Abstract
Adult right-lobe living-donor liver transplantation is a technically demanding operation. Since it was conducted for the first time in 1996, its application has been expanding tremendously and it has become the mainstay at most Asian liver transplant centers. This is the result of its success rate for both donors and recipients and because it has helped alleviated the severe shortage of deceased-donor liver grafts. Improved understanding of the anatomy of the liver and advances in surgical techniques has dramatically reduced the complication rates. Recipients now can have excellent long-term survival, while the risks borne by the donors are acceptable. This article presents the surgical tips and tricks for donor right hepatectomy, the back-table procedure and recipient operation. The management of small-for-size liver grafts and methods of biliary reconstruction are also discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver transplantation is a life-saving procedure for patients with end-stage liver diseases. Unfortunately, the demand for liver transplantation always exceeds the supply of liver grafts donated by the deceased. As a result, living-donor liver transplantation (LDLT) has been developed as an alternative option. LDLT was initially limited to pediatric patients because of graft size restrictions. In order to extend the benefits of LDLT to adult patients and best assure adequate graft size, the use of the right liver lobe was initiated by The University of Hong Kong in 1996 [1]. Following successful reports from the first series of eight cases in 1997 [2], right-lobe LDLT has developed rapidly and has been adopted by many transplant programs around the world. Through careful selection of donors with safe profiles, right-lobe LDLT has been successfully achieving satisfactory recipient outcomes [3–11].
In Asia, a region suffering an extreme shortage of liver grafts, LDLT has had the most significant impact thus far. The availability of right-lobe LDLT has been the driving force for a drastic increase in LDLTs in recent years. In 2005, LDLT accounted for 90 % of the 1,497 liver transplants performed in Asia (excluding Mainland China) [12]. In 2012, more than half of the liver transplants in Hong Kong were LDLTs and about 90 % were right-lobe LDLTs for adults.
Right-lobe LDLT is one of the most complicated and technically demanding surgical procedures. The posttransplant morbidity and reoperation rates were high in the first series of eight recipients [2]. Since then, significant advances in technique and management have been made, including a better understanding of the minimum graft size requirement and anatomic variants of the right liver lobe, improved selection criteria for donors and recipients, and technical modifications, particularly in venous outflow and biliary reconstructions [11, 13–15]. Overall, lessons learned in the first 100 cases resulted in dramatic improvement in donor and recipient outcomes [16]. Now an excellent graft survival rate of over 90 % can be achieved even in high-risk recipients.
This article discusses the tips and tricks for LDLT, including donor, back-table and recipient procedures, with emphasis on recent technical advances.
Donor Right Hepatectomy
Most complications suffered by recipients of LDLT originate from donor operations. Moreover, a steatotic graft could also be a source of morbidity. A recent study showed that a graft with 20–50 % macrovesicular steatosis was associated with significantly higher chances of biliary complication and delayed graft function [17•]. Therefore, results of preoperative imaging of the donor’s liver should be studied thoroughly and liver biopsy should be considered if the degree of steatosis is uncertain. Livers with >20 % macrovesicular steatosis should be rejected. At the authors’ center, routine preoperative biliary imaging is replaced by routine operative cholangiographies of good quality, and all right-lobe grafts contain the middle hepatic vein (MHV).
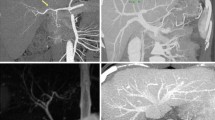
Preoperative three-phase contrast-enhanced computed tomography scans must be studied thoroughly. The minimum volume required for a liver remnant is 30 %. A recent study by Kim et al. [18•] suggested that it might be safe to reduce the volume threshold to 23 % in selected donors, but reduction of threshold has not yet gained recommendation by others. The authors’ center uses a newly derived University of Hong Kong formula to calculate the estimated standard liver volume (ESLV) and the predicted graft weight.[19•]. Other key characteristics should be noted, too. Specifically, appreciation of sizeable (>5 mm) inferior right hepatic veins (IRHVs) and the hepatic venous drainage in segment 4b is of utmost importance. For type-3 Nakamura drainage pattern, transection of the MHV should be made close to it. Dissection must be meticulous to avoid damage to the venous drainage and prevent significant congestion of segment 4 [20].
