Abstract
Until recently, only symptomatic therapies, in the form of acetylcholine esterase inhibitors and NMDA-receptor antagonists, have been available for the treatment of Alzheimer’s disease. However, advancements in our understanding of the amyloid cascade hypothesis have led to a development of disease-modifying therapeutic strategies. These include immunotherapies based on an infusion of monoclonal antibodies against amyloid-β, three of which have been approved for the treatment of Alzheimer’s disease in the USA (one of them, lecanemab, has also been approved in several other countries). They all lead to a dramatic reduction of amyloid plaques in the brain, whereas their clinical effects have been more limited. Moreover, they can all lead to side effects in the form of amyloid-related imaging abnormalities. Ongoing developments aim at facilitating their administration, further improving their effects and reducing the risk for amyloid-related imaging abnormalities. Moreover, a number of anti-tau immunotherapies are in clinical trials, but none has so far shown any robust effects on symptoms or pathology. Another line of development is represented by gene therapy. To date, only antisense oligonucleotides against amyloid precursor protein/amyloid-β and tau have reached the clinical trial stage but a variety of gene editing strategies, such as clustered regularly interspaced short palindromic repeats/Cas9-mediated non-homologous end joining, base editing, and prime editing, have all shown promise on preclinical disease models. In addition, a number of other pharmacological compounds targeting a multitude of biochemical processes, believed to be centrally involved in Alzheimer’s disease, are currently being evaluated in clinical trials. This article delves into current and future perspectives on the treatment of Alzheimer’s disease, with an emphasis on immunotherapeutic and gene therapeutic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Immunotherapies targeting amyloid-β, which can reduce amyloid plaque burden and slow down cognitive decline, are registered for use in several countries. |
Immunotherapies targeting tau are evaluated in clinical trials, but so far none has shown any clear effects. |
Gene therapies, including anti-sense oligonucleotides and gene editing strategies targeting amyloid precursor protein and tau, are in clinical trials and under preclinical development, respectively. |
1 Introduction
1.1 Demographics and Classical Treatments
Alzheimer’s disease (AD) is the most common neurodegenerative disorder, affecting 32 million people worldwide [1]. Age is the strongest risk factor for AD and, because of the increasing life expectancy, the numbers are likely to rise in the future. According to the World Health Organization 2021 global status report on the public health response to dementia, about 139 million affected individuals are expected worldwide by 2050 [2].
Until recently, only symptomatic therapies have been available for the treatment of cognitive symptoms in AD. Most of these are acetylcholine esterase inhibitors and act by increasing levels of acetylcholine in the brain. The cholinergic system has been implicated in the disease since the discovery of a progressive loss of limbic and neocortical cholinergic innervation in the AD brain (reviewed in [3]). The widespread presynaptic cholinergic denervation results in decreased acetylcholine and consequential deficits in memory, learning, and other essential aspects of cognition. The first such substance, tacrine, was approved in 1993 and was followed by three additional compounds of its class, donepezil, rivastigmine, and galantamine, in 1996, 1997, and 2001, respectively (reviewed in [4]).
Another therapeutic, memantine, was approved in Europe in 2002 and 1 year later in the USA. Memantine is an NMDA-receptor antagonist, which decreases the excitability of nerve cells that signal via excitatory amino acids to thereby reduce cell toxic effects (reviewed in [4]). In addition to these two groups of medications, aimed at temporarily ameliorating cognitive dysfunction, other symptomatic drugs are used to treat commonly related disease manifestations, such as depression and anxiety.
Classical drugs used in AD do not target the underlying molecular disease causes. However, over the last 25 years, there has been tremendous activity both in academia and industry to design disease-modifying treatments. In the following, we describe this development, focusing on recent and ongoing efforts to generate and evaluate such compounds. We also offer insights into potential advancements in pharmacological approaches, envisioning a future characterized by enhanced therapeutic efficiency and potentially even tailored strategies for personalized medicine.
1.2 The Amyloid Cascade Hypothesis
Already since 1907, when Alois Alzheimer published his report on the neuropathological evaluation of Auguste D [5], we have known that the disease that came to bear his name displays the presence of extra- and intra-cellular and intracellular deposits in the brain. With the advent of biomolecular laboratory tools, researchers could describe the composition of these characteristic plaques and tangles. Whereas it was found that plaques consist of the amyloid-β (Aβ) peptide [6], the main component of the intracellular tangles was identified as the tau protein [7]. As amyloid precursor protein (APP) and presenilin (PSEN1 and PSEN2) mutations, which increase the generation and aggregation of Aβ, were identified in familial early-onset forms of AD [8, 9] and as plaques also could be found in the brain of subjects with Down’s syndrome (who carry an extra copy of APP on chromosome 21) [6], Aβ was strongly implied in the pathogenesis (reviewed in [10]). Moreover, identification of the protective APP A673T mutation, which in an Icelandic population was found to be five times more common in healthy elderly individuals than in patients with AD, provides additional support for the central role of Aβ in AD [11].
The amyloid cascade hypothesis postulates that either an increase in the generation or a decrease in the degradation of Aβ is an early event in AD pathology that subsequently triggers hyperphosphorylation of tau and formation of neurofibrillary tangles. According to the hypothesis, additional downstream processes, such as synaptic loss and neuroinflammation, are believed to result from an Aβ-related toxic gain of function (reviewed in [12]).
The understanding of the role of Aβ in the pathogenesis has been essential for the development of therapies aimed at thwarting the initiation and progression of AD. Initially, there were expectations that inhibitors of the two enzymes, β-secretase and γ-secretase, which via subsequent cleavages generate Aβ from APP, could be developed into efficient therapies. Whereas inhibitors/modulators of both enzymes could lower Aβ production and shrink existing amyloid plaques in mouse models (reviewed in [13, 14]), the ensuing clinical trial outcomes were disappointing as they either failed to show efficacy or had to be terminated because of unacceptable side effects (reviewed in [13, 15]). As a possible explanation for their lack of efficacy, decreased Aβ production may not be able to change the clinical course once the disease process has advanced to a certain point. Instead, these compounds may be better suited for prevention. Nevertheless, a new generation of γ-secretase modulators are currently undergoing testing in clinical trials for AD (reviewed in [14]). As for β-secretase inhibitors, it has been speculated that the cognitive worsening seen in some of the trials could be avoided if lower doses are given over a longer period (reviewed in [13]). So far, the most promising strategy based on the amyloid cascade hypothesis has instead been to target Aβ with biologics, represented by active or passive immunotherapies.
2 Immunotherapies
2.1 Immunotherapies Targeting Aβ
In a pioneer study, Dale Schenk and colleagues were able to demonstrate that transgenic APP mice, which had been injected with intramuscular doses of fibrillar Aβ, displayed reduced plaque pathology together with less neuroinflammatory reactions, as compared with placebo-treated mice [16]. The outcome of this study, based on active immunization, spurred the development of a vaccine against AD. The Irish-American pharmaceutical company Elan designed a clinical trial based on the same approach as that of the mouse study. Unfortunately, it had to be halted after more than 5% of the treated participants with AD developed meningoencephalitis. However, a subgroup of patients who had received two doses and were classified as “responders” did demonstrate less decline on cognitive tests as compared with placebo-treated patients [17]. Moreover, post-mortem analyses of one trial participant suggested that anti-Aβ immunization could result in plaque clearance [18].
In order to lessen the risk of side effects, many academic groups and pharmaceutical companies instead turned their attention towards passive immunotherapy, i.e. treatment based on the administration of anti-Aβ monoclonal antibodies (mAbs). Such compounds are typically generated by applying the hybridoma method on laboratory mice. Once a murine mAb with desired properties has been generated, its protein sequence is humanized to increase its similarity to those antibodies that occur naturally in the body. Studies based on such anti-Aβ mAbs were initiated, but neither phase III trials with solanezumab [19] nor with crenezumab [20] showed any significant plaque clearance as assessed by amyloid positron emission tomography (PET). However, in the bapineuzumab phase III trial, a reduction in amyloid PET could be seen in APOEε4 carriers [21, 22]. A suboptimal target engagement for these compounds is the most likely explanation for their lack of effect. Moreover, in the earlier studies, a limited efficacy could most likely be partially explained by a lack of biomarker-based recruitment criteria that allowed also patients without proven Aβ brain pathology to be recruited into the studies.
Biogen was the first company to launch a passive immunotherapy trial, in which AD biomarkers were used for inclusion. Aducanumab binds to a conformational epitope close to the n-terminus of Aβ (amino acids 3–7). In a phase IIb trial, treatment with this antibody resulted in a dramatic decrease of the plaque load, as assessed by amyloid PET [23]. In two large ensuing phase III trials (EMERGE and ENGAGE), aducanumab continued to show robust effects against plaque deposition but both trials were stopped prematurely after futility analyses. However, upon post hoc analyses, it was found that EMERGE indeed had met its primary endpoint. Patients with high-dose treatment decreased 0.39 points less on the Clinical Dementia Rating-Sum of Boxes (CDR-SB) compared with those on placebo. As for side effects, 35.2% and 19.1% of patients at the 10 mg/kg dose developed perivascular edema and microhemorrhages, respectively (compared with 2.7% and 6.6% in the placebo group) [24]. The majority of these cases were asymptomatic and 98% of them resolved radiologically. The risk of such amyloid-related imaging abnormalities (ARIA-edema [ARIA-E] and ARIA-hemorrhages [ARIA-H]) is the reason that all patients undergoing immunotherapy with any anti-Aβ mAb need to be monitored with regular magnetic resonance imaging brain scans.
