Abstract
The rise in multidrug resistant (MDR) bacteria has become a global crisis. Rapid and accurate diagnosis of infection will facilitate antibiotic stewardship and preserve our ability to treat and cure patients from bacterial infection. Direct in situ imaging of bacteria offers the prospect of accurately diagnosing disease and monitoring patient outcomes and response to treatment in real-time. There have been many recent advances in the field of optical imaging of infection; namely in specific probe and fluorophore design. This combined with the advances in imaging device technology render direct optical imaging of infection a feasible approach for accurate diagnosis in the clinic. Despite this, there are currently no licensed molecular probes for clinical optical imaging of infection. Here we report some of the most promising and interesting probes and approaches under development for this purpose, which have been evaluated in in vivo models within the laboratory setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multidrug resistant (MDR) bacteria are now responsible for upwards of 23,000 deaths per year in the USA and 25,000 deaths per year within the EU; leading to total economic burdens of $35 bn and €1.5 bn, respectively [1, 2]. The inexorable rise of MDR bacteria has in large part been exacerbated by misdiagnosis and inappropriate use of antibiotics [3–6]. Accelerated development of diagnostic approaches is imperative in order to gain control and optimise infection treatment [7]. Improved antimicrobial stewardship will be essential to safeguard not only treatment of bacterial infections, but also to preserve many procedures common to modern medicine where an inability to prevent infection would deem them too risky to perform [8]. These include cancer chemotherapy, dialysis for end stage renal failure, organ and bone marrow transplantation and complex surgery, such as cardiac bypass [1]. On this basis, there is increasing pressure to find methods for the accurate and rapid diagnosis of infection; and in situ molecular imaging presents an ever-attractive tool to achieve this.
Molecular imaging
Molecular imaging is an approach which, broadly speaking, utilises a functional group to target disease biomarkers or pathways conjugated to an imaging contrast agent, such as a radionuclide or fluorophore. Due to the specificity of these tracers, this approach has the potential to provide a dynamic assessment of a disease site, enabling host–pathogen interactions to be elucidated and the microenvironment to be monitored (e.g. the presence of specific enzymes or pH of the surrounding tissue) rapidly and in real-time. An approach which is much more difficult to achieve using conventional molecular laboratory tests performed ex vivo.
Imaging and sensing infection within the context of the host has the potential to provide answers to fundamental questions, such as:
-
1.
Is the clinical presentation caused by bacteria or sterile inflammation?
-
2.
Are the bacteria Gram positive or Gram negative?
-
3.
Are the bacteria pathogenic; are they MDR?
-
4.
Is the innate host response sufficient to kill and remove the pathogens or should we treat with antimicrobials or other immunomodulatory approaches?
-
5.
Has treatment been effective; should treatment be continued or de-escalated?
To date, direct in situ real-time detection of infection has largely relied upon nuclear imaging of suspected infection with [18F]FDG (2-fluoro-2-deoxy-d-glucose) or radiolabelled leukocytes. Despite the high sensitivity of [18F]FDG, it has low specificity for bacterial infection and may result in misdiagnosis [9–15]. Conversely, leukocytes radiolabelled with Indium-111, Technicium-99m or [18F]FDG should provide enhanced specificity for bacterial infection compared to [18F]FDG [16–19], however, in practice specificity has shown to be varied [20, 21]. Other limitations of radiolabelled leukocyte imaging include the lengthy procedure required for retrieving and labelling leukocytes. Additionally, recovering enough leukocytes from immunocompromised patients for the procedure is not always possible, and not all bacterial infections elicit a robust neutrophil response, such as Mycobacterium tuberculosis.
Each of these existing ‘gold standard’ imaging techniques rely on imaging surrogates of the response to infection rather than targeting bacteria directly. Hence these methodologies are inherently lacking in ability to determine bacterial load or Gram status. Therefore, there is a concerted effort to develop bacteria specific radionuclide probes [22–33]. These probes are ultimately designed with a target product profile to have high sensitivity and specificity; meaning infection loci can be accurately identified by whole body imaging. These probes also strive to quantify bacterial load, elucidate the Gram status of the bacterial infection and be used to monitor treatment progression. However, there are several fundamental limitations associated with nuclear medicine, which are unlikely to be overcome with new generation bacterial tracers. Namely this is the cost associated with the labelling and synthesis of these probes; their short shelf-life due to decay of the radionuclide; the radiation dose to the patient and medical staff; and that the whole body scanning procedure is not suitable for some patients, e.g. for those in intensive care or in theatres; where near-patient imaging is optimal (some hand held devices are now available, however, the use of radioactivity in complex clinical environments is challenging and not always possible). Therefore, the development of optical molecular imaging tools based on fluorescence reporters is gaining in popularity, especially for superficial surfaces of the human body; such as skin or those accessible by endoscopy. Whilst these probes are designed to stand alone, it is highly likely that these probes would be used in combination with current whole body imaging; for example [18F]FDG could be used to determine potential infectious loci, which could then be further investigated and monitored with optical probes. This approach may be clinically important for patients with fever of unknown origin (FUO).
Optical molecular imaging
Optical molecular imaging relies on the detection of fluorescence at a target site. Despite its widespread use within the laboratory for generating insight into biological processes in small animal models, optical imaging for human diagnostics has not yet widely gained adoption within the clinical setting. This has been for a number of reasons; including poor signal to noise of fluorophores within the body, the lack of specificity and sensitivity of available probes, toxicity, and the inherent issue of light scattering and absorbance within tissues. The current challenges are discussed in further detail by Keereweer [34], thus to date, no optical probes have been licensed for use or extensively evaluated within the clinic for bacterial detection. Despite this, optical imaging has shown its feasibility in the field of oncology where its worth has been demonstrated using intraoperative imaging devices for image guided surgery [35].
Moreover, due to recent advances in both fluorophore design and synthesis, and in imaging technology [36], many of the limiting factors associated with optical imaging can now be addressed and minimised, and on-going efforts towards infection detection in vivo are producing a variety of interesting probe candidates.
There is an ever-increasing number of available fluorophores with desirable characteristics for in vivo and clinical imaging. These fluorophores are shifted towards the near infrared (NIR, 700–900 nm) region of the electromagnetic spectrum [37–39] and therefore have reduced tissue absorbance and scattering, so that they can be detected from greater depths and allow for more sensitive imaging [40–42]. Furthermore, indocyanine green (ICG) which fluoresces in the NIR region has US Food and Drug Administration (FDA) clinical approval and has been evaluated extensively in humans [43].
