Abstract
Living kidney donation is an important option for patients with end-stage renal disease (ESRD), and has improved life expectancy and quality for patients otherwise requiring maintenance dialysis or deceased-donor transplantation. Given the favorable outcomes of live donation and the shortage of organs to transplant, individuals with potentially unfavorable demographic and clinical characteristics are increasingly being permitted to donate kidneys. While this trend has successfully expanded the live donor pool, it has raised concerns as to which acceptance criteria are safe. This review aims to summarize the existing literature on the outcomes of transplantation from medically complex living kidney donors, including both donor and recipient outcomes when available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
End-stage renal disease (ESRD) is a highly prevalent cause of morbidity and mortality. At the end of 2011, over 615,000 Americans were living with ESRD [1]. Among options for renal replacement therapy, kidney transplantation is superior to dialysis with regard to mortality, morbidity, and quality of life. Although over 98,000 individuals are currently listed for kidney transplantation in the United States, demand for the organ outweighs supply by nearly an order of magnitude [2]. This disparity would be even greater, were it not for individuals who donate a kidney to benefit their relatives, friends, or complete strangers. In the United States, 34 % of all kidney transplants performed in 2012 were from living donors [2].
Recipients of live donor kidneys have better graft and patient survival compared to those receiving deceased donor organs because cold ischemia times are shorter, donors are generally healthier, and mechanisms of renal injury related to post-mortem procurement are avoided. Waiting times for deceased donor organs are often many years long, so living donation also minimizes dialysis time for the recipient.
The increasing familiarity with live donation and the generally successful outcomes of live donation to date have led the transplant community to loosen eligibility criteria for potential donors. Consequently, a growing proportion of today’s live donors have medical or demographic traits that may have once rendered them ineligible for donation. Such donors have been variably labeled as “marginal donors” or “expanded criteria donors” [3], although the term “medically complex donors” is preferred [4].
This relaxation of exclusion criteria has been coincident with the worsening obesity epidemic, and subsequently, has led to an older, more overweight group of live donors, with higher rates of glucose intolerance [5•]. As of 2008, an estimated one-quarter of living US donors had medical conditions potentially associated with future health risk [6•]. Therefore, it has become increasingly important that donor candidates receive accurate counseling about the potential risks of donation.
Toward this end, an international team convened in Amsterdam in 2004 to establish international standards for donor evaluations, although many recommendations lacked strong evidence and were therefore based on expert consensus [7]. Although the United Network for Organ Sharing (UNOS) policies for donor evaluations have recently been updated [8], conclusive data still often remains elusive and many specific decisions are left up to individual transplant centers. As a result, significant variability still exists among different institutions’ approaches to donor evaluations in the United States [9, 10] and abroad [11]. Decisions to accept or reject a given donor, therefore, continue to rely on a combination of scientific decision-making and individual provider judgment, although a Kidney Disease: Improving Global Outcomes (KDIGO) working group is reviewing the current state of evidence, with plans to release living donor guidelines in 2014 [12].
This article reviews the recent literature on the outcomes of living kidney transplantation from medically complex donors, with attention to implications for both donor and recipient.
Overall Outcomes of Living Donors
The medical outcomes of living donors have been a topic of interest for many years. Physiologic studies have demonstrated adaptive hypertrophy and increased GFR in the remaining kidney, within days of the nephrectomy. Post-donation donor GFR typically stabilizes at over 70 % of the pre-donation value in longitudinal follow up [13]; previous, less favorable estimates of post-nephrectomy donor GFR are based on small samples with short-term follow-up, and therefore may not reflect full compensation over time [14].
This adaptation translates into favorable outcomes for living donors. A provocative Swedish publication in 1997 reported that 430 donors had greater life expectancy than the general population, although this study did not control for important donor-specific factors [15]. Another landmark study from the University of Minnesota in 2009 reported a similar rate of survival between 3,698 living donors (98 % Caucasian) and controls from the NHANES cohort. In this study, rates of incident ESRD were also lower in the donor group, compared with the national Caucasian population (180 versus 268 cases per million persons per year). In addition, a more carefully studied subset of former donors within this cohort had higher quality of life scores than the general population [16].
Additional studies corroborate overall favorable long-term outcomes for kidney donors [6•, 17–20], suggesting that donation does not introduce substantial kidney-specific morbidity such as ESRD, hypertension, proteinuria, or anemia [20, 21], depression [22] or malignancy [23]. With the evolution in surgical techniques for donor nephrectomy [24], perioperative outcomes are excellent [6•, 20, 25••, 26–29] and continue to improve, despite increasing donor comorbidity [29]. Survival from nephrectomy is outstanding, with a perioperative death rate of 0.03 % [6•, 25••].
While emerging prospective data suggests that donors share metabolic abnormalities with CKD patients six months after donation [30••], it is unknown whether incident hyperuricemia or hyperparathyroidism in otherwise healthy donors correspond with clinically meaningful long-term outcomes [31]. Many have questioned whether or not standard definitions of CKD are applicable to living donors, who attain a reduced GFR via a much different mechanism than patients with hypertension, diabetes, or other intrinsic renal diseases [32, 33, 34•].
Thus, living kidney donors—as a whole—have favorable outcomes with respect to their surgery and long-term health and survival. The majority of existing studies have included young, healthy Caucasian donors in particular, who fare excellently following donation. Whether this holds true for medically complex donors, however, is less clear.
Medical Complexities at Donation, and Associated Outcomes
Reduced GFR.
The 2004 Amsterdam Forum recommended that all potential living donors undergo GFR testing as part of their workup, by either creatinine-based calculations or isotope-based measurements. The report advised that acceptable donors should have GFR either above 80 mL/min or within two standard deviations of the normal GFR range for their age and gender [7].