Proper positioning of the donor during operation is very important in preventing unnecessary morbidities. The upper limbs should be adducted to avoid brachial plexus injury and attention must be paid to pressure points at the occiput, knees and ankles to prevent alopecia and common peroneal nerve palsy. Second assistants should not lean over the donor’s lower limbs to avoid putting pressure on them. Prophylactic antibiotic (Augmentin™; GlaxoSmithKline, London, UK) and proton pump inhibitor are given at the induction of anesthesia.
The donor operation starts with a right subcostal incision with a sternal midline external incision. Intraoperative Doppler ultrasonography is done to delineate the vascular anatomy. Cholecystectomy is performed and the cystic duct is cannulated with a balloon catheter for operative cholangiography. In order not to damage any aberrant branch of the bile duct, the cystic duct is not cannulated before the whole gallbladder is detached from the liver. The hilar plate is lowered by sharp dissection, and the exact location of the lower border of the right hepatic duct (RHD) is clearly visualized. The division plane should be 3–4 mm away from the biliary confluence and a large metallic clip (Ethicon, Edinburgh, UK) is used to mark the site externally to correlate it with the findings of operative cholangiography. The balloon is inflated with 1 ml of air and the first operative cholangiography (anterior-posterior view) is performed. Then the C arm of the X-ray machine is rotated counterclockwise for a ‘true’ anterior-posterior view (right anterior-oblique) of the biliary system. This maneuver avoids overlapping of the biliary confluence so the exact site of division can be determined.
After the first cholangiography, the planned site of RHD transection is marked with diathermy on the liver parenchyma just above the hilar plate and hilar dissection is then performed. The right hepatic artery (RHA) should be palpated for location and the dissection should be close to the vessel. Any tiny branches, nerves and lymphatics should be ligated. The dissection should not go beyond the right side of the common hepatic duct (CHD). The right-sided hilar plate and the RHA should be completely separated and the latter slung up with a vessel loop. The hepatic artery (HA) in segment 4 should be preserved. The right portal vein (RPV) is dissected after the RHA has been dissected. All tiny caudal branches should be ligated in order to get extra length for anastomosis. The RPV is then slung up with another vessel loop. Mobilization of the right liver lobe is achieved by dividing the triangular and coronary ligaments. Excessive rotation may result in inflow and outflow occlusions and therefore should be avoided. Intermittent rotation may be required, preferably not more than 20 min each time. If the right adrenal gland adheres to the right liver lobe, which is often the case, dissection must be conducted with meticulous attention to prevent tearing and subsequent bleeding. Any IRHVs ≥5 mm should be preserved to the liver graft. Dissection between the liver and the retrohepatic inferior vena cava (IVC) should be slow and tiny short hepatic veins (HVs) should be ligated individually. The IVC ligament contains vessels and should be sutured after ligation as simple ligature can slip easily, resulting in significant bleeding. The right hepatic vein (RHV) is then encircled with a vessel loop. The anterior surface of the retrohepatic IVC should be cleared beyond the midline. A nylon tape is placed passing between the roots of the RHV and MHV.
The RHA and the RPV are clamped with nontraumatic vascular clamps for temporary inflow control. The ischemic demarcation is visualized and marked by diathermy. Intraoperative ultrasonography must be done to ascertain the patency of left-sided vessels. The line of demarcation is usually poorly defined between segments 8 and 4b at the cephalic end and is helped by extrahepatic dissection of the RHV and MHV. The transection line should be towards the root of the MHV. The caudal end of transection is directed towards the planned RHD transection site, which has been marked after cholangiography.
A Cavitron® ultrasonic surgical aspirator (CUSA) is used for precise liver transection without inflow or outflow occlusion. A fine precision tip (1.14 mm in diameter) is preferable to an ordinary microtip (1.54 mm in diameter). The CUSA is set at 70 % of the maximum amplitude, with irrigation with normal saline at about 4–6 ml/min, and 20 % of the maximum suction power. Hemostasis is done with fine sutures, metallic clips or an argon beam coagulator. Usually a segment-4a HV is visualized after 4–5 cm of transection. After dividing this vein, the main trunk of the MHV is exposed and the transection plane is on the left side of the MHV. Any segment-4a HVs >3 mm should be sutured after ligation. The transection plane is oblique or nearly horizontal, so following the MHV is crucial.
