Abstract
Rationale
Atrial fibrillation (AF) is associated with an increased risk of thromboembolism. This risk is currently assessed with scoring systems based on clinical characteristics. However, these tools have limited prognostic performance. Circulating biomarkers are proposed for improved prediction of major clinical events and individualization of treatments in patients with AF.
Objective
The aim was to assess the cost-effectiveness of precision medicine (PM), i.e., the use of combined biomarkers and clinical variables, in comparison to standard of care (SOC) for risk stratification in a hypothetical cohort of AF patients at risk of stroke.
Methods
A Markov cohort model was developed to evaluate the costs and quality-adjusted life-years (QALYs) of PM compared to SOC, over 20 years using a Canadian healthcare system perspective.
Results
PM decreased the mean per-patient overall costs by 7% ($94,932 vs $102,057 [Canadian dollars], respectively) and increased the QALYs by 12% (8.77 vs 7.68 QALYs, respectively). The calculated incremental cost-effectiveness ratio was negative, indicating that PM is an economically dominant strategy. These results were robust to one-way and probabilistic sensitivity analyses.
Conclusion
PM compared to SOC is economically dominant and is projected to generate cost savings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Accurate stroke risk stratification in atrial fibrillation is key for optimal treatment decisions. The currently endorsed and widely used risk score tools rely on clinical variables (standard of care [SOC]) and have limited prognostic performance. |
Using a combination of biomarkers and clinical characteristics (precision medicine [PM]) improves prognostication. |
Our cost-effectiveness model shows PM to increase quality-adjusted life-years and decrease costs versus SOC. PM is economically dominant. |
1 Introduction
Atrial fibrillation (AF) is a highly prevalent condition causing a considerable health burden worldwide [1,2,3]. AF predisposes patients to an increased risk of stroke and systemic embolism, two complications with high rates of morbidity, disability, and mortality [4,5,6,7]. A key goal in the clinical management of AF is the prevention of stroke, which depends on the accurate assessment of risk in individual patients and the early initiation of preventive therapy. Proper risk stratification helps the clinician to assess whether the risk of stroke is high enough to warrant the administration of an oral anticoagulant (OAC), a therapy proven to be effective in reducing the incidence of stroke, while carrying an increased risk of bleeding [4, 8].
Current clinical practice relies on demographic and clinical risk scores prediction models for stratifying patients with AF. The most endorsed and commonly used risk score instrument for stroke is the CHA2DS2-VASc [9] index, an updated version of CHADS2 [10] (congestive heart failure, hypertension, age ≥ 75 years, diabetes, and stroke or transient ischemic attack) with three additional variables (vascular disease, age 65–74, and female sex), and for bleeding, it is the HAS-BLED [11] index (hypertension, abnormal renal or liver function, stroke, bleeding history/predisposition, labile international normalized ratio [INR], elderly [≥ 65 years], and drug or alcohol use). Both tools are based on a scoring system that awards points to each parameter. The resulting cumulative score is used to classify patients into a low-, intermediate-, or high-risk stratum. Despite their popularity and endorsement, these clinical risk factor-based tools have demonstrated limited prognostic performance [12, 13].
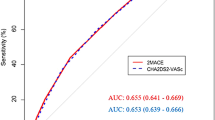
More recently, research in this field has explored the potential role of circulating biomarkers in improving the prediction or early diagnosis of stroke in patients with AF. Substudies [14,15,16,17] of large phase III trials [18,19,20] have analyzed biomarkers implicated in myocardial injury, myocardial stress and dysfunction, myocardial fibrosis, renal dysfunction, inflammation, and coagulation activity. Among those studied, cardiac troponin (cTn), N-terminal prohormone of brain natriuretic peptide (NT-proBNP), d-dimer, and growth-differentiation factor 15 (GDF-15) were identified as having an independent association with stroke/systemic embolism, bleeding, and/or death. These findings led to the development and validation of the ABC-AF risk scores [16, 17, 21]. The ABC-Stroke [17], ABC-Bleeding [16], and ABC-Death [21] scores include a combination of biomarkers (cTn, NT-proBNP, GDF-15, hemoglobin) and clinical parameters (age, prior stroke/transient ischemic attack [TIA], bleeding, heart failure) with the highest prognostic value and with improved prediction performance compared to existing risk scores (c-indices: ABC-Stroke 0.68 [CI 0.65, 0.71] vs CHA2DS2-VASc 0.62 [CI 0.60, 0.65]; ABC-Bleeding 0.68 [CI 0.66,0.70] vs HAS-BLED 0.61 [CI 0.59, 0.63]).
