Abstract
Background
Thyroid cancer is prevalent worldwide, including in China, where its incidence is on the rise. Papillary thyroid carcinoma (PTC) is the predominant subtype. Investigating the relationship between clinical data associated with PTC and gene mutations is crucial for improving detection and treatment.
Patients and Methods
We collected samples and associated clinical data from 700 PTC patients at Shanxi Provincial People’s Hospital. Using a panel of 57 genes linked to thyroid cancer, we sequenced the samples to determine the mutation frequency of thyroid cancer-associated genes in PTC. We further analyzed the correlation between gene variants and clinical information.
Results
The mean age of patients in this study was 42.5 years. Females predominated, comprising 507 of the total patient population, resulting in a female-to-male ratio of 2.63 (507:193). Tumor distribution revealed 198, 257, and 142 cases on the left, right, and both sides, respectively. Among the 57 thyroid cancer-related genes analyzed, we identified at least one driver gene in 83.6% of patients. Notably, 76.4% had BRAF mutations, mainly BRAFV600E, which constituted 90.9% of all BRAF mutations, with 535 cases exhibiting these mutations. Other significant driver genes included CHEK2 (n = 84), RET (n = 42), PIK3CA (n = 7), and EGFR (n = 7). RET fusions (n = 28) were also identified. Notably, patients under 55 years old exhibit a higher tendency towards advanced N staging, suggesting that younger individuals may be more prone to lymph node metastasis. Additionally, male patients were more likely to have advanced N stages. Importantly, a positive correlation was observed between higher BRAF allele frequencies and more advanced T and N stages. Similarly, correlation analysis revealed that a greater frequency of RET fusions correlated with later T and N stages.
Conclusion
This study uncovered several significant insights. Younger PTC patients exhibited a higher propensity for lymph node metastasis. An elevated mutation frequency of BRAF was correlated with a higher occurrence of RET fusions, predisposing individuals to lymph node metastasis and potentially indicating a poorer prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We evaluated the correlation between clinical features and genetic mutations in papillary thyroid carcinoma to better understand clinical trends in key gene mutations. |
Mutations in certain genes, such as BRAF and RET, can affect lymph node metastasis in thyroid cancer. Research on gene mutations and lymph node metastasis can help with prognosis assessment. |
1 Introduction
Thyroid cancer ranks as the most prevalent form of malignant endocrine cancer globally, including in China, where its incidence has been gradually rising [1]. Due to reproductive and hormonal factors, the incidence rate among females surpasses that among males by 2.9 times [2]. Papillary thyroid cancer (PTC) accounts for approximately 85% of all thyroid cancers and remains the most frequently encountered differentiated thyroid cancer (DTC) with a favorable prognosis [3]. Patients diagnosed with PTC typically undergo surgical intervention followed by postoperative thyroid-stimulating hormone suppression. The 5-year survival rate after surgery for PTC exceeds 95%, classifying it as a manageable condition. However, a subset of PTC patients with lymph node metastases faces an increased susceptibility to thyroidectomy [4]. Hence, an enhanced comprehension of genetic and clinical characteristics is crucial for future treatments [5].
Despite a significant increase in newly diagnosed PTC cases, mortality rates have remained constant, prompting an exploration into genetic alterations strongly correlated with disease progression and patient survival [6]. Thyroid cancer results from point mutations or gene rearrangements/fusions in key genes within thyroid cells, which activate the MAPK and PI3K/AKT pathways [7]. Consequently, the in-depth investigation of thyroid cancer’s molecular genetics has led to the integration of genetic testing in clinical patient management [8]. Genetic testing enhances precision in distinguishing between benign and malignant thyroid nodules, forecasting cancer risk stratification and selecting targeted drug therapy for advanced thyroid cancer.