Whilst shifting excitation and emission spectra towards the NIR region is imperative for enabling sensitive imaging of below the skin surface [42], other considerations for fluorophore development must be considered in order to make them useful. For example: the aqueous solubility, photostability, lack of auto quenching, ease of conjugation to targeting moieties, effect on the targeting moiety, function, biodistribution, and clearance route to name but a few. As shown by examples later within this review, there are several NIR fluorophores which make interesting candidates for optical imaging of bacterial infections in vivo.
The emergence of environmentally sensitive fluorophores and exploitation of FRET (fluorescence resonance energy transfer) systems has also been conducive to the progression of optical imaging probe design. NBD (7-nitrobenz-2-oxa-1,3-diazol-4-y) is one such environmentally sensitive fluorophore [44]; within an aqueous environment, NBD fluoresces weakly, whereas strong fluorescent signal can be detected from hydrophobic regions, such as the cell membrane. It must be noted that due to the short emission wavelength of NBD (λ em max = 535 nm), NBD is not a fluorophore suited at all applications due to high tissue autofluorescence at this wavelength, however as discussed later, NBD has been exploited for some applications and can be detected above tissue background using fibred confocal fluorescence microscopy (FCFM) [45]. FRET systems exploit the phenomenon of fluorescence quenching. If a fluorophore is placed in close proximity to a quencher, the quencher is able to accept the energy emitted from the excited fluorophore, preventing fluorescence signal emission from the probe. In the context of optical imaging probes, the fluorophore and quencher are often located either side of a specific peptide sequence. Cleavage of the peptide sequence by a target enzyme releases the quencher from the molecule, thus enabling fluorescent signal to be detected. This approach has been exploited to target several bacteria specific enzymes, such as β-lactamase [46] and micrococcal nuclease [47], as discussed later.
Additionally, the advancement in hand held-devices and optical endomicroscopy (OEM) platforms such as fibred confocal fluorescent microscopes (FCFM) mean that imaging of shallow infections and those in internally accessible areas such as lungs, stomach, gut etc. can be performed at the bedside without the need to move patients to cumbersome equipment, as is required for nuclear imaging and magnetic resonance imaging (MRI).
Due to the lack of reported clinical data for the evaluation of optical bacteria-specific molecular imaging probes, this review will report and comment on some of the most promising optical imaging agents under development, which have thus far been evaluated in vivo in small animal models.
Current probes undergoing in vivo assessment in small animal models
Probes for optical imaging are dependent on two key factors; the targeting region and the fluorophore (and quencher if applicable). Both of which are crucial for specific, sensitive imaging tools. Whilst this review is primarily focused on optical imaging of bacterial infections in vivo, probe development for the field of molecular imaging has largely been geared towards nuclear imaging. For this reason, where appropriate, examples from nuclear medicine are reported in the context of optical probe design. Table 1 lists optical probes currently under development as discussed within this review, including their key features and models of pre-clinical evaluation.
As is evidenced from Table 1 and the forthcoming discussion of reported molecular probe data, it is challenging to directly compare probe performance. This is due to the variation in study design; including the pathogen chosen, inoculation dose and infection site; the host immune status; the choice of controls; the injected probe route, concentration and determination of when peak signal to noise is likely to be achieved. It must be noted that the variance in study design is not limited to pre-clinical optical imaging, but is also common place in the field of pre-clinical nuclear imaging. Whilst extrapolating information from individual studies in order to compare probes across the field is difficult, the optical probes discussed in the remainder of this review each demonstrate potential for translation to the clinical setting.
Antimicrobial peptides
Antimicrobial peptides (AMPs) form part of the innate immune response. They are small amphipathic molecules and are able to readily insert into negatively charged bacterial membranes, thus offering a potential means for bacteria specific detection.
Ubiquicidin (UBI) is an AMP which shows much promise for diagnosing infection within the field of nuclear medicine. A number of studies pre-clinically [23–25, 28] and clinically [27] have demonstrated that a Technetium-99m radiolabelled UBI fragment, [99mTc]-UBI29–41 was able to specifically target a number of infection types, proving accurate diagnosis for at least 95 % of human patients for diseases including diabetic foot [48], fever of unknown origin [49], osteomyelitis [50] and hip prosthesis [51]. [99mTc]-UBI29–41 imaging has also shown promise in monitoring responses to treatment in vivo [23, 26] and clinically [52].
The same UBI29–41 fragment was subsequently labelled with NIR dye ICG02 and evaluated in vivo against Gram positive and Gram negative infections. This ligand was shown in vivo to have deep tissue penetration, and fast clearance. Moreover, the probe was able to accumulate at sites of bacterial infection and not at sites of sterile inflammation. Free dye did not accumulate at the infection site, and the probe could be blocked by pre-injections of unlabelled UBI29–41 [53].
An alternative approach for utilising the UBI29–41 fragment for bacterial imaging saw modification of the peptide structure in a number of ways, resulting in a cyclic form [45]. This led to improved peptide stability and resistance to proteolytic degradation, which had been observed for linear derivations of fluorescently labelled UBI29–41. In addition, the modified UBI scaffold was conjugated to the environmental fluorophore NBD (7-nitrobenz-2-oxa-1,3-diazol-4-y), enabling the probe to switch from ‘off’ to ‘on’ when inserted within a bacterial membrane. Despite NBD emitting in the ‘green’ region of the electromagnetic spectrum, using fibred confocal fluorescence microscopy (FCFM) the researchers were able to demonstrate that bacteria were labelled and visible above the level of tissue autofluorescence within ex vivo human lung tissue.
Further to labelling the linear UBI29–41 fragment with a radiolabel or a fluorophore, other approaches have been taken in order to multiplex fluorescently labelled UBI29–41 with either an antimicrobial for treatment of infection [54], or with a radiolabel for dual nuclear–optical imaging of infection [55].
To demonstrate the theranostic potential of fluorescently labelled UBI29–41 in vivo, UBI29–41 was conjugated to ZnO-quantum dots and NIR fluorophore MPA (a hydrophilic derivative of ICG) to yield ZnO@BSA-PEP-MPA for diagnosis of both Gram positive and Gram negative infections [54]. ZnO@BSA-PEP-MPA was further modified to incorporate the Gram positive antimicrobial vancomycin (Van). Whilst in vivo imaging of Van@ZnO@BSA-PEP-MPA does not appear to have been performed, the group showed in their murine model that the Van@ZnO@BSA-PEP-MPA probe was more effective at killing Staphylococcus aureus compared to free vancomycin alone; demonstrating that their approach was successful for combining non-invasive bacterial infection diagnosis and targeted treatment.