Like the clinical risk scores, the ABC-AF risk scores are based on a scoring system that attributes points to each parameter. Among the parameters that compose the ABC-AF nomograms, only one is binary (prior stroke/TIA on ABC-Stroke, previous bleeding on ABC-Bleeding, and heart failure on ABC-Death). The others are continuous variables (age and cTn on all three nomograms, NT-proBNP on ABC-Stroke and ABC-Death, and GDF-15 and hemoglobin on ABC-Bleeding and ABC-Death). Each parameter value is rated on a “points” scale of 0–10. In the ABC-Stroke [17] nomogram, for example, the “points” scale total is applied on a “total points” scale of 0–30 to find the corresponding 1-year stroke/systemic embolism risk on a scale of 0.01 and 0.15 and the 3-year risk on a scale of 0.01 and 0.3. These scales differ in the ABC-Bleeding [16] and the ABC-Death [21] nomograms.
Research on the utility of biomarkers as decision-support tools in AF is constantly growing. In this area, several questions remain, particularly those related to biomarkers’ cut-off values for the initiation and selection of treatment, the optimal frequency for measuring different biomarkers, and, finally, whether their usefulness in AF would translate into an added economic value. Thus, the objective of the present study was to evaluate the economic value of using the ABC-Stroke and ABC-Bleeding risk scores as an alternative to solely clinical-based risk scores (CHA2DS2-VASc and HAS-BLED) to stratify risks and guide the treatment decision in AF patients at risk of stroke (CHA2DS2-VASc > 1).
2 Methods
2.1 Type of Economic Evaluation
A cost-utility analysis was conducted to compare the incremental cost per quality-adjusted life-year (QALY) gained of two strategies for the clinical management of a hypothetical cohort of AF patients at risk of stroke (CHA2DS2-VASc > 1): “Precision Medicine” (PM) versus “standard of care” (SOC). The strategies were defined as follows:
-
SOC: The use of clinical risk scores (CHA2DS2-VASc and HAS-BLED) to assess the stroke and bleeding risks and to determine the pharmacological strategy based on current treatment recommendations. As the hypothetical patients in the model were at risk of stroke (CHA2DS2-VASc > 1), all patients under SOC were treated with an OAC.
-
PM: The use of the ABC-Stroke and ABC-Bleeding risk scores, i.e., a combination of biomarkers (high-sensitivity troponin I [hs-TnI], NT-proBNP, GDF-15, hemoglobin) and clinical information (age, prior stroke/TIA, previous bleeding), to assess the stroke and bleeding risks and to determine the pharmacological treatment strategy.
The analysis adopted a third-party payer perspective relating to a Canadian ministry of health where only direct medical costs were considered. A 1.5% discount rate was applied to costs and QALYs, in accordance with the Canadian Agency for Drugs and Technologies in Health (CADTH) guidelines [22]. Discount rates of 0 and 3% were included in the sensitivity analysis.
2.2 Target Population
The hypothetical population for this economic analysis was AF patients aged 65 years or older at risk for stroke (CHA2DS2-VASc > 1).
2.3 Time Horizon
The base-case analysis adopted a time horizon of 20 years with a cycle length of 3 months. This time length was considered sufficient to detect differences in the model outcomes between SOC and PM, with sensitivity analyses conducted at 10 and 30 years.
2.4 Model Structure
A Markov cohort model was used to compare the alternative strategies: SOC versus PM (Fig. 1). The clinical pathway was defined as follows: AF patients with at least one risk factor for stroke would enter the model, remain in this initial state (event-free) or experience a new health event. The model simulated patients’ progression to four major health states: stroke and systemic embolism, myocardial infarction (MI), major bleeding, and death from any cause. Stroke events were either ischemic or hemorrhagic, and bleeding events were intracranial hemorrhage (ICH) or any other major bleed. In each health state, the model allowed only one recurrent event for each patient. All non-fatal event health states were modeled as semi-absorbing states, i.e., patients can only transition to the death state. Event rates for stroke/systemic embolism, MI, major bleeding, and death were adjusted in each cycle to reflect an increase in risk over time, e.g., due to aging or a previous event.
Model diagram. AF atrial fibrillation, ICH intracranial hemorrhage, IS ischemic stroke, MB major bleed, MI myocardial infarction, SE systemic embolism.  Decision node—branches represent strategies;
Decision node—branches represent strategies;  Markov node—branches are health states;
Markov node—branches are health states;  Chance node—splits pathway into branches;
Chance node—splits pathway into branches;  Terminal node: endpoint for pathway or cycle
Terminal node: endpoint for pathway or cycle
The treatment model was based on current treatment guidelines and the prescription trends in Quebec [23]. All treated patients under SOC and PM received an OAC, with the assumption that 87% would be on a non-vitamin K oral anticoagulant (NOAC) and 13% on a vitamin K antagonist (VKA).