Genetic mutations have the potential to serve as predictive indicators of PTC treatment efficacy [9]. Previous research had highlighted major mutations within the MAPK pathway (e.g., BRAF and RAS mutations, gene fusion events like RET, NTRK1, and BRAF gene fusions) [10]. Recent studies had revealed that PTC patients with BRAF-positive/TERT-positive co-mutations have an increased risk of distant lymph node metastasis [11]. Hence, preoperative genetic testing may assist clinicians in forecasting patient prognosis and guiding clinical decision-making. In an extensive analysis of the genetic profile of PTC in the Chinese population, it was found that differences in genetic characteristics may occur due to ethnic differences [12]. Further research is essential to validate this hypothesis. Therefore, this study collected a wider range of PTC samples, aiming for a correlation analysis between clinical and molecular attributes. This endeavor seeks to foster a better comprehension of the interrelationships between clinical and molecular features of PTC, consequently furnishing assistance to inform thyroid gland diagnosis and treatment strategies.
2 Materials and Methods
2.1 Papillary Thyroid Cancer Patients and Samples
PTC samples were obtained from individuals who underwent thyroidectomy at Shanxi Provincial People’s Hospital between 2019 and 2022. The diagnosis for all participants was confirmed as PTC according to the World Health Organization (WHO) classification. Tissue specimens are evaluated by two pathologists, and the process of identifying PTC typically involves the following steps: (1) tissue specimen collection: tissue samples from suspected PTC cases are collected. (2) Pathologist evaluation: (i) two pathologists independently evaluate tissue specimens. (ii) Macroscopic examination of specimens, including shape, color, texture, etc. (iii) Microscopic examination, including assessment of cell morphology, structure and nuclear characteristics. (3) Evaluation criteria: (i) assessed according to WHO classification criteria. (ii) morphological characteristics, growth patterns, and degree of infiltration of the tumor are considered. (4) Consistency judgment: (i) comparison of assessment results by the two pathologists. (ii) If consistent, a preliminary PTC identification conclusion can be drawn. (5) Discussion of difficult cases: (i) disagreements between pathologists’ assessments may require further discussion and study. (ii) Additional steps may include referring to more pathological data, performing special staining, or immunohistochemical testing. (6) Final conclusion: comprehensive compilation of information to draw the final PTC identification conclusion. Prior to sample collection, none of the patients had received any form of treatment, and their medical history did not include any instances of other malignancies. The patients' fundamental characteristics were extracted from their clinical records. This study gained approval from the Ethics Committee of Shanxi Provincial People’s Hospital (approval number: 202025), and all participants provided written informed consent during the sample collection process. During the sample inclusion process, individuals who had undergone non-primary surgery, lacked a confirmed PTC diagnosis, or had incomplete pathological data were excluded.
After collecting all clinical data, the T, N, and M stages were classified according to the 2015 American Thyroid Association (ATA) guidelines [8]. Based on the pathological diagnosis records subsequent to the initial thyroidectomy, we categorized the primary site's location. Tumor sites were categorized as either unilateral or bilateral. For unilateral tumors, either left or right was also indicated.
2.2 DNA Extraction and Targeted Sequencing
Genomic DNA extraction was performed on fresh tumor tissue or FFPE samples utilizing the QIAamp DNA FFPE Tissue Kit from Qiagen. The extracted genomic DNA was then used for library construction with the MGIEasy Universal DNA Library Kit from MGI (China). Libraries that met the quality standards underwent 2 × 100 bp paired-end sequencing on the MGISEQ-2000 platform, also developed by MGI (China) [13]. In this study, all samples were sequenced using a panel consisting of 57 genes associated with thyroid cancer. These 57 genes have been identified as having significant value in supporting auxiliary diagnostics, assessing prognostic risks, evaluating targeted drug suitability and performing gene screening. This comprehensive panel covers a spectrum of genetic alterations, including single nucleotide variations (SNVs), small fragment insertions or deletions (INDELs), gene copy number variations (CNVs), and gene fusions.
2.3 Statistical Analysis
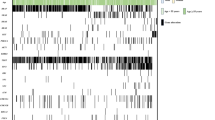
All data analyses were conducted using R version 4.1.0. Oncoplot plots were generated using ComplexHeatmap R package [14]. Genes and samples are automatically sorted in oncoplot plots. Rows are ordered by frequency of alterations between samples, and columns are ordered by sample to visualize mutual exclusivity between samples. The “memo sort” method was used to sort columns. To assess differences in variable means across groups, non-parametric tests such as the Wilcoxon test and Kruskal–Wallis test were employed. For categorical variables, Fisher’s exact test was utilized. Statistical significance was determined with a p value of < 0.05.