Despite ENGAGE failing to show any clinical benefits, the US Food and Drug Administration (FDA) issued a fast-track approval for the compound. The registration was conditional upon it showing success in yet another (phase IV) trial in order to gain full approval. However, it was recently announced that Biogen discontinued the development and commercialization of aducanumab as a measure to reprioritize their resources to bolster innovation of other assets in their pipeline [25].
The second anti-Aβ mAb to be assessed by the FDA, lecanemab, was given full approval in June 2023 after completion of the successful phase III CLARITY trial. Lecanemab was developed against the presumably toxic protofibrils, a large oligomeric species of Aβ that precedes the formation of fibrils. Similar to aducanumab, lecanemab was shown to have a robust effect on plaque removal and could also partially correct the downstream cerebrospinal fluid (CSF) biomarkers Aβ42, total tau, and phospho-tau [26]. On the primary clinical outcome, patients had 0.45 points less on the CDR-SB after 18 months of treatment compared with the placebo group. Much like aducanumab, ARIAs were the most significant side effects, with ARIA-E seen in 17.3% and ARIA-H in 12.6% of the patients (compared with 9.0% and 1.7% for those on placebo). Recent data presented at the Alzheimer’s Association International Conference (AAIC) 2024 show that 36 months of treatment with lecanemab delayed progression to the next disease stage (from mild cognitive impairment [MCI] to dementia or from mild AD to moderate AD) by 30% (hazard ratio 0.74) [27]. Additionally, when compared with the Alzheimer’s Disease Neuroimaging Initiative observational cohort, the differences between treated and non-treated patients continued to expand from 18 through 36 months. Furthermore, the delayed start group also showed benefit in the open-label extension cohort relative to the Alzheimer’s Disease Neuroimaging Initiative cohort [28]. Additionally, lecanemab was found to slow the accumulation of tau pathology in the medial temporal lobe compared with placebo, as assessed by tau PET [29].
A third immunotherapy targeting Aβ, donanemab, has recently also been given full approval by the FDA after having shown positive effects in the TRAILBLAZER-ALZ2 phase III trial [30]. Donanemab is raised against Aβ (p3-42), a pyroglutamate form of Aβ that is aggregated in amyloid plaques. Similar to aducanumab and lecanemab, plaques were efficiently removed and biomarkers were partially normalized. After 18 months of treatment, the group treated with the active compound differed by 0.63 on the CDR-SB compared with the placebo-treated group [30]. As with the other anti-Aβ mAbs, ARIAs occurred also with donanemab (ARIA-E 24.0% for treatment, 1.9% for placebo; ARIA-H 19.7% for treatment, 7.4% for placebo). As a unique feature with this trial, recruitment was based not only on a positive amyloid PET scan, but patients also had to be tau PET positive. Moreover, participants who demonstrated a certain degree of plaque reduction were switched to placebo, in keeping with the idea that treatment with donanemab, which targets aggregated Aβ, can be held when a certain effect has been achieved and reinitiated once the amyloid load increases again [30].
Biomarker findings indicate that the earliest molecular changes in AD may occur many years, or even decades, before the onset of symptoms [31]. For this reason, an optimal immunotherapeutic effect would probably require that treatment begins already at the presymptomatic stage. These possibilities are explored in several clinical trials. The already concluded A4 trial investigated the use of solanezumab in cognitively intact individuals with positive amyloid PET, but no clinical benefit could be seen after almost 5 years of treatment [32]. Another completed study, Dominantly Inherited Alzheimer Network-Trials Unit-001 (DIAN-TU-001), enrolled carriers of various AD-causing mutations at both presymptomatic and mild symptomatic stages. Subjects were treated for 4–7 years with either solanezumab or gantenerumab. No clinical effects were seen, but those subjects taking gantenerumab displayed a reduced amyloid plaque load, lower CSF tau (both total tau and p-tau 181) as well as a smaller increase of the CSF neurofilament light chain [33].
In the ongoing AHEAD 3-45 trial, cognitively normal subjects aged 55–85 years are treated with lecanemab, after having been included based on a pathological plasma Aβ42/40 ratio and amyloid PET screening steps [34]. Different primary outcome measures will be adopted in the two substudies; with one evaluating amyloid PET measures and the other assessing cognitive performance [34]. Yet another ongoing trial, TRAILBLAZER-ALZ3, will treat 3300 cognitively normal subjects aged 55–80 years, who have displayed elevated plasma levels of p-tau 217, with donanemab [35].
As an interesting feature of the anti-Aβ immunotherapies, patients may display a decrease in the volume of certain brain areas, as measured by magnetic resonance imaging, a feature that has been seen both for active [36] and passive [37] immunotherapy. This may seem paradoxical, but could be a consequence of efficient amyloid-plaque removal and a reduced presence of dystrophic neurites and inflammation/gliosis [38]. A summary of the three anti-Aβ immunotherapies that have so far shown success in phase III clinical trials is presented in Table 1.
2.2 Immunotherapies Targeting Tau
Plaque pathology corresponds poorly to disease severity and progression whereas tangle pathology is a much better clinicopathological correlate [39], making also tau a relevant target for AD therapy. Potentially, treatment against tau may be a more efficient therapeutic strategy, at least at later disease stages when the neurodegeneration may be mainly driven by tau-related mechanisms.
Similar to Aβ, immunotherapy against tau has been evaluated both experimentally and in clinical trials. Generally, preclinical results have been encouraging and transgenic/knock-in tau mice treated with both passive and active anti-tau immunotherapy have shown both reduced pathology and improved behavior as compared with placebo-treated mice (reviewed in [40]). Similar to the anti-Aβ mAbs, several of the anti-tau mAbs have been humanized and advanced to clinical trials. Currently, a number of active and passive anti-tau immunotherapies are being evaluated in patients with AD. There have been some disappointing outcomes to date, resulting in termination of several such agents. However, certain ongoing anti-tau immunotherapy trials have reported some encouraging results and, in the following, we provide examples from three such trials, one based on active immunization and two based on passive immunization.
The AADvac1 (Axon peptide 108 conjugated to KLH) vaccine was designed to target the second microtubule-binding domain of tau (present only in isoforms with four such repeat domains) [41]. In a phase II trial, it was found that the treatment can ameliorate clinical decline with better CDR-SB and ADCS-MCI-ADL scores in the treatment than in the placebo group, as well as lead to decreased CSF levels of p-tau 217 [42]. Furthermore, plasma neurofilament light, a marker of neurodegeneration, rose significantly less in the subset of treated patients who were positive for both Aβ and tau biomarkers [42].
An anti-tau mAb, semorinemab, was developed to target the n-terminus of monomeric and oligomeric tau [43]. In a phase II trial, semorinemab was shown to decrease CSF tau. In addition, it had some benefit on one of several included clinical scales. However, despite these somewhat promising results, it has not yet been declared whether this compound will advance to a phase III trial or not [44].
Yet another passive anti-tau immunotherapy, based on the E2814 mAb (raised against the second and fourth microtubule-binding repeats), has shown interesting preliminary results in a phase Ib/II trial on patients with dominantly inherited AD caused by APP or PSEN mutations [45]. Three weeks of treatment resulted in lower levels of a tau fragment (tau 243-254) in CSF [45]. This antibody is now being evaluated as either a monotherapy (NCT04971733) or together with lecanemab (NCT05269394) on both symptomatic and presymptomatic carriers of different early-onset AD mutations, within the DIAN-TU [46].
Numerous additional anti-tau immunotherapies have been formulated and evaluated in both the preclinical and clinical settings (reviewed in [40, 47]). In general, the completed and ongoing trials have so far not demonstrated any effects similar to those seen with anti-Aβ immunotherapies but the field is still at a relatively early stage of development.
Similar to anti-Aβ immunotherapy, the choice of which epitope to target is a central question for how to design a successful anti-tau immunotherapy. As described above, both n-terminal and microtubule-binding repeat mAbs are currently being evaluated. The microtubule-binding repeat region, as well as even more c-terminal sites should be particularly attractive as these epitopes make up most of the insoluble aggregates in the AD brain. In addition, different phosphorylated epitopes may be suitable therapeutic targets, but more research is needed in order to better understand the significance of the different phosphorylated tau species in AD.
With time, it may be feasible to refine anti-tau immunotherapies to selectively target the most pathogenic species and thereby potentially enhance their efficacy. For an optimal effect, it may be required to transition towards molecular precision, wherein patients are further divided, based on their disease stage and/or biomarker profiles, in order to identify the subgroup(s) for which anti-tau immunotherapy will have its most significant effects. However, it remains possible that tau will never become a successful target for AD therapy as it is more likely to be only a secondary effect to APP/Aβ pathology.