Although such guidelines aim to protect individuals from developing ESRD, the progression of GFR in former donors does not necessarily match that of the general population [8]. As compared with cross-sectional data suggesting an expected decrease in creatinine clearance of 5–10 mg/min with each passing decade of life [35], some studies have demonstrated a gradual post-donation rise in GFR that persists for years after donation [16, 21]. The eGFR pattern may be influenced by factors such as donor age and kidney function, but it appears that population-based prediction rules for GFR decline—which include people with kidney disease and strong risk factors for kidney disease—may not apply to carefully screened donors.
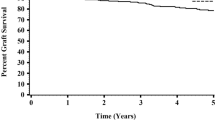
Young et al.’s 2008 literature review on donor outcomes included only two studies of donors with low pre-donation GFR; one was discounted due to presumed reporting errors [36]. In a more recent study, regression analyses demonstrated that higher pre-donation eGFR was protective against developing CKD, as defined by K/DOQI guidelines (HR = 0.952, p = 0.0199). Perhaps not unexpectedly, freedom-from-CKD curves significantly favored donors with higher baseline eGFR over 21 years, although few subjects remained at risk of the primary outcome after five years of follow-up [37].
Data on recipients of grafts with lower baseline function is also sparse. A 2009 meta-analysis of transplant recipients from “expanded criteria living donors” included seven studies featuring donors with reduced renal function, with six different definitions of low GFR. The studies’ outcomes of interest were also heterogeneous, including graft survival, death-censored graft survival, patient survival, and graft function by either serum creatinine or eGFR. Among those studies reporting significant differences, recipients of better-functioning kidneys generally achieved superior outcomes [38]. A more recent study reported no difference in adjusted hazard ratios for graft failure amongst recipients of live-donor kidneys with eGFR >110 vs < 80 mL/min; of note, more sensitive outcomes such as differences in graft function were not reported [39].
Older Age.
The 2008 review by Young et al. included twenty-two articles assessing outcomes among 987 “older” kidney donors. Age cutoffs for categorizing donors as young or old varied between studies, and median follow-up was 1.8 years. Collectively, the studies yielded no significant differences between donor age groups in surgical outcomes such as operative time, blood loss, length of hospital stay, infections, or hemorrhage. Studies evaluating changes in kidney function following donation were too heterogeneous to produce a unifying conclusion [36].
Segev et al.’s 2010 study of 80,000 living donors found no differences in short-term mortality across donor age groups, although there was a trend towards higher 12-month mortality in donors aged 60 and above compared with young donors (p = 0.08) [25••]. A subsequent publication reported superior survival among donors aged 70 or above compared with healthy controls from the NHANES III cohort [40]. Such a finding may reflect incomplete matching and selection bias relating to unusually healthy, elderly donors.
Garg et al. reported an age-associated increased risk of death and major cardiovascular events for older versus younger donors; when comparing donors versus non-donors, however, event-free survival was superior amongst donors [18]. Similarly, a 2012 publication from Norway demonstrated a monotonic increase in crude death rates across increasing donor age categories [17], mirroring trends seen among non-donor NHANES participants without exclusion criteria for kidney donation [41]. When donors were compared with non-donors in the Norwegian study, however, overall and cardiovascular mortality among donors was lower than matched controls.
Although this data suggests that donors appear to compare favorably to similar non-donors with regard to the specified outcomes, older age may still confer a risk of incident morbidity upon donors. Various studies have reported associations between older donor age and perioperative complications [27], incident hypertension [16], and reduced post-donation renal function [16, 21, 42]. Of note, older donors appear to demonstrate similar adaptive hyperfiltration and hypertrophy to that of younger donors after donation, suggesting that inferior renal function in older living donors is attributable to glomerulopenia [43].
Collectively, these studies highlight problems with age as a predictor of donor outcomes. Age is a continuous variable, and attempts to establish a single age cutoff for donor exclusion imply a dichotomous nature. Furthermore, chronological age is subject to extensive health-related confounders that collectively define one’s “physiological age.” Finally, as a rule, one’s chances of dying or developing incident illness always increase with advancing age. While a single age cutoff may simplify the donor screening process, the process should also consider medical traits associated with age that might more directly cause poorer donor outcomes.
The impact of donor age on transplant recipients has also been studied extensively. In Iordanous et al.’s meta-analysis, pooled data revealed a significantly worse 1- and 5-year composite outcome of graft and patient survival for recipients of kidneys from older live donors. However, death-censored graft survival and recipient survival were not statistically significantly different between donor age groups [38]. While this analysis and others report inferior graft function among recipients of older kidneys [38, 42, 44–46], older donors often have significantly lower baseline GFRs as compared with their younger counterparts prior to donation [42, 44, 45]. This trend calls into question whether it is truly age or reduced renal function that is the donor characteristic most directly responsible for differences in graft function.
Studies on various other recipient outcomes have produced discrepant findings. Various authors have reported inferior graft survival [36, 47–49], death-censored graft survival [44], acute rejection [37, 45–47] and recipient survival [48] among recipients of kidneys from older living donors. To the contrary, Balachandran et al. reported no difference in recipient survival, death-censored graft survival, or rates of vascular complications or acute rejection between young and old donor groups [42]. Similarly, a study of the ANZDATA registry reported no association between donor-recipient age difference and death-censored graft failure, recipient survival, or acute rejection [50]. Additional studies suggest the association between older donor age and recipient outcome fluctuates with time since transplant [51] or differs based on recipient age [40].