Development of a dual optical–nuclear probe for imaging infection circumvents the potential limitation of relying on optical imaging alone for identifying infectious foci by enabling non-invasive whole body imaging by PET or SPECT. This should identify infection sites independently of tissue depth and autofluorescence, which may be prohibitive for whole body optical imaging. After identification of suspected infection sites, the optical element of the probe can be imaged and monitored during intervention, such as surgical resection or treatment. The effectiveness of this approach has previously been demonstrated clinically for sentinel node biopsy [56, 57].
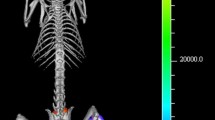
The potential of dual modality imaging of infection with UBI29–41 has been demonstrated in murine models of S. aureus (Gram positive) and Klebsiella pneumoniae (Gram negative) intramuscular infections, where UBI29–41 was dual-labelled with Cy5 and Indium-111 yielding [111ln]-DTPA-Cy5-UBI29–41 [55]. This probe accumulated at the sites of bacterial infection after intravenous (i.v) injection and could be detected by sequential SPECT and optical imaging.
Zn-DPA
Zn-DPA (zinc-(II)-dipicolyamine) is positively charged metal complex, and as such, it readily interacts with negatively charged membranes of both Gram positive and Gram negative bacterial cells, but not with the membranes of healthy mammalian cells [58, 59].
A number of differently labelled versions of Zn-DPA have been developed and evaluated in vivo with S. aureus infection models; including a Cy5-like-labelled ZnDPA probe [60] and a NIR-cyanine-labelled Zn-DPA [61, 62], the latter of which is now commercially available (Li-Cor Biosciences). Furthermore, Zn-DPA conjugated to squaraine-rotaxane moieties have also been developed in order to increase brightness and circumvent some of the known limitations of carbocyanine (Cy) dyes such as poor photostability [59, 63, 64].
Despite the successful in vivo labelling of bacterial infections in several studies [59–64], it must be noted that a fundamental flaw of Zn-DPA imaging is that Zn-DPA also labels negatively charged membranes of apoptotic and necrotic mammalian cells [65, 66]. This leads to false identification of bacterial infection by labelling sites of sterile inflammation, and thus renders it a non-specific imaging agent [60–62, 64].
Sugars
Bacteria and mammalian cells utilise different sugars, hence targeting bacteria specific sugar transport systems is a promising approach for probe design. To date, probes targeting maltohexaose, glucose-6-phosphate and sorbitol transport systems have been reported.
Maltohexaose is a sugar utilised by many bacteria [67], it is transported into bacteria via the maltodextrin transporter which is absent from mammalian cells [68, 69]. When labelled with the NIR dye IR786, the maltodextrin-based imaging probe (MDP) was shown to accumulate at sites of Escherichia coli infections in vivo and within S. aureus biofilms in vitro specifically due to uptake by the maltodextrin transport pathway. Due to the high activity of the bacterial maltodextrin transporter and the hydrophilic nature of MDP (meaning it cannot diffuse through mammalian cell membranes [70]), the probe demonstrated high signal to noise and showed high sensitivity compared to other bacterial targeting agents, including ZnDPA [71]. However, as with all metabolite-based probes, accumulation of the probe is likely to be dependent on the metabolic state of the bacteria.
Glucose-6-phosphate (G6P) is a sugar utilised only by certain bacteria; including E. coli and S. aureus [72]. It is transported into bacteria via a Universal Hexose Phosphate Transporter (UHPT) which is not expressed at the cell surface of mammalian cells. Therefore, UHPT is an ideal candidate for delivery of targeted bacteria specific probes. The feasibility of targeting UHPT for infection detection has been demonstrated with the G6P analogue [18F]FDG-6-P by nuclear imaging techniques [73]. Converting glucose to glucose-6-phosphate is achieved through a very simple hexokinase reaction; therefore, it could be possible to convert fluorescently labelled glucose to fluorescently labelled glucose-6-phosphate. Both environmentally sensitive NBD [74, 75] and NIR [76] glucose derivatives have been reported. Whilst NBD-glucose has been shown to be transported by specifically glucose transporters, the NIR labelled equivalent was not, speculatively due to the larger size of the NIR fluorophore [77]. However, it is not known whether the phosphorylated versions of these probes would be recognised by the UHPT.
Sorbitol is a metabolite utilised by the Gram negative Enterobacteriaceae family of bacteria [78]. These bacteria include E. coli, K. pneumoniae and Pseudomonas aeruginosa and are the main cause of Gram negative bacterial infections in humans. In order to target these bacteria in vivo, [18F]FDG was modified to produce 2-[18F]-fluorodeoxysorbitol ([18F]FDS). The probe was able to specifically differentiate sites of Enterobacteriaceae infection from Gram positive infection and sites of sterile inflammation in a range of infection sites; including brain and lung. Additionally, this probe was able to monitor infection levels during treatment of antibiotic sensitive and resistant E. coli infections [79]. The biodistribution and stability of [18F]FDS has since been evaluated clinically in a healthy volunteer, and was shown to be consistent with that of murine models [80]. Despite this promising route for targeting Enterobacteriaceae, fluorescently labelled sorbitol derivatives for optical imaging are yet to be reported.
Concanavalin A nanoprobe
Concanavalin A (Con A) is a lectin-binding protein with a high affinity for cell-surface mannose residues and other polysaccharides within the cell wall of Gram positive and Gram negative bacteria. To exploit Con A as a bacterial imaging tool, Con A was conjugated to a nanoparticle carrier and near NIR dye IR750 [81]. The Con A-IR750 nanoprobe was demonstrated to adhere to sites of superficial S. aureus wound site infections, and at sites of infected transcutaneously implanted catheters in mice. For each of these infection models the nanoprobe was added topically followed by a wash step and imaging. Fluorescence signal from the wound site was detected and increased proportionally with bacterial load.
Nuclease-activated FRET probe
Nucleases are a diverse group of enzymes responsible for the degradation of nucleic acids (through specific cleavage of the phosphodiester bonds between nucleotide subunits). Several modified oligonucleotides have been identified which show resistance to degradation by mammalian nucleases, but are susceptible to cleavage by certain bacterial nucleases [82]. One of the identified oligonucleotides was sensitive to digestion specifically by S. aureus Micrococcal Nuclease (MN), but resistant to mammalian serum nucleases [47].
This identified oligonucleotide was further modified to incorporate a FRET (fluorescence resonance energy transfer) system, where a Cy5.5 fluorescence group was incorporated 5′ of the enzyme cleavage site, and quenching groups (ZEN and Iowa Black RQ) 3′ of the cleavage site. The probe was silent until contact and cleavage by MN, enabling identification of S. aureus infections in vivo within 15 min of i.v administration.
