Abstract
Introduction
A possible alternative to pharmacological antihypertensive therapies in grade 1 low risk hypertensive patients or in those experienced drugs adverse effects could be acupuncture.
Aim
we focused on its possible effects on BP both as Office BP (OBP) and as Ambulatory BP Monitoring (ABPM) evaluating it before starting a 6 weeks twice weekly (total 12 session) acupuncture cycle and after 2 months from its completion.
Methods
in this prospective study we treated with acupuncture 45 patients: 24 of them presents high-normal BP values and low cardiovascular risk while 21 patients were on anti-hypertensive drug with slightly uncontrolled BP values (from 140 to 145 mmHg for Systolic BP—SBP—and/or from 90 to 95 mmHg for Diastolic BP—DBP).
Results
regarding SBP, a significant reduction have been observed for office values (from 134.2 ± 15.7 to 125.1 ± 12.2, p = 0.03), and for ABPM 24 h (from 131.1 ± 10.7 to 126.0 ± 10.1, p = 0.01) and day-time values (from 134.7 ± 10.5 to 127.1 ± 18.4, p = 0.02). For DBP, only ABPM 24 h and day-time values showed significant changes (from 85.3 ± 9.1 to 82.1 ± 7.5, p = 0.03; and from 88.5 ± 9.3 to 85.7 ± 7.8, p = 0.02). Within session SBP decrease was − 5.8 mmHg (-3.75%) during the first session while it falls to – 2.1 mmHg (– 1.25%) and stands firmly under 2 mmHg for all the next session. At the last session SBP reduction was − 1.9 mmHg (– 1.6%).
Conclusions
we found a significant reduction in office, 24 h and day-time ABPM SBP determined by a 6-weeks twice weekly acupuncture cycle that lasts at least for the first two months after its completion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hypertension is the leading risk factor for Cardio-Vascular (CV) events that affects more than 1 billion people worldwide [1]. Various pathophysiological factors (environmental factors, psychological stress, oxidative stress, altered dietary habits, excessive sodium intake) could act in genetically predisposed people finally determining elevated Blood Pressure (BP) values.
Lifestyle changes are the first-line therapy, but pharmacological treatment are needed for the majority of patients in order to reach BP target and reduce CV risk. However, owing to its possible adverse effects some patients choose to discontinue antihypertensive drugs.
A possible alternative in grade 1 low risk hypertensive patients or in those who experienced adverse effects with many anti-hypertensive therapies could be acupuncture. It has been extensively evaluated in the field of hypertension with heterogeneous results [2, 3]. Some problem exist when assessment its efficacy such as: (1) the choice of the control group (sham procedure vs. no treatment [4,5,6]); (2) it’s possible use in association with anti-hypertensive drugs [7]; (3) the different acupuncture methods and (4) the choice of the method to evaluate BP response. Regarding the latter the majority of study assess the efficacy only with Office BP (OBP) while only few of them use 24 h BP trough Ambulatory BP Measurement (ABPM) [8, 9].
In this paper we focused on the possible effects of acupuncture of BP evaluating it both as OBP and as ABPM. Patients were evaluated before starting a 6 weeks twice-weekly acupuncture cycle and 2 months after its completion. Furthermore we assess the BP reduction within each acupuncture session.
2 Methods
Study Populations In this prospective study we treated with acupuncture 45 patients: 24 of them presents high-normal BP values and low cardiovascular risk (and so doesn’t fall yet under the indication for anti-hypertensive therapies [1]) while 21 patients were on anti-hypertensive drug with slightly uncontrolled BP values (from 140 to 145 mmHg for Systolic BP—SBP—and/or from 90 to 95 mmHg for Diastolic BP—DBP).
Patients were enrolled from November 2015 to February 2020 from the hypertensive outpatient clinic of the Niguarda Hospital (Milan, Italy).