Patients in the PM strategy arm could either be at low (< 1%), intermediate (1–2%), or high risk (> 2%) of stroke. In the base-case analysis, the model assumed 28% of patients would be at low, 49% at intermediate, and 23% at high risk of stroke. These assumptions were based on the ABC-Stroke risk score data [16, 17, 21] and were varied in the sensitivity analysis. Patients at low stroke risk were untreated until a first ischemic stroke, then treated with an OAC. Fifty percent of those at intermediate stroke risk were treated with an OAC, reflecting a group where the risk of stroke outweighs the risk of bleeding. The other half were left untreated until a first stroke event, reflecting a group where the risk of stroke would be such that an OAC therapy would represent more harm than benefits given its associated risk of bleeding. These proportions were varied in the sensitivity analysis. All patients at high stroke risk were assumed to receive an OAC regardless of their bleeding risk.
2.5 Clinical Event Rates
The baseline estimates of the annual clinical event rates for the SOC strategy (Table 1) were obtained from the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial [19]. Those for the PM strategy, low and intermediate-untreated risk groups (Tables 2, 3) were obtained from published studies in low-risk and/or untreated or non-anticoagulated patients [24, 25]. The clinical event rates for the intermediate-treated and high-risk groups (Tables 4, 5) were obtained from the ABC-Stroke [17] and ABC-Bleeding [16] risk score data, except for ischemic and hemorrhagic stroke, MI, and death, which were derived from the hs-TnI substudy [26]. Annual event rates were increased by a factor of 1.46 for ischemic stroke, 1.97 for bleeding, and 1.30 for MI per decade of life [27]. Additionally, an event rate adjustment was incorporated in the model to account for an increased risk of recurrence after a first event of ischemic stroke (2.20) and MI (2.04) based on long-term prognosis and survival data from epidemiological studies [9, 28]. These increases were assumed to be half in the PM low risk (< 1%) group.
The distribution of patients experiencing certain events as to the subtype of the event was obtained from a published study [27] of a similar patient population and applied to the cohort during each cycle. The base-case event rates were varied by ± 25% in the sensitivity analysis.
2.6 Mortality
Death rates were derived from the ARISTOTLE trial [19] and the hs-TnI substudy [26]. An event fatality rate, derived from published trials [27, 29], was applied on the occurrence of each event. All fatal events were transferred, in the next cycle, to the “Death – All Cause” state.
2.7 Utility Values
Utility/disutility values (Table 6) were sourced from published studies in similar populations and applied whenever a patient experienced an event [30,31,32]. Utility values are measured on a scale from 0 (equivalent to death) to 1 (perfect health). In the initial AF disease state, a mean decrement of 0.045 was applied to the utility value for AF (0.81) to account for disutility due to age, OAC treatment, and stroke initial risk level. As patients progressed to different health states, an event decrement was also applied to the initial AF utility value (0.77). The model assumed no difference in utility values between SOC and PM. The disutility values were assumed to apply from the cycle in which the event occurred until the end of the follow-up period or death. Upper and lower disutility values (95% confidence interval [CI]) were obtained from the literature and applied in the sensitivity analysis [30,31,32].
2.8 Resource Use and Costs
In the initial AF health state, when no health events have yet occurred, the cost generated under SOC included the drug cost, whereas under PM, it included the biomarker testing cost for the untreated cohorts plus drug costs for the treated cohorts.
Acute events (one-time cost) and long-term costs (in Canadian dollars [CAD]) (Table 7) were based on Canadian sources from published literature [31, 32]. The cost of 3 months’ medication was obtained from the “Régie de l’Assurance Maladie du Québec” price list [33], with inclusion of a $8.50 prescription fee and an 8% pharmacist’s markup. The cost of drugs assumed daily use and no discontinuation. Since treated patients could receive either a VKA or an NOAC, the cost of treatment including INR monitoring costs was averaged in the base-case analysis. Further, considering the recent approval by Health Canada of a generic version of apixaban and the upcoming listing of the drug on Canadian drug formularies, the total price of treatment was lowered, in a sensitivity analysis, to include the price of generic apixaban. This price was assumed to be 25% of the original cost. The costs of biomarker tests were obtained from published literature [34,35,36,37] and were based on a frequency of once per 3-month cycle, since data have shown minimal fluctuation in biomarkers’ concentrations over a short time period [38]. The cost of drugs, acute events, and long-term monitoring were updated to 2022 CAD by using the Bank of Canada inflation calculator, which is based on the Consumer Price Index (CPI) [39]. All costs, except drug cost, were varied by ± 25% in the sensitivity analysis.