2.3 How to Manage Immunotherapies
There is an ongoing debate regarding how the immunotherapies should be administered. One perspective, applied for the donanemab phase III trial [30], suggests that anti-Aβ therapy should be administered only until the plaque load has become sufficiently suppressed, as measured by amyloid PET. With repeated PET examinations, one could determine an Aβ level at which it would be appropriate to restart the medication. This line of reasoning is predicated on the assumption that the primary therapeutic targets are the accumulated Aβ aggregates. However, Aβ is continuously generated and, regardless of whether it is due to increased production or decreased degradation, an intermittent therapy would allow for the build-up of toxic Aβ, which most likely will reduce clinical efficacy of any Aβ-lowering agent. Once more sophisticated PET methods that can visualize the toxic soluble Aβ aggregates are developed, such a strategy may become more rational.
As mentioned above, a combination of anti-Aβ and anti-tau immunotherapies may be an attractive option, but probably only when robust treatment effects can be demonstrated also for the tau immunotherapies when employed on their own. Such a combination approach may be particularly suitable once the capacity for early diagnosis improves. It should then be possible to intervene with anti-Aβ therapy before the tau pathology has become severe and once a robust treatment response has been achieved, one could continue with anti-tau treatment either alone or in combination with continued anti-Aβ mAb therapy. It is also plausible that a combined pharmacological approach should be reserved for patients with evidence of both Aβ and tau pathology above a certain threshold. Interestingly, post hoc analyses of data from the lecanemab phase III trial suggest that anti-Aβ immunotherapy works better if the treated patients only have a low degree of tau pathology [48]. In order to determine the treatment strategy for the individual patient, and to monitor the treatment responses, a combination of amyloid PET and tau PET would provide us with the best measures, but also CSF and/or plasma markers would be valuable in this context.
2.4 Improved Properties of mAbs for Immunotherapies
The currently approved anti-Aβ immunotherapies should be viewed as the first generation of treatments of its class. It is foreseeable, just as in other diseases like multiple sclerosis, that the first drugs on the market will pave the way for even more efficient therapies over time.
A number of strategies can be undertaken to drive improvement in therapeutic outcomes for the immunotherapies. First, the pharmacokinetics can be optimized. In their traditional immunoglobulin G format, it has been estimated that less than 0.1% of the mAbs reach the central nervous system (CNS) upon intravenous infusion in non-human primates [49]. Although this apparently is sufficient for robust plaque removal, it is not known if the mAbs have been efficiently distributed throughout the brain and if the overall levels of pathogenic species have been optimally suppressed.
The mAbs can enter the brain mainly via two routes, either by crossing into the brain directly from the blood vessels via the blood–brain barrier or by first being taken up to CSF via the choroid plexus and from there being absorbed into the brain parenchyma [50]. In their unmodified configuration, mAbs are believed to mainly reach the brain via the CSF route, which not only makes the passage less efficient but which also, in the case of anti-Aβ mAbs, may result in a higher degree of interaction with perivascular Aβ (which is believed to be the underlying reason for why ARIAs develop). By molecular modifications of the mAbs, it has become possible to steer them away from the CSF route and instead increase their uptake through the blood-brain barrier, so that they can interact more robustly with parenchymal aggregates and avoid the endothelial deposits [51]. The most investigated such “brain shuttles” are based on anti-transferrin receptor (anti-TfR) antibodies, which can be cloned onto the therapeutic anti-Aβ antibody. By binding to the TfR, such a bispecific antibody is being taken up at least ten times more efficiently than the non-modified anti-Aβ antibody. A study of mAb158 (the murine parent antibody of lecanemab) on a transgenic mouse model showed that its distribution became more global and its therapeutic effect more robust when the mice were treated with the bispecific mAb158 variant as compared with the regular mAb158 [52]. Moreover, another bispecific anti-Aβ antibody, trontinemab, resulted in a 4–18% increased brain uptake as compared with gantenerumab (its non-modified antibody) when used in non-human primates. Trontinemab is now in a phase I clinical trial [53] and was recently in a small set of cases reported to result in a rapid plaque clearance with a very low occurrence of ARIA-E [54]. Thus, apart from a better therapeutic response, bispecific anti-Aβ/TfR antibodies may also lead to a lower risk for severe side effects, which hopefully could reduce the need for regular magnetic resonance imaging monitoring. However, larger data sets are needed before we can conclude how the brain shuttle format compares to the traditional antibody format with respect to treatment efficacies and side-effect profiles. The brain shuttle strategy could potentially be adopted also for anti-tau immunotherapies, although to date no such clinical trials have been initiated.
Second, the mode of administration can be modified. Today, the patients need to receive their biweekly lecanemab or monthly donanemab intravenous infusions at specialized centers, but the development of subcutaneous preparations may allow them to have the injections in the primary care setting or even to self-administer the doses. These scenarios would help to somewhat ease the healthcare system burden associated with a large-scale use of immunotherapies in AD. In addition to its practical advantages, subcutaneous administration may be pharmacokinetically favorable. For example, it was recently reported from an open-label extension of its phase III trial that subcutaneous administration of lecanemab resulted in 11% higher and more stable blood concentrations compared with intravenous administration of the same drug. Accordingly, plaque removal was increased by 14% but the frequency of ARIA was also slightly higher, as compared with intravenous treatment [48].
Third, development of novel immunotherapy agents could be influenced by the growing realization that the protein pathology of AD may be propagated by species that are conferring their pathogenic properties upon their non-pathogenic physiological versions. Experimental evidence for the existence of such prion-like mechanisms have been obtained for both Aβ and tau, as well as for other proteins involved in neurodegenerative diseases [55, 56]. In addition, advances in structural imaging have allowed researchers to visualize different fibril types derived from the brains of both patients [57, 58] and transgenic mice [59] (reviewed in [60]). The presence of distinct Aβ/tau strains could play a role in the diversity observed in both the affected brain region patterns and the considerable variations in progression rates among individual patients. Future developments of immunotherapy for AD should therefore be geared towards the development of mAbs that can selectively recognize these different disease-propagating Aβ/tau strains.
3 Gene Therapies
3.1 Modulation of Aβ and Tau Production
Immunotherapies directed against Aβ have revolutionized the way we can treat AD and trials utilizing anti-tau mAbs may eventually also become successful. However, even if we can learn how to administer these treatments ahead of when the disease has caused extensive cell death, we may not be able to entirely prevent disease progression. Another, potentially more efficient, approach is to focus on genetic interventions to modulate the production of Aβ and/or tau. Several gene therapeutic strategies are under preclinical development, but in the following, we focus on two that we consider particularly attractive: RNA interference and gene editing. Such approaches have followed the initial unsuccessful attempts to develop gene therapies for AD, where for example nerve growth factor was delivered via local adeno-associated virus-mediated expression (61). However, one other approach deserves to be mentioned as it has shown promise in a small phase I trial. The protective apolipoprotein E gene variant, APOE€2, was expressed via the intrathecally administered adeno-associated virus on homozygous APOEε4 patients with AD [62]. Preliminary data indicate that this treatment may have had a beneficial effect, as indicated by favorable changes in CSF biomarkers [63].
3.2 RNA-Based Therapies
RNA interference (RNAi) is a naturally occurring process, which can serve to regulate protein synthesis as well as immunological functions. It uses small pieces of RNA to shut down protein translation by binding to the messenger RNAs that code for those proteins. It has been recognized for some time that this system can be mimicked by applying synthesized RNA, often referred to as antisense oligonucleotides (ASO) [64]. These single-stranded RNA molecules of 15–22 nucleotides in length are designed to bind complementary RNA targets and facilitate their degradation via RNase H. The first such drug, against cytomegalovirus infections, was approved in 1998 and, to date, at least 15 ASO-based therapies are available (reviewed in [65]).
For neurodegenerative disorders, where toxic gain-of-function processes are operating, ASOs offer an attractive therapeutic option. In AD, suppressed translation of both APP/Aβ and tau should in principle lead to a reduced build-up of brain pathology. Nevertheless, a primary challenge associated with this type of treatment lies in the necessity to prevent an excessive protein expression, but at the same time avoid reaching a point where its physiological functions may start to become compromised. As for the main proteins involved in AD pathogenesis, APP has been implicated in neural growth and maturation (reviewed in [66]), Aβ has been speculated to have antimicrobial functions [67], and tau is known to play a crucial role to stabilize the cytoskeleton ([68]). These are all representing physiological effects that could potentially be perturbed if the gene expression becomes too suppressed.
In order to operationalize ASOs for the treatment of CNS disorders, the components (synthetic single-stranded RNAs and a lipophilic conjugate to optimize distribution and cellular penetration) need to be repeatedly intrathecally (i.t.) delivered. In the case of nusinersen (Spinraza®), the currently only approved RNA interference treatment against a CNS disease, i.t. injections need to be given quarterly on an annual basis in patients with spinal muscular atrophy [69].