β-Lactamase-activated FRET probe
β-Lactamase is an enzyme produced by many bacteria and confers resistance to β-lactam antibiotics, such as penicillin [83–86]. The structure of β-lactamase encoded by Mycobacterium tuberculosis (M. tb) differs to that produced by other bacterial species and is known to be highly active [87, 88]. It has therefore has been exploited for detection of M. tb using a FRET-based NIR (Cy5.5 and QSY21/QSY22) substrate for M. tb β-lactamase. A number of probes were evaluated in subcutaneous in vivo murine models of M. tb infections [46], with each candidate accumulating and being activated at the site of infection. The probe with the highest sensitivity was selected for further investigation of pulmonary M. tb infection. Following i.v administration the probe was able to reach the site of infection, was activated and was detectible in situ with a high signal to noise. Signal was not detected in the lungs of non-infected mice both in situ and ex vivo.
Prothrombin
A mechanism of S. aureus immune evasion is to clot human blood through the binding of staphylocoagulase to prothrombin [89–91]. This phenomenon has been exploited to enable S. aureus detection in vivo in mouse models of endocarditis by optical imaging of an Alexa Fluor 680 labelled prothrombin analogue, AF680-Pro-T [92]. Accumulation of the probe at the infection site was shown to be specific to coagulase positive S. aureus; with no probe detected at sites of coagulase negative Staphylococcus epidermidis infection or non-infected controls.
Nitroreductase-activated probe
Nitroreductases are widespread throughout both Gram positive and Gram negative bacterial species, and therefore their exploitation through optical imaging would act as a general bacterial infection identifier [93]. This has been demonstrated by using the self-quenched NIR fluorophore CytoCy5S, which is reduced by nitroreductase to yield fluorescence signal [94]. Through this approach it was possible to detect a number of pathogens in different murine infection models in vivo by whole body imaging, including intramuscular E. coli infections, liver and spleen Salmonella typhimurium infections, and tumour colonisation by E. coli and Bifidobacterium breve.
Antibiotics
Historically, there have been numerous attempts at developing antibiotics as bacterial imaging agents [95]. The most widely explored was the commercially available probe Infecton ([99mTc]-ciprofloxacin) [96, 97]. Radiolabelled ciprofloxacin was anticipated to act as a general identifier of Gram positive and Gram negative bacterial infection; however, in vivo investigations and patient clinical studies demonstrated varying degrees of success; indicating that it may not enable a clear distinction between bacterial infection and sterile inflammation [98–101]. Due to the inconclusive data, development of infection was ceased in 2007.
More recently, a NIR-labelled vancomycin probe has begun in vivo evaluation. Vancomycin binds directly to the cell wall of Gram positive bacteria [102], and therefore accumulates at sites of infection. When Vancomycin-IRDye800CW was injected i.v into mice harbouring bilateral S. aureus and E. coli infections, the probe could be detected selectively in the S. aureus infected flank [103]. Moreover, this group also studied the feasibility of using Vancomycin-IRDye800CW to detect Gram positive biofilms on implanted medical devices within human cadavers. Osteosynthetic devices were coated with S. epidemidis biofilms pre-labelled with Vancomycin-IRDye800CW, and implanted into lower leg of cadavers. Fluorescence signal was detected through the skin using an intraoperative clinical multispectral imaging camera, whereas no signal was detected for bacteria free controls. It has not yet been determined whether this approach would be suitable for imaging deeper infections within the body, such as hip prosthesis or endocarditis.
A major drawback of targeting bacteria with radiolabelled antibiotics is that bacteria which are already resistant to the drug are unlikely to accumulate the probe, and as such could result in false negative results. Moreover, there are questions surrounding what effect administering sub-lethal doses of antibiotic probe may have on promoting antimicrobial resistance [104]; however, the dose required for imaging will remain low and this is likely to not be an issue.
Bacteriophage
The bacteriophage M13 (a filamentous, non-lytic phage with natural affinity for the E. coli F’ pili [105, 106]) has been exploited for bacterial targeting in vivo. Bacteriophage M13 was used as a scaffold for attaching single-walled carbon nanotubules (SWNTs). These fluoresce in the NIR-II region of the electromagnetic spectrum (900–1400 nm) [107], resulting in reduced tissue scattering and enhanced depth penetration, providing a potential improved signal to noise by 100-fold compared to other NIR probes (700–900 nm) [108–111]. The M13-SWNT probe was able to discriminate between F′ positive and F′ negative E. coli soft tissue infections in a mouse model with a custom made NIR-II imaging device. The M13-SWNT probe was further modified to contain an anti-S. aureus antibody (anti-S. aureus-M13-SWNT), which enabled specific targeting to soft tissue and endocarditis S. aureus infections in mice, and demonstrated the potential of bacteriophage-mediated imaging of infections other than E. coli.
Future perspectives
As the global number of MDR pathogens continues to rise, the urgency to answer the question of whether to treat or not, whether treatment is effective, and when to stop treatment on a case-by-case basis is imperative. To this end, a range of bacterial probe targets have been identified and the approaches under development to image these are varied. Whilst the emphasis in recent years has been to develop tools for specifically imaging infection by nuclear medicine, the cost, short shelf-life and radiation dose exposure are all undesirable characteristics inherent to this approach. The expanding field of optical probe design presents an alternative means to detect infections in situ whilst circumventing many of the drawbacks of nuclear imaging. Whilst optical imaging approaches do have several potential limitations; such as low sensitivity, poor depth penetration and unavoidable tissue autofluorescence; advances in detection technology and the availability of self-quenched, FRET-systems, environmentally activated, and ‘always-on’ fluorophores with distinct spectral properties could minimise these limitations and offer advantages for multiplexing probes and improve signal to noise compared to ‘always-on’ radionuclides.
It is clear that infection specific molecular probes for both nuclear and optical imaging modalities should continue to be developed in order to solve the unmet clinical need for rapid and accurate in situ diagnostics of a range of bacterial species. It is unlikely that whole-body optical imaging will ever be feasible to identify unknown infection loci sites. For this type of investigation, radiolabelled probes offer a clear advantage. Despite this, optical probes my offer advantages during surgical intervention, identifying prosthetic joint infections or in locations accessible by optical endoscopes, such as for pulmonary infection.
There are currently no molecular probes licensed for clinical optical imaging of infection. However, the field of optical imaging of infection is rapidly expanding and is poised for evaluation of lead probes in first-in-man clinical studies within the coming years; where on-target labelling, ability to target MDR bacteria, ability to target bacteria within a biofilm, probe sensitivity limits and probe biodistribution will be evaluated. We predict that the likeliest probes to be accelerated into clinical practice will be fluorescently labelled antibiotic derivatives and modified antimicrobial peptides. The versatility of optical molecular imaging of bacterial infections is immense and the potential to multiplex to image host–pathogen interactions will lead to a new generation of biological insights.