3 Results
3.1 Clinical Characteristics of Patients and Tumor Samples
A total of 700 patients from the People’s Hospital of Shanxi Province, China, were enrolled in this study. The mean age was 42.5 years, ranging from 16 to 77 years. The female-to-male ratio was 2.63, with 507 female and 193 male participants. Regarding tumor location, 198 patients had tumors on the left side, 257 on the right side, and 142 on both sides. Interestingly, PTCs were less frequently observed on the left side compared to the right. In terms of tumor stage, the majority of patients were categorized as T1 (84.6%), followed by T2 (13.2%). Regarding the N stage distribution, 290 patients were classified as N0, 281 as N1a, and 128 as N1b. No instances of distant metastases were observed among the study participants. The clinical characteristics of all patients are depicted in Fig. 1, Table 1, and Online Supplementary Material (OSM) 1.
By analyzing 57 genes associated with thyroid cancer, we identified at least one driver varaint in 585 patients (83.6%). The most prevalent mutation was found in the BRAF gene, detected in 532 patients (76.0%). Notably, BRAF mutations constituted the predominant mutation type among all mutation-positive patients (532 out of 585, 90.9%), with all 532 BRAF mutations corresponding to the BRAFV600E mutation. Other notable driver genes included CHEK2 (n = 84), RET (n = 42), PIKC3A (n = 7), and EGFR (n = 7). Additionally, RET fusions (n = 28) were also identified, involving various partner genes such as CCDC6 (n = 21), TTC27 (n = 3), ACBD5 (n = 2), TRIM27 (n = 2), ABLIM1 (n = 1), GRIPAP1 (n = 1), MAT2B (n = 1), PRKCQ (n = 1), PTPN4 (n = 1), SSBP2 (n = 1), TMEM26 (n = 1), TBC1D22A (n = 1), MBD5 (n = 1) and NCOA4 (n = 1) (Fig. 1).
3.2 Correlation Analysis Between Clinical Information and TNM Stage, Lymph Node Metastasis, Tumor Size
We conducted an analysis to explore the relationships between age, gender, tumor location, TNM stage, lymph node metastasis count, and tumor size. According to guidelines from the ATA and the American Joint Committee on Cancer (AJCC), the age of 55 years is a critical determinant in AJCC staging. Consequently, we divided our study cohort into two categories: ≥ 55 years and < 55 years. Using Fisher’s exact test, we found no significant correlation between age and T stage (Fig. 2A). However, individuals younger than 55 years exhibited a higher propensity for advanced N stage compared to those aged ≥ 55 years (Fig. 2B), suggesting that younger individuals may be more susceptible to lymph node metastasis.
Correlation between clinical information and TNM stage, lymph node metastasis, and tumor size. A Correlation between age and T stage. B Correlation between age and N stage. C Correlation between gender and T stage. D Correlation between gender and N stage. E, F Correlation between tumor location and lymph node metastases
Further examination revealed that male patients were more likely to exhibit a higher N stage (Fig. 2D), whereas gender did not have a significant influence on T stage (Fig. 2C). Subsequently, we investigated the impact of tumor location on lymph node metastasis. Notably, patients with lesions located bilaterally displayed a higher count of lymph node metastases (Fig. 2E).
3.3 Correlation Analysis Between BRAF Mutation and T and N Stages
The most prevalent mutation identified in this study was the BRAF mutation (n = 535/700). Statistical analysis revealed that patients with a positive BRAF status showed a tendency towards advanced N stage compared to those negative for BRAF and RET mutations. Furthermore, patients with bilateral tumors exhibited a relatively higher frequency of BRAF mutations (Fig. 2F). Conversely, patients with a positive RET status were more likely to be associated with later N and T stages.
