Abstract
Introduction
Cardiovascular diseases (CVD) are a leading cause of death worldwide, and several modifiable and unmodifiable risk factors contribute to this burden of disability and mortality. Thus, effective cardiovascular prevention relies on appropriate strategies to control risk factors within the frame of unmodifiable traits.
Methods
We conducted a secondary analysis of treated hypertensive adults aged ≥ 50 years enrolled in Save Your Heart. CVD risk and hypertension control rates based on the 2021 updated European Society of Cardiology guidelines were evaluated. Comparisons with previous standards in terms of risk stratification and hypertension control rates were performed.
Results
Among the 512 patients evaluated, with the application of the new parameters for fatal and non-fatal cardiovascular risk assessment, the proportion of individuals at high or very high risk rises from 48.7 to 86.7% of cases. A trend towards lower hypertension control rates was observed based on 2021 European guidelines compared with the 2018 edition (likelihood estimate for difference: 1.76%, 95% CI − 4.1 to 7.6%, p = 0.589).
Conclusions
In this secondary analysis on the Save Your Heart study, the application of the new parameters reported in the European Guidelines for Cardiovascular Prevention 2021 showed a hypertensive population with a very high probability of encountering a fatal or non-fatal cardiovascular event due to failure to control risk factors. For this reason, a better management of risk factors must be the main goal for the patient and all the involved stakeholders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cardiovascular diseases (CVD), including coronary heart disease and stroke, represent the leading cause of death from non-communicable diseases worldwide, trespassing 18.6 millions deaths in the year 2019, meaning around one third of total deaths globally [1]. It was estimated that, only in the US, around 1.2–2.0 million major CVD events could potentially be prevented on a yearly basis if the adult population attained moderate to high cardiovascular health, respectively [2].
Several factors, both modifiable and unmodifiable, contribute to this burden of disease in a fashion that differs among countries [3]. The increasing population aging and the sexually dimorphic susceptibility to CVD through life stages explain part of the observed epidemiological trend [4, 5]. Then, tobacco smoke, high blood pressure (BP), and dyslipidaemia concur in the exacerbation of the individual risk profile [3, 5].
Hypertension is a major contributor to CVD-related disability and mortality [6]. Recent evidence has substantially changed the approach to hypertension management for cardiovascular prevention. Indeed, while the previous European Guidelines [7] placed more permissive target pressures in treated patients over 65 years of age, the new guidelines for cardiovascular prevention [5] have changed the definition of the elderly, resulting in the application of more stringent target pressures in treated patients aged 65–70 years in the absence of chronic kidney disease (CKD) [5]. In parallel, also the prediction model of risk assessment of future cardiovascular events was recently updated (SCORE2), replacing total cholesterol with non-HDL cholesterol among the evaluation parameters, introducing different algorithms available for four distinct European risk regions, and expanding the assessable population with the elderly population over 70 (SCORE2-OP). The ultimate goal of this update was to improve reliability of risk assessment of fatal and non-fatal future cardiovascular events considering the epidemiological changes across European regions [8]. Therefore, the aim of this data review is to evaluate the evolution of cardiovascular risk in hypertensive patients in the light of the updated cardiovascular risk stratification and the new antihypertensive treatment targets. For this purpose, we chose to retrospectively reassess the population previously involved in the Italian observational study Save Your Heart [9].
2 Methods
2.1 Study Design and Population
Study population involved in this data review is the same of Save Your Heart, a cross-sectional, multicentre, observational study, which involved 21 community pharmacies belonging to the Italian Society of Clinical Pharmacy (SIFAC) spread over 15 Italian regions, with the primary aim of determining the prevalence of uncontrolled hypertension as well as that of untreated/uncontrolled hypercholesterolemia and diabetes among treated hypertensive women and men aged 50 years and above without established CVD [9]. Patients who were willing to take self-analysis of BP, lipid profile, and blood glucose as well as to fill out a questionnaire on adherence to current therapies were enrolled. In this regard, the following information was collected: the presence of cardiovascular risk factors (age, smoking habits, reported previous cardiovascular events, reported CKD); demographic data; any known diagnosis of hypercholesterolaemia and/or diabetes; BP (systolic and diastolic); pharmacological treatments taken; lipid profile (total cholesterol, high-density lipoprotein [HDL] and low-density lipoprotein [LDL]) and glycaemia; adherence to current treatments. The secondary analysis of the Save Your Heart study data was possible thanks to the approval for secondary use of these latter obtained by the Ethics Committee ATS Sardinia-Sassari (approval code 294/2021/CE of 16/03/2021) [9]. Signed informed consent was obtained from each participant. The survey and related research fulfil the principles stated in the Declaration of Helsinki [9].