References
CDC (2013) Antibiotic resistance threats in the United States. Centers for Disease Control and Prevention, USA
ECDC (2009) The bacterial challenge: time to react. European Centre for Disease Prevention and Control, Stockholm
WHO (2014) Antimicrobial resistance: global report on surveillance 2014. World Health Organisation, Geneva. URL: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1
Beceiro A, Tomás M, Bou G (2013) Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world? Clin Microbiol Rev 26(2):185–230
ECDC (2012) Antimicrobial resistance surveillance in Europe 2011. European Centre for Disease Prevention and Control, Stockholm
ECDC (2013) Antimicrobial resistance surveillance in Europe 2012. European Centre for Disease Prevention and Control, Stockholm
WHO (2015) Global action plan on antimicrobial resistance. World Health Organisation, Geneva 2015. URL: http://apps.who.int/iris/bitstream/10665/193736/1/9789241509763_eng.pdf?ua=1
Friedman ND, Temkin E, Carmeli Y (2016) The negative impact of antibiotic resistance. Clin Microbiol Infect. doi:10.1016/j.cmi.2015.12.002
Chacko TK, Zhuang H, Nakhoda KZ, Moussavian B, Alavi A (2003) Applications of fluorodeoxyglucose positron emission tomography in the diagnosis of infection. Nucl Med Commun 24(6):615–624
De Winter F, Vogelaers D, Gemmel F, Dierckx RA (2002) Promising role of 18-F-fluoro-d-deoxyglucose positron emission tomography in clinical infectious diseases. Eur J Clin Microbiol Infect Dis 21(4):247–257
Kwee TC, Kwee RM, Alavi A (2008) FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur J Nucl Med Mol Imaging 35(11):2122–2132
Stumpe KD, Dazzi H, Schaffner A, von Schulthess GK (2000) Infection imaging using whole-body FDG-PET. Eur J Nucl Med 27(7):822–832
Haroon A, Zumla A, Bomanji J (2012) Role of fluorine 18 fluorodeoxyglucose positron emission tomography-computed tomography in focal and generalized infectious and inflammatory disorders. Clin Infect Dis 54(9):1333–1341
Zhuang H, Duarte PS, Pourdehnad M, Maes A, Van Acker F, Shnier D, Garino JP, Fitzgerald RH, Alavi A (2001) The promising role of 18F-FDG PET in detecting infected lower limb prosthesis implants. J Nucl Med 42(1):44–48
Zhuang H, Yu JQ, Alavi A (2005) Applications of fluorodeoxyglucose-PET imaging in the detection of infection and inflammation and other benign disorders. Radiol Clin North Am 43(1):121–134
Signore A, Glaudemans AW (2011) The molecular imaging approach to image infections and inflammation by nuclear medicine techniques. Ann Nucl Med 25(10):681–700
Palestro CJ, Love C, Bhargava KK (2009) Labeled leukocyte imaging: current status and future directions. Q J Nucl Med Mol Imaging 53(1):105–123
Kumar V (2005) Radiolabeled white blood cells and direct targeting of micro-organisms for infection imaging. Q J Nucl Med Mol Imaging 49(4):325–338
Aksoy SY, Asa S, Ozhan M, Ocak M, Sager MS, Erkan ME, Halac M, Kabasakal L, Sonmezoglu K, Kanmaz B (2014) FDG and FDG-labelled leucocyte PET/CT in the imaging of prosthetic joint infection. Eur J Nucl Med Mol Imaging 41(3):556–564
Palestro CJ (2014) Nuclear medicine and the failed joint replacement: past, present, and future. World J Radiol 6(7):446–458
Glaudemans AW, Galli F, Pacilio M, Signore A (2013) Leukocyte and bacteria imaging in prosthetic joint infection. Eur Cell Mater 25:61–77
Liu X, Cheng D, Gray BD, Wang Y, Akalin A, Rusckowski M, Pak KY, Hnatowich DJ (2012) Radiolabeled Zn-DPA as a potential infection imaging agent. Nucl Med Biol 39(5):709–714
Nibbering PH, Welling MM, Paulusma-Annema A, Brouwer CPJM, Lupetti A, Pauwels EKJ (2004) 99mTc-Labeled UBI 29–41 peptide for monitoring the efficacy of antibacterial agents in mice infected with Staphylococcus aureus. J Nucl Med 45(2):321–326
Welling MM, Lupetti A, Balter HS, Lanzzeri S, Souto B, Rey AM, Savio EO, Paulusma-Annema A, Pauwels EK, Nibbering PH (2001) 99mTc-labeled antimicrobial peptides for detection of bacterial and Candida albicans infections. J Nucl Med 42(5):788–794
Welling MM, Mongera S, Lupetti A, Balter HS, Bonetto V, Mazzi U, Pauwels EK, Nibbering PH (2002) Radiochemical and biological characteristics of 99mTc-UBI 29–41 for imaging of bacterial infections. Nucl Med Biol 29(4):413–422
Akhtar M, Khan M, Khan B, Irfanullah J, Afzal M, Khan M, Nadeem M, Jehangir M, Imran M (2008) An imaging analysis of 99mTc-UBI (29–41) uptake in S. aureus infected thighs of rabbits on ciprofloxacin treatment. Eur J Nucl Med Mol Imaging 35(6):1056–1064
Akhtar MS, Qaisar A, Irfanullah J, Iqbal J, Khan B, Jehangir M, Nadeem MA, Khan MA, Afzal MS, Ul-Haq I et al (2005) Antimicrobial peptide 99mTc-ubiquicidin 29–41 as human infection-imaging agent: clinical trial. J Nucl Med 46(4):567–573
Brouwer CP, Gemmel FF, Welling MM (2010) Evaluation of 99mTc-UBI 29–41 scintigraphy for specific detection of experimental multidrug-resistant Staphylococcus aureus bacterial endocarditis. Q J Nucl Med Mol Imaging 54(4):442–450
Davis SL, Be NA, Lamichhane G, Nimmagadda S, Pomper MG, Bishai WR, Jain SK (2009) Bacterial thymidine kinase as a non-invasive imaging reporter for Mycobacterium tuberculosis in live animals. PLoS One 4(7):e6297
Cho S, Yung R, Jeffrey-Kwanisai A, Foss C, Nimmagadda S, Pomper M (2013) 124I-FIAU thymidine kinase-based PET imaging of lung infection. J Nucl Med Meet Abstr 54:649
Pullambhatla M, Tessier J, Beck G, Jedynak B, Wurthner JU, Pomper MG (2012) [(125)I]FIAU imaging in a preclinical model of lung infection: quantification of bacterial load. Am J Nucl Med Mol Imaging 2(3):260–270