Given the strong correlation between BRAF mutation and PTC, we gathered BRAF Mutation Allele Frequency (MAF) data from 535 patients and explored its connection to T and N stages (Fig. 3 and OSM 1). MAFs ranged from 0.32% to 45.7%, with an average MAF of 12.5%. Notably, advanced T and N stages correlated with higher average BRAF mutation frequencies. This trend was consistently observed across all samples, regardless of whether the tumor was situated on the left or right side (Fig. 3A–C). However, this pattern did not hold true for patients with lesions located on both the left and the right sides (Fig. 3D).
The relationship between mutation frequency at different primary foci locations and T and N staging in the BRAF-positive mutation population. A The relationship between gene frequency and T and N stages without considering location. B The relationship between gene frequency and T and N stages of the left side tumor. C The relationship between gene frequency and T and N stages of the left right tumor. D The relationship between gene frequency and T and N stages of the both-side tumor
3.4 RET Fusions Significantly Indicated Advanced T and N Stages
Within our study cohort, patients who tested positive for RET mutations (n = 28) exhibited distinct clinical characteristics compared to the RET-negative group (n = 672). These RET positive patients were notably younger, exhibited later T stages and displayed a pronounced inclination toward lymph node metastasis (Table 1). Utilizing correlation analysis, we identified a positive correlation between the frequency of RET fusions and advanced T and N stages (Fig. S1, OSM).
3.5 Correlation Analysis of BRAF Mutation and RET Fusion with TNM Stage, Lymph Node Metastasis, and Tumor Size
Furthermore, a correlation analysis was conducted to investigate potential associations between BRAF mutations, RET fusions and clinical factors such as age, tumor size, lymph node metastases count, and TNM stage. The results, as depicted in Fig. 4, revealed no substantial correlations. Specifically, the presence of BRAF mutations and RET fusions exhibited no dependence on age, tumor size, or the number of lymph node metastases (Fig. 4A–C). Similarly, no discernible correlation was found between BRAF mutations or RET fusions and T and N stages (Fig. 4D, 4E). However, we observed a noteworthy result: among patients with RET fusions, the number of individuals with stage T4 was significantly increased (Fig. 4D).
Correlation analysis of BRAF mutation and RET fusion with TNM stage, lymph node metastasis, and tumor size. A Statistics of age differences among patients without mutations, patients with BRAF mutations, and patients with RET fusion mutations. B Statistics of tumor size differences among patients without mutations, patients with BRAF mutations, and patients with RET fusion mutations. C Statistics of lymph node metastasis differences among patients without mutations, patients with BRAF mutations, and patients with RET fusion mutations. D Distribution of T stages in patients without mutations, patients with BRAF mutations, and patients with RET fusion mutations. E Distribution of N stages in patients without mutations, patients with BRAF mutations, and patients with RET fusion mutations
4 Discussion
In recent decades, thyroid cancer has emerged as one of the most rapidly escalating and widespread endocrine malignancies worldwide [15, 16]. The incidence of newly diagnosed PTC has experienced a significant surge [17, 18]. However, mortality rates have remained relatively stable. This phenomenon has prompted an investigation into the genetic alterations closely linked with disease progression and patient survival [6]. Thyroid cancer arises from point mutations or gene rearrangements/fusions involving pivotal genes within thyroid cells, leading to the activation of the MAPK and PI3K/AKT pathways [7]. Consequently, as researchers delve deeper into the molecular genetics of thyroid cancer, genetic testing has emerged as a valuable tool in guiding clinical treatment for patients [8]. Genetic testing enhances accuracy in distinguishing between benign and malignant thyroid nodules, prognosticating cancer risk stratification, and aiding in the selection of targeted drug therapies for advanced stages of thyroid cancer [19].