To put into context the potentially worse outcomes among recipients of older live-donor kidneys, multiple authors have compared such recipients to those receiving deceased-donor kidneys. Berger et al. reported that older living donors permitted similar recipient and graft survival as that seen in younger, non-ECD deceased donors [40]. An earlier analysis demonstrated superior graft function and less DGF among recipients of older live-donor kidneys, compared with ECD graft recipients [45]. This and other analyses have also demonstrated that grafts from older live donors fare equally well or better than those from comparable SCD donors [45, 52, 53]. Such findings suggest that older age alone should not preclude donation [54], and have important implications for ESRD patients whose options are limited to remaining on dialysis or accepting a kidney from an older living donor.
Younger Age.
Questions also arise about the youngest age at which individuals can donate a kidney. Most programs exclude prospective donors below eighteen years of age, the legal age of consent in the US. Donation between the age of 18 and 21 is often considered a relative contraindication [55•], although international guidelines differ with regard to absolute prohibition of kidney donation by minors in particular situations [56]. Besides issues of consent, younger potential donors presumably also have longer cumulative lifetime risk of developing conditions that predispose them to renal disease (e.g., diabetes, hypertension, obesity), and a normal initial donor evaluation may not accurately predict one’s lifetime risk of ESRD [57].
Hypertension.
The Amsterdam Forum considered individuals with BP > 140/90 mmHg to be suboptimal donors, although flexibility was recommended for donors with easily controlled hypertension and acceptable renal function [7]. According to 2008 UNOS data, 1.8 % of living donors had BP of ≥ 140/90; hypertension rates differed between ethnic groups, BMI categories, and donor relationships [6•]. Young et al.’s 2008 review featured six studies examining 125 hypertensive donors, although substantial variability existed between studies’ definitions of hypertension, inclusion of patients on anti-hypertensive medications, and duration of follow-up. The studies with greater follow-up disagreed as to whether donors with high or low BP have greater decline in GFR following donation [36].
Segev et al.’s study suggested that hypertension may increase the risk for perioperative death. Ninety-day mortality was significantly higher for donors with a history of hypertension (36.7 vs. 1.3 per 10,000 donors, RR 27.4, p < 0.001). In multivariate analysis, donors with SBP ≥ 140 had significantly higher rates of death than those with measurements < 120 mmHg [25••]. More recently, donor hypertension was found to be an independent predictor of longer hospital length of stay and surgical complications [29].
The association between donor hypertension and recipient outcomes has not been extensively studied. One study compared 24 recipients of kidneys from hypertensive donors with 124 controls; in this cohort, recipient GFR at 1 year post-transplant was not significantly different between groups [38]. In Issa et al.’s 2007 analysis, donor systolic BP > 120 mmHg was significantly associated with lower recipient eGFR at 2 years post-transplant, after adjusting for various other donor demographic and clinical characteristics [58].
Elevated BMI.
Obese individuals may have higher GFR due to altered transcapillary hemodynamics [59], and excess weight is a known risk factor for ESRD [60]. The Amsterdam report recommended discouraging individuals with BMI > 35 kg/m2 from donating, especially when other comorbidities are present [7]. Nevertheless, today’s donors are increasingly heavy; OPTN data revealed a 19.5 % rate of obesity (defined as BMI > 30 kg/m2) among living donors in 2008, an increase from 14.4 % in 2000. Rates of obesity among 2008 donors varied significantly between ethnic groups; only 10.7 % of Asian donors were obese, compared with 34.2 % of American Indian/Alaskan Native donors [6•].
Young et al.’s meta-analysis examined ten studies comparing the outcomes of obese donors. BMI cutoffs for comparison varied between studies, from 30 to 39 kg/m2. The pooled data yielded statistically significant (but of questionable clinical significance) differences favoring less-heavy donors, with regard to operative time, blood loss, and hospital stay. Rates of surgical complications such as infections or hemorrhage did not differ between BMI groups. Only two of ten studies had follow-up greater than 4 years; these two studies reached conflicting conclusions about the impact of donor BMI on trends in serum creatinine or eGFR over time. Similarly, no conclusions were reached regarding changes in blood pressure or urinary protein [36].
More recent studies have reported worse outcomes for obese living donors. A multicenter study of over three thousand donors reported a significant association between obesity and perioperative complications in a logistic regression model (adjusted odds ratio 1.92, p = 0.037) [27]. Schold et al.’s recent analysis of NIS and SRTR data reported that obesity was associated with significantly longer post-donation length of stay [29]. Postoperative wound infections were more common among donors with BMI > 25 kg/m2 (adjusted odds ratio 4.03, p = 0.001) [26]. In a multivariate analysis of 255 donors from the Ibrahim study, per-unit BMI was independently associated with GFR < 60 mL/min/1.73 m2 and with hypertension requiring medications [16].
Conversely, other recent studies suggest no increased risk of long-term morbidity or mortality in kidney donors with elevated BMI. Segev et al. reported similar survival up to 12 months across BMI categories[25••]. A study of donors over a 35 year period revealed no difference in long-term renal function between those with BMI greater or less than 30 [61]. Similarly, a 2009 study of OPTN data on 3,302 living donors with BMI > 25 revealed no difference in eGFR decline or percent change in serum creatinine levels at 6 months post-donation. Baseline and 6-month blood pressures were higher in the obese group, but did not rise by a significantly greater margin than those of non-obese donors [62].
This last study also examined outcomes for recipients of kidneys from heavier donors. As compared with donors with BMI < 25, recipients from very obese donors (BMI ≥ 35) had significantly higher rates of DGF (OR 2.16, 95 % confidence interval 1.20–3.89). Recipient mortality and allograft failure were similar across categories of donor BMI [62].