Signore A, Lauri C, Galli F (2014) Radiolabelled probes targeting infection and inflammation for personalized medicine. Curr Pharm Des 20(14):2338–2345
Sasser TA, Van Avermaete AE, White A, Chapman S, Johnson JR, Van Avermaete T, Gammon ST, Leevy WM (2013) Bacterial infection probes and imaging strategies in clinical nuclear medicine and preclinical molecular imaging. Curr Top Med Chem 13(4):479–487
Keereweer S, Van Driel PB, Snoeks TJ, Kerrebijn JD, Baatenburg de Jong RJ, Vahrmeijer AL, Sterenborg HJ, Lowik CW (2013) Optical image-guided cancer surgery: challenges and limitations. Clin Cancer Res 19(14):3745–3754
Vahrmeijer AL, Hutteman M, van der Vorst JR, van de Velde CJ, Frangioni JV (2013) Image-guided cancer surgery using near-infrared fluorescence. Nat Rev Clin Oncol 10(9):507–518
Gioux S, Choi HS, Frangioni JV (2010) Image-guided surgery using invisible near-infrared light: fundamentals of clinical translation. Mol Imaging 9(5):237–255
Escobedo JO, Rusin O, Lim S, Strongin RM (2010) NIR dyes for bioimaging applications. Curr Opin Chem Biol 14(1):64–70
Koide Y, Urano Y, Hanaoka K, Piao W, Kusakabe M, Saito N, Terai T, Okabe T, Nagano T (2012) Development of NIR fluorescent dyes based on Si-rhodamine for in vivo imaging. J Am Chem Soc 134(11):5029–5031
Su D, Teoh CL, Samanta A, Kang NY, Park SJ, Chang YT (2015) The development of a highly photostable and chemically stable zwitterionic near-infrared dye for imaging applications. Chem Commun (Camb) 51(19):3989–3992
Jacques SL (2013) Optical properties of biological tissues: a review. Phys Med Biol 58(11):R37–R61
Welsher K, Sherlock SP, Dai H (2011) Deep-tissue anatomical imaging of mice using carbon nanotube fluorophores in the second near-infrared window. Proc Natl Acad Sci USA 108(22):8943–8948
Stolik S, Delgado JA, Perez A, Anasagasti L (2000) Measurement of the penetration depths of red and near infrared light in human “ex vivo” tissues. J Photochem Photobiol B 57(2–3):90–93
Alander JT, Kaartinen I, Laakso A, Patila T, Spillmann T, Tuchin VV, Venermo M, Valisuo P (2012) A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging 2012:940585
Chattopadhyay A (1990) Chemistry and biology of N-(7-nitrobenz-2-oxa-1,3-diazol-4-yl)-labeled lipids: fluorescent probes of biological and model membranes. Chem Phys Lipids 53(1):1–15
Akram AR, Avlonitis N, Lilienkampf A, Perez-Lopez AM, McDonald N, Chankeshwara SV, Scholefield E, Haslett C, Bradley M, Dhaliwal K (2015) A labelled-ubiquicidin antimicrobial peptide for immediate in situ optical detection of live bacteria in human alveolar lung tissue. Chem Sci 6(12):6971–6979
Kong Y, Yao H, Ren H, Subbian S, Cirillo SL, Sacchettini JC, Rao J, Cirillo JD (2010) Imaging tuberculosis with endogenous beta-lactamase reporter enzyme fluorescence in live mice. Proc Natl Acad Sci USA 107(27):12239–12244
Hernandez FJ, Huang L, Olson ME, Powers KM, Hernandez LI, Meyerholz DK, Thedens DR, Behlke MA, Horswill AR, McNamara JO 2nd (2014) Noninvasive imaging of Staphylococcus aureus infections with a nuclease-activated probe. Nat Med 20(3):301–306
Saeed S, Zafar J, Khan B, Akhtar A, Qurieshi S, Fatima S, Ahmad N, Irfanullah J (2013) Utility of 99mTc-labelled antimicrobial peptide ubiquicidin (29–41) in the diagnosis of diabetic foot infection. Eur J Nucl Med Mol Imaging 40(5):737–743
Sepulveda-Mendez J, de Murphy CA, Rojas-Bautista JC, Pedraza-Lopez M (2010) Specificity of 99mTc-UBI for detecting infection foci in patients with fever in study. Nucl Med Commun 31(10):889–895
Assadi M, Vahdat K, Nabipour I, Sehhat MR, Hadavand F, Javadi H, Tavakoli A, Saberifard J, Kalantarhormozi MR, Zakani A et al (2011) Diagnostic value of 99mTc-ubiquicidin scintigraphy for osteomyelitis and comparisons with 99mTc-methylene diphosphonate scintigraphy and magnetic resonance imaging. Nucl Med Commun 32(8):716–723
Aryana K, Hootkani A, Sadeghi R, Davoudi Y, Naderinasab M, Erfani M, Ayati N (2012) (99m)Tc-labeled ubiquicidin scintigraphy: a promising method in hip prosthesis infection diagnosis. Nuklearmedizin 51(4):133–139
Nazari B, Azizmohammadi Z, Rajaei M, Karami M, Javadi H, Assadi M, Asli IN (2011) Role of 99mTc-ubiquicidin 29–41 scintigraphy to monitor antibiotic therapy in patients with orthopedic infection: a preliminary study. Nucl Med Commun 32(8):745–751
Chen H, Liu C, Chen D, Madrid K, Peng S, Dong X, Zhang M, Gu Y (2015) Bacteria-targeting conjugates based on antimicrobial peptide for bacteria diagnosis and therapy. Mol Pharm 12(7):2505–2516
Chen H, Zhang M, Li B, Chen D, Dong X, Wang Y, Gu Y (2015) Versatile antimicrobial peptide-based ZnO quantum dots for in vivo bacteria diagnosis and treatment with high specificity. Biomaterials 53:532–544
Welling MM, Bunschoten A, Kuil J, Nelissen RG, Beekman FJ, Buckle T, van Leeuwen FW (2015) Development of a hybrid tracer for SPECT and optical imaging of bacterial infections. Bioconjug Chem 26(5):839–849
van den Berg NS, Brouwer OR, Schaafsma BE, Matheron HM, Klop WM, Balm AJ, van Tinteren H, Nieweg OE, van Leeuwen FW, Valdes Olmos RA (2015) Multimodal surgical guidance during sentinel node biopsy for melanoma: combined gamma tracing and fluorescence imaging of the sentinel node through use of the hybrid tracer indocyanine green-(99m)Tc-nanocolloid. Radiology 275(2):521–529