The advancement of next-generation sequencing (NGS) technology has revolutionized tumor diagnosis and treatment. By employing tumor-specific targeted sequencing panels, hundreds of pertinent genes can be analyzed simultaneously, leading to more precise tumor detection and treatment guidance. Understanding the molecular mechanisms underpinning tumor formation is imperative for achieving accurate diagnoses and enabling personalized therapies [20]. Consequently, molecular assays utilizing NGS for oncology research and clinical applications are rapidly developing. In this study, NGS was employed to identify various genetic variations using a thyroid cancer-related multi-gene panel, aiming to provide patients with more personalized treatment and promote the development of precision medicine. Furthermore, establishing a connection between genetic variants and the clinical characteristics of tumors could yield enhanced clinical significance [21].
Within this study, BRAF mutations were detected in 76.4% of patients (n = 535/700), with BRAFV600E mutations being the predominant type. The genotype distribution observed here closely resembled findings from a prior single-center study in China, where BRAF mutations constituted 72.4% of cases. These congruent results indicate that while the genetic makeup of PTC might exhibit regional variations; these differences are relatively minor [12]. Limited research has explored the influence of BRAF mutation frequency on the clinical behavior of PTC. Some international studies have indicated that a heightened frequency of BRAF mutations correlates with larger tumor sizes [22, 23]. Furthermore, a multi-center study in China revealed that BRAF mutations have a more pronounced impact on the PTC population in China [13]. These findings align with our research outcomes and provide valuable guidance for treatment strategies and prognostic assessments.
This study examined the correlation between gene mutation status in PTC and clinical variables such as lymph node metastasis. Our findings agree with prior research conducted using data from The Cancer Genome Atlas (TCGA), reinforcing the reliability of these results across different studies [24]. Within our study group, BRAF mutations were the most prevalent, aligning with findings from numerous significant studies in the field [12, 25]. Among the study group, 28 patients had RET fusions. Nonetheless, the rare coexistence of BRAF mutations and RET fusion implies that BRAF mutation may serve as an alternative to RET fusion in PTC. It’s conceivable that BRAF mutation and RET fusion might act as two distinct, mutually exclusive driver mechanisms, each potentially giving rise to varying clinical outcomes.
Based on our findings, RET fusion patients showed a higher prevalence of lymph node metastases. Lee et al. similarly evaluated the impact of lymph node-related factors on the risk of recurrence in the patient population [4]. Zheng et al. conducted an analysis encompassing factors like clinical outcomes, pathological records, ultrasound findings, and the BRAFV600E status of PTC, identifying risk factors associated with cervical lymph node metastasis [26]. Thus, investigating the interplay between clinical factors and gene variations proves is valuable for obtaining a comprehension understanding of PTC, offering substantial support for diagnosis and treatment endeavors by enhancing our understanding of the disease's intricate dynamics.
Although many factors influence outcomes for patients with thyroid cancer, patient age and tumor stage at initial treatment are crucial. Age is the most important prognostic variable for thyroid cancer mortality [27, 28]. Using Fisher’s exact test, we found that patients younger than 55 years were associated with higher N stage. No significant inflection points were found when age was treated as a continuous variable. To eliminate the effects of gender and location, multidimensional contingency analysis was performed, and CMH test and exact condition test were used. This association persisted at the cutoff point of 55 years, suggesting that maybe lymph node metastasis tends to occur in younger patients. This is consistent with previous studies [29, 30]. For example, Liu et al.'s analysis of data from 50,347 surgically treated PTC patients in the SEER database showed a linear correlation between diagnostic age and lymph node metastasis, with the rate of lymph node metastasis decreasing as age increased [30].
Our study does possess certain limitations that should be acknowledged. Firstly, the samples are derived from a single hospital, potentially limiting the diversity and generalizability of our findings. Moreover, thyroid cancer encompasses various subtypes, each potentially exhibiting distinct clinical and molecular attributes. Comprehensive research encompassing the entirety of thyroid cancer is imperative. Lastly, our dataset lacks follow-up treatment and survival data, necessitating future supplementation for more comprehensive investigations.
In summary, our study comprehensively examined the correlation between clinical factors and gene mutations in PTC patients. This effort aids in fostering an enhanced understanding of the distinctive attributes of PTC, consequently paving the way for improved diagnoses and more effective treatment strategies moving forward.