The association between donor BMI and recipient outcomes was further examined in a 2011 analysis that categorized donor-recipient pairs by degree of “BMI mismatch,” or the difference in BMI categories. The data confirmed that two-thirds of living donors fall into overweight or obese categories by BMI; the proportion of overweight/obese donors was highest for African American and Hispanic donors. With a mean follow up of 1.8 years, multivariate analysis demonstrated a significantly higher risk of death-censored graft loss for BMI mismatch +3 (donors three categories higher than recipients; HR = 2.31, 95 % confidence intervals 1.05, 5.08). Other categories of BMI mismatch did not confer an elevated risk, and neither donor nor recipient BMI alone was associated with graft loss in the multivariate model [63].
Graft Size.
Graft size has also been examined as a potentially important surrogate for the “dose” of healthy kidney provided by living donation. In line with previous concepts of ‘nephron number’ [64], some studies suggest that allograft size (as estimated by cross-sectional imaging) predicts long-term outcomes for both living donors [65] and their recipients [66]. A 2011 analysis refined this relationship by adjusting graft volume for donor and recipient body surface area (BSA); the authors reported an association between lower adjusted graft volume and elevated risk of rejection, chronic changes on biopsy, graft glomerulonephritis and graft loss in multivariate analysis. Long-term eGFR and graft survival were also inferior in the lower adjusted graft volume group [67].
A more recent study categorized 123 consecutive live-donor transplants with grafts functioning beyond 1 year by the ratio of donor kidney weight to recipient body weight (Kw/Rw). Although creatinine levels were significantly lower during the first post-transplant year in the highest Kw/Rw group, no significant difference was seen in longer-term follow-up. Rates of acute rejection did not differ between groups. Graft survival was highest in the group with the highest Kw/Rw ratio in multivariate logistic regression, but there was no difference in recipient survival [68].
Proteinuria.
The Amsterdam group recommended excluding individuals from kidney donation if they have a 24-h urine protein excretion > 300 mg. No consensus was reached on screening donors for microalbuminuria, out of concern for less consistency between labs and higher costs than other traditional measures of urinary protein excretion, such as dipsticks [7]. Young et al.’s meta-analysis cited a single 1999 study of eight donors with proteinuria, who maintained normal BP and had similar measured GFRs as controls, after 1 year [36].
Glucose Intolerance.
Current guidelines dictate that individuals should be excluded from donating a kidney if they have a personal history of diabetes, fasting glucose ≥ 126 mg/dL on two separate occasions, or a 2-h oral glucose tolerance test (OGTT) serum glucose level > 200 mg/dL [7]. While the majority of US transplant centers exclude potential donors with 2-h OGTT glucose > 140 mg/dL [9], a 2010 Japanese study compared 373 control donors with 71 other donors with impaired glucose tolerance by OGTT; these individuals all had A1c levels < 6.5 % and no known diabetic complications. There were no significant differences between groups with regard to perioperative complications or mortality at 5-, 10-, or 20-year follow-up. Among those with higher OGTT results, none had developed severe diabetic complications or ESRD at a mean follow-up of 88 months [69].
Hematuria.
While isolated microscopic hematuria is not an absolute contraindication to donation, the Amsterdam Forum recommends that potential donors with persistent hematuria should undergo a complete urologic workup, including urine cytology or cystoscopy, prior to donation [7]. Few studies exist on the outcomes of donors with hematuria. Young et al.’s meta-analysis included only two small samples of donors with microscopic hematuria in the setting of familial Alport’s syndrome and biopsy-proven IgA nephropathy. Results were inconsistent with respect to blood pressure, GFR, or urinary protein excretion [36].
Stone Disease.
The Amsterdam Forum report recommended screening potential donors with stone disease for metabolic abnormalities predisposing them to stone formation, such as hypercalciuria, hyperuricemia, hyperoxaluria, or cystinuria. If such conditions are excluded and an individual does not have urinary tract infections, multiple stones, or nephrocalcinosis on imaging, he or she may still donate. If stones are present in the setting of underlying systemic diseases that predispose to further stone formation (e.g., inflammatory bowel disease or sarcoidosis), such individuals should be excluded from donating, given the potential obstruction of a solitary remaining kidney by additional stones [7].
Young et al. included four studies of 32 donors with kidney stones at donation in their meta-analysis, among whom a single case of ureteral obstruction from recurrent nephrolithiasis was reported [36]. More recently, a single-center study from the United Kingdom examined the role of ex vivo ureteroscopy for 17 kidneys from donors with asymptomatic kidney stones. Of these, ten underwent successful stone removal with basket extraction or fragmentation, prior to transplantation. Eight donors were followed for over a year, among whom no new stones were identified on serial imaging. Similarly, ultrasounds performed on recipients showed no new stone formation [70].
Smoking.
The Amsterdam report advised smoking cessation at least 4 weeks prior to donation, consistent with recommendations for other elective surgical procedures [7]. Multiple large studies have subsequently demonstrated worse outcomes among living donors who smoke. In Segev’s analysis, multivariate analysis adjusting for age, gender, race, systolic BP, and history of hypertension revealed a significantly higher death rate among smokers [25••]. Donors who smoke also have more perioperative complications [27] and postoperative wound infections [26], and are less likely to provide follow-up information requested by transplant centers [71].
Donor smoking also appears to adversely affect recipient outcomes. A 2011 study reported that kidneys from live donors who smoke were associated with smaller long-term improvements in recipient creatinine and calculated GFR than those from non-smoking donors; this relationship appeared to follow a dose-dependent pattern, as donors with the highest levels of tobacco exposure were associated with the smallest recipient creatinine improvements. This study also reported a trend towards higher rates of graft failure among recipients of kidneys from donors who smoke [72].
Dyslipidemia.