Brouwer OR, van den Berg NS, Matheron HM, van der Poel HG, van Rhijn BW, Bex A, van Tinteren H, Valdes Olmos RA, van Leeuwen FW, Horenblas S (2014) A hybrid radioactive and fluorescent tracer for sentinel node biopsy in penile carcinoma as a potential replacement for blue dye. Eur Urol 65(3):600–609
Leevy WM, Johnson JR, Lakshmi C, Morris J, Marquez M, Smith BD (2006) Selective recognition of bacterial membranes by zinc(II)-coordination complexes. Chem Commun 15:1595–1597
DiVittorio KM, Leevy WM, O’Neil EJ, Johnson JR, Vakulenko S, Morris JD, Rosek KD, Serazin N, Hilkert S, Hurley S et al (2008) Zinc(II) coordination complexes as membrane-active fluorescent probes and antibiotics. Chembiochem 9(2):286–293
White AG, Gray BD, Pak KY, Smith BD (2012) Deep-red fluorescent imaging probe for bacteria. Bioorg Med Chem Lett 22(8):2833–2836
Leevy WM, Gammon ST, Jiang H, Johnson JR, Maxwell DJ, Jackson EN, Marquez M, Piwnica-Worms D, Smith BD (2006) Optical imaging of bacterial infection in living mice using a fluorescent near-infrared molecular probe. J Am Chem Soc 128(51):16476–16477
Leevy WM, Gammon ST, Johnson JR, Lampkins AJ, Jiang H, Marquez M, Piwnica-Worms D, Suckow MA, Smith BD (2008) Noninvasive optical imaging of Staphylococcus aureus bacterial infection in living mice using a bis-dipicolylamine-zinc(II) affinity group conjugated to a near-infrared fluorophore. Bioconjug Chem 19(3):686–692
Johnson JR, Fu N, Arunkumar E, Leevy WM, Gammon ST, Piwnica-Worms D, Smith BD (2007) Squaraine rotaxanes: superior substitutes for Cy-5 in molecular probes for near-infrared fluorescence cell imaging. Angew Chem Int Ed Engl 46(29):5528–5531
White AG, Fu N, Leevy WM, Lee JJ, Blasco MA, Smith BD (2010) Optical imaging of bacterial infection in living mice using deep-red fluorescent squaraine rotaxane probes. Bioconjug Chem 21(7):1297–1304
Hanshaw RG, Lakshmi C, Lambert TN, Johnson JR, Smith BD (2005) Fluorescent detection of apoptotic cells by using zinc coordination complexes with a selective affinity for membrane surfaces enriched with phosphatidylserine. Chembiochem 6(12):2214–2220
Thakur ML, Zhang K, Paudyal B, Devakumar D, Covarrubias M, Cheng C, Gray B, Wickstrom E, Pak K (2012) Targeting apoptosis for optical imaging of infection. Mol Imaging Biol 14(2):163–171
Dahl MK, Manson MD (1985) Interspecific reconstitution of maltose transport and chemotaxis in Escherichia coli with maltose-binding protein from various enteric bacteria. J Bacteriol 164(3):1057–1063
Boos W, Shuman H (1998) Maltose/maltodextrin system of Escherichia coli: transport, metabolism, and regulation. Microbiol Mol Biol Rev 62(1):204–229
Gopal S, Berg D, Hagen N, Schriefer EM, Stoll R, Goebel W, Kreft J (2010) Maltose and maltodextrin utilization by Listeria monocytogenes depend on an inducible ABC transporter which is repressed by glucose. PLoS One 5(4):e10349
Reuss R, Ludwig J, Shirakashi R, Ehrhart F, Zimmermann H, Schneider S, Weber MM, Zimmermann U, Schneider H, Sukhorukov VL (2004) Intracellular delivery of carbohydrates into mammalian cells through swelling-activated pathways. J Membr Biol 200(2):67–81
Ning X, Lee S, Wang Z, Kim D, Stubblefield B, Gilbert E, Murthy N (2011) Maltodextrin-based imaging probes detect bacteria in vivo with high sensitivity and specificity. Nat Mater 10(8):602–607
Winkler HH (1973) Distribution of an inducible hexose-phosphate transport system among various bacteria. J Bacteriol 116(2):1079–1081
Murphy AG, O’Keeffe KM, Lalor SJ, Maher BM, Mills KH, McLoughlin RM (2015) Correction: Staphylococcus aureus infection of mice expands a population of memory gammadelta T cells that are protective against subsequent infection. J Immunol 194(9):4588
Zou C, Wang Y, Shen Z (2005) 2-NBDG as a fluorescent indicator for direct glucose uptake measurement. J Biochem Biophys Methods 64(3):207–215
O’Neil RG, Wu L, Mullani N (2005) Uptake of a fluorescent deoxyglucose analog (2-NBDG) in tumor cells. Mol Imaging Biol 7(6):388–392
Cheng Z, Levi J, Xiong Z, Gheysens O, Keren S, Chen X, Gambhir SS (2006) Near-infrared fluorescent deoxyglucose analogue for tumor optical imaging in cell culture and living mice. Bioconjug Chem 17(3):662–669
Tseng JC, Wang Y, Banerjee P, Kung AL (2012) Incongruity of imaging using fluorescent 2-DG conjugates compared to 18F-FDG in preclinical cancer models. Mol Imaging Biol 14(5):553–560
Isono M, Nakanishi I, Sasajima K-I, Motizuki K, Kanzaki T, Okazaki H, Yoshino H (1968) 2-keto-l-gulonic acid fermentation. Part I. Paper chromatographic characterization of metabolic products from sorbitol and l-sorbose by various bacteria. Agric Biol Chem 32(4):424–431
Weinstein EA, Ordonez AA, DeMarco VP, Murawski AM, Pokkali S, MacDonald EM, Klunk M, Mease RC, Pomper MG, Jain SK (2014) Imaging Enterobacteriaceae infection in vivo with 18F-fluorodeoxysorbitol positron emission tomography. Sci Transl Med 6(259):259ra146
Yao S, Xing H, Zhu W, Wu Z, Zhang Y, Ma Y, Liu Y, Huo L, Zhu Z, Li Z et al (2015) Infection imaging with [18F]-FDS and first-in-human evaluation. Nucl Med Biol 43(3):206–214
Tang EN, Nair A, Baker DW, Hu W, Zhou J (2014) In vivo imaging of infection using a bacteria-targeting optical nanoprobe. J Biomed Nanotechnol 10(5):856–863
Hernandez FJ, Stockdale KR, Huang L, Horswill AR, Behlke MA, McNamara JO 2nd (2012) Degradation of nuclease-stabilized RNA oligonucleotides in Mycoplasma-contaminated cell culture media. Nucleic Acid Ther 22(1):58–68
Knox JR, Moews PC, Frere JM (1996) Molecular evolution of bacterial beta-lactam resistance. Chem Biol 3(11):937–947
