malnourished men and women with sarcopenia: a multicenter, randomized, double-blinded, controlled trial. J Am Med Dir Assoc. 2016;17(11):1044–55.
Kim JS, Wilson JM, Lee SR. Dietary implications on mechanisms of sarcopenia: roles of protein, amino acids and antioxidants. J Nutr Biochem. 2010;21(1):1–13.
Evans WJ. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. 2010;91(4):1123s–7s.
van Vugt JL, Levolger S, de Bruin RW, van Rosmalen J, Metselaar HJ, JN IJ. Systematic review and meta-analysis of the impact of computed tomography-assessed skeletal muscle mass on outcome in patients awaiting or undergoing liver transplantation. Am J Transplant. 2016;16(8):2277–92.
Englesbe MJ, Patel SP, He K, Lynch RJ, Schaubel DE, Harbaugh C, et al. Sarcopenia and mortality after liver transplantation. J Am Coll Surg. 2010;211(2):271–8.
Durand F, Buyse S, Francoz C, Laouénan C, Bruno O, Belghiti J, et al. Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness on computed tomography. J Hepatol. 2014;60(6):1151–7.
Tandon P, Ney M, Irwin I, Ma MM, Gramlich L, Bain VG, et al. Severe muscle depletion in patients on the liver transplant wait list: its prevalence and independent prognostic value. Liver Transpl. 2012;18(10):1209–16.
Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Shirai H, Yagi S, et al. Impact of skeletal muscle mass index, intramuscular adipose tissue content, and visceral to subcutaneous adipose tissue area ratio on early mortality of living donor liver transplantation. Transplantation. 2017;101(3):565–74.
Waits SA, Kim EK, Terjimanian MN, Tishberg LM, Harbaugh CM, Sheetz KH, et al. Morphometric age and mortality after liver transplant. JAMA Surg. 2014;149(4):335–40.
Han A, Bokshan SL, Marcaccio SE, DePasse JM, Daniels AH. Diagnostic criteria and clinical outcomes in sarcopenia research: a literature review. J Clin Med. 2018;7(4).
Wang CW, Feng S, Covinsky KE, Hayssen H, Zhou LQ, Yeh BM, et al. A comparison of muscle function, mass, and quality in liver transplant candidates: results from the functional assessment in liver transplantation study. Transplantation. 2016;100(8):1692–8.
Yadav A, Chang YH, Carpenter S, et al. Relationship between sarcopenia, six-minute walk distance and health-related quality of life in liver transplant candidates. Clin Transpl. 2015;29(2):134–41.
Giusto M, Lattanzi B, Albanese C, Galtieri A, Farcomeni A, Giannelli V, et al. Sarcopenia in liver cirrhosis: the role of computed tomography scan for the assessment of muscle mass compared with dual-energy X-ray absorptiometry and anthropometry. Eur J Gastroenterol Hepatol. 2015;27(3):328–34.
Wada Y, Kamishima T, Shimamura T, Kawamura N, Yamashita K, Sutherland K, et al. Pre-operative volume rather than area of skeletal muscle is a better predictor for post-operative risks for respiratory complications in living-donor liver transplantation. Br J Radiol. 2017;90(1072):20160938.
Carey EJ, Lai JC, Wang CW, et al. A multicenter study to define sarcopenia in patients with end-stage liver disease. Liver Transpl. 2017;23(5):625–33.
Golse N, Bucur PO, Ciacio O, et al. A new definition of sarcopenia in patients with cirrhosis undergoing liver transplantation. Liver Transpl. 2017;23(2):143–54.
Kalafateli M, Mantzoukis K, Choi Yau Y, Mohammad AO, Arora S, Rodrigues S, et al. Malnutrition and sarcopenia predict post-liver transplantation outcomes independently of the Model for End-stage Liver Disease score. J Cachexia Sarcopenia Muscle. 2017;8(1):113–21.
Nardelli S, Lattanzi B, Torrisi S, Greco F, Farcomeni A, Gioia S, et al. Sarcopenia is risk factor for development of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt placement. Clin Gastroenterol Hepatol. 2017;15(6):934–6.
Bhanji RA, Moctezuma-Velazquez C, Duarte-Rojo A, Ebadi M, Ghosh S, Rose C, et al. Myosteatosis and sarcopenia are associated with hepatic encephalopathy in patients with cirrhosis. Hepatol Int. 2018;12:377–86.