The first ASO strategy against APP/Aβ to be assessed clinically, ALN-APP, uses a synthetic small interfering RNA together with a 2′-O-hexadecyl (C16) lipophilic conjugate. Studies in mice [70] demonstrated target engagement and a phase I trial on patients with AD was initiated in 2022. Interim data suggested that CSF APP (sAPPα and sAPPβ) are lowered in a dose-dependent manner already after 2 weeks and that CSF Aβ (Aβ40 and Aβ42) are lowered after 2 months [71]. The current study is based on single i.t. doses, but also a multiple ascending dose study has been initiated.
As for ASOs against tau, neurofibrillary pathology and neuronal loss could be efficiently reduced in a transgenic mouse model [72]. In 2017, a phase Ib trial with BIIB080 was initiated, in which patients with biomarker-positive AD at either the MCI or mild dementia stage were given i.t. therapy, and in 2019, an open-label extension with quarterly injections was added. The treatment resulted in a dose-dependent decrease of CSF total tau and phospho-tau 181 by up to 60% and these levels stayed low for at least 6 months [73]. In addition, there was a clear reduction in tau PET signals. Twelve patients had participated in the PET substudy and they all displayed a reduced ligand uptake in the investigated brain regions [74]. In addition, favorable trends on cognitive and functional scales (Mini-Mental State Examination, CDR-SB, and Functional Activities Questionnaire (FAQ)) were reported for the high-dose group [75]. The ongoing phase II trial is using CDR-SB as a primary outcome, as well as several other cognitive and functional scales as secondary outcomes, and will be completed in December 2026.
Another anti-tau ASO drug, NIO 752, which has already been evaluated on patients with progressive supranuclear palsy, is planned to be assessed also for AD, but is not yet recruiting patients. As of yet, no data have been reported from the progressive supranuclear palsy trial, so it is unknown if this drug has any effects on tau or other biomarkers. Whereas RNA-based gene therapeutic strategies are further ahead for the treatment of neurological diseases, gene editing strategies may offer even more attractive opportunities for effective future therapies.
3.3 Gene Editing
Gene editing refers to a group of technologies that can either introduce DNA breaks or, more recently, replace single nucleotides in the DNA molecule. The three first such methods were the meganucleases, zinc finger nucleases and transcription activator-like effector-based nucleases. More recently, the clustered regularly interspaced short palindromic repeats (CRISPRs) have been added to the toolbox. This approach is based on the concerted action of the Cas9 endonuclease and a guide RNA, which is designed to bind a specific site on the DNA molecule where this complex can induce a double-stranded break. As the DNA repair machinery is error prone, the wrong nucleotide will occasionally be inserted, mainly resulting in insertions or deletions. The levels of correctly translated proteins will thus decrease and this can be leveraged for the treatment of disorders caused by toxic gain-of-function mechanisms.
In AD, this therapeutic principle could potentially be suitable for all disease forms, but perhaps especially for the monogenic variants associated with an increased generation of either total Aβ (as for several APP mutations) or the more aggregation prone Aβ42 (as for a majority of the PSEN1/PSEN2 mutations). In two separate studies on cultured cells from patients with the APP Swe [76] and PSEN1 M146L [77] mutations, we showed that the CRISPR-Cas9 system can be designed to specifically disrupt the disease-causing alleles with targeting efficiencies of about 50%. For APP Swe, we also performed a proof-of-principle experiment in which it was demonstrated that the approach also works in vivo, upon intracerebral injections into transgenic mice [76]. For the PSEN1 M146L study, we performed careful analyses of possible off target effects but could not find any evidence of unwanted consequences, which otherwise is a general concern with this type of treatment [77].
In addition to our studies, it has been shown in mice that peripherally administered CRISPR-Cas9 can reach the brain and affect both brain pathology and symptoms. In a study from 2022, it was demonstrated that adeno-associated virus-based delivery of Cas9 and gRNA against APP Swe can ameliorate both plaque load and behavior in a transgenic APP mouse model [78].
Researchers have also begun to explore the effects of introducing protective nucleotide alterations. The APOE gene is an obvious candidate as it offers possibilities to edit nucleotides to allow for the residues at position 112 and 158 to switch from arginines, as in APOEε4, to cysteines, as in APOEε2. Alternatively (or in combination with the above), position 136 could be edited from its commonest amino acid arginine to a serine. This Christchurch mutation was found to confer protection from the development of neurofibrillary pathology and dementia in a carrier of the PSEN1 E280A mutation [79] and a recent study on cerebral organoids generated from fibroblasts of this patient suggested that the mutation suppresses hyperphosphorylation of tau [80].
Collectively, the cell and animal studies illustrate that we are nearing readiness to implement gene editing in patients. No clinical trial based on the CRISPR technology has yet been initiated for a CNS disorder, but recently the first ex vivo CRISPR-based treatment were approved by the FDA. Exagamglogene autotemcel (Casgevy®) is used to treat sickle cell disease and works by knocking out the stop codon that prevents cells from producing fetal hemoglobin [81]. As for in vivo therapy, no treatments have yet been approved but several are undergoing clinical trials. Of particular interest from an AD perspective is the ongoing CRISPR-Cas9 trial with NTLA-2001 against hereditary forms of transthyretin amyloidosis [82]. Like AD, this is a disorder that leads to accumulation of an aggregated protein with amyloid properties, which similar to Aβ results in a toxic gain of function but instead affects the heart, kidneys and peripheral neurons. Interim results from an ongoing phase I trial showed a median 91% reduction of circulating transthyretin after a one-time peripheral treatment. To investigate whether there is a parallel clinical benefit, a phase III trial has now been initiated.
We are currently witnessing a rapid development of novel technologies for precision medicine. For gene editing, it has now become possible to use methods that can replace nucleotides by using enzymes that only cut one of the two DNA molecules in the helix. This principle can be divided into base editing and prime editing. For base editing, there have been two classes of tools described: cytosine base editors and adenine base editors. Thus, the technique can only be used to make certain nucleotide replacements (reviewed in [83]). Contrary to base editing, prime editing allows for all 12 possible transition and transversion mutations, as well as for small insertions and deletions (reviewed in [84]).
In a recent tau gene (MAPT) study, it was shown that a base editor designed to convert the MAPT-P301S mutation to wild-type MAPT could correct 5.7% of all cells (corresponding to 10–11% of the neurons) upon a intrahippocampal injection of the base-editing components into mice [85]. Intriguingly, this modest degree of editing had significant effects both on brain pathology and behavioral testing [85]. Although this approach was assessed on a model for familial frontotemporal dementia, it suggests that MAPT gene editing could be a feasible strategy also for AD.
Furthermore, gene-editing approaches aimed at providing disease resilience are beginning to be explored. By introducing the protective Icelandic APP A673T mutation, Canadian researchers have demonstrated that Aβ generation can be effectively suppressed upon either base [86] or prime [87] editing of human cells with certain pathogenic APP mutations.
With a combination of different CRISPR-based gene editing technologies in the toolbox, we will have the capability to correct any possible genetic aberration for the purpose of treating AD. As remaining challenges, we need to further improve our methods for off-target analyses, to develop more precise delivery strategies as well as to improve targeting efficiencies. Especially for prime editing, it has been challenging to target neurons or glia in the CNS, but recent advances have improved the rate of editing also in such cells [88].
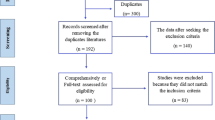
For an overview of the main immunotherapeutic and gene therapeutic targets in AD, please see Fig. 1.
Target points for disease-modifying immunotherapies and gene therapies aimed at the amyloid-β (Aβ) and tau aggregation cascades. The three anti-Aβ immunotherapies that have been approved by the US Food and Drug Administration are indicated on the left side of the panel. The three tau immunotherapies displayed on the right were chosen as they have all shown some promise in concluded or ongoing clinical trials. The ongoing anti-sense oligonucleotide (ASO) trials, together with the preclinical gene editing based approaches, all targeting either amyloid precursor protein (APP)/Aβ or tau, are also illustrated. CRISPR clustered regularly interspaced short palindromic repeats, dsDNA double-stranded DNA, mAB monoclonal antibody, mRNA messenger RNA, siRNA small interfering RNA. Image created by Gustavo Grimmer using BioRender
4 Other Pharmacological Approaches
4.1 The 2024 AD Pipeline
Although we have here focused on immunotherapies and gene therapies, we would like to emphasize that a large number of other pharmacological approaches have been or are being assessed for the treatment of AD. In the 2024 pipeline, there were 164 trials testing 127 different drugs of which 32 are in phase III (reviewed in [89]). Of the phase III trials, 66% are considered disease-modifying therapies, including nine biologics and 12 small molecules. Those compounds that were registered at ClinicalTrials.gov on 1 January, 2024 are shown in Fig. 2 [89]. Their mechanistic targets include Aβ/tau, synaptic plasticity/neuroprotection, inflammation, and metabolism/proteostasis. In the following, we highlight some of the phase III small-molecule compounds related to these strategies.