2.2 Cardiovascular Risk Assessment
To estimate cardiovascular risk the revised prediction model Systematic COronary Risk Evaluation 2 (SCORE2) was applied in non-CVD individuals aged 50–69 years among those enrolled in the Save Your Heart study [8]. Briefly, SCORE2 is an updated prediction algorithm that provides age-, sex-, and region-specific estimates for 10-year CVD risk for four distinct European risk regions (low, moderate, high, and very high risk). By combining demographic and clinical features (age, sex, European region, smoking habits, systolic BP values, and non HDL-cholesterol), the algorithm stratifies the risk of future fatal and non-fatal cardiovascular events that is calibrated to current CVD rates, with improved risk prediction for individuals at younger ages and for non-fatal cardiovascular events. In the age range 50–69 years, risk is defined as low-to-moderate for scores < 5%, high for scores between 5 and 10%, and very high for scores equal or higher than 10% [5]. For CVD individuals enrolled in the Save Your Heart study population the classification criteria of European guidelines for the management of dyslipidaemia were considered and, for this reason, included in the highest cardiovascular risk group [10].
Regarding the over-70 non-CVD population, since it was not possible to know the exact age of the participants, it was decided to consider them as belonging to the 70–74 age group of the SCORE2-OP algorithm, underestimating de facto the cardiovascular risk in patients aged over 74. The data collected in this analysis were subsequently compared with the data from the Save Your Heart study with the aim of assessing changes in the distribution of risk in the examined population.
2.3 BP Measurement and Definitions
Participating individuals self-measured BP and answered a questionnaire on adherence to ongoing therapies. BP was measured in sitting position using a validated automatic digital BP monitor (Omron M6®) [11].
BP was used as a continuous (mmHg) and categorical (controlled/uncontrolled hypertension) variable. Based on the 2021 European Society of Cardiology guidelines, uncontrolled hypertension was defined as mean BP ≥ 130/80 mmHg in treated participants with self-reported normal renal function aged < 70 years, and ≥ 140/80 mmHg if ≥ 70 years or with self-reported CKD [5]. This definition of hypertension is more stringent than the one used for the assessment of patients in the Save Your Heart study, which referred to the 2018 European guidelines on the management of high BP. In the latter, uncontrolled hypertension was defined as mean BP ≥ 140/80 mmHg in treated patients aged > 65 years [7]. Hypertension control rates were defined as having BP values below the previously specified targets.
2.4 Covariates of Interest
Covariates of interest in this analysis included main demographics (age as both a dichotomous [< or ≥ 70 years] and a continuous [if < 70 years] variable; sex) and clinical features (body mass index [BMI]; smoking habits; self-reported history of CVD, CKD, high blood cholesterol, and diabetes), which were used for descriptive statistics and cardiovascular risk assessment.
2.5 Statistical Analysis
Differences in participants’ characteristics were evaluated with unpaired t tests for continuous variables (mean ± standard deviation, SD) and χ2 tests for categorical variables (N, %). Hypertension control rates were assessed overall and across strata of SCORE2. The likelihood estimate for the difference in hypertension control rates (95% confidence intervals) according to 2018 ESC/ESH guidelines [7] or 2021 ESC recommendation on cardiovascular prevention [5] was assessed using Yates correction for continuity [4]. Statistical analyses were performed using R (v 4.0.2) [12]. Statistical significance was set at p < 0.05.
3 Results
Of 512 patients enrolled (45.1% women), 36.1% were aged 70 years and older, 2.5% had a history of CKD, 14.6% reported a history of CVD, and 16.4% had diabetes. Their demographic and clinical features according to sex are reported in Table 1. No difference between female and male participants was recorded in terms of age range distribution. Similarly, no sex-based differences were observed in terms of prevalent CKD (p = 0.720), diabetes (p = 0.125), and smoking habits (p = 0.604). Women tended to be leaner, have better BP control, lower 10-year cardiovascular risk, and less prevalent CVD than men.
3.1 Cardiovascular Risk
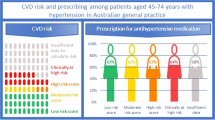
The review of data collected during the Save Your Heart study, in the light of the changes introduced by the 2021 European guidelines on prevention in clinical practice [5], clearly shows how the percentage of patients at high or very high risk increases considerably compared with the previous assessment [9]. Indeed, although the risk in the population aged > 70 years is underestimated, a more overall alarming picture arises than in the Save Your Heart study. Indeed, with the application of the new parameters for fatal and non-fatal cardiovascular risk assessment, the proportion of individuals at high or very high risk rises over 80% of the cases (86.7–41.9% at high risk and 44.7% at very high risk) (Fig. 1), while, with the previous indications, cases with a high or very high risk of a fatal cardiovascular event were almost the half of the population (48.7%). In this assessment, however, it should be considered that, unlike the SCORE, which assesses the risk of fatal cardiovascular events, the SCORE2 also assesses the risk of non-fatal cardiovascular events (Table 2).