The Amsterdam Forum acknowledged that hyperlipidemia is an important cardiovascular risk factor and may hasten the progression of kidney disease, but is itself not a contraindication to kidney donation. A 2007 analysis of 264 living-donor kidney transplants at the Cleveland Clinic demonstrated an independent association between donor total cholesterol levels > 200 mg/dL and lower recipient eGFR at 2 years post-transplant. This association remained significant after adjusting for other donor variables such as gender, race, BMI, fasting glucose, uric acid, and donor-recipient relatedness [58].
Non-medical “Complexities” that Affect Outcomes
Race.
This topic is covered in detail elsewhere in this issue. The existing data on outcomes of non-Caucasian living donors was recently summarized in a thorough review [73•], showing that African American and Hispanic living donors have higher rates of renal disease [74–76], hypertension [74, 77, 78], and diabetes [74] than Caucasian donors. In addition, African Americans appear to have inferior perioperative [71] and longitudinal [25••] survival. Given the higher prevalence of ESRD among African-Americans, these findings may partially explain the lower likelihood of an African-American recipient receiving a live-donor kidney [2]. However, the relative risk of ESRD among African-American versus Caucasian donors is similar to the relative risk of ESRD among the general population who are African-American versus Caucasian [76]. Therefore, African American race is not an absolute contraindication to donation.
Gender.
Certain donor outcomes have been associated with donor gender. Male donors were shown to have a significantly higher rate of 90-day postoperative mortality than female donors (5.1 versus 1.7 per 10,000 donors, p = 0.007), although this risk was no longer significant after adjusting for multiple covariates [25••]. Other authors have also demonstrated higher rates of renal disease among male former donors, including albuminuria [16] and ESRD [76]. Conversely, women may be more likely to have a low GFR [16], and are more than twice as likely as men to develop depression after donation (15.5 % vs. 7 %, p < 0.0001) [22].
Donor gender may also have implications for recipient outcomes. In a recent study of 1,967 consecutive live-donor transplants spanning three decades at a single Egyptian transplant center, male donors had greater 5-year and 10-year overall graft survival [49]. To the contrary, a trend towards inferior 5-year death-censored graft survival among kidneys from male living donors was demonstrated in a Norwegian study of living-donor transplants between 1994 and 2004; this difference achieved statistical significance only among those recipients who did not suffer an acute rejection episode, suggesting that rejection outweighs donor gender in its impact on death-censored graft survival [47].
Health Insurance/Socioeconomic Status (SES).
Lower SES appears to impact one’s likelihood of donating a kidney, as a recent study demonstrated a lower incidence of live-kidney donation in the lowest quintiles of income [79]. Among those individuals who do donate, 12.2 % lack health insurance. Perhaps not unexpectedly, rates of follow-up and data submission are lower in donors without health insurance or US citizenship [71]. Furthermore, a recent analysis of US data demonstrated that non-private insurance was an independent risk factor for perioperative complications related to donor nephrectomy [29].
Conclusion.
Donating a kidney is a serious decision, and an altruistic act with a potentially huge impact on the life and health of both donor and recipient. It is therefore vital that both parties receive thoughtful counseling based on the most accurate and current data regarding outcomes for both. While much research has focused on donor age, other characteristics such as donor renal function, blood pressure, obesity, graft size, and recipient age are important factors in the donor evaluation. Consideration of recipient outcomes from medically complex living donors versus deceased donors provides important context to how ESRD patients and their potential donors weigh their options.
More long-term and complete collection of donor-related data will address current knowledge gaps and help improve risk assessment for both donor and recipients [80]. Today, however, the lack of strong outcome data on donors with medical complexities, especially when multiple risk factors may be found in an individual, limits the clinician’s ability to determine a convincing risk assessment. We may assume that the more medically complex a donor is, the more likely that donor or the corresponding recipient would be to have inferior outcomes, but the magnitude of differences is poorly defined. Similarly, it can be assumed that graft function will be worse in transplants featuring smaller or older kidneys, or kidneys with reduced baseline GFR, although the relative contributions of such factors remains ill-defined. Although efforts are underway to further translate existing data into evidence-based guidelines [12], clinical judgment and experience will continue to play important roles in donor evaluations.
Abbreviations
- ANZDATA:
-
Australia and New Zealand Dialysis and Transplant
- ATN:
-
acute tubular necrosis
- BMI:
-
body mass index
- BP:
-
blood pressure
- BSA:
-
body surface area
- CKD:
-
chronic kidney disease
- DGF:
-
delayed graft function
- ECD:
-
expanded criteria donor
- eGFR:
-
estimated glomerular filtration rate
- ESRD:
-
end stage renal disease
- GFR:
-
glomerular filtration rate
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- K/DQOI:
-
Kidney Disease Outcomes Quality Initiative
- NHANES:
-
National Health and Nutrition Examination Survey
- NIS:
-
Nationwide inpatient sample
- OGTT:
-
oral glucose tolerance test
- OPTN:
-
Organ Procurement and Transplantation Network
- SCD:
-
standard criteria donor
- SES:
-
socioeconomic status
- SRTR:
-
scientific registry of transplant recipients
- UNOS:
-
United Network for Organ Sharing
References
Papers of particular interest, published recently, have been highlighted as • Of importance •• Of major importance
U.S. Renal Data System, USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2013.
U.S. Department of Health and Human Services, “Organ Procurement and Transplantation Network Data Report.” Accessed December 5, 2013.
Petrini C. A few ethical criteria for evaluating the risks for ‘marginal’ living kidney donors. Transplant Proc. 2013;45(3):1267–9.
Reese PP, Caplan AL, Kesselheim AS, Bloom RD. Creating a medical, ethical, and legal framework for complex living kidney donors. Clin J Am Soc Nephrol. 2006;1(6):1148–53.