At the cephalic end of the transection, the MHV is exposed until the junction of the left hepatic vein. Studying the preoperative computed tomography and intraoperative ultrasound scans is of utmost importance. Any sizeable segment-4b HVs should be preserved to the liver remnant. If there is a segment-3 HV joining the MHV, the former must be safeguarded.
At the caudal and inferior end of the transection, the hilar plate should not be denuded of liver tissue so as to prevent ischemia. Complete hilar plate encircling can be performed safely without damaging the right-sided inflow vessels [21]. A 3.5-Fr Argyle™ catheter, which is radiopaque on cholangiography, is used to encircle the whole right-sided hilar plate. A large metallic clip is applied to the RHD just next to the catheter. The clip and the catheter can serve as a guide to the exact site of RHD transection following another cholangiography (right anterior-oblique view). The RHD should be cut in parallel to the transection plane of the liver and it should be a sharp cut in one go.
The RHD stump is repaired with 6/0 polydioxanone (PDS) suture. After completion of the transection, cholangiography is performed again to confirm the patency of the left ductal system. Methylene blue test is carried out with gentle injection upon conclusion of the procedure to detect leakage. The cystic duct is tied with a 2/0 Vicryl™ suture after removal of the balloon catheter. The nylon tape previously placed between the RHV and the MHV serves the Hanging Maneuver to guide the plane of liver transection (Fig. 1).
Graft delivery starts with clamping and division of the RHA. The RPV is then clamped in a plane perpendicular to its axis to avoid narrowing of the portal vein (PV) bifurcation. A large bulldog clamp is applied to the graft PV to prevent vigorous back bleeding. The graft PV is then divided, with a 2-mm stump left above the clamp. It is necessary to expose the roof of the MHV, which is to be controlled by a vascular stapler (TA 30, V3, 2.5 mm; United States Surgical, Norwalk, CT, USA). The right liver lobe is rotated and another vascular stapler is used to control the RHV. The IRHV is also controlled in this manner. The IRHV, RHV and MHV are divided sequentially. The right-lobe graft is then delivered and put into ice sludge immediately.
The RPV stump in the donor is sutured by running 6/0 Prolene™ suture back and forth, and ultrasonography is performed to ascertain the patency of left-sided vessels. Diluted methylene blue is instilled into the bile duct through the balloon catheter to detect bile leakage at the stump and the transection surface. Later, the catheter is removed and the cystic duct is doubly ligated with 2/0 Vicryl suture.
The falciform ligament is reconstituted with nonabsorbable sutures to avoid twisting of the vessels. Abdominal drain is not placed routinely. The wound is infiltrated with 0.5 % levobupivacaine between the fascial layers and closed with PDS suture. The subcutaneous layer is closed with 2/0 Vicryl suture and the skin is closed with absorbable subcuticular sutures.
Back-Table Procedure
The graft is flushed with histidine-tryptophan-ketoglutarate solution via the RPV. The color of the graft must be inspected and areas not completely clear of blood should gain more attention. Retrograde flushing via the HVs can be of help. If there are two separate RPV openings, flushing should be done by cannulation of both openings simultaneously.
There is a 10–35 % chance of PV anomaly in a right liver lobe [22–24] and techniques have been devised to tackle such anomalies in right-lobe grafts, including the use of autologous vein (e.g., the great saphenous vein) grafts procured from donors or recipients or cryopreserved cadaveric vein grafts. However, vein procurement from the donor prolongs the donor operation and may cause donor morbidities, whereas that from the recipient is not always possible (e.g., when the recipient has edematous lower limbs). Additionally, the long-term results of cryopreserved vein grafts are suboptimal. Dual PV venoplasty [25] is another technique that can be employed. It uses a portion (around 1 cm long) of the main portal vein (MPV) of the recipient as an ‘interpositional graft’, which is anastomosed to the venoplasty with a 6/0 Prolene suture. A leakage test can be done and additional stitches can be added at the bloodless field before graft implantation. Dual PV venoplasty can expedite the recipient operation as PV anastomosis will be without size mismatch and the orientation will be perfect in preventing twisting.
