Abstract
The approach to hypertensive emergiencies (HE) and urgencies (HU) may be different according to local clinical practice, despite recent guidelines and position papers recommendations. The Italian Society of Hypertension (Società Italiana della Ipertensione Arteriosa, SIIA) developed an online survey, in order to explore the awareness, management and treatment of HU in Italy, sending by e mail a 12 items questionnaire to the members of the SIIA. The results show that the definition of HU was correctly identified by 62% of the responders. Most physicians identified the role of pharmacological therapy or legal/illegal substances abuse as possible cause of BP elevation; the use of a benzodiazepine drugs was considered worthwhile by 65% of responders. The prescription of diagnostic test and drug administration significantly differed from guidelines recommendations and only 57% of the physicians reported to treat HU with oral drug administration. Sub-lingual nifedipine was prescribed by 13% or responders. This survey shows the need to further spread the updated scientific information on the management and treatment of HE and HU, along with the improvement of the interrelationship with the general practitioner health system in Italy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In most recent years the diagnostic approach and the treatment of hypertension have gained interest by patients and physicians. Acute elevations in blood pressure (BP), usually defined as ≥ 180/110 mmHg, may present with highly heterogeneous profiles ranging from absence of symptoms to life-threatening target organ damage [1,2,3]. The rate of hospitalization has significantly increased in the last 10 years while the related mortality has declined in USA [4], while few epidemiological data have been collected in Europe [5,6,7,8,9].
Increased BP (above 140/90 mmHg) was found in more than 30% of patients admitted to the Emergency Departments (EDs) [10]. The association of an acute and severe rise in blood pressure with an acute end-organ damage, influences patients’ prognosis and is usually defined as hypertensive emergency (HE). However, the same amount of BP increase may be observed in the absence of acute end-organ injury in a larger number of patients/subjects and has been recently renamed by the term hypertensive urgency (HU) or uncontrolled hypertension [3, 11]. Because of pain and/or anxiety frequently present in patients admitted to the ED, elevated BP levels are commonly observed, although the value of increased BP measurements is usually not adequately taken into account and the influence of different stressors is overlooked [12]. Oras et al have recently shown that raised BP in the ED is significantly associated with increases in incident ASCVD, MI, or stroke in the long-term [13], reinforcing the paramount importance of a correct recognition and therapeutic approach in these different groups of clinical conditions.
The American Heart Association statement has given some recommendations, guiding the appropriate management of acutely elevated BP [1], the 2018 European Society of Hypertension/European Society of Cardiology Guidelines [2] and a focused statement of the European Society of Cardiology [3] gave appropriate attention to hypertensive emergencies and urgencies.
The GEAR (Gestione delle Emergenze e urgenze in ARea critica) project [14] reported the results of a questionnaire, prepared by the group of Young Investigators of the Italian Society of Hypertension (SIIA) aimed to evaluate the awareness, diagnosis and treatment of hypertensive emergencies and urgencies in Italy. Overall the results have underscored the incomplete knowledge, some wrong beliefs and behaviors in the treatment of hypertensive urgencies, including the use of intravenous administration of drugs and an excessive use of sublingual (s.l.) nifedipine [15].
We therefore considered worthwhile to administer another questionnaire to physicians members of the SIIA, after having conducted educational initiatives in national and local meetings, aimed to improve both the management of hypertensive emergencies and urgencies and the interrelationship with the general practitioner health system.
2 Methods
SIIA developed a survey on HU and HE called UrgeRe (Urgenze ipertensive: un Progetto educazionale fondato sulla vita Reale, Hypertensive urgencies: a project in the Real world). This survey was administered between June 10th 2020 and September 20th 2020 through a web platform to the members of the SIIA. The invitation to join the survey was sent by an email describing the purpose with a direct link to the questionnaire. The participation was voluntary and confidential and each responder could withdraw at any point. The questionnaire consisted of 12 different items regarding diagnosis, management, treatment of HU and HE, methodology for BP measurements, eventual patients’ admission and follow-up after discharge; some were multiple choice questions, while others required only one answer (supplemental material). The survey was developed according to the 2018 ESH/ESC hypertension guidelines [2].