Exclusion criteria were: pregnancy, epilepsy, secondary hypertension, self-reported bleeding tendency, anticoagulant or dual antiplatelet therapies as well as ongoing acupuncture treatment for other disease.
Before starting acupuncture, biochemical evaluation (fasting glucose, total cholesterol, HDL, LDL, triglycerides and creatinine levels) and a trans-thoracic echocardiography were performed. Height and weight were obtained to calculate Body Mass Index (BMI) and Waist Circumference (WC) was assessed halfway between the lower ribs and the iliac crest.
The study protocol complies with the Declaration of Helsinki and it was approved by the Ethics Committee of the Institutions involved. All participants provided informed written consent after being informed of its nature and purpose.
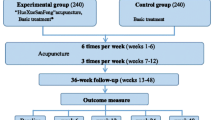
Acupuncture Protocol All the patients received 2 treatments per week for 6 weeks twice-weekly lasting 30 min each (for a total of 12 session). The choice of acupuncture points was made on the basis of the best results in literature [3, 9,10,11,12,13]. In particular they were chosen according to traditional Chinese medicine which considers hypertension ascribable to a deficiency in kidney yin with a relative rise in yang. So, the chosen point were: (1) CV 4 GUAN YUAN: it toning xue and yin acting on kidneys and Yuan-Qi and sedate the Shen; (2) LV 3 TAI CHONG: it lower the yang of the Liver and has a sedative action on the shen; (3): LI 11 WHO: it expels the wind and heat and release the Yang of the Liver; (4): ST 36 ZÚ SAN LÎ: it toning the Spleen-Stomach couple, acting on energy, blood and yin.
The treatment was done with the patient lying in the supine position after sterilizing the areas where the needles will be inserted with 75% alcohol. Tewa disposable steel needles CJ 2530 and CJ 2225 have been used.
BP Evaluation BP measurements (OBP and ABPM) were performed before the initiation of acupuncture (T0) and 2 months after its completion (T1). Furthermore OBP was also measured at the beginning of each acupuncture session and after 10 min from its end (to evaluate within session BP reduction).
With the patient in the sitting position for at least 5 min and with the arm placed at heart level, two semi-automated OBP measurements were taken (OMRON Helthcare Europe, Hoofddorp, The Netherlands) and the average was used for statistics.
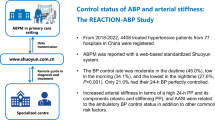
Regarding ABPM, it was performed using the Mobil-O-Graph 24 h Monitor (IEM, Stolberg, Germany). With a sphygmomanometric cuff at the brachial level, measurements were done every 15 min during the day and every 20 min at night. Values were averaged and 24 h, day and night mean values were used for the analysis. The Mobil-O-Graph ABPM device is validated according to BHS and ESH recommendations for peripheral BP [14].
Cardiac Ultrasonography Two-dimensional (2D) echocardiograms were performed by an experienced cardiologist using a dedicated ultrasound machine (General Electric Vivid 9 with an ultrasound transducer of 2.5 MHz) in each patient. 2D high frame rate gray-scale loops of four-chamber, two-chamber and three-chamber views with average frame rate of 50 frames per second (fps) were used in order to measure LV End-Diastolic Diameter (LVEDD), interventricular septum and posterior wall thickness; LV Ejection Fraction (LVEF) was evaluated using the Simpson biplane method.
LV Mass (LVM) was calculated using the Devereux formula [15, 16]: LVM (g) = 0.8*{1.04*[(LVEDD (cm) + interventricular septum + posterior wall thickness (cm))3 – (LVEDD (cm))3]} + 0.6. LVM values were normalized for Body Surface Area (BSA) to obtain the LVM Index (LVMI). We calculated BSA using the DuBois formula: BSA (m2) = 0.007184*height (cm)0.725*weight (kg)0.425.
Statistical Analysis The characteristics of the cohort were described with mean and standard deviation (SD) for continuous variables and with percentages for categorical ones. Comparison between two different time point were conducted with repeated measure t-test.