2.9 Analyses
The incremental cost-effectiveness ratio (ICER) was computed to determine the costs/QALY of PM versus SOC over 20 years at a Canadian willingness to pay (WTP) of $50K CAD.
One-way sensitivity analyses were conducted to test the impact on the ICER of changes in underlying parameter values and assumptions within the model. The analyses included key model parameters and were presented as a tornado diagram. Joint model parameter uncertainty was assessed using probabilistic sensitivity analysis (PSA). The PSA was conducted using Monte Carlo simulations [40]. Estimates of incremental costs and QALYs were obtained by running 10,000 iterations where the value of each model parameter was randomly sampled from a probability distribution. A beta distribution was used for varying the clinical events and utility values, and a gamma distribution for costs, except drug cost (fixed). All parameters were varied by ± 25% except where measures of dispersion were available. Cost-effectiveness acceptability curves (CEACs) were derived to illustrate the probability of each strategy being optimal given different values of WTP/QALY gained. Additionally, an incremental cost-effectiveness scatter plot was generated to present the difference in the total aggregated costs versus the difference in QALYs accrued through 20-year use of PM versus SOC.
The cost-effectiveness analyses were carried out using the TreeAge Pro Healthcare 2022 software (TreeAge Software, Williamstown, MA, USA; software available at http://www.treeage.com).
2.10 Model Validation
At the design stage, the face validity of the model was examined by a clinical pharmacology and pharmacoepidemiology specialist (J. LeLorier). The purpose of the evaluation was to check the model's clinical assumptions and structure in view of what is known in the field and available data. Internal validation was done as a quality check, first, electronically by using the TreeAge software model validation tool and, second, manually. Electronic validation checked the model for errors such as coding, missing or unused data, end/terminal nodes, and consistency in half-cycle corrections. Manual validation included the logical structure of the model, a review of the model inputs against data sources, programming, i.e., coding, formulas, and their execution in the model, and the model results. The model results were validated at each step to ensure that the data generated were consistent with the expected data. For instance, the SOC strategy outcomes were equivalent to those of PM intermediate-risk, treated patients. This result was in line with the expected outcomes in these groups as the clinical data input for the SOC strategy was obtained from the ARISTOTLE trial [19], whose patient population was treated and had a mean CHADS2 of 2.1 (range 1 to ≥ 3). External validation was done by comparing the model results to those of the ARISTOPHANES [41] observational study, which assessed stroke/systemic embolism and major bleeding outcomes in a similar population.
3 Results
3.1 Base-Case Analysis
In this model, PM, as compared to SOC, resulted in a lower incidence of hemorrhagic events and deaths. Among a hypothetical cohort of 1000 AF patients followed over 20 years, PM is predicted to cause four fewer hemorrhagic strokes, 36 fewer ICHs, 119 fewer other major bleeds, and 119 fewer deaths than SOC. These benefits would be mainly generated by the low and low-intermediate risk groups not receiving an anticoagulant and, hence, avoiding the treatment’s bleeding adverse events. On the other hand, SOC, compared to PM, is predicted to cause fewer strokes/systemic embolisms and MI events (34 and 25, respectively). These benefits would result from the protective effect of anticoagulation therapy against stroke being broadened to patients who may have needed it.
The cost-effectiveness analysis showed PM, as compared to SOC, to decrease the mean per-patient overall costs by 7% ($94,932 vs $102,057 CAD, respectively) and to increase the QALYs by 12% (8.77 vs 7.68 QALYs, respectively). The resulting ICER was negative (−$6541 CAD) indicating that PM was a dominant strategy (Table 8).
3.2 One-Way Sensitivity Analysis
A tornado diagram (Fig. 2) presents the results from one-way sensitivity analyses with the top 25 parameters that had the most impact on the ICERs. The ICERs varied between −$13,209 and $3025 CAD per QALY gained. Those values were obtained with a ± 25% variation in the rate of stroke/systemic embolism under SOC. Regardless of the variation in costs, utility/disutility, events’ rate, time horizon, or discount rate, the PM strategy remained dominant.