The donor right hepatectomy graft requires hepatic venoplasty between the RHV and the MHV. A triangular cuff is fashioned for a single anastomosis to the recipient IVC [14, 26]. If the distance between the venoplasty and the IRHV is ≤3 cm, the IRHV is also incorporated to form a wide single cuff.
Recipient Operation
During operation, the recipient’s upper limbs should be adducted to avoid brachial plexus injury and second assistants should not lean over the lower limbs to avoid putting pressure on them. A generous bilateral subcostal incision with midline sternal extension is essential for adequate exposure. Veno-veno bypass is no longer used in current practice. All hilar varices should be ligated and divided and all three HAs should be dissected as high as possible. A nontraumatic vascular clamp (S&T, Neuhausen, Switzerland) is best for controlling the artery. Dissection of the CHD should also be as high as possible, but not into the hilar plate. Excessive skeletonization of the CHD must be prohibited to avoid ischemia. In the case of fulminant hepatic failure, the patient is very unstable due to massive release of inflammatory cytokines into the systemic circulation during mobilization, so removal of the diseased liver should be expeditious. A temporary portocaval shunt may be used to prevent excessive bowel wall edema and congestion, which otherwise would render subsequent hepaticojejunostomy (HJ) difficult or impossible. Stringent monitoring of the level of blood glucose and measures to prevent cerebral edema by the anesthesiologist are required.
The retrohepatic IVC is fully mobilized after sutured ligation of all lumbar veins. Bilateral diaphragmatic veins should be sutured after ligation in order to get an extra length of the suprahepatic IVC. A nylon tape and a Rummel tourniquet are applied to occlude the infrahepatic IVC and an Ulrich Swiss® clamp is applied to occlude the suprahepatic IVC. The native RHV stump is reopened (i.e. at the ‘base’ of the venoplasty of the graft HVs) and a horizontal transverse incision is made according to the ‘height’ of the venoplasty. The incision must not be extended beyond the lateral wall of the IVC; otherwise the IVC may be twisted and pulled up, resulting in poor venous outflow. In order to achieve best venous outflow, any IRHVs >5 mm should be preserved in the graft and anastomosed separately to the IVC if the distance between the venoplasty and the IRHV is >3 cm.
PV anastomosis is done carefully in order to avoid excessive length. HA anastomosis is performed after reperfusion of the graft by microvascular surgeons under an operative microscope [27]. Both hands of the second assistant should be placed on an abdominal pack and retract the transverse colon, stomach and small bowel towards the patient’s left leg to expose the deep liver hilum. Routine daily bedside Doppler is required until the day of discharge to check for vascular thrombosis.
Management of Small-for-Size Grafts
The size of liver grafts from living donors is almost universally small for adult recipients [28], so a key focus of adult LDLT must be techniques to prevent small-for-size syndrome. Adequate portal flow and pressure are essential for graft regeneration. Routine portal flowmetry and manometry guiding portal inflow modulation should be performed for any graft <50 % of the ESLV [29••, 30]. Manometry is performed by cannulation of the inferior mesenteric vein, or by direct PV puncturing if there are significant retroperitoneal varices prohibiting dissection of the inferior mesenteric vein. With unimpeded venous outflow (as in right-lobe grafts containing the MHV), the portal pressure is not high even if the portal flow is >250 ml/100 g/min. Portal inflow modulation can be done by splenic artery ligation if the portal pressure is >20 mmHg [31•]. In patients with long-standing MPV thrombosis, spontaneous shunting may develop, resulting in portal hypoperfusion after transplantation [32]. Detailed study of preoperative imaging results may reveal some spontaneous shunts (e.g., splenorenal shunt at left renal vein and large engorged coronary vein at the lesser sac). If the portal flow is <100 ml/100 g/min and the portal pressure is low, shunt ligation can help to augment the flow and the pressure. Occasionally, a graft <35 % of the ESLV can be safely used [33••]. At the authors’ center, 5.8 % of the right-lobe grafts transplanted were <35 % of the ESLV of the recipients (unpublished data). These relatively small grafts are safe for patients with low Model for End-stage Liver Disease scores and without significant portal hypertension (i.e. patients with unresectable hepatocellular carcinomas). Further lowering the safety limit of the graft-weight-to-ESLV ratio allows the use of smaller grafts (i.e. left-lobe grafts), thereby reducing donor risks, while not jeopardizing recipient outcomes [34•].