Montano-Loza AJ, Duarte-Rojo A, Meza-Junco J, Baracos VE, Sawyer MB, Pang JXQ, et al. Inclusion of sarcopenia within MELD (MELD-sarcopenia) and the prediction of mortality in patients with cirrhosis. Clin Transl Gastroenterol. 2015;6:e102.
van Vugt JLA, Alferink LJM, Buettner S, et al. A model including sarcopenia surpasses the MELD score in predicting waiting list mortality in cirrhotic liver transplant candidates: a competing risk analysis in a national cohort. J Hepatol. 2017.
Montano-Loza AJ, Meza-Junco J, Prado CM, et al. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2012;10(2):166–73 173.e161.
van Vugt JLA, Buettner S, Alferink LJM, Bossche N, de Bruin RWF, Darwish Murad S, et al. Low skeletal muscle mass is associated with increased hospital costs in patients with cirrhosis listed for liver transplantation-a retrospective study. Transpl Int. 2018;31(2):165–74.
Kaido T, Ogawa K, Fujimoto Y, Ogura Y, Hata K, Ito T, et al. Impact of sarcopenia on survival in patients undergoing living donor liver transplantation. Am J Transplant. 2013;13(6):1549–56.
Cruz RJ Jr, Dew MA, Myaskovsky L, Goodpaster B, Fox K, Fontes P, et al. Objective radiologic assessment of body composition in patients with end-stage liver disease: going beyond the BMI. Transplantation. 2013;95(4):617–22.
DiMartini A, Cruz RJ Jr, Dew MA, Myaskovsky L, Goodpaster B, Fox K, et al. Muscle mass predicts outcomes following liver transplantation. Liver Transpl. 2013;19(11):1172–80.
Krell RW, Kaul DR, Martin AR, Englesbe MJ, Sonnenday CJ, Cai S, et al. Association between sarcopenia and the risk of serious infection among adults undergoing liver transplantation. Liver Transpl. 2013;19(12):1396–402.
Kim G, Kang SH, Kim MY, Baik SK. Prognostic value of sarcopenia in patients with liver cirrhosis: a systematic review and meta-analysis. PLoS One. 2017;12(10):e0186990.
Hamaguchi Y, Kaido T, Okumura S, Fujimoto Y, Ogawa K, Mori A, et al. Impact of quality as well as quantity of skeletal muscle on outcomes after liver transplantation. Liver Transpl. 2014;20(11):1413–9.
Lee CS, Cron DC, Terjimanian MN, Canvasser LD, Mazurek AA, Vonfoerster E, et al. Dorsal muscle group area and surgical outcomes in liver transplantation. Clin Transpl. 2014;28(10):1092–8.
Masuda T, Shirabe K, Ikegami T, Harimoto N, Yoshizumi T, Soejima Y, et al. Sarcopenia is a prognostic factor in living donor liver transplantation. Liver Transpl. 2014;20(4):401–7.
Izumi T, Watanabe J, Tohyama T, Takada Y. Impact of psoas muscle index on short-term outcome after living donor liver transplantation. Turk J Gastroenterol. 2016;27(4):382–8.
Terjimanian MN, Harbaugh CM, Hussain A, Olugbade KO Jr, Waits SA, Wang SC, et al. Abdominal adiposity, body composition and survival after liver transplantation. Clin Transpl. 2016;30(3):289–94.
Underwood PW, Cron DC, Terjimanian MN, Wang SC, Englesbe MJ, Waits SA. Sarcopenia and failure to rescue following liver transplantation. Clin Transpl. 2015;29(12):1076–80.
Shirai H, Kaido T, Hamaguchi Y, et al. Preoperative low muscle mass has a strong negative effect on pulmonary function in patients undergoing living donor liver transplantation. Nutrition. 2018;45:1–10.
Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Shirai H, Yao S, et al. Proposal for new selection criteria considering pre-transplant muscularity and visceral adiposity in living donor liver transplantation. J Cachexia Sarcopenia Muscle. 2018;9(2):246–54.