All analyses were conducted using the SPSS software. All p-values were 2-sided, with p-values < 0.05 considered statistically significant.
3 Results
Population characteristics Table 1 showed the clinical characteristics of enrolled patients. Patients showed a mean age of 53.4 ± 11.2 years, 63.8% of them were females. Regarding CV risk factors 7.1% of patients were diabetic, 47.1% were obese, 8% had peripheral arterial disease, 2.4% had previous myocardial infarction and stroke and 25% had dyslipidemia). At echocardiography, mean LVEF and LVMI were within the normal range.
About half of the patients (47.6%) were on anti-hypertensive therapies with angiotensin receptor blockers, calcium channel blockers and beta-blockers being the most used drugs (22, 17.1 and 17.5% respectively). No significant difference in general, biochemical, echocardiographic and baseline BP data were found between anti-hypertensive treated and untreated patients (Supplementary Table 1).
No adverse reactions occurred during acupuncture cycle and no adverse events were reported from patients till the end of follow-up.
Office and ambulatory blood pressure Table 2; Fig. 1 showed OBP and ABPM values at baseline (T0) and after 2 months (T2) from acupuncture cycle completion.
Regarding SBP, a significant reduction have been observed for office values (from 134.2 ± 15.7 to 125.1 ± 12.2, p = 0.03; mean ∆ = – 8.6 ± 19.1; Fig. 1A), and for ABPM 24 h (from 131.1 ± 10.7 to 126.0 ± 10.1, p = 0.01; mean ∆=-5.1 ± 11.5; Fig. 1C) and day-time values (from 134.7 ± 10.5 to 127.1 ± 18.4, p = 0.02; mean ∆ = – 7.6 ± 16.4). For DBP, only ABPM 24 h (Fig. 1D) and day-time values showed significant changes (from 85.3 ± 9.1 to 82.1 ± 7.5, p = 0.03; mean ∆ = – 3.1 ± 6.6; from 88.5 ± 9.3 to 85.7 ± 7.8, p = 0.02; mean ∆ = – 2.4 ± 6.9) while no difference were seen for office DBP (Fig. 1B). Night-time ABPM values doesn’t showed any significant changes both for SBP and DBP as well as for dipping percentage and dipping pattern.
Finally, we analyze the acupuncture within session SBP decrease that was − 5.8 mmHg (– 3.75%) during the first session while it falls to – 2.1 mmHg (– 1.25%) and stands firmly under 2 mmHg for all the next session. At the last session SBP reduction was − 1.9 mmHg (– 1.6%), with a p values of 0.002 when first session reduction was compared to the other one.
No differences were seen in BP reduction between anti-hypertensive treated patients and those who were not (supplementary Table 1).
4 Discussion
The main results of our study is the finding of a significant reduction in office, 24 h and day-time ABPM SBP determined by a 6-weeks acupuncture cycle and which lasts at least for the first 2 months after its completion. On the opposite, DBP and night-time ABPM values seems not to be modified by acupuncture treatment.
Our results confirm the one published in previous studies and meta-analysis [2,3,4,5] while the absence of an effects on office DBP could be determined by the low number of subjects in our analysis.
How long the BP lowering effects of acupuncture last is an issue that need to be discussed. In fact, our study found that the effects lasts at least for two months but we doesn’t assess it for a longer period. Other study and metanalysisinvestigates this point founding that after 3 [17] or 6 months from acupuncture cycle completion no significant effects on BP are still presents [18].
Similarly to anti-hypertensive drugs that need to be chronically and daily assumed to maintain BP reduction effects, it is likely that also acupuncture need to be periodically performed to maintain its effects. So, evaluating how long the effects last and if its repetition still determine a significant reduction in BP could be something really interesting in order to determine how often the cycle need to be repeated. However, to the best of our knowledge no studies on this point have been already performed.