Taler SJ, Messersmith EE, Leichtman AB, Gillespie BW, Kew CE, Stegall MD, et al. Demographic, metabolic, and blood pressure characteristics of living kidney donors spanning five decades. Am J Transplant. 2013;13(2):390–8. RELIVE study, establishes increasing age/BMI in large cohort of multicenter data with geographically and demographically diverse populations.
Davis CL, Cooper M. The state of U.S. living kidney donors. Clin J Am Soc Nephrol. 2010;5(10):1873–80. Review of UNOS data on current and former practices.
Delmonico F. A Report of the Amsterdam Forum On the Care of the Live Kidney Donor. Transplantation. 2005;79(Supplement 2):S53–66.
U.S. Department of Health and Human Services., “Organ Procurement and Transplantation Network (OPTN) Policies. Policy 12.0,”2013.
Mandelbrot DA, Pavlakis M, Danovitch GM, Johnson SR, Karp SJ, Khwaja K, et al. The medical evaluation of living kidney donors: a survey of US transplant centers. Am J Transplant. 2007;7(10):2333–43.
Reese PP, Feldman HI, McBride MA, Anderson K, Asch DA, Bloom RD. Substantial variation in the acceptance of medically complex live kidney donors across US renal transplant centers. Am J Transplant. 2008;8(10):2062–70.
Arunachalam C, Garrues M, Biggins F, Woywodt A, Ahmed A. Assessment of living kidney donors and adherence to national live donor guidelines in the UK. Nephrol Dial Transplant. 2013;28(7):1952–60.
K. D. I. G. O. (K/DIGO), Press release, May 15, 2013.
Goldfarb DA, Matin SF, Braun WE, Schreiber MJ, Mastroianni B, Papajcik D, et al. Renal outcome 25 years after donor nephrectomy. J Urol. 2001;166(6):2043–7.
Mueller TF, Luyckx VA. The natural history of residual renal function in transplant donors. J Am Soc Nephrol. 2012;23(9):1462–6.
Fehrman-Ekholm I, Elinder CG, Stenbeck M, Tydén G, Groth CG. Kidney donors live longer. Transplantation. 1997;64:976–8.
Ibrahim HN. Long-term consequences of kidney donation. N Engl J Med. 2009;360(22):459–69.
Mjøen G, Reisaeter A, Hallan S, Line P-D, Hartmann A, Midtvedt K, et al. Overall and cardiovascular mortality in Norwegian kidney donors compared to the background population. Nephrol Dial Transplant. 2012;27(1):443–7.
Garg AX YA, Meirambayeva A, Huang A, Kim J, Prasad GV, Knoll G, et al. Cardiovascular disease in kidney donors: matched. BMJ. 2012;e1203:1–10.
Tsai S-F, Shu K-H, Ho H-C, Wu M-J, Cheng C-H, Lian J-D, et al. Long-term outcomes of living kidney donors over the past 28 years in a single center in Taiwan. Transplant Proc. 2012;44(1):39–42.
Okamoto M, Akioka K, Nobori S, Ushigome H, Kozaki K, Kaihara S, et al. Short- and long-term donor outcomes after kidney donation: analysis of 601 cases over a 35-year period at Japanese single center. Transplantation. 2009;87(3):419–23.
Fehrman-Ekholm I, Kvarnström N, Söfteland JM, Lennerling A, Rizell M, Odén A, et al. Post-nephrectomy development of renal function in living kidney donors: a cross-sectional retrospective study. Nephrol Dial Transplant. 2011;26(7):2377–81.
Lentine KL, Schnitzler MA, Xiao H, Axelrod D, Davis CL, McCabe M, et al. Depression diagnoses after living kidney donation: linking U.S. Registry data and administrative claims. Transplantation. 2012;94(1):77–83.
Lentine KL, Vijayan A, Xiao H, Schnitzler MA, Davis CL, Garg AX, et al. Cancer diagnoses after living kidney donation: linking U.S. Registry data and administrative claims. Transplantation. 2012;94(2):139–44.
Yuan H, Liu L, Zheng S, Yang L, Pu C, Wei Q, et al. The safety and efficacy of laparoscopic donor nephrectomy for renal transplantation: an updated meta-analysis. Transplant Proc. 2013;45(1):65–76.
Segev DL, Muzaale AD, Caffo BS, Mehta SH, Singer AL, Taranto SE, et al. Perioperative mortality and long-term survival following live kidney donation. JAMA. 2010;303(10):959–66. Assessed perioperative and long-term risk of death among large cohort (80K) of living donors and compared to selected controls from NHANES.
Mjøen G, Øyen O, Holdaas H, Midtvedt K, Line P-D. Morbidity and mortality in 1022 consecutive living donor nephrectomies: benefits of a living donor registry. Transplantation. 2009;88(11):1273–9.
Patel S, Cassuto J, Orloff M, Tsoulfas G, Zand M, Kashyap R, et al. Minimizing morbidity of organ donation: analysis of factors for perioperative complications after living-donor nephrectomy in the United States. Transplantation. 2008;85(4):561–5.
Permpongkosol S, Link RE, Su L-M, Romero FR, Bagga HS, Pavlovich CP, et al. Complications of 2,775 urological laparoscopic procedures: 1993 to 2005. J Urol. 2007;177(2):580–5.
Schold JD, Goldfarb DA, Buccini LD, Rodrigue JR, Mandelbrot DA, Heaphy ELG, et al. Comorbidity burden and perioperative complications for living kidney donors in the United States. Clin J Am Soc Nephrol. 2013;8(10):1773–82.
Kasiske BL, Anderson-Haag T, Ibrahim HN, Pesavento TE, Weir MR, Nogueira JM, et al. A Prospective Controlled Study of Kidney Donors: Baseline and 6-Month Follow-up. Am J Kidney Dis. 2013;62(3):577–86. Preliminary data from the first prospective study of living donors, with donor candidates who did not donate enrolled as controls.