Agents in clinical trials for treatment of Alzheimer's disease in 2024 (from ClinicalTrials.gov as of the index date of 1 January, 2024). Phase III agents are displayed in the inner ring, phase II agents in the middle ring, and phase I agents in the outer ring. Agents in green areas are biologics; agents in purple areas are disease‐modifying small molecules; agents in orange areas are agents targeting cognitive enhancement or behavioral symptoms; and agents in blue areas target behavioral and neuropsychiatric symptoms. The shape of the icon shows the target population of the trial; the icon color shows the Common Alzheimer’s Disease Research Ontology (CADRO)‐based class of the agent (“Other” category includes CADRO classes that have three or fewer agents in trials). ApoE apolipoprotein E, CBD cannabidiol, DHA docosahexaenoic acid, THC delta-9-tetrahydrocannabinol, Tx treatment. Used with permission from the authors [89] and from Alzheimer’s & Dementia: Translational Research & Clinical Interventions published by Wiley Periodicals LLC on behalf of Alzheimer’s Association.
4.2 Compounds Targeting Aβ/Tau
Valiltramiprosate (ALZ-801), the prodrug of tramiprosate that targets Aβ, is of particular interest because it is administered orally. It is currently evaluated on patients with early AD homozygous for APOEε4 [90] (reviewed in [89]).
4.3 Compounds Promoting Synaptic Plasticity/Neuroprotection
Blarcamesine (Anavex-2-73), a sigma-1 receptor agonist and M2 autoreceptor antagonist, met primary endpoints in a phase II trial and is now undergoing an open-label extension study. Another agent, fosgonimeton (ATH-1017), is a hepatocyte growth factor that is believed to activate signaling via the hepatocyte growth factor/MET receptor system and thereby promote survival of neurons and enhance hippocampal synaptic plasticity (both drugs are reviewed in [89]. Simufilam (PTI-125), a filamin A protein inhibitor that stabilizes interaction of Aβ42 and the α7 nicotinic acetylcholine receptor, aims at decreasing tau phosphorylation and improving synaptic function. Recruitment for a phase III trial has finished, but to date no results have been reported [91]. Levetiracetam, a substance that can modulate synaptic vesicle protein 2A and reduce aberrant neuronal hyperactivity, is currently in a clinical study [89], although a previous phase III trial showed negative results [92].
4.4 Compounds Targeting Proteostasis/Proteinopathies
Buntanetap, a novel translational inhibitor of multiple neurotoxic proteins, decreases protein translation. Results of a small phase II/III trial were presented at the AAIC 2024, showing an improvement in the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) but a larger phase III trial remains to be performed [93]. Nilotinib BE, an Abl tyrosine kinase inhibitor, has autophagy enhancement properties and is supposed to promote degradation of dysfunctional proteins in the brain (reviewed in [89]).
4.5 Compound Targeting Inflammation
Masitinib is a tyrosine kinase inhibitor exhibiting neuroprotection via inhibition of mast cell and microglia/macrophage activity. A phase III trial showed significant benefit over placebo on primary cognitive and functional endpoints [94, 95]. A confirmatory phase III trial was set to begin [89].
4.6 Compounds Targeting Various Other Mechanisms
AR1001, a phosphodiesterase 5 inhibitor that reduces Aβ production and decreases inflammation in animal models of AD, is actively recruiting to a clinical trial. Metformin, an insulin sensitizer involved in metabolism, is in an ongoing trial. Piromelatine, a melatonin and serotonin receptor agonist, believed to affect circadian rhythm, is also currently being assessed with recruitment finished. All of the above compounds are reviewed in [89].
Other noteworthy targets that deserve to be highlighted include AL002, a mAb targeting TREM2 receptors, which is currently in phase II, and semaglutide, a glucagon-like peptide 1 agonist with anti-inflammatory and insulin sensitivity effects, which is currently in a phase III trial with enrollment finished (both reviewed in [89]).
5 Future Perspectives: Moving Towards Personalized Medicine in AD
The recent advancements in anti-Aβ immunotherapies provide optimism that individuals with AD can be effectively treated with interventions that target the underlying pathogenesis, rather than solely relying on symptomatic therapies. It must be acknowledged that the clinical effects of these disease-modifying drugs thus far have been limited. However, it is essential to consider that the trials are conducted over a period of 18 months for a disease that may span several decades (including its prodromal stages). A longer continuous treatment will hopefully result in more robust therapeutic effects. Accordingly, recently reported data from an open-label extension study of the lecanemab phase III study suggest that the CDR-SB outcome measure continues to diverge between the treatment and placebo groups [48].
As we progress in the implementation of disease-modifying therapies in AD, it will become crucial to gather more knowledge. Longitudinal studies in which data are carefully collected on treated patients will help to elucidate the long-term effects and identify which patient populations that are likely to respond best and thus result in a successful treatment outcome. For example, patients with AD may benefit more from anti-Aβ immunotherapy if their Aβ pathology is more extensive than their tau pathology. In support of this notion, and as already mentioned above, open-label extension data from the lecanemab phase III trial indicate that patients with a lower tangle load in their brain, as determined by tau PET, respond better than those with a higher tangle load [48]. Analyses of yet other biomarkers for neurodegeneration, neuroinflammation and the concomitant presence of other protein pathologies will provide us with further insight into how various aspects of the disease may influence the individual therapeutic response and how we can use such information to identify appropriate patients for treatment and thus deliver personalized medicine.
We also need to know how to select patients to minimize the risk for severe side effects. From the lecanemab trial, there are indications that sex and age-related differences may impact the patient response [26]. Moreover, certain patient groups seem to be more vulnerable to side effects. Mainly, the APOEε4 genotype has in all studies shown to confer an increased risk for ARIAs. From both the aducanumab and lecanemab phase III trials, a two to three times increased risk for ARIA-E could be seen in APOEε4 carriers with the 10-mg/kg dose [24, 26]. From the lecanemab phase III trial, it was reported that, among them, homozygotes had a six to seven times increased risk for ARIA-E as compared with non-carriers [26].
A particularly interesting question is whether a combination of anti-Aβ and anti-tau immunotherapies could lead to more robust treatment effects. Ongoing trials will eventually provide us with such information, but the prospect for a combination approach may only become attractive when a tau monotherapy has been proven effective.
The advent of gene therapies is providing us with exciting opportunities. Among these, RNA interference represents the most mature strategy and reports from ongoing trials aimed at both APP/Aβ and tau have suggested robust target engagements. Larger studies, designed to also look at clinical effects, will inform us on whether this approach can be developed into a viable therapy, either on its own or possibly in combination with immunotherapy.
Gene editing, especially based on CRISPR-Cas9, represents another exciting therapeutic possibility to target both APP/Aβ and tau. Once we have learned how the CNS neurons (and glial cells) can be more selectively and efficiently targeted and how we can minimize the risk for off-target effects, the techniques may enable very effective disease-modifying treatments. The early-onset familial forms, with the possibility to start intervention well before the expected age at onset, may represent the most attractive patient populations for this type of approach. With base and prime editing we could, instead of disrupting a gene, correct disease-causing mutations or risk gene polymorphisms such as those of APOE. The day may also come when it becomes feasible to introduce protective gene changes in asymptomatic individuals with certain risk profiles. For example, it may soon become possible to use gene editing to introduce disease-protective gene variants in individuals at risk. Preclinical studies are underway to explore such possibilities. For example, by introducing the APOE Christchurch mutation in a mouse model of tau pathology, neuroprotective effects could be seen [96]. Other studies have indicated that prime editing can be employed on cultured cells to introduce the protective Icelandic APP A673T mutation and thereby decrease Aβ levels [86, 87]. The transmembrane 106B (TMEM106B) T185S polymorphism, which has been described as a protective haplotype in AD [97] as well as in other conditions including genetic forms of frontotemporal dementia [98], may be another candidate for therapeutic gene editing.
Results from the concluded and ongoing clinical trials described in this article have provided us with some insights on how we can personalize the treatment for AD. The clinical trial successes were made possible by biomarker-based recruitment, but even participants at the MCI stage may be too advanced to allow for robust therapeutic effects. We must persist in our efforts to develop instruments, mainly fluid and imaging biomarkers, that can help us to detect the disease at even earlier stages. As already pointed out, such tools can also allow for identifying and targeting subgroups of patients that may respond differentially to the treatments.
Another possibility for personalizing treatment comes from the increasing understanding of how AD is propagating across the affected brain. Development of a set of antibodies against different variants of pathogenic Aβ and tau species/strains would enable a more selective targeting of the protein forms that are causing harm in a particular brain. An associated challenge with this approach will be to understand which pathological species that are relevant in a specific individual. Potentially, the rapid development of various seeding assays that can be applied to samples from living patients may soon provide us with the tools needed to make such assessments.