Another major problem posed by a small-for-size graft is the big gap between the graft hilar structure and the recipient hepatoduodenal ligament. This gap means there is inadequate length for tension-free HA, PV and duct-to-duct biliary anastomoses. In such cases, the use of the caudal shifting technique should be considered [35]. The concept of caudal shifting is simple. During IVC-venoplasty anastomosis, while the cranial part of the original RHV stump is partially or totally closed, a new vertical incision in the caudal part of the RHV stump is made, extending downwards for 2 cm. A new triangular venotomy is then made according to the size of the venoplasty and the IVC-venoplasty anastomosis can be performed in a usual manner. The technique brings the graft downwards for 2 cm and allows tension-free anastomoses without the use of interpositional conduits.
Biliary Reconstruction
Duct-to-duct anastomosis (DDA) and HJ are the two most common methods of biliary reconstruction. At the authors’ center, DDA is preferred [33••] unless the native bile duct is not suitable or should not be used (e.g., in the presence of primary sclerosing cholangitis).
Technique of DDA
At the end of graft implantation when all vascular anastomoses are complete and hemostasis has been achieved, biliary reconstruction is performed. Bleeding from the graft hepatic duct is treated by plication of the bleeding points with fine suture rather than by diathermy. If there are two or more adjacent ductal openings (<5 mm apart), DDA is done with incorporation of the hilar plate [36]; ductoplasty might cause strangulation of the surrounding tissue and is therefore not advisable. End-to-end anastomosis is performed with 6/0 PDS continuous suture for the posterior wall. A short segment of cannula (3.5-Fr Argyle catheter) is temporarily placed across the anastomosis until anastomosis at the anterior wall is completed with 6/0 PDS multiple interrupted suture. The cannula is removed before the sutures are tied up. The placement of abdominal drain is not a routine practice. If two ductal openings are >5 mm apart, biliary reconstruction should be performed with one DDA and one HJ or two HJs.
One pitfall in recipient total hepatectomy is preserving a CHD that is ‘too long,’ with the fear that not enough length is left for a tension-free DDA. An excessively long CHD would leave an ischemic segment, causing ischemic anastomotic stricture or even bile leakage. In fact, the caudal shifting technique is useful if the CHD happens to be not long enough.
Technique of HJ
The RHD is anastomosed to a Roux jejunal loop of sufficient length (>60 cm) prepared with staplers and running in a retrocolic or preferably retrogastric route. The anastomosis uses 6/0 PDS continuous suture for the posterior wall and 6/0 PDS multiple interrupted suture for the anterior wall. A side-to-side jejunojejunostomy is then made at least 40 cm from the anastomosis with single-layer 5/0 PDS continuous suture. All mesenteric windows must be closed meticulously with nonabsorbable sutures to prevent internal bowel herniation.
Conclusion
Right-lobe LDLT is an extremely complicated and technically demanding operation and is the preferred approach to LDLT for many transplant centers. For the best recipient outcomes, every step in donor and recipient operations must be perfect, which requires the accumulation of significant experience [33••]. It is our hope that these “Technical Tips and Tricks for Living Donation” will aid in a greater understanding of the physiology and anatomy of the liver and in the refinement of surgical skills, thereby contributing to the improvement of LDLT outcomes. A summary of technical tips and tricks for donor and recipient operations can be found in Table 1.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lo CM, Fan ST, Liu CL, et al. Extending the limit on the size of adult recipient in living donor liver transplantation using extended right lobe graft. Transplantation. 1997;63:1524–8.
Lo CM, Fan ST, Liu CL, et al. Adult-to-adult living donor liver transplantation using extended right lobe grafts. Ann Surg. 1997;226:261–9. discussion 269-70.