Garg AX. Living Kidney Donation: Biochemical Changes and Patient Outcomes. Am J Kidney Dis. 2013;62(3):448–9.
Srinivas TR, Poggio ED. Do living kidney donors have CKD? Adv Chronic Kidney Dis. 2012;19(4):229–36.
Poggio ED, Braun WE, Davis C. The science of Stewardship: due diligence for kidney donors and kidney function in living kidney donation–evaluation, determinants, and implications for outcomes. Clin J Am Soc Nephrol. 2009;4(10):1677–84.
Matas AJ, Ibrahim HN. The Unjustified Classification of Kidney Donors as Patients with CKD: Critique and Recommendations. Clin J Am Soc Nephrol. 2013;8(8):1406–13. Critique of classification of kidney donors as having CKD.
Rowe JW, Andres R, Tobin JD, Norris AH, Shock NW. The Effect of Age on Creatinine Clearance in Men: A Cross-Sectional and Longitudinal Study. J Gerontol. 1976;31(2):155–63.
Young A, Storsley L, Garg AX, Karpinski M, Investigators N, Boudville N, et al. Health Outcomes for Living Kidney Donors with Isolated Medical Abnormalities: A Systematic Review. Am J Transplant. 2008;8:1878–90.
Tsai S-F, Shu K-H, Wu M-J, Ho H-C, Wen M-C, Su C-K, et al. A higher glomerular filtration rate predicts low risk of developing chronic kidney disease in living kidney donors. World J Surg. 2013;37(4):923–9.
Iordanous Y, Seymour N, Young A, Johnson J, Iansavichus AV, Cuerden MS, et al. Recipient outcomes for expanded criteria living kidney donors: the disconnect between current evidence and practice. Am J Transplant. 2009;9(7):1558–73.
Young A, Kim SJ, Garg AX, Huang A, Knoll G, Prasad GVR, et al. Living kidney donor estimated glomerular filtration rate and recipient graft survival. Nephrol Dial Transplant. 2013;73:3–10.
Berger JC, Muzaale AD, James N, Hoque M, Wang JMG, Montgomery RA, et al. Living kidney donors ages 70 and older: recipient and donor outcomes. Clin J Am Soc Nephrol. 2011;6(12):2887–93.
Lin J, Kramer H, Chandraker AK. Mortality among living kidney donors and comparison populations. N Engl J Med. 2010;363(8):797–8.
Balachandran VP, Aull MJ, Charlton M, Afaneh C, Serur D, Leeser DB, et al. Kidneys from older living donors provide excellent intermediate-term outcomes after transplantation. Transplantation. 2012;94(5):499–505.
Tan JC, Busque S, Workeneh B, Ho B, Derby G, Blouch KL, et al. Effects of aging on glomerular function and number in living kidney donors. Kidney Int. 2010;78(7):686–92.
Noppakun K, Cosio FG, Dean PG, Taler SJ, Wauters R, Grande JP. Living donor age and kidney transplant outcomes. Am J Transplant. 2011;11(6):1279–86.
Gill J, Bunnapradist S, Danovitch GM, Gjertson D, Gill JS, Cecka M. Outcomes of kidney transplantation from older living donors to older recipients. Am J Kidney Dis. 2008;52(3):541–52.
Chen GD, Gu JL, Zhang XD, Qiu J, Wang CX, Chen LZ. Donor factors predictive for poor outcomes of living donor kidney transplantation. Transplant Proc. 2013;45(4):1445–8.
Øien CM, Reisaeter AV, Leivestad T, Dekker FW, Line PD, Os I. Living donor kidney transplantation: the effects of donor age and gender on short- and long-term outcomes. Transplantation. 2007;83(5):600–6.
Rizzari MD, Suszynski TM, Gillingham KJ, Matas AJ. Consideration of donor age and human leukocyte antigen matching in the setting of multiple potential living kidney donors. Transplantation. 2011;92(1):70–5.
Ghoneim MA, Bakr MA, Refaie AF, Akl AI, Shokeir AA, Shehab El-Dein AB, et al. Factors Affecting Graft Survival among Patients Receiving Kidneys from Live Donors: A Single-Center Experience. Biomed Res Int. 2013;2013:912413.
Ferrari P, Lim W, Dent H, McDonald SP. Effect of donor-recipient age difference on graft function and survival in live-donor kidney transplantation. Nephrol Dial Transplant. 2011;26(2):702–8.
Fuggle SV, Allen JE, Johnson RJ, Collett D, Mason PD, Dudley C, et al. Factors affecting graft and patient survival after live donor kidney transplantation in the UK. Transplantation. 2010;89(6):694–701.
Chang P, Gill J, Dong J, Rose C, Yan H, Landsberg D, et al. Living donor age and kidney allograft half-life: implications for living donor paired exchange programs. Clin J Am Soc Nephrol. 2012;7(5):835–41.
Young A, Kim SJ, Speechley MR, Huang A, Knoll GA, Prasad GVR, et al. Accepting kidneys from older living donors: impact on transplant recipient outcomes. Am J Transplant. 2011;11(4):743–50.
M. Hourmant, L. Lerat, and G. Karam, “Donation from old living donors: how safe is it?,” Nephrol. Dial. Transplant, 2013.
Kher A, Mandelbrot DA. The living kidney donor evaluation: focus on renal issues. Clin J Am Soc Nephrol. 2012;7(2):366–71. In-depth review of the evaluation of potential kidney donors, with a focus on medical and renal issues.
Thys K, Van Assche K, Nobile H, Siebelink M, Aujoulat I, Schotsmans P, et al. Could minors be living kidney donors? A systematic review of guidelines, position papers and reports. Transpl Int. 2013;26(10):949–60.