Jeon JY, Wang HJ, Ock SY, Xu W, Lee JD, Lee JH, et al. Newly developed sarcopenia as a prognostic factor for survival in patients who underwent liver transplantation. PLoS One. 2015;10(11):e0143966.
Chae MS, Moon KU, Jung JY, Choi HJ, Chung HS, Park CS, et al. Perioperative loss of psoas muscle is associated with patient survival in living donor liver transplantation. Liver Transpl. 2018;24(5):623–33.
Carey EJ, Steidley DE, Aqel BA, Byrne TJ, Mekeel KL, Rakela J, et al. Six-minute walk distance predicts mortality in liver transplant candidates. Liver Transpl. 2010;16(12):1373–8.
Dunn MA, Josbeno DA, Schmotzer AR, et al. The gap between clinically assessed physical performance and objective physical activity in liver transplant candidates. Liver Transpl. 2016;22(10):1324–32.
Pattullo V, Duarte-Rojo A, Soliman W, Vargas-Vorackova F, Sockalingam S, Fantus IG, et al. A 24-week dietary and physical activity lifestyle intervention reduces hepatic insulin resistance in the obese with chronic hepatitis C. Liver Int. 2013;33(3):410–9.
Roman E, Torrades MT, Nadal MJ, et al. Randomized pilot study: effects of an exercise programme and leucine supplementation in patients with cirrhosis. Dig Dis Sci. 2014;59(8):1966–75.
Debette-Gratien M, Tabouret T, Antonini MT, Dalmay F, Carrier P, Legros R, et al. Personalized adapted physical activity before liver transplantation: acceptability and results. Transplantation. 2015;99(1):145–50.
Macias-Rodriguez RU, Ilarraza-Lomeli H, Ruiz-Margain A, et al. Changes in hepatic venous pressure gradient induced by physical exercise in cirrhosis: results of a pilot randomized open clinical trial. Clin Transl Gastroenterol. 2016;7(7):e180.
Berzigotti A, Albillos A, Villanueva C, et al. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: the SportDiet study. Hepatology. 2017;65(4):1293–305.
Roman E, Garcia-Galceran C, Torrades T, et al. Effects of an exercise programme on functional capacity, body composition and risk of falls in patients with cirrhosis: a randomized clinical trial. PLoS One. 2016;11(3):e0151652.
•• Zenith L, Meena N, Ramadi A, et al. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin Gastroenterol Hepatol. 2014;12(11):1920–1926.e1922. Improvement of sarcopenia components over relatively short time frame supports inclusion of supervised exercise program into clinical practice.
Zenith L, Qamar H, Myers R, et al. Severe muscle mass loss in cirrhosis: can bedside tools be used to predict a CT or MRI diagnosis of sarcopenia. Can J Gastroenterol. 2013;27(Suppl A):83A.
Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47(11):2473–9.
Tandon P, Ismond KP, Riess K, Duarte-Rojo A, al-Judaibi B, Dunn MA, et al. Exercise in cirrhosis: translating evidence and experience to practice. J Hepatol. 2018;69(5):1164–77.
Chen HW, Dunn MA. Muscle at risk: the multiple impacts of ammonia on sarcopenia and frailty in cirrhosis. Clin Transl Gastroenterol. 2016;7:e170.
Kato M, Miwa Y, Tajika M, Hiraoka T, Muto Y, Moriwaki H. Preferential use of branched-chain amino acids as an energy substrate in patients with liver cirrhosis. Intern Med. 1998;37(5):429–34.
Moriwaki H, Miwa Y, Tajika M, Kato M, Fukushima H, Shiraki M. Branched-chain amino acids as a protein- and energy-source in liver cirrhosis. Biochem Biophys Res Commun. 2004;313(2):405–9.
Tsien C, Davuluri G, Singh D, et al. Metabolic and molecular responses to leucine-enriched branched chain amino acid supplementation in the skeletal muscle of alcoholic cirrhosis. Hepatology. 2015;61(6):2018–29.
Toshima T, Shirabe K, Kurihara T, Itoh S, Harimoto N, Ikegami T, et al. Profile of plasma amino acids values as a predictor of sepsis in patients following living donor liver transplantation: special reference to sarcopenia and postoperative early nutrition. Hepatol Res. 2015;45(12):1170–7.