Wachs ME, Bak TE, Karrer FM, et al. Adult living donor liver transplantation using a right hepatic lobe. Transplantation. 1998;66:1313–6.
Marcos A, Fisher RA, Ham JM, et al. Right lobe living donor liver transplantation. Transplantation. 1999;68:798–803.
Trotter JF, Wachs M, Everson GT, Kam I. Adult-to-adult transplantation of the right hepatic lobe from a living donor. N Engl J Med. 2002;346:1074–82.
Bak T, Wachs M, Trotter J, et al. Adult-to-adult living donor liver transplantation using right-lobe grafts: results and lessons learned from a single-center experience. Liver Transpl. 2001;7:680–6.
Boillot O, Dawahra M, Mechet I, et al. Liver transplantation using a right liver lobe from a living donor. Transplant Proc. 2002;34:773–6.
Nakamura T, Tanaka K, Kiuchi T, et al. Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation. 2002;73:1896–903.
Olthoff KM, Merion RM, Ghobrial RM, et al. Outcomes of 385 adult-to-adult living donor liver transplant recipients—a report from the A2ALL consortium. Ann Surg. 2005;242:314–25.
Fan ST, Lo CM, Liu CL, et al. Safety of donors in live donor liver transplantation using right lobe grafts. Arch Surg. 2000;135:336–40.
Fan ST, Lo CM, Liu CL. Technical refinement in adult-to-adult living donor liver transplantation using right lobe graft. Ann Surg. 2000;231:126–31.
de Villa V, Lo CM. Liver transplantation for hepatocellular carcinoma in Asia. Oncologist. 2007;12:1321–31.
Lo CM, Fan ST, Liu CL, et al. Minimum graft size for successful living donor liver transplantation. Transplantation. 1999;68:1112–6.
Lo CM, Fan ST, Liu CL, Wong J. Hepatic venoplasty in living-donor liver transplantation using right lobe graft with middle hepatic vein. Transplantation. 2003;75:358–60.
Liu CL, Lo CM, Chan SC, Fan ST. Safety of duct-to-duct biliary reconstruction in right-lobe live-donor liver transplantation without biliary drainage. Transplantation. 2004;77:726–32.
Lo CM, Fan ST, Liu CL, et al. Lessons learned from one hundred right lobe living donor liver transplants. Ann Surg. 2004;240:151–8.
Li HY, Wei YG, Li B, et al. Impact of graft steatosis on the post-transplantation biliary complications for living donor liver transplant recipients in China. Hepato-Gastroenterol. 2012;59:1194–7. The use of liver grafts with 20-50 % fatty change should be balanced between donor risks and recipient benefits. On multivariate analysis, the use of such grafts significantly increased the incidence of posttransplant biliary complications.
Kim SH, Kim YK, Lee SD, Park SJ. Selection and outcomes of living donors with a remnant volume less than 30 % after right hepatectomy. Liver Transpl. 2013;19:872–8. The minimum size of liver remnant after donation of the right liver lobe is a controversial subject. This paper concludes that donor right hepatectomy preserving the middle hepatic vein with a remnant-to-total-liver-volume ratio of <30 % can be safely indicated for carefully selected living donors less than 50 years old with no or mild steatosis.
Chan SC, Lo CM, Chok KS, et al. Validation of graft and standard liver size predictions in right liver living donor liver transplantation. Hepatol Int. 2011;5:913–7. This paper validates the University of Hong Kong formula. The formula, which is used to calculate the estimated standard liver volume in Chinese patients and is found to be very accurate, reads: [standard liver weight (g) = 218 + body weight (kg) × 12.3 + 51 (if male); standard liver volume is obtained by a conversion factor of 1.19 ml/g].
Chan SC, Lo CM, Liu CL, et al. Tailoring donor hepatectomy per segment 4 venous drainage in right lobe live donor liver transplantation. Liver Transpl. 2004;10:755–62.
Soejima Y, Fukuhara T, Morita K, et al. A simple hilar dissection technique preserving maximum blood supply to the bile duct in living donor liver transplantation. Transplantation. 2008;86:1468–9.
Marcos A, Orloff M, Mieles L, et al. Reconstruction of double hepatic arterial and portal venous branches for right-lobe living donor liver transplantation. Liver Transpl. 2001;7:673–9.