Steiner RW. ‘Normal for now’ or ‘at future risk’: a double standard for selecting young and older living kidney donors. Am J Transplant. 2010;10(4):737–41.
Issa N, Stephany B, Fatica R, Nurko S, Krishnamurthi V, Goldfarb DA, et al. Donor factors influencing graft outcomes in live donor kidney transplantation. Transplantation. 2007;83(5):593–9.
Chagnac GUA, Weinstein T, Korzets A, Ramadan E, Hirsch J. Glomerular hemodynamics in severe obesity Glomerular hemodynamics in severe obesity. Am J Physiol Ren Physiol. 2000;278:F817–22.
Hsu C, Mcculloch CE, Iribarren C, Darbinian J, Go AS. Body Mass Index and Risk for End-Stage Renal Disease. Ann Intern Med. 2006;144(1):21–8.
Tavakol MM, Vincenti FG, Assadi H, Frederick MJ, Tomlanovich SJ, Roberts JP, et al. Long-term renal function and cardiovascular disease risk in obese kidney donors. Clin J Am Soc Nephrol. 2009;4(7):1230–8.
Reese PP, Feldman HI, Asch DA, Thomasson A, Shults J, Bloom RD. Short-term outcomes for obese live kidney donors and their recipients. Transplantation. 2009;88(5):662–71.
Lin J, McGovern ME, Brunelli SM, Gaccione P, Malek S, Tullius SG, et al. Longitudinal trends and influence of BMI mismatch in living kidney donors and their recipients. Int Urol Nephrol. 2011;43(3):891–7.
Luyckx VA, Brenner BM. The clinical importance of nephron mass. J Am Soc Nephrol. 2010;21(6):898–910.
Sikora MB, Shaaban A, Beddhu S, Bourija H, Wei G, Baird B, et al. Effect of donor kidney volume on recipient outcome: does the ‘dose’ matter? Transplantation. 2012;94(11):1124–30.
Yano NVM, Lin MF, Hoffman KA, Vijayan A, Pilgram TK. Renal Measurements on CT Angiograms: Correlation with Graft Function at Living Donor Renal. Radiology. 2012;265(1):151–7.
Han SS, Yang SH, Oh YJ, Cho JY, Moon KC, Ha J, et al. Graft volume as the surrogate marker for nephron number affects the outcomes of living-donor kidney transplantation. Clin Transplant. 2011;25(3):E327–35.
Hwang JK, Kim YK, Kim SD, Park SC, Choi BS, Kim JI, et al. Does donor kidney to recipient body weight ratio influence long-term outcomes of living-donor kidney transplantation? Transplant Proc. 2012;44(1):276–80.
Okamoto M, Suzuki T, Fujiki M, Nobori S, Ushigome H, Sakamoto S, et al. The Consequences for Live Kidney Donors With Preexisting Glucose Intolerance Without Diabetic Complication: Analysis at a Single Japanese Center. Transplantation. 2010;89(11):1391–5.
Olsburgh J, Thomas K, Wong K, Bultitude M, Glass J, Rottenberg G, et al. Incidental renal stones in potential live kidney donors: prevalence, assessment and donation, including role of ex vivo ureteroscopy. BJU Int. 2012;111(5):784–92.
Ommen ES, LaPointe Rudow D, Medapalli RK, Schröppel B, Murphy B. When good intentions are not enough: obtaining follow-up data in living kidney donors. Am J Transplant. 2011;11(12):2575–81.
Heldt J, Torrey R, Han D, Baron P, Tenggardjaja C, McLarty J, et al. Donor Smoking Negatively Affects Donor and Recipient Renal Function following Living Donor Nephrectomy. Adv Urol. 2011;2011:929263.
Lentine KL, Segev DL. Health outcomes among non-Caucasian living kidney donors: knowns and unknowns. Transpl Int. 2013;26(9):853–64. Recent review of kidney donation outcomes for non-Caucasian donors.
Lentine KL, Schnitzler MA, Xiao H, Saab G, Salvalaggio PR, Axelrod D, et al. Racial variation in medical outcomes among living kidney donors. N Engl J Med. 2010;363(8):724–32.
Gibney EM, King AL, Maluf DG, Garg AX, Parikh CR. Living kidney donors requiring transplantation: focus on African Americans. Transplantation. 2007;84(5):647–9.
Cherikh WS, Young CJ, Kramer BF, Taranto SE, Randall HB, Fan P-Y. Ethnic and gender related differences in the risk of end-stage renal disease after living kidney donation. Am J Transplant. 2011;11(8):1650–5.
Lentine KL, Patel A. Risks and outcomes of living donation. Adv Chronic Kidney Dis. 2012;19(4):220–8.
Doshi GA, Goggins MO, Li L. Medical outcomes in African American live kidney donors: a matched cohort study. Am J Transplant. 2013;13(1):111–8.
J. Gill, J. Dong, C. Rose, O. Johnston, and D. Landsberg, “The Effect of Race and Income on Living Kidney Donation in the United States,” J. Am. Soc. Nephrol., pp. 1–8, 2013.
Leichtman A, Abecassis M, Barr M, Charlton M, Cohen D, Confer D, et al. Living kidney donor follow-up: state-of-the-art and future directions, conference summary and recommendations. Am J Transplant. 2011;11(12):2561–8.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Matthew Niemi and Didier A. Mandelbrot declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Niemi, M., Mandelbrot, D.A. The Outcomes of Living Kidney Donation from Medically Complex Donors: Implications for the Donor and the Recipient. Curr Transpl Rep 1, 1–9 (2014). https://doi.org/10.1007/s40472-013-0001-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-013-0001-6