2.1 Statistical Analysis
We reported continuous variables as mean ± SD. Categorical variables, were expressed as frequencies and percentages. The chi-square distribution was used to compare categorical variables. Differences between continuous variables were calculated by Student’s t-test. Data were analyzed using excel system, and Statistical Package for the Social Sciences version 25 (SPSS Inc., Chicago, IL). A two-tailed p-value < 0.05 was considered statistically significant in all analyses.
3 Results
We collected 245 questionnaires: 53% from Internal Medicine Departments, 12% from Cardiology Departments 9% from EDs and from Emergency and Urgency Medicines, 24% from other departments and 1% from Intensive Care or Stroke Units.
Among participants (18–35 years 29.4%, 35–55 years 30.3%, 55–65 years 30.2% and > 65 years 10.2%; 64% males) 73% were physicians with different specialties, 20% were residents, 7% were general practitioners or private practice doctors.
The definition of HU, according to ESH/ESC 2018 guidelines [2] was correctly identified by 62 % of the responders (Fig. 1). Most physicians (84%) declared a low estimated annual rate of HU (between 0 and 25%) among all patients followed by each of them.
Physicians reported to repeat at least 2 office BP measurements (35%) or more than 2 BP measurements (22%) while few adopt unattended office BP measurements (10%) and none accepted to rely on a single measurement. The prescription of benzodiazepines was considered a reasonable therapeutic choice by 65% of participants.
When participants were asked about BP cuffs availability, most of the responders (94%) used of standard cuffs (24–32 cm), while large (32–42 cm) or extra-large (> 42 cm) cuffs were less frequently available (70% and 63% respectively). BP measurement was performed in both arms by 34% of participants.
The role of pharmacological therapy or legal/illegal substances abuse as possible cause of BP elevation was investigated: (87% of participants identified illegal substances abuse, steroids, vasoconstrictor agents or steroidal anti-inflammatory drugs as the most frequent causes, while 112 responders suggested that antineoplastic drugs could induce an acute BP elevation. One-hundred fifty-four responders identified all 4 causes (abuse substances, steroids, vasoconstrictor agents and non-steroidal anti-inflammatory drugs) as most frequent drugs responsible for an acute BP elevation (Table 1).
The diagnostic tests most frequently prescribed to exclude an hypertensive emergency were: an electrocardiogram (77%), urine and blood samples for proteinuria and creatinine (58%), a fundus oculi examination (49%) blood samples for BNP and troponin evaluation (27%), echocardiography (18%), 24 h blood pressure monitoring (18%), brain CT scan (17%), chest X-ray (15% or chest ultrasound (4.5%). No laboratory or instrumental tests were suggested by 14% of responders to differentiate a HE from an HU.
Only 57% of the physicians reported to treat HU with oral drug administration, although in 30% of the cases the use of intravenous (i.v.) administration was indicated; intramuscular (i.m.) and s.l administration was preferred in 2% and 11% of the cases. The use of a benzodiazepine drugs was considered worthwhile by 65 % of responders (Fig. 2b).
When the treatment of an HU occurring at patients’ home was investigated, the drug most frequent prescribed was a calcium channel blocker, given by oral administration (59%), followed by the increase of daily therapy regimen dosages (49%) or the association of another drug (45%). The use of an oral administration of an ACE-inhibitor, of an angiotensin 2 receptor antagonist or of oral furosemide was suggested by 40%, 22% and 30% of physicians, respectively. Thirty-two physicians suggested the administration of s.l. nifedipine (13%) and 21 (9%) would have sent the patient directly to the ED.