Nevertheless, our data are able to give others important information on this point. Analyzing within session reduction we found that the first one determines a stronger BP reduction when compared to all the other one. It is also true that within session BP reduction are clearly less than what is observed on the long term (– 2 mmHg for within session mean office SBP while its reduction at T1 is – 9 mmHg) so probably acute effects is not directly related to medium and long-term efficacy of acupuncture.
Regarding this latter point, several studies have been published focused in understanding the possible mechanisms through which acupuncture could act on BP values. Different mechanisms are implicated starting from local reaction, i.e.when the needle penetrates the skin leads to impulse resulting in local vasodilatation and release of vascular and neuroactive mediators (principally nitric oxide) [19]. Furthermore, it could act regulating sympathetic nervous which increased activity is a well-known pathological evidence in hypertensive subjects [20]. Acupuncture act at the hypothalamic level regulating the expression of neuronal nitric oxide synthase [10, 21,22,23]. Finally, it could activate the endogenous opioid system. Finally, acupuncture could act also reducing anxiety. In fact, there is increasing evidence of a positive association between anxiety and hypertension determined again by the activation of sympathetic nervous system and its negative effects. [24]. However, acupuncture is a well-established therapy for anxiety disorders [25] and, as already mentioned, act on sympathetic hyperactivation. So, it is possible that also action on anxiety are able to determine a further decrease of BP values.
The fact that in our study it principally act on office BP (as also founded by other studies [9]) and day ABPM could lead us to say that probably action on sympathetic nervous system prevail. In fact, during the day and, even more, during the office BP measurements, hyperactivation of sympathetic nervous system were reported [15].
However, this must be taken as a working hypothesis. Although some preclinical evidences have been published in favour of this hypothesis [26, 27] some data on a few number of healthy subjects seem not to found changes in skin [28] and muscle [29] sympathetic nerve activity.
Furthermore, also in our study HR, another marker of autonomic function, doesn’t showed any significant changes. Even more, a study evaluating BP variability (another marker of autonomic hyperactivation) found it to be unchanged after acupuncture [30] while studies on HR variability showed heterogeneous results [31, 32].
Another point of our study deserved to be mentioned, i.e. the presence of a positive effects also in already drug treated hypertensive patients. These point have been previously confirmed in other studies and meta-analysis [33]. Furthermore, its positive effects have been confirmed over the different anti-hypertensive drug classes [34] and also to be more effective in treated than in untreated patients [5]. This data could leads to the possibility to use acupuncture in patients that are near to reach the target BP, at least in those who experienced adverse effects with the addition of furthers drugs.
Our study presents some limitations. The main one is the low number of subjects: this sample size can limit our power to detect important associations or findings (such as the reduction in office DBP). Furthermore, a longer study follow-up time could help us defining the lasting effects of acupuncture. The third limitation of our study is the fact that the majority of subjects were females (61.8%). This could limit the results of our study in term of generalizability also in males subjects. Although there are not gender specific analysis previously reported (also in meta-analysis paper [34]), results of a significant reduction in BP values were reported both in studies with a majority of females subjects but also in studies where males were the majority.
Finally, no extensive evaluation of sympathetic activity have been done.
In conclusion, we found a significant reduction in office, 24 h and day-time ABPM SBP determined by a 6-weeks twice weekly acupuncture cycle that lasts at least for the first two months after its completion. Studies with longer follow-up and with a more extensive evaluation of sympathetic activity are needed in order to understand how long the effects of acupuncture last and if sympathetic overdrive amelioration is effectively the principal determinants of its effects.
References
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
Yang J, Chen J, Yang M, Yu S, Ying L, Liu GJ, Ren YL, Wright JM, Liang FR. Acupuncture for hypertension. Cochrane Database Syst Rev. 2018;14(11):CD008821.
Chen H, Shen FE, Tan XD, Jiang WB, Gu YH. Efficacy and safety of acupuncture for essential hypertension: a meta-analysis. Med Sci Monit. 2018;8:2946–69.