Tornado diagram representing one-way sensitivity analyses. The diagram shows the top 25 parameters (clinical event rate, cost, or utility) whose variation had the most impact on the ICER. The solid vertical lines represent: (1) the base-case EV of the ICER of PM compared to SOC and (2) the WTP at $50K CAD. The horizontal bars indicate the range of the ICERs obtained by varying each parameter between its lowest and highest value while holding all others constant. The highest and lower ICER values were obtained with ± 25% variation of stroke/SE rate under SOC. PM was a dominant strategy in all scenarios. AF atrial fibrillation, CAD Canadian dollars, EV expected value, ICER incremental cost-effectiveness ratio, ICH intracranial hemorrhage, IS ischemic stroke, MI myocardial infarction, OAC oral anticoagulant, PM precision medicine, SE systemic embolism, SOC standard of care, WTP willingness to pay
3.3 Scenario Analysis
Since the decision of treatment under PM was based on our best clinical judgement and the observed stroke risk in the ABC-AF score studies, we conducted sensitivity analyses to assess the impact of varying the size of the low-risk and low-intermediate-risk cohorts and, consequently, the rate of treated and untreated patients in the model. Reducing the relative size of the low-risk cohort from 28% (base-case value) to 0%, increased the ICER from −$6541 to $12,539 CAD per QALY gained. Also, reducing the low-intermediate cohort (untreated group) from 50% (base-case value) to 0%, i.e., 100% of patients in the intermediate group were treated, decreased the ICER to − $12,860 CAD per QALY gained. Additionally, lowering the total cost of treatment by including the price of a generic NOAC resulted in an ICER of − $2119 CAD per QALY gained, and varying the time horizon to 10 or 30 years generated ICERs of − $11,975 and − $3167 CAD per QALY gained, respectively. In all scenarios, the PM strategy remained dominant.
3.4 Probabilistic Sensitivity Analysis
The PSA resulted in a mean ICER (95% CI) of − $6555 (− $11,406 to − $1896) CAD per QALY gained. The conclusions relating to the cost-effectiveness analysis were robust. The incremental CEAC (Fig. 3a) showed PM to be 100% cost-effective at a WTP threshold between $0 and $100K CAD per QALY gained. Furthermore, 100% of the trials (10,000 iterations) showed PM to be a dominant strategy, representing a maximum net benefit over SOC (Fig. 3b).
Probabilistic sensitivity analysis of precision medicine (PM) vs standard of care (SOC). a Cost-effectiveness acceptability curve. The red line representing PM shows it is 100% cost-effective over the range of the willingness-to-pay values. b Incremental cost-effectiveness scatter plot. Each green dot represents the incremental cost over the incremental quality-adjusted life-year obtained in each of the 10,000 simulations. PM is 100% dominant
4 Discussion
Circulating biomarkers have been proposed to improve risk stratification and the clinical management of AF patients. The present study showed that this clinical utility generates an added economic value compared to the SOC. In the base-case analysis, PM, i.e., use of the ABC-Stroke and the ABC-Bleeding scores for risk stratification and treatment management, was cost-effective at a WTP of $50K CAD and at a WTP as low as $0 CAD per QALY gained compared to SOC. The estimated ICER was − $6541 CAD per QALY gained. PM reduced healthcare costs by 7%, increased QALYs by 12%, and was, therefore, an economically dominant strategy. These results were robust in all sensitivity analyses.
The added economic value of PM was driven by the discriminatory capacity of the ABC-Stroke and ABC-Bleeding risk scores to identify among patients classified “at risk” of stroke with SOC a subgroup at low stroke risk who will likely not benefit from an OAC, while being put at unnecessary risk of bleeding. In our model, this translated into four fewer hemorrhagic strokes, 36 fewer ICHs, 119 fewer major bleeds, and 119 fewer deaths than with SOC.
4.1 Clinical Implications
The relationship between biomarkers and AF has been well established [42]. Studies have demonstrated that abnormal biomarker concentrations reflecting cardiac and renal dysfunction as well as inflammation and oxidative stress identify patients at higher risk of developing AF. Merino-Merino et al. [43], in a recent study comparing AF patients with healthy study participants, showed a relationship between NT-proBNP, ST2, high-sensitivity cardiac troponin T, and the presence of AF, with NT-proBNP showing the highest yield in differentiating patients with AF from healthy participants.
In the AF setting, including biomarkers in risk scales for stroke and bleeding risk prediction added a statistically significant improvement to conventional clinical-based scores. Validation studies of the ABC-Stroke and ABC-Bleeding scores (ABC-AF scores) demonstrated an enhanced discriminatory performance when compared to CHA2DS2-VASc and HAS-BLED scores (c-indices: ABC-Stroke 0.68 [CI 0.65, 0.71] vs CHA2DS2-VASc 0.62 [CI 0.60, 0.65]; ABC-Bleeding 0.68 [CI 0.66, 0.70] vs HAS-BLED 0.61 [CI 0.59, 0.63]) [16, 17]. In multivariate analyses, congestive heart failure, hypertension, diabetes mellitus, and gender added very little discriminatory information beyond what was provided by circulating biomarkers included in the ABC-AF scores. This finding supports the evidence of the limited ability of clinical variables-based risk scores to accurately predict risk in this population and underscores the need for improved risk prediction in AF.