3.2 Hypertension Control
As already mentioned, the 512 participants enrolled in the Save Your Heart study were reassessed about the achievement of BP target. According to 2021 ESC guidelines on cardiovascular prevention, 30.3% (95% CI 26.4–34.5%) of participants achieved the target BP values. Women were more likely than men to be at goal based on the updated targets (Fig. 2). In comparison, the hypertension control rate according to 2018 ESC/ESH hypertension guidelines was higher (32.0%, 95% CI 20.8–36.3%), though the observed difference was not significant (1.76%, 95% CI − 4.1 to 7.6%, p = 0.589). No sex-based differences were observed in achieving 2018 BP targets (Fig. 2).
4 Discussion
The main objective of this analysis was to assess the evolution of cardiovascular risk in a hypertensive population in the light of the new European guidelines on prevention in clinical practice [5]. As expected, the updating of the BP targets and the application of the new SCORE2 algorithm revealed a more severe cardiovascular risk and worse hypertension control in the hypertensive population on treatment, previously involved in the Save Your Heart study. In particular, considering the results obtained in this data review, an increase of almost 80% of cases at high or very high risk in comparison with the Save Your Heart study was reported. In parallel, the application of the novel recommended BP targets, which raised the upper age limit for the achievement of optimal goals from 65 to 70 years, confirmed the presence of a large percentage of individuals out of BP targets (69.7%) despite the antihypertensive treatment. Specifically, data review revealed a trend towards a decreased control rate, mostly attributable to men. In fact, unlike what was observed when the 2018 ESC/ESH targets were applied, women were more likely than men to achieve hypertension control based on the updated targets. Also, as expected, a decrease in hypertension control rates was observed with the transition from individuals at low-to-moderate risk towards those at high and very high 10-year risk for cardiovascular events.
Undoubtedly, the obvious reclassification of a larger proportion of study participants as at higher risk as compared with the previous scoring system reflects the inclusion in SCORE2 of risk estimates for nonfatal events. By accounting for the burden of disease in survivors, this change reflects a wide range of socioeconomic implications encompassing disability, quality of life deterioration, caregivers’ exhaustion, and healthcare systems expenditures, thereby conceptually emphasising the already mandatory need for a widespread and effective cardiovascular risk reduction.
Essentially, this analysis confirms the importance of developing and implementing evidence-based preventive and therapeutic approaches to health surveillance and monitoring to prevent inadequately controlled cardiovascular risk factors from contributing critically to increase the overall morbidity and mortality burden.
Similarly, recent real-world data from an Italian nationwide cross-sectional survey on individuals aged 65 years and above, including participants with treated hypertension, showed that a considerable proportion of the latter failed to achieve BP control and was therefore reclassified as having uncontrolled hypertension according to the more stringent goal that was applicable based on their age [13], in agreement with previous reports [14]. The optimization of treatment targets and risk scoring systems according to individuals’ features customises the approach to and the management of risk factors, with the ultimate goal of reducing the burden of disease through a timely and tailored intervention. The observation that a considerable part of the examined population is at high and very high CVD risk and fails to achieve the desirable BP goals raises a warning against therapeutic inertia, rather emphasising the need to avoid undertreatment to achieve higher lifetime benefit, even at an advanced age [4].
Pharmacological treatments can substantially reduce cardiovascular morbidity and mortality, but the effectiveness of such interventions is limited in the case of non-adherence or early discontinuation of therapy. The European guidelines themselves recommend a diagnostic-therapeutic approach, customised for the individual characteristics of these complex patients and obviously takes into account their cardiovascular risk over time. To counteract therapeutic inertia and increase patient adherence, the follow-up of patients, the update and, where possible, the simplification of therapy is fundamental, especially in elderly individuals and/or those undergoing multiple pharmacological treatments.
Sex-based factors, including sex hormones, have a prominent role in hypertension, as supported by the observation of lower BP in premenopausal women and steeper increases in both systolic BP and pulse pressure in postmenopausal women compared with age-matched men [15, 16]. While incident hypertension occurs at faster rates in women than men after middle age [17], women usually show better BP control compared with men [18], although age disparities have been reported. For instance, according to a cross sectional analysis of US primary care clinics, women aged 65–80 years were less likely than men to have controlled hypertension, despite multivariate adjustment [19]. According to our data, more women than men, including those aged 65 years and above, achieved BP values below the recommended target. Women also carried a lower burden of concomitant risk factors and related diseases. Thus, a combination of hormonal, genetic, and environmental factors are likely to contribute to our observations.