For patients with an HU admitted to the ED or seen in the hospital, the use of intravenous or oral therapy was selected by 37% and 40% of responders, respectively, while 49 physicians would have used both oral and intravenous drug administration. Among intravenous administered drugs, furosemide (n = 94), and/or nitroglycerin (n = 89) and/or labetalol/urapidil (n = 99) were chosen by in 35 % of physicians. The oral administration of a calcium channel blocker was the preferred choice by 48% of responders (n = 118), followed by the use of an oral administration of an ACE-inhibitor, of an angiotensin 2 receptor antagonist or of oral furosemide; 36 physicians would have used a fixed combination. Twenty-seven (11%) physicians would have used s.l. nifedipine and 57 would have used a pain-killer drug in the presence of any painful clinical condition (Table 2).
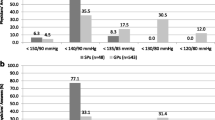
When the target BP to be reached and the time needed to decrease BP were explored, 52% of physicians suggested a target BP < 140/90 mmHg in 24–48 h, while 21% suggested a reduction below 160/100 mmHg in 30 min, 15% considered a target of 140/90 mmHg in 60 min and 29 (12%) of participants selected to consider a target below 160/100 mmHg in 48 h (Fig. 2a).
Among the management options after the occurrence of an HU, 109 physicians asked for a 24 h BP monitoring, while 104 physicians suggested a short term (2–3 days) follow-up visit and 92 considered a hypertension specialist consultation. An increase in the dosage of patients’ drug therapy or a general practitioner re-evaluation were less frequently recommended.
After the occurrence of an HU, several options were given, including a 24 h BP monitoring, suggested by 109 physicians, 104 responders suggested a short term (2–3 days) follow-up visit and 92 considered a hypertension specialist consultation (with short term visit in 22 cases). An increase in the dosage of patients’ drug therapy or a general practitioner re-evaluation were less frequently recommended.
Some differences in the definition of HU were observed, being GPs the group with the lowest percentage (33%) of correct identification of clinical characteristics associated with a HU. We did not observe any significant difference in most of laboratory and instrumental examinations and in the therapeutic approach for BP reduction. The prescription of 24 h ABPM was less frequently prescribed by emergency physicians (7%) than other specialists (45 to 50%), despite the difference did not reach statistical significance.
4 Discussion
The UrgeRe survey was directed to physicians members of the SIIA, more deeply involved in the management of hypertensive patients, in order to investigate the clinical approach to HU and HE in daily clinical practice. This survey represents an update of previous data collected in the framework of the GEAR project [14], which included healthcare providers working mainly in the ED and intensive care units throughout Italy. A slightly lower proportion of residents participated to the UrgeRE survey as compared to the GEAR one (20% vs 27%, respectively); this suggests an older age of responders to the UrgeRE questionnaire, although data on GEAR participants’ age is not currently available.
Altogether, a substantial proportion (80%) of the sample was able to correctly identify an HU, while about 90% of the interviewed gave a correct definition for HE. This result may be influenced by the publication of the recent ESH/ESC guidelines [2] and by the position paper by the ESC Council on hypertension [3]. In this document it is suggested to abandon the term “HU”, since there is no clear evidence that treatment in patients who lack acute clinical evidence of hypertension-mediated organ damage should be different from that usually proposed to patients with asymptomatic uncontrolled hypertension [3], and consider the presence of an uncontrolled hypertension. The results of the previous GEAR survey, conducted before the release of the ESC Position Paper, found superimposable results, underscoring the need of a more precise definition and management of HU.
Most of the participants recognized the use of drugs including steroids, vasoconstrictor agents and NAIDS or toxic substances (cocaine/meth) as related to acute BP increase [1,2,3], while a slightly lower portion of physicians indicated anticancer drugs as possible cause of an HU [16, 17]. Therefore, the awareness of drug-induced hypertension is high among hypertension specialists, leading them to ask about any drug /substance use to properly identify possible causes of acute BP rise.
In addition, anxiety or acute pain were recognized as possible conditions contributing to the acute rise of BP and about a half of participants agreed on the use of an anti-anxiety drug such a benzodiazepine. Moreover, in the presence of acute pain, at least 24% of physicians would prescribe a pain killer drug. It is well known that patients with HU/HE, even when managed at home, are exposed to a stressful condition, which could itself raise BP levels [12]. In a small number of patients admitted to the ED and presenting with an HU, it has been shown that oral diazepam was associated to a SBP decrease SBP of more than 40 mmHg 3 h after administration [18]. Therefore, treatment with benzodiazepine may reduce the anxiety related to the clinical condition and associated adverse consequences.