Sato K, Sekiguchi S, Watanabe T, et al. The use of recipient superficial femoral vein as a venous graft for portal vein reconstruction in right lobe living donor liver transplantation. Transplant Proc. 2009;41:195–7.
Xu MQ, Yan LN, Li B, et al. Surgical procedures for management of right portal venous branching in right lobe living donor liver transplantation. Transplant Proc. 2008;40:1529–33.
Chan AC, Lo CM, Chok KS, et al. Life made easy: simplifying reconstruction for dual portal veins in adult right lobe live donor liver transplantation. Hepatobiliary Pancreat Dis Int. 2010;9:547–9.
Liu CL, Zhao Y, Lo CM, Fan ST. Hepatic venoplasty in right lobe live donor liver transplantation. Liver Transpl. 2003;9:1265–72.
Wei WI, Lam LK, Ng RW, et al. Microvascular reconstruction of the hepatic artery in live donor liver transplantation—experience across a decade. Arch Surg-Chicago. 2004;139:304–7.
Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: Definition, mechanisms of disease and clinical implications. Am J Transplant. 2005;5:2605–10.
Chan SC, Lo CM, Ng KK, et al. Portal inflow and pressure changes in right liver living donor liver transplantation including the middle hepatic vein. Liver Transpl. 2011;17:115–21. This important paper shows that in a small right-lobe graft containing the middle hepatic vein, the portal pressure remains low despite the high portal flow. It demonstrates the correlation between portal flow and pressure and illustrates the importance of a wide and unobstructed outflow.
Man K, Fan ST, Lo CM, et al. Graft injury in relation to graft size in right lobe live donor liver transplantation—a study of hepatic sinusoidal injury in correlation with portal hemodynamics and intragraft gene expression. Ann Surg. 2003;237:256–64.
Chan SC, Lo CM, Chok KS, et al. Modulation of graft vascular inflow guided by flowmetry and manometry in liver transplantation. Hepatobiliary Pancreat Dis Int. 2011;10:649–56. This article reports four cases with different clinical scenarios in right-lobe living-donor liver transplantation. It highlights the usefulness of the proposed flowmetry- and manometry-guided inflow modulation in tackling portal hyper- and hypoperfusion.
Chan SC, Lo CM, Chik BH, et al. Flowmetry-based portal inflow manipulation for a small-for-size liver graft in a recipient with spontaneous splenorenal shunt. Clin Transplant. 2010;24:410–4.
Chan SC, Lo CM, Ng KK, Fan ST. Alleviating the burden of small-for-size graft in right liver living donor liver transplantation through accumulation of experience. Am J Transplant. 2010;10:859–67. This landmark paper shows that center experience in right-lobe living-donor liver transplantation is of utmost importance. It significantly decreased hospital mortality (Era I the first 50 cases vs. Era II the later 270 cases). Furthermore, with mature management of small-for-size syndrome, recipient survival was excellent despite the use of smaller grafts.
Chan SC, Fan ST, Chok KS, et al. Increasing the recipient benefit/donor risk ratio by lowering the graft size requirement for living donor liver transplantation. Liver Transpl. 2012;18:1078–82. This paper concludes that the graft-weight-to-standard-liver-volume (GW/SLV) ratio can be less than 40 % without jeopardizing recipient outcomes. It hypothesizes that if GW/SLV can be further lowered safely, more left-lobe grafts can be used and donor safety can be enhanced without compromising recipient outcomes.
Fan ST. Caudal shifting of hepatic vein anastomosis in right liver living donor liver transplantation. Hepatobiliary Pancreat Dis Int. 2008;7:654–7.
Fan ST. Living donor liver transplantation. 2nd ed. Singapore: World Scientific Publishing; 2011. p. 268.
Compliance with Ethics Guidelines
Conflict of Interest
Kenneth S. H. Chok and Chung Mau Lo declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chok, K.S.H., Lo, C.M. Technical Tips and Tricks for Living Donations. Curr Transpl Rep 1, 61–67 (2014). https://doi.org/10.1007/s40472-013-0007-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-013-0007-0