5 Conclusion
The findings of our study have illuminated several key insights. Specifically, we observed that younger PTC patients exhibit a heightened likelihood of lymph node metastasis. Furthermore, an elevated frequency of BRAF mutations correlates with a greater occurrence of RET fusions, both of which are associated with an increased susceptibility to lymph node metastasis. Additionally, these factors could potentially indicate a less favorable prognosis for affected individuals.
References
Chen P, Pan L, Huang W, Feng H, Ouyang W, Wu J, Wang J, Deng Y, Luo J, Chen Y. BRAF V600E and lymph node metastases in papillary thyroid cancer. Endocr Connect. 2020;9(10):999–1008.
Rahbari R, Zhang L, Kebebew E. Thyroid cancer gender disparity. Future Oncol (Lond, Engl). 2010;6(11):1771–9.
Kim S, Roh J, Gong G, Cho K, Choi S, Nam S, Kim S. Differences in the recurrence and survival of patients with symptomatic and asymptomatic papillary thyroid carcinoma: an observational study of 11,265 person-years of follow-up. Thyroid. 2016;26(10):1472–9.
Lee Y, Sung T, Kim W, Chung K, Yoon J, Hong S. Risk factors for recurrence in patients with papillary thyroid carcinoma undergoing modified radical neck dissection. Br J Surg. 2016;103(8):1020–5.
Lim H, Devesa S, Sosa J, Check D, Kitahara C. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017;317(13):1338–48.
Hoang J, Nguyen X, Davies L. Overdiagnosis of thyroid cancer: answers to five key questions. Acad Radiol. 2015;22(8):1024–9.
Nikiforov Y, Nikiforova M. Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol. 2011;7(10):569–80.
Haugen B, Alexander E, Bible K, Doherty G, Mandel S, Nikiforov Y, Pacini F, Randolph G, Sawka A, Schlumberger M, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133.
Ge J, Wang J, Wang H, Jiang X, Liao Q, Gong Q, Mo Y, Li X, Li G, Xiong W, et al. BRAFThe V600E mutation is a predictor of the effect of radioiodine therapy in papillary thyroid cancer. J Cancer. 2020;11(4):932–9.
Xing M. Molecular pathogenesis and mechanisms of thyroid cancer. Nat Rev Cancer. 2013;13(3):184–99.
Li C, Lee K, Schneider E, Zeiger M. BRAF V600E mutation and its association with clinicopathological features of papillary thyroid cancer: a meta-analysis. J Clin Endocrinol Metab. 2012;97(12):4559–70.
Liang J, Cai W, Feng D, Teng H, Mao F, Jiang Y, Hu S, Li X, Zhang Y, Liu B, et al. Genetic landscape of papillary thyroid carcinoma in the Chinese population. J Pathol. 2018;244(2):215–26.
Wang Z, Tang P, Hua S, Gao J, Zhang B, Wan H, Wu Q, Zhang J, Chen G. BRAF genetic and clinicopathologic characteristics of papillary thyroid carcinoma in the Chinese population: high mutation allele frequency, multiple driver gene mutations, and fusion may indicate more advanced TN stage. Onco Targets Ther. 2022;15:147–57.
Zuguang G, Roland E, Matthias S. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 2016;32(18):2847–9.
Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, Li L, Wei W, He J. Cancer incidence and mortality in China, 2022. Zhonghua Zhong Liu Za Zhi. 2024;46(3):221–31.
Freddie B, Mathieu L, Hyuna S, Jacques F, Rebecca L S, Isabelle S, Ahmedin J. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229–63.
Jingxin M, Lijing T, Ling F, Cheng T, Zhaojing Z, Yan L. Systematic pharmacology-based strategy to explore the mechanism of Semen Strychni for treatment of papillary thyroid carcinoma. Sci Rep. 2023;13(1):18492.
Baoyu W, Pengyi D, Wenli D, Peng W, Zhizhi D, Chaojun Y, Jinling T, Tao H, Kai Y. Association between programmed cell death ligand 1 expression and thyroid cancer: a meta-analysis. Medicine (Baltimore). 2021;100:e25315.