Another aspect related to the need for personalized medicine is represented by the fact that mixed pathologies are very common in neurodegenerative diseases. A large portion of patients with AD have different forms of vascular pathology and/or additional intra-cellular or extra-cellular protein pathologies. Not only patients with the Lewy body variant of AD, but also at least half of all patients with sporadic AD, display α-synuclein deposits inside brain neurons [99, 100]. Moreover, aggregated TDP-43 is found in up to 57% of AD brains [101]. It is not always clear how much these concomitant pathologies are contributing to the overall clinical picture and whether they appear independently or as a consequence of the Aβ/tau pathologies. In either way, it is possible that they need to be targeted separately for an optimal therapeutic effect. An additional challenge related to both α-synuclein and TDP-43 is the lack of diagnostic markers, although seeding assays of α-synuclein have made significant progress and may soon become widely adapted diagnostic tools. In addition, the development of therapies targeting these pathologies has not advanced as much as those targeting Aβ and tau. As for α-synuclein, immunotherapies are being developed (reviewed in [102]), but so far clinical trials aimed at TDP-43 have only been launched for amyotrophic lateral sclerosis/frontotemporal dementia where this pathology is seen in more than 95% of all cases (reviewed in [103]).
The disease-modifying drugs, based on decades of research into the underlying molecular disease mechanisms, are now providing new opportunities to treat AD. However, we must not forget to let our patients take advantage of the traditional treatments. Both the acetylcholinesterase inhibitors and NMDA-receptor antagonists have been proven efficacious on mild and moderate/severe disease, respectively. In fact, donepezil has been shown to slow down the progression of symptoms by 0.3–0.6 on CDR-SB, as compared with placebo [104, 105]. Thus, although these effects are not long-lasting they have, in the short term, been similar to those for the anti-Aβ immunotherapies. We also need to continue to improve treatments for vascular risk factors and become better at encouraging our patients to make those lifestyle changes that are likely to promote healthy brain aging [106, 107]. Thus, we need to adopt a perspective that considers both pharmacological and non-pharmacological approaches to optimize brain function in patients affected by AD.
References
Gustavsson A, Norton N, Fast T, Frolich L, Georges J, Holzapfel D, et al. Global estimates on the number of persons across the Alzheimer’s disease continuum. Alzheimers Dement. 2023;19(2):658–70.
WHO. Global status report on the public health response to dementia. Geneva: WHO; 2021.
Hampel H, Mesulam MM, Cuello AC, Farlow MR, Giacobini E, Grossberg GT, et al. The cholinergic system in the pathophysiology and treatment of Alzheimer’s disease. Brain. 2018;141(7):1917–33.
Ringman JM, Cummings JL. Current and emerging pharmacological treatment options for dementia. Behav Neurol. 2006;17(1):5–16.
Alzheimer A. Über eine eigenartige Erkrankung der Hirnrinde. Allg Zschr Psychiatr Psych Gerichtl Med. 1907;64:146–8.
Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natil Acad Sci U S A. 1985;82(12):4245–9.
Grundke-Iqbal I, Iqbal K, Tung YC, Quinlan M, Wisniewski HM, Binder LI. Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci U S A. 1986;83(13):4913–7.
Goate A, Chartier-Harlin MC, Mullan M, Brown J, Crawford F, Fidani L, et al. Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature. 1991;349(6311):704–6.
Mullan M, Crawford F, Axelman K, Houlden H, Lilius L, Winblad B, et al. A pathogenic mutation for probable Alzheimer’s disease in the APP gene at the N-terminus of beta-amyloid. Nat Genet. 1992;1(5):345–7.
Hardy J. Amyloid, the presenilins and Alzheimer’s disease. Trends Neurosci. 1997;20(4):154–9.
Jonsson T, Atwal JK, Steinberg S, Snaedal J, Jonsson PV, Bjornsson S, et al. A mutation in APP protects against Alzheimer’s disease and age-related cognitive decline. Nature. 2012;488(7409):96–9.
Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595–608.
McDade E, Voytyuk I, Aisen P, Bateman RJ, Carrillo MC, De Strooper B, et al. The case for low-level BACE1 inhibition for the prevention of Alzheimer disease. Nat Rev. 2021;17(11):703–14.
De Strooper B, Karran E. New precision medicine avenues to the prevention of Alzheimer’s disease from insights into the structure and function of gamma-secretases. EMBO J. 2024;43(6):887–903.
Luo JE, Li YM. Turning the tide on Alzheimer’s disease: modulation of gamma-secretase. Cell Biosci. 2022;12(1):2.
Schenk D, Barbour R, Dunn W, Gordon G, Grajeda H, Guido T, et al. Immunization with amyloid-beta attenuates Alzheimer-disease-like pathology in the PDAPP mouse. Nature. 1999;400(6740):173–7.
Hock C, Konietzko U, Streffer JR, Tracy J, Signorell A, Muller-Tillmanns B, et al. Antibodies against beta-amyloid slow cognitive decline in Alzheimer’s disease. Neuron. 2003;38(4):547–54.
Nicoll JA, Wilkinson D, Holmes C, Steart P, Markham H, Weller RO. Neuropathology of human Alzheimer disease after immunization with amyloid-beta peptide: a case report. Nat Med. 2003;9(4):448–52.
Doody RS, Thomas RG, Farlow M, Iwatsubo T, Vellas B, Joffe S, et al. Phase 3 trials of solanezumab for mild-to-moderate Alzheimer’s disease. N Engl J Med. 2014;370(4):311–21.
Ostrowitzki S, Bittner T, Sink KM, Mackey H, Rabe C, Honig LS, et al. Evaluating the safety and efficacy of crenezumab vs placebo in adults with early Alzheimer disease: two phase 3 randomized placebo-controlled trials. JAMA Neurol. 2022;79(11):1113–21.
Salloway S, Sperling R, Fox NC, Blennow K, Klunk W, Raskind M, et al. Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s disease. N Engl J Med. 2014;370(4):322–33.
Rinne JO, Brooks DJ, Rossor MN, Fox NC, Bullock R, Klunk WE, et al. 11C-PiB PET assessment of change in fibrillar amyloid-beta load in patients with Alzheimer’s disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol. 2010;9(4):363–72.
Sevigny J, Chiao P, Bussiere T, Weinreb PH, Williams L, Maier M, et al. The antibody aducanumab reduces Abeta plaques in Alzheimer’s disease. Nature. 2016;537(7618):50–6.
Budd Haeberlein S, Aisen PS, Barkhof F, Chalkias S, Chen T, Cohen S, et al. Two randomized phase 3 studies of aducanumab in early Alzheimer’s disease. J Prev Alzheimers Dis. 2022;9(2):197–210.
Biogen to realign resources for Alzheimer's disease franchise. 2024. Available from: https://investors.biogen.com/news-releases/news-release-details/biogen-realign-resources-alzheimers-disease-franchise. Accessed 24 Aug 2024.
van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9–21.
Van Dyck CH SR, Dhadda S, Li D, Hersch S, Irizarry MC, Kramer LD, editors. Is there evidence for a continued benefit for long-term lecanemab treatment? A benefit/risk update from long-term efficacy, safety and biomarker data. In: Alzheimer's Association International Conference; 28 Jul–1 Aug 2024; Philadelphia (PA).
Charil A CY, Willis BA, Hersch S, Irizarry MC, Reyderman L, editors. Lecanemab slows tau PET accumulation. In: Alzheimer’s Association International Conference; 28 Jul–1 Aug 2024; Philadelphia (PA).
Teunissen CWB, Bhagunde P, Bell R, Penner N, Sachdev P, Reyderman L, editors. Long-term effects of lecanemab on biomarkers of neurodegeneration in plasma Alzheimer’s Association International Conference; 28 Jul–1 Aug 2024; Philadelphia (PA).
Sims JR, Zimmer JA, Evans CD, Lu M, Ardayfio P, Sparks J, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330(6):512–27.
Palmqvist S, Janelidze S, Quiroz YT, Zetterberg H, Lopera F, Stomrud E, et al. Discriminative accuracy of plasma phospho-tau217 for Alzheimer disease vs other neurodegenerative disorders. JAMA. 2020;324(8):772–81.
Sperling RA, Donohue MC, Raman R, Rafii MS, Johnson K, Masters CL, et al. Trial of solanezumab in preclinical Alzheimer’s disease. N Engl J Med. 2023;389(12):1096–107.
Salloway S, Farlow M, McDade E, Clifford DB, Wang G, Llibre-Guerra JJ, et al. A trial of gantenerumab or solanezumab in dominantly inherited Alzheimer’s disease. Nat Med. 2021;27(7):1187–96.
Rafii MS, Sperling RA, Donohue MC, Zhou J, Roberts C, Irizarry MC, et al. The AHEAD 3–45 Study: design of a prevention trial for Alzheimer’s disease. Alzheimers Dement. 2023;19(4):1227–33.
Donanemab overview. Available from: https://www.alzforum.org/therapeutics/donanemab2024. Accessed 24 Aug 2024.
Fox NC, Black RS, Gilman S, Rossor MN, Griffith SG, Jenkins L, et al. Effects of Abeta immunization (AN1792) on MRI measures of cerebral volume in Alzheimer disease. Neurology. 2005;64(9):1563–72.
Swanson CJ, Zhang Y, Dhadda S, Wang J, Kaplow J, Lai RYK, et al. A randomized, double-blind, phase 2b proof-of-concept clinical trial in early Alzheimer’s disease with lecanemab, an anti-Aβ protofibril antibody. Alzheimers Res Ther. 2021;13(1):80.