Hermann JC, Ridder L, Holtje HD, Mulholland AJ (2006) Molecular mechanisms of antibiotic resistance: QM/MM modelling of deacylation in a class A beta-lactamase. Org Biomol Chem 4(2):206–210
Davies J (1994) Inactivation of antibiotics and the dissemination of resistance genes. Science 264(5157):375–382
Fisher JF, Mobashery S (2009) Three decades of the class A beta-lactamase acyl-enzyme. Curr Protein Pept Sci 10(5):401–407
Wang F, Cassidy C, Sacchettini JC (2006) Crystal structure and activity studies of the Mycobacterium tuberculosis beta-lactamase reveal its critical role in resistance to beta-lactam antibiotics. Antimicrob Agents Chemother 50(8):2762–2771
Campbell RE (2004) Realization of beta-lactamase as a versatile fluorogenic reporter. Trends Biotechnol 22(5):208–211
Friedrich R, Panizzi P, Fuentes-Prior P, Richter K, Verhamme I, Anderson PJ, Kawabata S, Huber R, Bode W, Bock PE (2003) Staphylocoagulase is a prototype for the mechanism of cofactor-induced zymogen activation. Nature 425(6957):535–539
Panizzi P, Friedrich R, Fuentes-Prior P, Richter K, Bock PE, Bode W (2006) Fibrinogen substrate recognition by staphylocoagulase. (pro)thrombin complexes. J Biol Chem 281(2):1179–1187
Loeb L (1903) The influence of certain bacteria on the coagulation of the blood. J Med Res 10(3):407–419
Panizzi P, Nahrendorf M, Figueiredo JL, Panizzi J, Marinelli B, Iwamoto Y, Keliher E, Maddur AA, Waterman P, Kroh HK et al (2011) In vivo detection of Staphylococcus aureus endocarditis by targeting pathogen-specific prothrombin activation. Nat Med 17(9):1142–1146
Stanton M, Cronin M, Lehouritis P, Tangney M (2015) In vivo bacterial imaging without engineering; a novel probe-based strategy facilitated by endogenous nitroreductase enzymes. Curr Gene Ther 15(3):277–288
Roldan MD, Perez-Reinado E, Castillo F, Moreno-Vivian C (2008) Reduction of polynitroaromatic compounds: the bacterial nitroreductases. FEMS Microbiol Rev 32(3):474–500
Mirshojaei SF (2015) Advances in infectious foci imaging using 99mTc radiolabelled antibiotics. J Radioanal Nucl Chem 304(3):975–988
Hall AV, Solanki KK, Vinjamuri S, Britton KE, Das SS (1998) Evaluation of the efficacy of 99mTc-Infecton, a novel agent for detecting sites of infection. J Clin Pathol 51(3):215–219
Solanki K, Bomanji J, Siraj Q, Small M, Britton K (1993) Tc-99m Infecton-a new class of radiopharmaceutical for imaging infection. J Nucl Med (abstract) 34(5):P119
Sarda L, Saleh-Mghir A, Peker C, Meulemans A, Cremieux AC, Le Guludec D (2002) Evaluation of (99m)Tc-ciprofloxacin scintigraphy in a rabbit model of Staphylococcus aureus prosthetic joint infection. J Nucl Med 43(2):239–245
Peremans K, De Winter F, Janssens L, Dumont F, Van Bree H, Dierckx R (2002) An infected hip prosthesis in a dog diagnosed with a 99mTc-ciprofloxacin (infecton) scan. Vet Radiol Ultrasound 43(2):178–182
Sarda L, Cremieux AC, Lebellec Y, Meulemans A, Lebtahi R, Hayem G, Genin R, Delahaye N, Huten D, Le Guludec D (2003) Inability of 99mTc-ciprofloxacin scintigraphy to discriminate between septic and sterile osteoarticular diseases. J Nucl Med 44(6):920–926
Malamitsi J, Giamarellou H, Kanellakopoulou K, Dounis E, Grecka V, Christakopoulos J, Koratzanis G, Antoniadou A, Panoutsopoulos G, Batsakis C et al (2003) Infecton: a 99mTc-ciprofloxacin radiopharmaceutical for the detection of bone infection. Clin Microbiol Infect 9(2):101–109
Hiramatsu K (2001) Vancomycin-resistant Staphylococcus aureus: a new model of antibiotic resistance. Lancet Infect Dis 1(3):147–155
van Oosten M, Schafer T, Gazendam JA, Ohlsen K, Tsompanidou E, de Goffau MC, Harmsen HJ, Crane LM, Lim E, Francis KP et al (2013) Real-time in vivo imaging of invasive- and biomaterial-associated bacterial infections using fluorescently labelled vancomycin. Nat Commun 4:2584
Kohanski MA, DePristo MA, Collins JJ (2010) Sublethal antibiotic treatment leads to multidrug resistance via radical-induced mutagenesis. Mol Cell 37(3):311–320
Silverman PM, Clarke MB (2010) New insights into F-pilus structure, dynamics, and function. Integr Biol (Camb) 2(1):25–31
O’Callaghan R, Bradley R, Paranchych W (1973) The effect of M13 phage infection upon the F pili of E. coli. Virology 54(1):220–229
Bardhan NM, Ghosh D, Belcher AM (2014) Carbon nanotubes as in vivo bacterial probes. Nat Commun 5:4918
Weissleder R (2001) A clearer vision for in vivo imaging. Nat Biotechnol 19(4):316–317
Smith AM, Mancini MC, Nie S (2009) Bioimaging: second window for in vivo imaging. Nat Nanotechnol 4(11):710–711
Troy TL, Thennadil SN (2001) Optical properties of human skin in the near infrared wavelength range of 1000 to 2200 nm. J Biomed Opt 6(2):167–176
Lim YT, Kim S, Nakayama A, Stott NE, Bawendi MG, Frangioni JV (2003) Selection of quantum dot wavelengths for biomedical assays and imaging. Mol Imaging 2(1):50–64
Acknowledgments
The authors gratefully acknowledge the UK Engineering and Physical Sciences Research Council (EP/K03197X/1) for funding this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Mills has no conflict of interest to disclose. M. Bradley and K. Dhaliwal are founder directors of Edinburgh Molecular Imaging.
Human and animal studies
This article does not contain any studies with human or animal subjects performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mills, B., Bradley, M. & Dhaliwal, K. Optical imaging of bacterial infections. Clin Transl Imaging 4, 163–174 (2016). https://doi.org/10.1007/s40336-016-0180-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-016-0180-0