As far as treatment options were investigated, only two thirds of participants correctly preferred oral BP lowering drugs for HU while were keen to use intravenous drugs in 30% of cases, confirming the lack of an homogeneous approach to the treatment of HU [19]. This was further shown when several drugs options were proposed, including both oral and i.v. administration; again, an oral calcium channel blocker was proposed by only 59 and 48% % of participants for the treatment of an HU at home or in the ED/hospital, respectively. Other reasonable options, such as the increase of the dosage of current antihypertensive treatment or the combination with another drug were also suggested by nearly half of participants.
The rate of physicians choosing the use of sub-lingual nifedipine for the control of BP in an HU was unacceptably high, and against the recommendations of guidelines [1, 2, 20] or expert consensus documents [3, 21]. Sub-lingual nifedipine, as well as the inappropriate prescription of i.v. drugs for HU might induce a reduction in BP levels which is too fast and possibly dangerous because of the risk of cerebral hypoperfusion [21]. Almost 25 % of responders considered appropriate the administration of clonidine in HU, despite its use by i.v. route has been suggested for the treatment hypertensive emergencies only, with caution on side effects such as sedation and rebound hypertension [3].
Other 2 important items investigated BP measurements, including the available equipment and the number of BP measurements. Concerning BP measurement technique, only two-thirds of the responders had universal or large/extra-large cuffs. It is well known that the use of a cuff with a bladder too narrow or too short for the arm circumference, may lead to an overestimation of BP levels, with inappropriate diagnosis or overtreatment of the patients; the opposite is true when a too large or to long bladder are used. Several guidelines and consensus documents, including the one released by the Italian Society of Hypertension, have highlighted the importance of a correct size of cuffs and bladders [1, 2, 22, 23]. Therefore, a wider use of different cuffs was expected being participants all members of the Italian society of Hypertension, while in the GEAR survey participants were mostly physicians working in EDs [13].
Participants suggested the use of several measurements of BP, in 25 % of cases on both arms. It is encouraging that none declared to rely on a single BP detection, since it could lead to overestimation of risk and that a small proportion of interviewed physicians have adopted the unattended BP measurement, especially if the patient is clearly alarmed.
Among the diagnostic tests, a detectable proportion of participants indicated fundus oculi examination as an important clue for the diagnosis of an HE, as malignant hypertension or hypertensive encephalopathy [24]; nowadays the lack of fundoscopy perfomed by an ophtalmologist may be overcome by the use of smartphone-based devices for ocular fundus photography, proven to be feasible and reliable in the ED [25]. Creatinine and urine dipstick were performed frequently prescribed, representing “standard tests” for all hypertensive patients, according to guidelines [1, 2]. Few participants indicated the use of lung ultrasound, possibly related to the higher sensitivity in the diagnosis of lung congestion [26].
Recent evidences suggest that the adequate approach to patients with HU is based on a strict outpatient-clinic visits. A retrospective cohort study including patients with HU showed that both patients sent home and those sent to the ED had the same, very low, incidence of major adverse cardiovascular events at 30 days [27]. Other more recent data have shown that even one single measurement of elevated BP taken in the ED, in the absence of acute organ damage, may predict an unfavorable event free survival during the following 10 years [12]. Very few data are currently available in order to differentiate the long-term clinical outcome of patients with HE or with HU or with uncontrolled hypertension. [27, 28].