Fox N CA, Sachdev P, Niu H, Irizarry MC, Hersch S, Reyderman L, editors. "Paradoxical” cerebral volume changes in anti-amyloid immunotherapy trials. In: Alzheimer’s Association International Conference; 28 Jul–1 Aug 2024; Philadelphia (PA).
Ingelsson M, Fukumoto H, Newell KL, Growdon JH, Hedley-Whyte ET, Frosch MP, et al. Early Aβ accumulation and progressive synaptic loss, gliosis, and tangle formation in AD brain. Neurology. 2004;62(6):925–31.
Congdon EE, Ji C, Tetlow AM, Jiang Y, Sigurdsson EM. Tau-targeting therapies for Alzheimer disease: current status and future directions. Nat Rev. 2023;19(12):715–36.
Kontsekova E, Zilka N, Kovacech B, Novak P, Novak M. First-in-man tau vaccine targeting structural determinants essential for pathological tau-tau interaction reduces tau oligomerisation and neurofibrillary degeneration in an Alzheimer’s disease model. Alzheimers Res Ther. 2014;6(4):44.
Novak P, Kovacech B, Katina S, Schmidt R, Scheltens P, Kontsekova E, et al. ADAMANT: a placebo-controlled randomized phase 2 study of AADvac1, an active immunotherapy against pathological tau in Alzheimer’s disease. Nat Aging. 2021;1(6):521–34.
Ayalon G, Lee SH, Adolfsson O, Foo-Atkins C, Atwal JK, Blendstrup M, et al. Antibody semorinemab reduces tau pathology in a transgenic mouse model and engages tau in patients with Alzheimer's disease. Sci Transl Med. 2021;13(593):eabb2639. https://doi.org/10.1126/scitranslmed.abb2639.
Monteiro C, Toth B, Brunstein F, Bobbala A, Datta S, Ceniceros R, et al. Randomized phase II study of the safety and efficacy of semorinemab in participants with mild-to-moderate Alzheimer disease: Lauriet. Neurology. 2023;101(14):e1391–401.
Roberts M, Sevastou I, Imaizumi Y, Mistry K, Talma S, Dey M, et al. Pre-clinical characterisation of E2814, a high-affinity antibody targeting the microtubule-binding repeat domain of tau for passive immunotherapy in Alzheimer’s disease. Acta Neuropathol Commun. 2020;8(1):13.
Clinical.Trials.gov. 2024. Available from: https://clinicaltrials.gov/. Accessed 24 ug 2024.
Congdon EE, Sigurdsson EM. Tau-targeting therapies for Alzheimer disease. Nat Rev. 2018;14(7):399–415.
Eisai presents new Leqembi® (Lecanemab-IRMB) investigational subcutaneous formulation interim study results and clinical improvement data in earlier stages of early Alzheimer's disease from additional analyses of Clarity AD at the Clinical Trials on Alzheimer's disease (CTAD) Conference [press release]. 2023. https://www.eisai.com/news/2023/news202368.html.
Kariolis MS, Wells RC, Getz JA, Kwan W, Mahon CS, Tong R, et al. Brain delivery of therapeutic proteins using an Fc fragment blood-brain barrier transport vehicle in mice and monkeys. Sci Transl Med. 2020;12(545):eaay1359.
Pizzo ME, Wolak DJ, Kumar NN, Brunette E, Brunnquell CL, Hannocks MJ, et al. Intrathecal antibody distribution in the rat brain: surface diffusion, perivascular transport and osmotic enhancement of delivery. J Physiol. 2018;596(3):445–75.
Gustavsson T, Syvanen S, O’Callaghan P, Sehlin D. SPECT imaging of distribution and retention of a brain-penetrating bispecific amyloid-beta antibody in a mouse model of Alzheimer’s disease. Transl Neurodegen. 2020;9(1):37.
Syvanen S, Hultqvist G, Gustavsson T, Gumucio A, Laudon H, Soderberg L, et al. Efficient clearance of Abeta protofibrils in AbetaPP-transgenic mice treated with a brain-penetrating bifunctional antibody. Alzheimers Res Ther. 2018;10(1):49.
Grimm HP, Schumacher V, Schafer M, Imhof-Jung S, Freskgard PO, Brady K, et al. Delivery of the brainshuttle amyloid-beta antibody fusion trontinemab to non-human primate brain and projected efficacious dose regimens in humans. MAbs. 2023;15(1):2261509.
Alzforum. Fast plaque clearance with little ARIA? So teases trontinemab at AD/PD 2024. Available from: https://www.alzforum.org/news/conference-coverage/fast-plaque-clearance-little-aria-so-teases-trontinemab-adpd-2024. Accessed 24 Aug 2024.
Prusiner SB. Cell biology: a unifying role for prions in neurodegenerative diseases. Science. 2012;336(6088):1511–3.
Jucker M, Walker LC. Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature. 2013;501(7465):45–51.
Fitzpatrick AWP, Falcon B, He S, Murzin AG, Murshudov G, Garringer HJ, et al. Cryo-EM structures of tau filaments from Alzheimer’s disease. Nature. 2017;547(7662):185–90.
Yang Y, Arseni D, Zhang W, Huang M, Lovestam S, Schweighauser M, et al. Cryo-EM structures of amyloid-beta 42 filaments from human brains. Science. 2022;375(6577):167–72.
Zielinski M, Peralta Reyes FS, Gremer L, Schemmert S, Frieg B, Schafer LU, et al. Cryo-EM of Abeta fibrils from mouse models find tg-APP(ArcSwe) fibrils resemble those found in patients with sporadic Alzheimer’s disease. Nat Neurosci. 2023;26(12):2073–80.
Scheres SHW, Ryskeldi-Falcon B, Goedert M. Molecular pathology of neurodegenerative diseases by cryo-EM of amyloids. Nature. 2023;621(7980):701–10.
Rafii MS, Baumann TL, Bakay RA, Ostrove JM, Siffert J, Fleisher AS, et al. A phase1 study of stereotactic gene delivery of AAV2-NGF for Alzheimer’s disease. Alzheimers dement. 2014;10(5):571–81.
Rosenberg JB, Kaplitt MG, De BP, Chen A, Flagiello T, Salami C, et al. AAVrh.10-mediated APOE2 central nervous system gene therapy for APOE4-associated Alzheimer’s disease. Hum Gene Ther Clin Dev. 2018;29(1):24–47.
Kaplitt MLP, Noch E, Ivanidze J, Chazen L, Crystal R, Kaminsky S, et al. A phase 1, open-label, 52-week, multicenter study to evaluate the safety and biochemical efficacy of AAV gene therapy (LX1001) in patients with APOE4 homozygote Alzheimer’s disease. In: Clinical Trials on Alzheimer's Disease conference (CTAD): JPAD; 2022, p. S33.
Zamecnik PC, Stephenson ML. Inhibition of Rous sarcoma virus replication and cell transformation by a specific oligodeoxynucleotide. Proc Natl Acad Sci U S A. 1978;75(1):280–4.
Lauffer MC, van Roon-Mom W, Aartsma-Rus A, Collaborative N. Possibilities and limitations of antisense oligonucleotide therapies for the treatment of monogenic disorders. Commun Med (Lond). 2024;4(1):6.
Coronel R, Bernabeu-Zornoza A, Palmer C, Muniz-Moreno M, Zambrano A, Cano E, et al. Role of amyloid precursor protein (APP) and its derivatives in the biology and cell fate specification of neural stem cells. Mol Neurobiol. 2018;55(9):7107–17.
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, et al. The Alzheimer’s disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS ONE. 2010;5(3): e9505.
Avila J, Lucas JJ, Perez M, Hernandez F. Role of tau protein in both physiological and pathological conditions. Physiol Rev. 2004;84(2):361–84.
Finkel RS, Chiriboga CA, Vajsar J, Day JW, Montes J, De Vivo DC, et al. Treatment of infantile-onset spinal muscular atrophy with nusinersen: final report of a phase 2, open-label, multicentre, dose-escalation study. Lancet Child Adolesc Health. 2021;5(7):491–500.
Brown KM, Nair JK, Janas MM, Anglero-Rodriguez YI, Dang LTH, Peng H, et al. Expanding RNAi therapeutics to extrahepatic tissues with lipophilic conjugates. Nat Biotechnol. 2022;40(10):1500–8.
Alnylam and Regeneron report positive interim phase 1 clinical data on ALN-APP, an investigational RNAi therapeutic for Alzheimer’s disease and cerebral amyloid angiopathy [press release]. 2023. https://investor.regeneron.com/news-releases/news-release-details/regeneron-and-alnylam-report-positive-interim-phase-1-clinical/.
DeVos SL, Miller RL, Schoch KM, Holmes BB, Kebodeaux CS, Wegener AJ, et al. Tau reduction prevents neuronal loss and reverses pathological tau deposition and seeding in mice with tauopathy. Sci Transl Med. 2017;9(374):eaag0481.
Mummery CJ, Borjesson-Hanson A, Blackburn DJ, Vijverberg EGB, De Deyn PP, Ducharme S, et al. Tau-targeting antisense oligonucleotide MAPT(Rx) in mild Alzheimer’s disease: a phase 1b, randomized, placebo-controlled trial. Nat Med. 2023;29(6):1437–47.