In the management of patients with AF, physicians are faced with the challenge of finding a balance between the benefits of anticoagulation therapy and the risk of bleeding. The ABC-AF scores may be useful tools to identify patients who may benefit most from anticoagulation since they are constituted by specific markers with less overlap between thromboembolic and bleeding risk. In patients at low risk for both stroke and bleeding, studies have demonstrated no meaningful difference in outcomes when patients were treated with NOAC (low or high dose) or VKA. By contrast, the NOAC regimen was superior to the VKA regimen among patients with high ABC-Stroke or ABC-Bleeding scores. Further, when a high risk of both stroke and bleeding was predicted, patients had the best outcome with a higher dose of the NOAC, while those with a low risk of stroke but with a high risk of bleeding had the best outcomes with the lower dosage [17].
Biomarkers play an important role in PM. Since ABC-Stroke and ABC-Bleeding are based on a continuous variables scoring system, they allow the monitoring of increases or decreases in risk of future events, and thus provide decision support for personalized patient care. However, more data are needed on their applicability to daily practice and on their cost-effectiveness compared to usual care, which was shown in our study to generate economic savings.
4.2 Limitations
The main limitation of this study is the fact that it is based on a hypothetical cohort of AF patients whose data were derived from several published studies. The ARISTOTLE [19] clinical trial and its biomarker substudies [16, 17, 21] were the principal source of data for the anticoagulated cohorts, whereas the AVERROES trial [29] and an observational study by Lip et al. [24] were the data source for the untreated cohorts. Although efforts were made to match the populations on two criteria, risk score and absence of OAC therapy, the event rates used may not be reflective of real-life observations in these groups. Also, differences between the trials and population characteristics may have contributed to uncertainties in the model.
Our model assessed the clinical and economic benefits in patients at risk of stroke who, under SOC, would generally be treated with OAC without accounting for those untreated patients under SOC who may be treated under PM. As the ABC-Stroke risk score has the potential of reclassifying risk levels upward or downward, this may have implications in terms of overall clinical benefits and costs. Nevertheless, the internal validation of the ABC-Stroke score in a subgroup of patients without prior stroke, taken as a proxy for a primary prevention setting, showed a higher c-index compared to CHA2DS2-VASc score (0.66 vs 0.59, P < 0.001) [17]. Data from these studies have also indicated that, within both low- and high-risk CHA2DS2-VASc score cohorts, the ABC-Stroke further stratified patients into subgroups with 1-year observed event rates close to the 1-year predicted by the ABC-Stroke score. Based on these observations, one may assume that any misclassification upward by the ABC-AF scores, e.g., false positive cases, would be outweighed by their increased accuracy versus CHA2DS2-VASc to identify true positive patients needing anticoagulation therapy. This, ultimately, would result in a decrease in harmful events and, consequently, costs.
One of the main advantages of measuring biomarker levels in AF patients is the ability to monitor changes in atrial dysfunction and thromboembolic risk over time and to adjust treatment accordingly. In our model, the event rates used in the PM strategy arm came from the ABC-AF risk score studies, which assessed the biomarkers’ levels at study entry and the risk of events over 1.9 years. To account for changes in event rates over time, we modeled the increases in risks with every decade of age and after a first event, using published data [27, 31]. We also assumed that these increases were the same for all groups but half in the PM low-risk group. This may have led to an underestimation of the outcomes in this group and/or an over or underestimation of the outcomes in the PM intermediate- to high-risk groups. Additionally, there are presently no guidelines regarding the optimal cut-off value of the ABC-AF risk scores as a decisive tool for selecting different treatment strategies. Our analysis considered OAC treatment for the mid-intermediate- and high-risk patients without considering changes to the type of OAC or its dosage in relation to the level of risk or other clinical parameters. This treatment strategy represents our best clinical judgement based on the available data and may not represent an optimal approach for these patients. Translating biomarker study results into clear clinical practice guidelines would help the medical community understand how the ABC-AF risk scores may be used as decision support tools while accounting for all potential benefits and harms to patients. Nevertheless, from a cost-effectiveness perspective, our analysis showed PM to remain a dominant strategy even when there were no patients in the PM low-risk group or when the entire intermediate group was treated with an OAC.