DiGennaro C, Vahdatzad V, Jalali M, Toumi A, Watson T, Gazelle G, Mercaldo N, Lubitz C. Assessing bias and limitations of clinical validation studies of molecular diagnostic tests for indeterminate thyroid nodules: systematic review and meta-analysis. Thyroid. 2022;32(10):1144–57.
Cha Y, Koo J. Next-generation sequencing in thyroid cancer. J Transl Med. 2016;14(1):322.
Salvatore D, Santoro M, Schlumberger M. The importance of the RET gene in thyroid cancer and therapeutic implications. Nat Rev Endocrinol. 2021;17(5):296–306.
Guerra A, Fugazzola L, Marotta V, Cirillo M, Rossi S, Cirello V, Forno I, Moccia T, Budillon A, Vitale M. A high percentage of BRAFV600E alleles in papillary thyroid carcinoma predicts a poorer outcome. J Clin Endocrinol Metab. 2012;97(7):2333–40.
Kim M, Bae J, Lim D, Lee H, Jeon S, Park G, Jung C. Quantification of BRAF V600E alleles predicts papillary thyroid cancer progression. Endocr Relat Cancer. 2014;21(6):891–902.
Integrated genomic characterization of papillary thyroid carcinoma. Cell. 2014;159(3):676–90.
Morton L, Karyadi D, Stewart C, Bogdanova T, Dawson E, Steinberg M, Dai J, Hartley S, Schonfeld S, Sampson J, et al. Radiation-related genomic profile of papillary thyroid carcinoma after the Chernobyl accident. Science (New York, NY). 2021;372(6543):eabg2538.
Zheng X, Peng C, Gao M, Zhi J, Hou X, Zhao J, Wei X, Chi J, Li D, Qian B. Risk factors for cervical lymph node metastasis in papillary thyroid microcarcinoma: a study of 1,587 patients. Cancer Biol Med. 2019;16(1):121–30.
Alexandra K, Rouhi F, Iwao S, Akira M, Lehana T, David PG, Sangeet G, Anna MS. Association of patient age with progression of low-risk papillary thyroid carcinoma under active surveillance: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2020;146:552.
Chou R, Dana T, Haymart M, Leung A, Tufano R, Sosa J, Ringel M. Active surveillance versus thyroid surgery for differentiated thyroid cancer: a systematic review. Thyroid. 2022;32(4):351–67.
Miranda-Filho A, Lortet-Tieulent J, Bray F, Cao B, Franceschi S, Vaccarella S, Dal Maso L. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 2021;9(4):225–34.
Yuanchao L, Yizeng W, Ke Z, Dongyang L, Zuoyu C, Ruoyu J, Xiaoning W, Xianghui H. Lymph node metastasis in young and middle-aged papillary thyroid carcinoma patients: a SEER-based cohort study. BMC Cancer. 2020;20(1):181.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors’ contributions
QW and BY designed the research study and wrote the manuscript. SL Z and YJ Z co-wrote the manuscript and was responsible for data analysis. DW L co-designed the manuscript and oversaw writing of the manuscript. DL W and ZF X optimized the experimental approach and provided general guidance. HJ M, LX D, YH Z, and JW searched the clinical data. ZB H optimized the experimental approach. All authors contributed to editorial changes in the manuscript. All authors read and approved the final manuscript.
Funding
No funding to report.
Availability of data and materials
The datasets used and/or analyzed during the current study will be made available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Competing interests
Qiang Wang, Bo Yu, Shuilong Zhang, Dongliang Wang, Zhifu Xiao, Hongjing Meng, Lingxiang Dong, Yuhang Zhang, Jie Wu, Zebin Hou, Yunji Zhu, and Dewei Li declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Shanxi Provincial People’s Hospital, and was conducted in accordance with the Declaration of Helsinki.
Consent to participate
All participants provided written informed consent at the time of sample collection.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, Q., Yu, B., Zhang, S. et al. Papillary Thyroid Carcinoma: Correlation Between Molecular and Clinical Features. Mol Diagn Ther (2024). https://doi.org/10.1007/s40291-024-00721-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s40291-024-00721-1