The importance of the follow-up of patients with a HU, even after discharge by ED or hospital, is confirmed by the high proportion of physicians (71%) suggesting either a Hypertension Center visit or a short term outpatient visit or both. In a recent study, early follow-up after leaving ED with a diagnosis of hypertension, was associated with an improvement of long-term outcome [29] and the assessment by an hypertension specialist may represent the proper follow-up for these patients [12, 30, 31].. Hypertension reference centers are widely distributed in Italy, with a regular activity 3 to 5 days/week, and easy contacts in order to improve clinic schedule appointments (https://siia.it/centri-e-ambulatori/) [30]. In all Excellence Centers and in most Hypertension Outpatients Clinics endorsed by the Italian Society of Hypertension, an ABPM, prescribed by 44% of participants to the survey may be performed, during all the weekdays. This result differs from the GEAR survey, in which very few ED physicians prescribed ABPM, despite its crucial role in confirming the diagnosis of hypertension or BP control under treatment [13, 30]. It would be therefore desirable to update protocols for improving access to an outpatient hypertension center after an HU.
4.1 Limitations
First of all, this is a descriptive analysis, being based on a survey, and we cannot extrapolate any causative relationship of the results. Data based on physician self-reporting, in the absence of more objective measures or quantifications, may have potential biases, although it may truly reflect the practice of HU management in Italy, being the questionnaire answer anonymous. In addition, the answers given to the questionnaire may not represent the opinion of a larger number of physicians members of the SIIA. No data related to the management of acute BP increase in pregnant women were collected, being pregnant women usually managed by gynecologists. Finally, the response rate (40%), despite a good distribution of the Italian country, was lower than expected.
5 Conclusion
In conclusion, this survey adds new information about the management of HU in Italy. The survey was directed to members of the SIIA, in order to evaluate the effect of new scientific statements and of some educational initiatives conducted in national and local meetings, aimed to improve the management of HE and HU. The results show the need to further spread the updated scientific information on the management and treatment of HE and HU, even among members of the SIIA, along with the improvement of the interrelationship with the general practitioner health system.
References
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–324.
Williams B, Mancia G, Spiering W, et al. Authors/Task Force Members: 2018 ESC/ESH guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041.
van den Born BH, Lip GYH, Brguljan-Hitij J, et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur Heart J Cardiovasc Pharmacother. 2019;5(1):37–46.
Janke AT, Mcnaughton CD, Brody AM, Welch RD, Levy PD. Trends in the incidence of hypertensive emergencies in US Emergency Departments From 2006 to 2013. J Am Heart Assoc. 2016;5(12):e004511.
Paini A, Aggiusti C, Bertacchini F, et al. Definitions and epidemiological aspects of hypertensive urgencies and emergencies. High Blood Press Cardiovasc Prev. 2018;25:241–4.
Lip GY, Beevers M, Beevers G. The failure of malignant hypertension to decline: a survey of 24 years’ experience in a multiracial population in England. J Hypertens. 1994;12:1297–305.
Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension. 1996;27:144–7.
Pinna G, Pascale C, Fornengo P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PLoS ONE. 2014;9:1–6.
Salvetti M, Paini A, Colonetti E, et al. Hypertensive emergencies and urgencies: a single-centre experience in Northern Italy 2008–2015. J Hypertens. 2020;38(1):52–8.
Skoglund PH, Svensson P. Asking the patient or measuring blood pressure in the emergency department: which one is best? Curr Hypertens Rep. 2016;18:53. https://doi.org/10.1007/s11906-016-0659-0.
Mancusi C, Losi MA, Albano G, et al. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting: the campania salute network. Am J Hypertens. 2020;33:414–21.
Saguner AM, Dür S, Perrig M, et al. Risk factors promoting hypertensive crises: evidence from a longitudinal study. Am J Hypertens. 2010;23(7):775–80.
Oras P, Häbel H, Skoglund PH, Svensson P. Elevated blood pressure in the emergency department: a risk factor for incident cardiovascular disease. Hypertension. 2020;75:229–36. https://doi.org/10.1161/HYPERTENSIONAHA.119.14002).
Saladini F, Mancusi C, Bertacchini F, et al. Diagnosis and treatment of hypertensive emergencies and urgencies among Italian emergency and intensive care departments. Results from an Italian survey: Progetto GEAR (Gestione dell’Emergenza e urgenza in ARea critica). Eur J Intern Med. 2020;71:50–6.
Grossman E, Messerli FH, Grodzicki T, Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996;276:1328–31.