Zheng H, Li J, Li Y, Zhao L, Wu X, Chen J, Li X, Huang YL, Chang XR, Liu M, Cui J, Wang RH, Du X, Shi J, Guo TP, Liang FR. Acupuncture for patients with mild hypertension: a randomized controlled trial. J Clin Hypertens (Greenwich). 2019;21(3):412–20.
Li DZ, Zhou Y, Yang YN, Ma YT, Li XM, Yu J, Zhao Y, Zhai H, Lao L. Acupuncture for essential hypertension: a meta-analysis of randomized sham-controlled clinical trials. Evid Based Complement Alternat Med. 2014;2014:279478.
Li J, Zheng H, Zhao L, Li Y, Zhang Y, Chang XR, Wang RH, Shi J, Cui J, Huang YL, Li X, Chen J, Li DH, Liang FR. Acupuncture for patients with mild hypertension: study protocol of an open-label multicenter randomized controlled trial. Trials. 2013;14:380.
Li YM. Efficacy on borderline hypertension treated with acupuncture combined with anti-hypertensive plaster intervention. Zhongguo Zhen Jiu. 2014;34(11):1057–60.
Li H-J, Shen P-F, Gao H, Liu J-L. Effect of acupuncture on blood pressure variability in elderly patients with cerebral infarction complicated with essential hypertension. Zhongguo Zhen Jiu. 2019;39(7):685–8.
Yang D-H. Effect of electroacupuncture on Quchi (LI 11) and Taichong (LR 3) on blood pressure variability in young patients with hypertension. Zhongguo Zhen Jiu. 2010;30(7):547–50 Chinese.
Lee CH, Jung HS, Lee TY, Lee SR, Yuk SW, Lee KG, Lee BH. Studies of the central neural pathways to the stomach and Zusanli (ST36). Am J Chin Med. 2001;29(2):211–20.
Kim DD, Pica AM, Durán RG, Durán WN. Acupuncture reduces experimental renovascular hypertension through mechanisms involving nitric oxide synthases. Microcirculation. 2006;13(7):577–85.
Litscher G, Cheng WP, Cheng GY, Wang L, Zhao J, Litscher D, Gaischek I, Sheng Z, Kuang H. Acupuncture point laterality: investigation of acute effects of Quchi (LI11) in patients with hypertension using heart rate variability. Evid Based Complement Alternat Med. 2014;2014:979067.
Li J, Sun M, Ye J, Li Y, Jin R, Zheng H, Liang F. The mechanism of acupuncture in treating essential hypertension: a narrative review. Int J Hypertens. 2019;7:8676490.
Franssen PM, Imholz BP. Evaluation of the Mobil-O-Graph new generation ABPM device using the ESH criteria. Blood Press Monit. 2010;15(4):229–31.
Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977;55:613–8.
Lang RM. Badano LP, Mor-Avi V. Afilalo J, Armstrong A. Ernande L et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–70.
Flachskampf FA, Gallasch J, Gefeller O, Gan J, Mao J, Pfahlberg AB, Wortmann A, Klinghammer L, Pflederer W, Daniel WG. Randomized trial of acupuncture to lower blood pressure. Circulation. 2007;115(24):3121–9.
Yang J, Chen J, Yang M, Yu S, Ying L, Liu GJ, Ren YL, Wright JM, Liang FR. Acupuncture for hypertension. Cochrane Database Syst Rev. 2018;11(11):CD008821.
Chmielnicki B. Evidence based acupunture. Signal transmission.
Dell’Oro R, Quarti-Trevano F, Seravalle G, Zanchettin F, Bertoli S, Airoldi F, Mancia G, Grassi G. Sympathetic nerve traffic and arterial baroreflex function in apparent drug-resistant hypertension. Hypertension. 2019;74(4):903–9. https://doi.org/10.1161/HYPERTENSIONAHA.119.13009.
