Abstract
Objective
Volume overload is typical of haemodialysis patients; correct volume status evaluation is crucial in achieving blood pressure homeostasis, hypertension management and good treatment planning. This study evaluates the effect of acute volume depletion on ultrasonographic parameters and suggests two of them as able to predict patients volume overload.
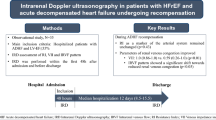
Patients and intervention
27 patients with end stage renal disease treated with haemodialysis underwent a complete echocardiographic exam before, after 90 min and at the end of the dialysis.
Main outcome and results
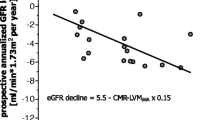
Blood pressure levels significantly drop during the first 90 min of dialysis (139 ± 20 vs 126 ± 18; p < 0.0001), reaching a steady state with significantly lower values compared to baseline (130 ± 28; p = 0.02). LV and left atrial volume significantly decreased (baseline vs end dialysis 98 ± 32 vs 82 ± 31 p = 0.003 and 28 ± 10 vs. 21 ± 9 cc/m2 p < 0.001). A significant reduction of systolic function (EF 61.6 % ± 9 vs 58.7 % ± 9 p = 0.04), of diastolic flow velocities (E/A 1.13 ± 0.37 vs. 0.87 ± 0.38 p < 0.001) and mitral annulus TDI tissue velocity (i.e. E′ lat 10.6 ± 3 vs. 9.4 ± 3 cm/s; p 0.0001) were observed. Stroke work (SW) and LV end-diastolic diameter (LVEDd) indexed to height 2.7(LVEDdi) were able to predict volume overload: cut off values of respectively 13.5 mm/m2.7 for LVEDdi and 173 cJ for SW were able to predict with a specificity of 100 % the presence of a volemic overload of at least 4 %.
Conclusions
Blood pressure, cardiac morphology and function are significantly modified by acute volume depletion and such variations are strictly interrelated. SW and LVEDd/height2.7 may identify ESRD patients carrying an higher volume load.


Similar content being viewed by others
References
Mailloux LU, Haley WE. Hypertension in the ESRD patient: pathophysiology, therapy, outcomes, and future directions. Am J Kidney Dis. 1998;32(5):705–19.
Agarwal R, Alborzi P, Satyan S, et al. Dry-weight reduction in hypertensive hemodialysis patients (DRIP): a randomized, controlled trial. Hypertension. 2009;53(3):500–7.
Davenport A. Intradialytic complications during hemodialysis. Hemodial Int. 2006;10(2):162–7.
Shoji T, Tsubakihara Y. Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int. 2004;66(3):1212–20.
Goldfarb-Rumyantzev AS, Chelamcharla M, Bray BE, et al. Volume indicators and left ventricular mass during aggressive volume management in patients on thrice-weekly hemodialysis. Nephron Clin Pract. 2009;113(4):c270–80.
Raimann J, Liu L, Tyagi S, et al. A fresh look at dry weight. Hemodial Int. 2008;12(4):395–405.
Barberato SH, Mantilla DE, Misocami MA, et al. Effect of preload reduction by hemodialysis on left atrial volume and echocardiographic Doppler parameters in patients with end-stage renal disease. Am J Cardiol. 2004;94(9):1208–10.
Palecek T, Skalicka L, Lachmanova J, et al. Effect of preload reduction by hemodialysis on conventional and novel echocardiographic parameters of left ventricular structure and function. Echocardiography. 2008;25(2):162–8.
Fijalkowski M, Koprowski A, Gruchala M, et al. Effect of preload reduction by hemodialysis on myocardial ultrasonic characterization, left atrial volume, and Doppler tissue imaging in patients with end-stage renal disease. J Am Soc Echocardiogr. 2006;19(11):1359–64.
Del Rosario ME, Dellsperger KC. The role of echocardiography in cardiac structural and functional assessment in dialysis patient. Adv Perit Dial. 2009;25:133–9.
Paneni F, Gregori M, Pignatelli G, et al. Pathophysiology of biventricular dysfunction during hemodialysis: emerging concepts. Int J Cardiol. 2012;155(3):478–9.
Pecoits-Filho R, Barberato SH. Echocardiography in chronic kidney disease: diagnostic and prognostic implications. Nephron Clin Pract. 2010;114(4):c242–7.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7(2):79–108.
Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57(6):450–8.
Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007;28(12):1462–536.
Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22(2):107–33.
Hung KC, Huang HL, Chu CM, et al. Evaluating preload dependence of a novel Doppler application in assessment of left ventricular diastolic function during hemodialysis. Am J Kidney Dis. 2004;43(6):1040–6.
Zoccali C. Left ventricular mass index as an outcome measure in clinical trials in dialysis patients: a word of caution. Am J Nephrol. 2011;33(4):370–2 Epub 2011 Mar 30.
Drighil A, Madias JE, Mathewson JW, et al. Haemodialysis: effects of acute decrease in preload on tissue Doppler imaging indices of systolic and diastolic function of the left and right ventricles. Eur J Echocardiogr. 2008;9(4):530–5.
Ie EH, Vletter WB, ten Cate FJ, et al. Preload dependence of new Doppler techniques limits their utility for left ventricular diastolic function assessment in hemodialysis patients. J Am Soc Nephrol. 2003;14(7):1858–62.
Agarwal R, Bouldin JM, Light RP, et al. Inferior vena cava diameter and left atrial diameter measure volume but not dry weight. Clin J Am Soc Nephrol. 2011;6(5):1066–72.
Palmer BF, Henrich WL. Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol. 2008;19(1):8–11.
Tislér A, Akócsi K, Borbás B, et al. The effect of frequent or occasional dialysis-associated hypotension on survival of patients on maintenance haemodialysis. Nephrol Dial Transpl. 2003;18(12):2601–5.
Agarwal R. Assessment of blood pressure in hemodialysis patients. Semin Dial. 2002;15(5):299–304.
Kumar A, Anel R, Bunnell E, et al. Preload-independent mechanisms contribute to increased stroke volume following large volume saline infusion in normal volunteers: a prospective interventional study. Crit Care. 2004;8(3):R128–36.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milan, A., Avenatti, E., Della Valle, E. et al. Non Invasive Evaluation of Cardiac Hemodynamics in End Stage Renal Disease (ESRD). High Blood Press Cardiovasc Prev 21, 261–268 (2014). https://doi.org/10.1007/s40292-014-0045-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-014-0045-4