Small HY, Montezano AC, Rios FJ, Savoia C. Touyz RM Hypertension due to antiangiogenic cancer therapy with vascular endothelial growth factor inhibitors: understanding and managing a new syndrome. Can J Cardiol. 2014;30(5):534–43.
Rizzoni D, De Ciuceis C, Porteri E, Agabiti-Rosei C, Agabiti-Rosei E. Use of antihypertensive drugs in neoplastic patients. High Blood Press Cardiovasc Prev. 2017;24(2):127–32.
Grossman E, Nadler M, Sharabi Y, et al. Antianxiety treatment in patients with excessive hypertension. Am J Hypertens. 2005;18(9 Pt 1):1174–7.
Maloberti A, Cassano G, Capsoni N, et al. Therapeutic approach to hypertension urgencies and emergencies in the emergency room. High Blood Press Cardiovasc Prev. 2018;25(2):177–89.
Chobanian AV, Bakris GL, Black HR, et al. Joint national committee on prevention, detection, valuation, and treatment of high blood pressure. National heart, lung, and blood institute; national high blood pressure education program coordinating committee. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–52.
Burton TJ, Wilkinson IB. The dangers of immediate-release nifedipine in the emergency treatment of hypertension. J Hum Hypertens. 2008;22:301–2.
Palatini P, Asmar R, O’Brien E, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring, Cardiovascular Variability, the International Standardisation Organisation (ISO) Cuff Working Group. Recommendations for blood pressure measurement in large arms in research and clinical practice: position paper of the European society of hypertension working group on blood pressure monitoring and cardiovascular variability. J Hypertens. 2020;38(7):1244–50.
Parati G, Omboni S, Palatini P, et al. Italian society of hypertension guidelines for conventional and automated blood pressure measurement in the office, at home and over 24 hours. High Blood Press Cardiovasc Prev. 2008;15(4):283–310.
Rubin S, Cremer A, Boulestreau R, et al. Malignant hypertension: diagnosis, treatment and prognosis with experience from the Bordeaux cohort. J Hypertens. 2019;37(2):316–24.
Muiesan ML, Salvetti M, Paini A, et al. Ocular fundus photography with a smartphone device in acute hypertension. J Hypertens. 2017;35(8):1660–5.
Leidi F, Casella F, Cogliati C. Bedside lung ultrasound in the evaluation of acute decompensated heart failure. Intern Emerg Med. 2016;11(4):597–601.
Patel KK, Young L, Howell EH, et al. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med. 2016;176(7):981–8.
Koracevic G, Lovic D, Zdravkovic M, Stojanovic M, Djordjevic D. How should we treat very high blood pressure until we distinguish between hypertensive emergency and urgency? Hypertens Res. 2020;43:470–2.
Atzema CL, Yu B, Schull MJ, et al. Physician follow-up and long-term use of evidence-based medication for patients with hypertension who were discharged from an emergency department: a prospective cohort study. CMAJ Open. 2018;6(2):E151–61.
Vinker S, Kitai E, Or Y, Nakar S. Primary care follow up of patients discharged from the emergency department: a retrospective study. BMC Fam Pract. 2004;5:16.
Tocci G, Palano F, Battistoni A, et al. Clinical management of patients with hypertension and high cardiovascular risk in specialised centers and in general practice. Analysis from an Italian Survey Questionnaire. Nutr Metab Cardiovasc Dis. 2015;25(9):866–74.
Acknowledgements
The UrgeRe project was conducted with an educational contribution by Sanofi s.r.l.
Funding
Open Access funding provided by Università degli Studi di Brescia.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interests
Nothing to declare.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Muiesan, M.L., Rosei, E.A., Borghi, C. et al. The UrgeRe (Urgenze Ipertensive: Un Progetto Educazionale Fondato Sulla Vita Reale, Hypertensive Urgencies: A Project in the Real World) Project. High Blood Press Cardiovasc Prev 28, 151–157 (2021). https://doi.org/10.1007/s40292-021-00433-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-021-00433-1