Edwards AL, Collins JA, Junge C, Kordasiewicz H, Mignon L, Wu S, et al. Exploratory tau biomarker results from a multiple ascending-dose study of BIIB080 in Alzheimer disease: a randomized clinical trial. JAMA Neurol. 2023;80(12):1344–52.
New data from Biogen’s Investigational antisense oligonucleotide (ASO) targeting tau shows promise for potential new generation of treatments in early Alzheimer’s disease [press release]. 2023. https://investors.biogen.com/news-releases/news-release-details/new-data-biogens-investigational-antisense-oligonucleotide-aso.
Gyorgy B, Loov C, Zaborowski MP, Takeda S, Kleinstiver BP, Commins C, et al. CRISPR/Cas9 mediated disruption of the Swedish APP allele as a therapeutic approach for early-onset Alzheimer’s disease. Mol Ther Nucleic Acids. 2018;11:429–40.
Konstantinidis E, Molisak A, Perrin F, Streubel-Gallasch L, Fayad S, Kim DY, et al. CRISPR-Cas9 treatment partially restores amyloid-beta 42/40 in human fibroblasts with the Alzheimer’s disease PSEN 1 M146L mutation. Mol Ther Nucleic Acids. 2022;28:450–61.
Duan Y, Ye T, Qu Z, Chen Y, Miranda A, Zhou X, et al. Brain-wide Cas9-mediated cleavage of a gene causing familial Alzheimer’s disease alleviates amyloid-related pathologies in mice. Nat Biomed Eng. 2022;6(2):168–80.
Arboleda-Velasquez JF, Lopera F, O’Hare M, Delgado-Tirado S, Marino C, Chmielewska N, et al. Resistance to autosomal dominant Alzheimer’s disease in an APOE3 Christchurch homozygote: a case report. Nat Med. 2019;25(11):1680–3.
Perez-Corredor P, Vanderleest TE, Vacano GN, Sanchez JS, Villalba-Moreno ND, Marino C, et al. APOE3 Christchurch modulates beta-catenin/Wnt signaling in iPS cell-derived cerebral organoids from Alzheimer’s cases. Front Mol Neurosci. 2024;17:1373568.
Hoy SM. Exagamglogene autotemcel: first approval. Mol Diagn Ther. 2024;28(2):133–9.
Gillmore JD, Gane E, Taubel J, Kao J, Fontana M, Maitland ML, et al. CRISPR-Cas9 in vivo gene editing for transthyretin amyloidosis. N Engl J Med. 2021;385(6):493–502.
Newby GA, Liu DR. In vivo somatic cell base editing and prime editing. Mol Ther. 2021;29(11):3107–24.
Chen PJ, Liu DR. Prime editing for precise and highly versatile genome manipulation. Nat Rev Genet. 2023;24(3):161–77.
Gee MS, Kwon E, Song MH, Jeon SH, Kim N, Lee JK, et al. CRISPR base editing-mediated correction of a tau mutation rescues cognitive decline in a mouse model of tauopathy. Transl Neurodegen. 2024;13(1):21.
Guyon A, Rousseau J, Begin FG, Bertin T, Lamothe G, Tremblay JP. Base editing strategy for insertion of the A673T mutation in the APP gene to prevent the development of AD in vitro. Mol Ther Nucleic Acids. 2021;24:253–63.
Tremblay G, Rousseau J, Mbakam CH, Tremblay JP. Insertion of the Icelandic mutation (A673T) by prime editing: a potential preventive treatment for familial and sporadic Alzheimer’s disease. CRISPR J. 2022;5(1):109–22.
Davis JR, Banskota S, Levy JM, Newby GA, Wang X, Anzalone AV, et al. Efficient prime editing in mouse brain, liver and heart with dual AAVs. Nat Biotechnol. 2024;42:253–64.
Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F. Alzheimer’s disease drug development pipeline: 2024. Alzheimers Dement (N Y). 2024;10(2): e12465.
Alzforum. Available from: https://www.alzforum.org/therapeutics/alz-8012024. Accessed 24 Aug 2024.
Cassava Sciences completes enrollment for pivotal phase 3 program of simufilam in Alzheimer’s disease [press release]. Available from: https://www.cassavasciences.com/news-releases/news-release-details/cassava-sciences-completes-enrollment-pivotal-phase-3-program2023. Accessed 24 Aug 2024.
Mohs R, Bakker A, Rosenzweig-Lipson S, Rosenblum M, Barton RL, Albert MS, et al. The HOPE4MCI study: a randomized double-blind assessment of AGB101 for the treatment of MCI due to AD. Alzheimers Dement (N Y). 2024;10(1): e12446.
Fang C, editor. Data from phase 2/3 clinical study in mild to moderate Alzheimer's disease. In: Alzheimer’s Association International Conference; 28 Jul–1 Aug 2024; Philadelphia (PA).
Dubois B, Lopez-Arrieta J, Lipschitz S, Doskas T, Spiru L, Moroz S, et al. Masitinib for mild-to-moderate Alzheimer’s disease: results from a randomized, placebo-controlled, phase 3, clinical trial. Alzheimers Res Ther. 2023;15(1):39.
Dubois B, Lopez-Arrieta J, Lipschitz S, Doskas T, Spiru L, Moroz S, et al. Correction: Masitinib for mild-to-moderate Alzheimer’s disease: results from a randomized, placebo-controlled, phase 3, clinical trial. Alzheimers Res Ther. 2023;15(1):85.
Nelson MR, Liu P, Agrawal A, Yip O, Blumenfeld J, Traglia M, et al. The APOE-R136S mutation protects against APOE4-driven tau pathology, neurodegeneration and neuroinflammation. Nat Neurosci. 2023;26(12):2104–21.
Li Z, Farias FHG, Dube U, Del-Aguila JL, Mihindukulasuriya KA, Fernandez MV, et al. The TMEM106B FTLD-protective variant, rs1990621, is also associated with increased neuronal proportion. Acta Neuropathol. 2020;139(1):45–61.
Perneel J, Manoochehri M, Huey ED, Rademakers R, Goldman J. Case report: TMEM106B haplotype alters penetrance of GRN mutation in frontotemporal dementia family. Front Neurol. 2023;14:1160248.
Hamilton RL. Lewy bodies in Alzheimer’s disease: a neuropathological review of 145 cases using alpha-synuclein immunohistochemistry. Brain Pathol. 2000;10(3):378–84.
Arai Y, Yamazaki M, Mori O, Muramatsu H, Asano G, Katayama Y. Alpha-synuclein-positive structures in cases with sporadic Alzheimer’s disease: morphology and its relationship to tau aggregation. Brain Res. 2001;888(2):287–96.
Josephs KA, Whitwell JL, Weigand SD, Murray ME, Tosakulwong N, Liesinger AM, et al. TDP-43 is a key player in the clinical features associated with Alzheimer’s disease. Acta Neuropathol. 2014;127(6):811–24.
Knecht L, Folke J, Dodel R, Ross JA, Albus A. Alpha-synuclein immunization strategies for synucleinopathies in clinical studies: a biological perspective. Neurotherapeutics. 2022;19(5):1489–502.
Hayes LR, Kalab P. Emerging therapies and novel targets for TDP-43 proteinopathy in ALS/FTD. Neurotherapeutics. 2022;19(4):1061–84.
Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT. A 24-week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer’s disease. Donepezil Study Group Neurology. 1998;50(1):136–45.
Burns A, Rossor M, Hecker J, Gauthier S, Petit H, Moller HJ, et al. The effects of donepezil in Alzheimer’s disease: results from a multinational trial. Dement Geriatr Cogn Disord. 1999;10(3):237–44.
Rosenberg A, Ngandu T, Rusanen M, Antikainen R, Backman L, Havulinna S, et al. Multidomain lifestyle intervention benefits a large elderly population at risk for cognitive decline and dementia regardless of baseline characteristics: the FINGER trial. Alzheimers Dement. 2018;14(3):263–70.
Livingston G, Huntley J, Liu KY, Costafreda SG, Selbaek G, Alladi S, et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet. 2024.
Acknowledgments
Martin Ingelsson is supported by the Krembil Family. Maria Carmela Tartaglia is supported by the Marion and Gerald Soloway Chair in Brain Injury and Concussion Research and runs clinical trials for Alzheimer's disease. Stefan Lichtenthaler and Stina Syvänen provided important input to this article. Gustavo Grimmer created Fig. 1, using BioRender. Drs. J. Cummings and M. de la Flor generously allowed for the reuse of Fig. 2.
Funding
Open access funding provided by Uppsala University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Uppsala University.
Conflicts of Interest/Competing Interests
Martin Ingelsson is a paid consultant to BioArctic AB. Maria Carmela Tartaglia has provided consultancy to EISAI, Lilly and Roche.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors’ Contributions
MCT and MI drafted and finalized the manuscript together.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tartaglia, M.C., Ingelsson, M. Molecular Therapeutics in Development to Treat Alzheimer’s Disease. Mol Diagn Ther (2024). https://doi.org/10.1007/s40291-024-00738-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s40291-024-00738-6