Li QQ, Shi GX, Xu Q, Wang J, Liu CZ, Wang LP. Acupuncture effect and central autonomic regulation. Evid Based Complement AlternMed. 2013; p. 267959.
Hsiao SH, Tsai LJ. A neurovascular transmission model for acupuncture-induced nitric oxide. J Acupunct Meridian Stud. 2008;1(1):42–50.
Li Q-Q, Shi G-X, Xu Q, Wang J, Liu C-Z, Wang L-P. Acupuncture effect and central autonomic regulation. Evid-Based Complement Altern Med. 2013. p. 267959.
Johnson HM. Anxiety and hypertension: is there a link? A literature review of the comorbidity relationship between anxiety and hypertension. Curr Hypertens Rep. 2019;18(9):66.
Amorim D, Amado J, Brito I, Fiuza SM, Amorim N, Costeira C, Machado J. Acupuncture and electroacupuncture for anxiety disorders: a systematic review of the clinical research. Complement Ther Clin Pract. 2018 May;31:31–7.
Yang JW, Ye Y, Wang XR, Li F, Xiao LY, Shi GX, Liu CZ. Acupuncture attenuates renal sympathetic activity and blood pressure via beta-adrenergic receptors in spontaneously hypertensive rats. Neural Plast. 2017; p. 8696402.
Paterno JC, Bergamaschi CT, Campos RR, Higa EM, Soares MF, Schor N, Freire AO, Teixeira VP. Electroacupuncture and moxibustion decrease renal sympathetic nerve activity and retard progression of renal disease in rats. Kidney Blood Press Res. 2012;35(5):355–64.
Toma K, Walkowski S, Metzler-Wilson K, Wilson TE. Acupuncture attenuates exercise-induced increases in skin sympathetic nerve activity. AutonNeurosci. 2011;162(1–2):84–8.
Kimura K, Ishida K, Takahashi N, Toge Y, Tajima F. Effects of acupuncture at the ST-36 point on muscle sympathetic nerve activity and blood pressure in normal adults. AutonNeurosci. 2017;208:131–6.
Zheng H, Li J, Li Y, Zhao L, Wu X, Chen J, Li X, Huang YL, Chang XR, Liu M, Cui J, Wang RH, Du X, Shi J, Guo TP, Liang FR. Acupuncture for patients with mild hypertension: a randomized controlled trial. J ClinHypertens (Greenwich). 2019;21(3):412–20.
Kimura K, Kitagawa Y, Tajima F. Effects of a single session of acupuncture treatment on blood pressure and heart rate variability in patients with mild hypertension. J Altern Complement Med. 2021;27(4):342–8.
Chang S, Chao WL, Chiang MJ, Li SJ, Lu YT, Ma CM, Cheng HY, Hsieh SH. Effects of acupuncture at Neiguan (PC 6) of the pericardial meridian on blood pressure and heart rate variability. Chin J Physiol. 2008;51(3):167–77.
Lee H, Kim SY, Park J, Kim YJ, Lee H, Park HJ. Acupuncture for lowering blood pressure: systematic review and meta-analysis. Am J Hypertens. 2009;22(1):122–8.
Chen H, Shen FE, Tan XD, Jiang WB, Gu YH. Efficacy and safety of acupuncture for essential hypertension: a meta-analysis. Med Sci Monit. 2018;24:2946–69.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi di Milano - Bicocca within the CRUI-CARE Agreement. This work was funded by the A. De Gasperis Cardiology and Cardiac Surgery Foundation.
Conflict of interest
The Authors declares that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Migliarese, C., Maloberti, A., Gatto, R. et al. Acupuncture in Arterial Hypertension: Evaluation of its Efficacy with Both Office and Ambulatory Blood Pressure Measurements. High Blood Press Cardiovasc Prev 29, 429–434 (2022). https://doi.org/10.1007/s40292-022-00530-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00530-9