This analysis is not without limitations. Age was collected as a categorical variable above the age of 70 years, thus conditioning the estimation of SCORE2 for older persons (SCORE2-OP [20]). Moreover, limitations of the present data review are, substantially the same of Save Your Heart study, which can be attributed to the lack of statistical adjustments for sex, age and years of diagnosis and to the fact that other factors were not taken into account, particularly behavioural factors that would have been difficult to measure objectively. Furthermore, all clinical parameters were derived from self-analyses and the biological parameters were obtained from capillary blood samples.
5 Conclusions
According to the updated cardiovascular risk assessment parameters and the new definition of the elderly population (characterised by more stringent BP targets), reported in the 2021 European Guidelines for cardiovascular prevention, this secondary analysis showed that the majority of the evaluated population (86.7%) has a high or very high risk of incurring fatal and non-fatal cardiovascular events due to the failure to control risk factors. Improving this aspect should therefore be considered a key goal in the management of patients. The participation of several players such as the specialist doctor, the general practitioner and the pharmacist is thus fundamental. A therapeutic approach in line with the European Guidelines shared between all actors involved and patients, a greater awareness of the latter about their cardiovascular risk, periodic updating of therapies and simplification of treatments when possible are winning strategies to achieve a greater control of risk factors and consequently a reduction of fatal and non-fatal cardiovascular events.
Change history
13 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40292-023-00599-w
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–639.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Del Pinto R, Desideri G, Ferri C, Agabiti RE. Real-world antihypertensive treatment patterns, treatment adherence, and blood pressure control in the elderly: an Italian awareness-raising campaign on hypertension by Senior Italia FederAnziani, the Italian Society of Hypertension and the Italian Federation of General Practitioners. High Blood Press Cardiovasc Prev. 2021;28:457–66.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42:3227–337.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mmHg, 1990–2015. JAMA. 2017;317:165–82.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42:2439–54.
Save Your Heart—Studio osservazionale trasversale, multicentrico, italiano, sulla presenza di fattori di rischio cardiovascolare in partecipanti affetti da ipertensione. [cited 12 Sep 2022]. Available: https://springerhealthcare.it/GIHTAD/2022/02/07/save-your-heart-studio-osservazionale-trasversale-multicentrico-italiano-sulla-presenza-di-fattori-di-rischio-cardiovascolare-in-partecipanti-affetti-da-ipertensione/.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Website. Available: Documenti on line STRIDE BP (2021) Validated devices for home blood pressure monitoring. https://stridebp.org/bp-monitors/37-pdfs/734-home?format=pdf&tmpl=component&-box=home.
Rizzo ML. Statistical computing with R. Philadelphia: Chapman & Hall/CRC; 2007. https://doi.org/10.1201/9781420010718.
Del Pinto R, Dobre M, Pagliacci S, Ferri C. Impact of guidelines on hypertension control in the elderly. Curr Pharm Des. 2021;27:1952–9.
Del Pinto R, Pagliacci S, De Feo M, Grassi D, Ferri C, Italian Society of Hypertension and Federfarma. Prevalence of hypertension and associated cardiovascular risk factors among pharmacies customers: an Italian nationwide epidemiological survey. Eur J Prev Cardiol. 2020;27:1228–30.
Wenger NK, Arnold A, Bairey Merz CN, Cooper-DeHoff RM, Ferdinand KC, Fleg JL, et al. Hypertension across a woman’s life cycle. J Am Coll Cardiol. 2018;71:1797–813.
Martins D, Nelson K, Pan D, Tareen N, Norris K. The effect of gender on age-related blood pressure changes and the prevalence of isolated systolic hypertension among older adults: data from NHANES III. J Gend Specif Med. 2001;4(10–3):20.
Coylewright M, Reckelhoff JF, Ouyang P. Menopause and hypertension: an age-old debate. Hypertension. 2008;51:952–9.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–603.
Keyhani S, Scobie JV, Hebert PL, McLaughlin MA. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–55.
SCORE2-OP Working Group and ESC Cardiovascular Risk Collaboration. SCORE2-OP risk prediction algorithms: estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur Heart J. 2021;42:2455–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work and the Open Access publication fees were funded by Servier Italia.
Conflict of interest
The authors Rita Del Pinto, Corrado Giua, Enrico Keber and Claudio Ferri declare that they have no conflict of interest.
Author contributions
CF was responsible for conceptualization, data analysis and interpretation; TM and CF performed the SCORE2 risk assessment; RDP wrote the first draft and edited the manuscript; GE, TM, CG, EK and CF edited the manuscript. All authors read and approved the manuscript.
Additional information
The original article has been updated: Due to textual changes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Del Pinto, R., Giua, C., Keber, E. et al. Impact of 2021 ESC Guidelines for Cardiovascular Disease Prevention on Hypertensive Patients Risk: Secondary Analysis of Save Your Heart Study. High Blood Press Cardiovasc Prev 30, 167–173 (2023). https://doi.org/10.1007/s40292-023-00568-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-023-00568-3