Other limitations include the use of data from a controlled trial setting where patients are generally treated and followed under optimal conditions; thus, the outcomes observed may not be representative of real-life data. Other data used in the model such as patient definition (age and risk level), OAC type and dosage regimen, drug and event costs, and the Canadian healthcare system perspective make the results not necessarily generalizable to other settings. We acknowledge the possibility that minor unforeseen errors may have escaped the scrutiny and thoroughness of our validation processes. If any, we are confident these would have little to no impact on the overall results and conclusions. Finally, we were unable to compare our results to others since no studies on the cost-effectiveness of the ABC-AF scores have been published.
5 Conclusion
This cost-effectiveness analysis indicates that PM, i.e., using the ABC-Stroke and the ABC-Bleeding risk score tools for risk stratification and treatment selection in non-valvular AF patients, generates cost savings and increased effectiveness compared to SOC and is therefore economically dominant.
References
Chugh SS, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129(8):837–47.
Benjamin EJ, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–528.
Piccini JP, et al. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries: 1993–2007. Circ Cardiovasc Quality Outcomes. 2012;5(1):85–93.
Kirchhof P, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Kardiologia Polska (Polish Heart Journal). 2016;74(12):1359–469.
O’Donnell MJ, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case–control study. Lancet. 2016;388(10046):761–75.
Wolf PA, et al. Impact of atrial fibrillation on mortality, stroke, and medical costs. Arch Intern Med. 1998;158(3):229–34.
Staerk L, et al. Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res. 2017;120(9):1501–17.
Andrade JG, et al. The 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society comprehensive guidelines for the management of atrial fibrillation. Can J Cardiol. 2020;36(12):1847–948.
Lip GY, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–72.
Gage BF, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–70.
Pisters R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
Nielsen PB, et al. Stroke and thromboembolic event rates in atrial fibrillation according to different guideline treatment thresholds: a nationwide cohort study. Sci Rep. 2016;6(1):1–7.
Borre ED, et al. Predicting thromboembolic and bleeding event risk in patients with non-valvular atrial fibrillation: a systematic review. Thromb Haemost. 2018;118(12):2171–87.
Siegbahn A, et al. d-Dimer and factor VIIa in atrial fibrillation–prognostic values for cardiovascular events and effects of anticoagulation therapy. Thromb Haemost. 2016;116(05):921–30.
Ruff CT, et al. Cardiovascular biomarker score and clinical outcomes in patients with atrial fibrillation: a subanalysis of the ENGAGE AF-TIMI 48 Randomized clinical trial. JAMA Cardiol. 2016;1(9):999–1006.
Hijazi Z, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet. 2016;387(10035):2302–11.
Hijazi Z, et al. The ABC (age, biomarkers, clinical history) stroke risk score: a biomarker-based risk score for predicting stroke in atrial fibrillation. Eur Heart J. 2016;37(20):1582–90.
Giugliano RP, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Granger CB, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Paikin JS, Haroun MJ, Eikelboom JW. Dabigatran for stroke prevention in atrial fibrillation: the RE-LY trial. Expert Rev Cardiovasc Ther. 2011;9(3):279–86.
Hijazi Z, et al. A biomarker-based risk score to predict death in patients with atrial fibrillation: the ABC (age, biomarkers, clinical history) death risk score. Eur Heart J. 2018;39(6):477–85.
CADTH. Guidelines for the economic evaluation of health technologies: Canada. 2017.
Perreault S, et al. Oral anticoagulant prescription trends, profile use, and determinants of adherence in patients with atrial fibrillation. Pharmacotherapy J Hum Pharmacol Drug Therapy. 2020;40(1):40–54.
Lip GYH, et al. Oral anticoagulation, aspirin, or no therapy in patients with nonvalvular AF with 0 or 1 stroke risk factor based on the CHA2DS2-VASc score. J Am Coll Cardiol. 2015;65(14):1385–94.
Lip GYH, et al. Clinical and economic implications of apixaban versus aspirin in the low-risk nonvalvular atrial fibrillation patients. Stroke. 2015;46(10):2830–7.
Hijazi Z, et al. High-sensitivity troponin I for risk assessment in patients with atrial fibrillation: insights from the Apixaban for Reduction in Stroke and other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial. Circulation. 2014;129(6):625–34.
Dorian P, et al. Cost-effectiveness of apixaban vs. current standard of care for stroke prevention in patients with atrial fibrillation. Eur Heart J. 2014;35(28):1897–1906.
Cupples LA, et al. Preexisting cardiovascular conditions and long-term prognosis after initial myocardial infarction: the Framingham study. Am Heart J. 1993;125(3):863–72.
Connolly SJ, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(9):806–17.