Kinny-Koster B, Bartels M, Becker S, et al. Plasma amino acid concentrations predict mortality in patients with end-stage liver disease. PLoS One. 2016;11(7):e0159205.
Muto Y, Sato S, Watanabe A, Moriwaki H, Suzuki K, Kato A, et al. Effects of oral branched-chain amino acid granules on event-free survival in patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2005;3(7):705–13.
Kumada H, Okanoue T, Onji M, Moriwaki H, Izumi N, Tanaka E, et al. Guidelines for the treatment of chronic hepatitis and cirrhosis due to hepatitis C virus infection for the fiscal year 2008 in Japan. Hepatol Res. 2010;40(1):8–13.
Hiraoka A, Michitaka K, Kiguchi D, Izumoto H, Ueki H, Kaneto M, et al. Efficacy of branched-chain amino acid supplementation and walking exercise for preventing sarcopenia in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 2017;29(12):1416–23.
•• Uojima H, Sakurai S, Hidaka H, et al. Effect of branched-chain amino acid supplements on muscle strength and muscle mass in patients with liver cirrhosis. Eur J Gastroenterol Hepatol. 2017;29(12):1402–7. Treatment with BCAAs improved muscle strength in ESLD patients when compared with controls. Given low side effect profile, this encourages clinical adoption. However, further US trials with larger number of sarcopenic ESLD patients and longer follow-up are needed.
Qiu J, Thapaliya S, Runkana A, Yang Y, Tsien C, Mohan ML, et al. Hyperammonemia in cirrhosis induces transcriptional regulation of myostatin by an NF-kappaB-mediated mechanism. Proc Natl Acad Sci U S A. 2013;110(45):18162–7.
Nishikawa H, Enomoto H, Ishii A, Iwata Y, Miyamoto Y, Ishii N, et al. Elevated serum myostatin level is associated with worse survival in patients with liver cirrhosis. J Cachexia Sarcopenia Muscle. 2017;8(6):915–25.
Elkina Y, von Haehling S, Anker SD, Springer J. The role of myostatin in muscle wasting: an overview. J Cachexia Sarcopenia Muscle. 2011;2(3):143–51.
•• Becker C, Lord SR, Studenski SA, et al. Myostatin antibody (LY2495655) in older weak fallers: a proof-of-concept, randomised, phase 2 trial. Lancet Diabetes Endocrinol. 2015;3(12):948–57 Novel inhibition of myostatin has shown efficacy in phase II study of elderly, frail, non-cirrhotic patients to decrease sarcopenia. Further studies in ESLD patients are necessary.
Grossmann M, Hoermann R, Gani L, Chan I, Cheung A, Gow PJ, et al. Low testosterone levels as an independent predictor of mortality in men with chronic liver disease. Clin Endocrinol. 2012;77(2):323–8.
Moctezuma-Velazquez C, Low G, Mourtzakis M, et al. Association between low testosterone levels and sarcopenia in cirrhosis: a cross-sectional study. Ann Hepatol. 2018;17(4):615–23.
Sinclair M, Gow PJ, Grossmann M, Shannon A, Hoermann R, Angus PW. Low serum testosterone is associated with adverse outcome in men with cirrhosis independent of the model for end-stage liver disease score. Liver Transpl. 2016;22(11):1482–90.
•• Sinclair M, Grossmann M, Hoermann R, Angus PW, Gow PJ. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: a randomised controlled trial. J Hepatol. 2016;65(5):906–913. Treatment of low testosterone in ESLD patients is associated with decreased sarcopenia, but further studies in US population are needed before clinical adoption can be recommended.
Hassan J, Barkin J. Testosterone deficiency syndrome: benefits, risks, and realities associated with testosterone replacement therapy. Can J Urol. 2016;23(Suppl 1):20–30.
Sinclair M, Angus PW, Gow PJ, Hoermann R, Mogilevski T, Grossmann M. Low-serum testosterone levels pre-liver transplantation are associated with reduced rates of early acute allograft rejection in men. Transplantation. 2014;98(7):788–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
John Montgomery declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Frailty and Gerontology
Rights and permissions
About this article
Cite this article
Montgomery, J., Englesbe, M. Sarcopenia in Liver Transplantation. Curr Transpl Rep 6, 7–15 (2019). https://doi.org/10.1007/s40472-019-0223-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-019-0223-3