Sullivan PW, et al. The cost effectiveness of anticoagulation management services for patients with atrial fibrillation and at high risk of stroke in the US. Pharmacoeconomics. 2006;24(10):1021–33.
Coyle D, et al. Cost-effectiveness of new oral anticoagulants compared with warfarin in preventing stroke and other cardiovascular events in patients with atrial fibrillation. Value Health. 2013;16(4):498–506.
Sorensen SV, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation: a Canadian payer perspective. Thromb Haemost. 2011;105(05):908–19.
Québec, R.d.l.A.M.d. Liste des Médicaments. 2022.
Almeida N, D.N. What is the added clinical value of pre-operative brain natriuretic peptide (BNP/NT-proBNP) in predicting post-operative cardiac complications in patients undergoing non-cardiac surgery across the MUHC RUIS? Montreal: Technology Assessment Unit of the McGill University Health Centre (MUHC); 2020. p. 1–39.
Health, O.M.o. and L.a.G. Branch. OHIP schedule of benefits for laboratory services. 2020.
Costing, O.C. OCC costing analysis tool. Ottawa, ON, 2018.
Drugs, C.A.f. and T.i. Health. High-sensitivity cardiac troponin for the rapid diagnosis of acute coronary syndrome in the emergency department: a clinical and cost-effectiveness evaluation. Canadian Agency for Drugs and Technologies in Health; 2013.
Hijazi Z, et al. Repeated measurements of cardiac biomarkers in atrial fibrillation and validation of the ABC stroke score over time. J Am Heart Assoc. 2017;6(6): e004851.
Calculator, I. Bank of Canada.
Briggs AH. Handling uncertainty in cost-effectiveness models. Pharmacoeconomics. 2000;17(5):479–500.
Lip GY, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients: the ARISTOPHANES study. Stroke. 2018;49(12):2933–44.
T O’Neal W, et al. Biomarkers and the prediction of atrial fibrillation: state of the art. Vasc Health Risk Manag. 2016;12:297.
Merino-Merino A, et al. A differential profile of biomarkers between patients with atrial fibrillation and healthy controls. J Personal Med. 2022;12(9):1406.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the Montreal Heart Institute. The Montreal Heart Institute received funding from the Health Collaboration Acceleration Fund (FACS) from the Government of Quebec.
Conflict of interest
Drs. G. Nakhlé and J. LeLorier have received Grants from the Montreal Heart Institute for this project. The Montreal Heart Institute received funding from the Health Collaboration Acceleration Fund (FACS) from the Government of Quebec. Drs. D. Roy, M. Samuel, and A. Dubois have no relevant financial or non-financial interests to disclose. Dr. J-C. Tardif reports Grants from Amarin, Grants and personal fees from AstraZeneca, Grants, personal fees, and other from Dalcor, Grants from Esperion, Grants from Ionis, Grants and personal fees from Sanofi, Grants and personal fees from Servier, Grants from RegenXBio, Grants from Novartis, Grants and personal fees from Pfizer, personal fees from HLS Pharmaceuticals, personal fees from Pendopharm, outside the submitted work. In addition, Dr. Tardif has a patent “Genetic markers for predicting responsiveness to therapy with hdl-raising or hdl mimicking agent” pending, a patent “Methods for using low dose colchicine after myocardial infarction” pending (invention assigned to the Montreal Heart Institute), a patent “Methods of treating a coronavirus infection using Colchicine” pending, and a patent “Early administration of low-dose colchicine after myocardial infarction" pending. Dr. L. Rivard reports Grants from Bayer Inc. during the conduct of the study and Grants from the Montreal Heart Institute Foundation, the Heart and Stroke Foundation of Canada, and the Canadian Institutes of Health Research (CHIR) outside the submitted work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Authorship statement
All persons who meet authorship criteria are listed as authors and all authors certify that they have approved the version of the manuscript to be published and take responsibility for the content of the manuscript.
Author contributions
GN: Ideas, formulation of research question, statement of hypothesis, development and design of methodology, creation of models, programming and statistical analysis, data collection, writing the initial draft, and finalizing manuscript for publication. J-CT and AD: Funding acquisition, critical review, commentary, and revisions. DR, LR, and MS: Critical review, commentary, and revisions. JL: Ideas, supervising of research, funding acquisition, critical review, commentary, and revisions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nakhlé, G., Tardif, JC., Roy, D. et al. A Cost-Effectiveness Analysis of Biomarkers for Risk Prediction in Atrial Fibrillation. Mol Diagn Ther 27, 383–394 (2023). https://doi.org/10.1007/s40291-023-00639-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-023-00639-0